Back to Journals » Neuropsychiatric Disease and Treatment » Volume 10
Clozapine-induced seizures, electroencephalography abnormalities, and clinical responses in Japanese patients with schizophrenia
Authors Kikuchi Y, Sato W, Ataka K, Yagisawa K, Omori Y, Kanbayashi T, Shimizu T
Received 22 June 2014
Accepted for publication 28 July 2014
Published 15 October 2014 Volume 2014:10 Pages 1973—1978
DOI https://doi.org/10.2147/NDT.S69784
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Roger Pinder
Yuka Sugawara Kikuchi, Wataru Sato, Keiichiro Ataka, Kiwamu Yagisawa, Yuki Omori, Takashi Kanbayashi, Tetsuo Shimizu
Department of Neuropsychiatry, Akita University Graduate School of Medicine, Hondo, Akita, Japan
Purpose: We describe electroencephalography (EEG) abnormalities and seizures associated with clozapine treatment in Japanese patients with schizophrenia and retrospectively compare EEG results and total Positive and Negative Syndrome Scale (PANSS [T]) scores before and after treatment.
Methods: Twenty-six patients with treatment-resistant schizophrenia were enrolled in this study. EEG measurements were obtained prior to clozapine treatment and every 4 weeks thereafter. EEG measurements were also obtained at the time of seizure. After seizures or EEG abnormalities were noted, additional EEGs were performed every 2 weeks. PANSS (T) scores were used to determine clozapine treatment outcome.
Results: All 26 patients had normal baseline EEG measurements, and ten patients (38.5%) later manifested EEG abnormalities. The mean age was significantly lower than in the abnormal EEG group. Six patients (23.1%) experienced seizures. The mean dose of clozapine at the first occurrence of seizure was 383.3 mg/day. Five of six patients who experienced seizures in this study were successfully treated with valproate or lamotrigine without discontinuation of clozapine. The one patient who continued to experience seizures was successfully treated without antiepileptic drugs. The mean baseline PANSS (T) scores were not significantly different between the normal and abnormal EEG groups, but the mean score in the abnormal EEG group was significantly lower than that in the normal EEG group at the final follow-up (P=0.02).
Conclusion: EEG abnormalities may appear in younger patients, and our findings indicate that there is no need to discontinue clozapine when seizures occur. EEG abnormalities that appeared after clozapine treatment were associated with a good clinical response.
Keywords: treatment-resistant schizophrenia, side effects, PANSS, convulsions
Introduction
Despite pharmacological advances, about 10%–30% of patients with schizophrenia exhibit little or no response to antipsychotic medications, and persistent symptoms make it difficult for these patients to re-enter society. Clozapine is effective against treatment-resistant schizophrenia (TRS) and was introduced to Japan in 2009. In Japan, all physicians who prescribe clozapine, as well as the patients receiving the drug, must be registered with the Clozaril Patient Monitoring Service (CPMS). In addition, clozapine is limited to patients with TRS according to the following poor response and poor tolerance criteria. The poor response criterion is a failure to respond to a sufficient term (at least 4 weeks) of treatment with a sufficient dose of at least two well-tolerated antipsychotics (including at least one atypical antipsychotic [eg, risperidone, perospirone, olanzapine, quetiapine, or aripiprazole at over 600 mg/day chlorpromazine equivalent]). The poor tolerance criterion is defined as a failure to adequately respond to monotherapy with at least two atypical antipsychotics (eg, risperidone perospirone, olanzapine, quetiapine, and aripiprazole) due to failure to increase the dose to a necessary level for any of the following reasons: occurrence or worsening of moderate or severe tardive dyskinesia, tardive dystonia, or other tardive extrapyramidal symptoms, or occurrence of uncontrolled parkinsonian symptoms, akathisia, or acute dystonia.
Clozapine also causes serious side effects, such as agranulocytosis and seizures. Clozapine-induced seizures are more frequent than agranulocytosis,1 and electroencephalography (EEG) abnormalities are even more common. The appearance of paroxysmal discharges indicates a high risk for convulsion.2 However, EEG abnormalities that develop after clozapine treatment appear to be associated with good responses.3 Herein, we describe EEG abnormalities and seizures associated with clozapine treatment in Japanese patients with schizophrenia and retrospectively compare EEG results and total Positive and Negative Syndrome Scale (PANSS [T]) scores before and after treatment.
Materials and methods
Subjects and demographic profiles
The subjects were all consecutive hospitalized patients with TRS. All patients met the criteria of poor response or poor tolerance described above. No patient had received clozapine before or had a history of prior seizure or brain injury. Twenty-eight patients were recruited in this study, but two patients were excluded because clozapine was discontinued when they developed side effects before post-treatment EEG measurement. One patient developed cardiomyopathy 4 weeks after starting clozapine, and the other developed agranulocytosis 3 weeks after initiating clozapine. Ultimately, 26 patients (eight males, 18 females) with an average age of 37 years were enrolled. Clozapine was initiated at a starting dose of 12.5 mg/day on the first day and was increased to 25 mg/day on the second day. On the third day and thereafter, the daily dose could be slowly increased in 25 mg increments to achieve a dose of up to 200 mg/day over 3 weeks. The dose was increased depending on the symptoms; however, at least 4 days were required to pass for dose increases in increments of up to 100 mg. The maximum dose in Japan is 600 mg/day. In principle, the duration of hospitalization was defined as 18 weeks after initiating clozapine according to the manufacturer’s specifications (Novartis International AG, Basel, Switzerland). However, as long as certain criteria were met, patients could be discharged before 18 weeks. These criteria were desirable for discharge; achievement of the maintenance dosage, at least 3 weeks’ hospitalization, improvement of clinical symptoms, and confirmation of safety.
EEG recording and clinical response
EEG recordings were performed with the use of the International 10–20 system and a 21-channel monitor. The patient’s history and medications were blinded to readers who read the EEG recordings. EEG measures were obtained several days prior to the initiation of clozapine treatment, and every 4 weeks thereafter. EEG measures were also obtained immediately after seizures occurred. Following seizures or EEG abnormalities, additional EEGs were performed every 2 weeks. PANSS (T) scores were used to determine clozapine treatment outcomes.
Data analysis
The incidences of seizures and EEG abnormality were obtained, and subjects were divided into two groups depending on whether their EEG recording was normal or abnormal. Student’s t-tests and chi-square tests were used to compare demographic profiles between the two groups. PANSS (T) scores were compared at baseline and at the last observation with Student’s t-tests.
Results
Clozapine-induced EEG abnormality
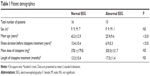
All patients had normal baseline EEG measures, and ten patients (38.5%) later showed EEG abnormalities. The daily dose of clozapine at the occurrence of EEG abnormalities varied from 125 to 600 mg (mean 305 mg/day). There were no significant differences between the normal and abnormal EEG groups in terms of sex, mean dose of clozapine, or length of clozapine treatment (Table 1). In the abnormal EEG group, the mean age and illness duration were significantly lower and shorter, respectively, than the corresponding values in the normal EEG group (Table 1). The time to the occurrence of EEG abnormalities varied from 4 to 52 weeks (mean 14.6 weeks). The clinical courses of the patients with EEG abnormality are summarized in Table 2. The numbers of patients with EEG abnormalities were as follows: spikes in one patient, spike and wave complexes in ten patients, and slow waves in four patients (Table 2). No patients withdrew from the study because of the appearance of EEG abnormalities.
  | Table 2 Clinical courses of patients with EEG abnormalities and seizure |
Clozapine-induced seizures
Six patients (23.1%) experienced seizures: one with both tonic–clonic and myoclonic, one with tonic–clonic, and four with myoclonic seizures (Table 2). The daily dose of clozapine at first seizure varied from 300–600 mg (mean 383.3 mg/day), and the time to first seizure varied from 8–23 weeks (mean 12.3 weeks). Five of six patients who experienced seizures in this study were successfully treated with valproate or lamotrigine without discontinuation of clozapine. The persistent seizures in one patient were ultimately controlled without the use of antiepileptic drugs. The clinical courses are summarized in Table 2.
Case 1 experienced a myoclonic seizure 23 weeks after starting clozapine, and the dosage when the seizure occurred was 600 mg. Lamotrigine 200 mg was begun because myoclonus was still observed 52 weeks after clozapine initiation, although the incidence was low. Tonic–clonic seizure was observed 130 weeks after clozapine initiation. The lamotrigine dose was increased to 300 mg, and clozapine was decreased to 550 mg. After that, neither seizures nor EEG abnormalities were observed. Case 5 experienced tonic–clonic seizure 8 weeks after starting clozapine, when the dosage was 300 mg. Valproate 400 mg was initiated and subsequently increased to 600 mg. Although the seizures stopped, the patient’s psychological symptoms exacerbated. Therefore, clozapine was increased to 400 mg. Partial seizure appeared 18 weeks after clozapine initiation despite treatment with valproate (600 mg). Increasing the valproate dosage to 800 mg effectively prevented further seizures without reduction of clozapine.
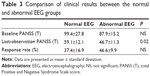
Comparison of PANSS (T) scores
PANSS (T) scores at baseline and at the last observation were compared between the normal and abnormal EEG groups. The mean baseline PANSS (T) scores were not significantly different between the two groups, but the mean score in the abnormal EEG group was significantly lower than that in the normal EEG group at the final follow-up (P=0.02). The response rate in the abnormal EEG group was higher than that in the normal EEG group, albeit not significantly (Table 3).
Discussion
Compared with other neuroleptics, clozapine appears to cause more seizures at therapeutic doses than the most epileptogenic of standard antipsychotic agents.4 The mechanism of clozapine-induced seizure is not well understood. Typical antipsychotic drugs primarily target striatonigral dopamine D2 receptors, whereas clozapine blocks mesolimbic and cortical dopamine D4 receptors.5 Mesolimbic structures are common sites of seizure onset. The selectivity of clozapine for mesolimbic dopamine receptors may explain its high epileptogenicity in comparison with other antipsychotic drugs.4 Further possible mechanisms include its effects on other receptor types, including gamma-aminobutyric acid A, nicotinic acetylcholine, glutamate N-methyl-D-aspartate, serotonin 5-HT2A, and strychnine-sensitive glycine.6–10 A dose-related risk of seizures with clozapine has been described in the literature, with reported risks of 0.6%–2% for doses <300 mg, 1.8%–4% for doses of 300–599 mg, and 5%–14% for patients taking 600–900 mg daily.11–13 Previously identified risk factors for clozapine-induced seizures include rapid upward titration, preexisting seizure, and concurrent use of other epileptogenic medications.14 Furthermore, clozapine-induced myoclonus can be a precursor to generalized seizure.15,16 In the present study, six patients (23.1%) experienced myoclonic or tonic–clonic seizure. Only tonic–clonic seizure was experienced by two patients (7.7%). One patient with tonic–clonic seizure had previously had myoclonic seizure. The mean dose of clozapine was 380.3 mg (300–600 mg) at seizure onset. The incidence of seizure in this study was higher than in other reports in the literature.11–13 These results may suggest that clozapine is more likely to cause seizures in the Japanese population. However, Kishi et al reported efficacy and tolerability of clozapine in Japanese patients with TRS and described the incidence of seizure in Japanese patients as 5.26%.17 Our study involved a small number of patients, so we cannot conclude that Japanese patients with schizophrenia have a higher risk of seizure with clozapine use; additional studies with larger samples are needed to verify our observation. White and Van Cott18 described the treatment of clozapine-associated seizures with dosage reduction and/or the addition of an antiepileptic drug. Praharaj et al19 reported that it was prudent to add anticonvulsants immediately after the first seizure. Although valproate is recommended as the standard therapy, other drugs such as lamotrigine, gabapentin, and clonazepam are also useful.15,16,19 Carbamazepine is contraindicated because of the increased risk of bone marrow suppression, and barbiturates may exacerbate sedation caused by clozapine.1 Antiepileptic drugs that are highly protein-bound may displace clozapine from serum proteins.4 However, why antiepileptic drugs are effective for clozapine-induced seizure without exacerbating psychological symptoms is unclear. All patients who experienced seizures in this study were successfully treated either with antiepileptic drugs or no drug with a small or no reduction of clozapine. Therefore, we believe that there is no need to discontinue clozapine in patients who experience seizures.
Studies have reported that EEG abnormalities associated with clozapine treatment range from 16%–74%.2,20 Among typical and atypical antipsychotics, clozapine was most strongly associated with EEG abnormalities (clozapine: 47.1%, olanzapine: 38.5%, risperidone: 28.0%, typical neuroleptics: 14.5%, quetiapine: 0.0%).21 We found that the incidence of clozapine-induced EEG abnormalities in Japanese subjects with schizophrenia was 38.5%. It has been reported that clozapine-induced EEG abnormalities occur in a dose-dependent manner and correlate with the serum level of clozapine.2,22–24 However, Centorrino et al21 did not find a relationship between dose and EEG abnormalities. Goyal et al25 reported EEG abnormalities in 61.9% of patients receiving clozapine at a dose of 100 mg or less. In this study, the mean dose of clozapine at the occurrence of EEG abnormalities varied from 125–600 mg (mean 305 mg/day) and was lower than that in the normal EEG group (mean 378.1 mg/day), albeit not significantly. In one-half of the patients with EEG abnormalities, the clozapine dose was <300 mg. Thus, the relationship between clozapine dosage and EEG abnormalities remains controversial. Haring et al24 described EEG abnormalities in 52% of patients and reported that these were dependent on plasma levels; they also determined that dose was not statistically related to EEG abnormalities. It is necessary to identify the relationship of EEG abnormalities and clozapine serum level. Centorrino et al21 determined that significant risk factors for EEG abnormalities were the use of various antipsychotic drugs, including clozapine; age over 40 years; and hypertension. On the other hand, Chung et al26 suggested that younger patients on the same clozapine dosage as older patients were more likely to have EEG abnormalities. In this study, patients in the abnormal EEG group were significantly younger than those in the normal EEG group. The abnormal EEG group also had a significantly shorter illness duration before clozapine treatment than the normal EEG group. These results indicate that EEG abnormalities may appear in patients who started clozapine treatment in the early phase of schizophrenia or when they were young.
Risby et al3 reported that EEG abnormalities that developed after clozapine treatment appeared to be associated with good clinical response. In this study, there was no significant difference in baseline PANSS (T) scores between the normal and abnormal EEG groups. However, the mean PANSS (T) score from the last observation was significantly lower in the abnormal EEG group, and the response rate of the abnormal EEG group was also higher, albeit not significantly, compared to that of the normal EEG group. These results indicate that EEG abnormalities that appear after clozapine treatment are associated with a good clinical response. Another study reported that pretreatment intrahemispheric asymmetry on EEG predicted the short-term response to clozapine in patients with schizophrenia.27 The change in theta frequency in quantitative EEG, and particularly changes in the midline electrodes over the frontocentral scalp area, might be a more sensitive indicator for evaluating clozapine treatment adequacy.28 Welch et al2 reported that the appearance of paroxysmal discharges with bursts of slow waves, polyspike bursts, and spike and sharp waves indicated a high risk for convulsions. Thus, the presence of EEG abnormalities is not necessarily indicative of a good response to clozapine. However, EEG results may be useful for adjusting clozapine dose if it is clarified which EEG results are related to good clinical responses or convulsions.
Conclusion
EEG abnormalities may appear in younger patients, and our findings indicate that there is no need to discontinue clozapine when seizures occur. EEG abnormalities that appeared after clozapine treatment were associated with a good clinical response.
Acknowledgments
We are grateful to all the participants in this study. We also thank Kazumi Shimizu for providing the symptom assessment.
Disclosure
This work was supported by Health and Labor Sciences Research Grant Number 3000000301. The authors report no other conflicts of interest in this work.
References
Karper LP, Salloway SP, Seibyl JP, Krystal JH. Prolonged postictal encephalopathy in two patients with clozapine-induced seizures. J Neuropsychiatry Clin Neurosci. 1992;4(4):454-457. | ||
Welch J, Manschreck T, Redmond D. Clozapine-induced seizures and EEG changes. J Neuropsychiatry Clin Neurosci. 1994;6(3):250-256. | ||
Risby ED, Epstein CM, Jewart RD, et al. Clozapine-induced EEG abnormalities and clinical response to clozapine. J Neuropsychiatry Clin Neurosci. 1995;7(4):466-470. | ||
Devinsky O, Pacia SV. Seizures during clozapine therapy. J Clin Psychiatry. 1994;55 Suppl B:153-156. | ||
Mansour A, Meador-Woodruff J, Burke S. Differential distribution of D2 and D4 dopamine receptor mRNAs in rat brain: an in situ hybridization study. Abstr Soc Neurosci. 1991;17:599. | ||
Arvanov VL, Wang RY. Clozapine, but not haloperidol, prevents the functional hyperactivity of N-methyl-D-aspartate receptors in rat cortical neurons induced by subchronic administration of phencyclidine. J Pharmacol Exp Ther. 1999;289(2):1000-1006. | ||
Liu Y, Hu C, Tang Y, et al. Clozapine inhibits strychnine-sensitive glycine receptors in rat hippocampal neurons. Brain Res. 2009;1278:27-33. | ||
Singhal SK, Zhang L, Morales M, Oz M. Antipsychotic clozapine inhibits the function of alpha7-nicotinic acetylcholine receptors. Neuropharmacology. 2007;52(2):387-394. | ||
Squires RF, Saederup E. Clozapine and several other antipsychotic/antidepressant drugs preferentially block the same ‘core’ fraction of GABA(A) receptors. Neurochem Res. 1998;23(10):1283-1290. | ||
Steward LJ, Kennedy MD, Morris BJ, Pratt JA. The atypical antipsychotic drug clozapine enhances chronic PCP-induced regulation of prefrontal cortex 5-HT2A receptors. Neuropharmacology. 2004;47(4):527-537. | ||
Ereshefsky L, Watanabe MD, Tran-Johnson TK. Clozapine: an atypical antipsychotic agent. Clin Pharm. 1989;8(10):691-709. | ||
Haller E, Binder RL. Clozapine and seizures. Am J Psychiatry. 1990;147(8):1069-1071. | ||
Lieberman JA, Kane JM, Johns CA. Clozapine: guidelines for clinical management. J Clin Psychiatry. 1989;50(9):329-338. | ||
Ravasia S, Dickson RA. Seizure on low-dose clozapine. Can J Psychiatry. 1998;43(4):420. | ||
Usiskin SI, Nicolson R, Lenane M, Rapoport JL. Gabapentin prophylaxis of clozapine-induced seizures. Am J Psychiatry. 2000;157(3):482-483. | ||
Wong J, Delva N. Clozapine-induced seizures: recognition and treatment. Can J Psychiatry. 2007;52(7):457-463. | ||
Kishi T, Fujita K, Furukawa O, et al. Efficacy and tolerability of clozapine in Japanese patients with treatment-resistant schizophrenia: results from a 12-week, flexible dose study using raters masked to antipsychotic choice. Asian J Psychiatr. 2013;6(3):200–207. | ||
White DM, Van Cott AC. Clozapine (Clozaril), seizures, and EEG abnormalities. Am J Electroneurodiagnostic Technol. 2007;47(3):190-197. | ||
Praharaj SK, Venkatesh BG, Sarkhel S, Zia-ul-Haq M, Sinha VK. Clozapine-induced myoclonus: a case study and brief review. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34(1):242-243. | ||
Naber D, Leppig M, Grohmann R, Hippius H. Efficacy and adverse effects of clozapine in the treatment of schizophrenia and tardive dyskinesia – a retrospective study of 387 patients. Psychopharmacology (Berl). 1989;99 Suppl:S73-S76. | ||
Centorrino F, Price BH, Tuttle M, et al. EEG abnormalities during treatment with typical and atypical antipsychotics. Am J Psychiatry. 2002;159(1):109-115. | ||
Freudenreich O, Weiner RD, McEvoy JP. Clozapine-induced electroencephalogram changes as a function of clozapine serum levels. Biol Psychiatry. 1997;42(2):132-137. | ||
Günther W, Baghai T, Naber D, Spatz R, Hippius H. EEG alterations and seizures during treatment with clozapine. A retrospective study of 283 patients. Pharmacopsychiatry. 1993;26(3):69-74. | ||
Haring C, Neudorfer C, Schwitzer J, et al. EEG alterations in patients treated with clozapine in relation to plasma levels. Psychopharmacology (Berl). 1994;114(1):97-100. | ||
Goyal N, Praharaj SK, Desarkar P, Nizamie H. Electroencephalographic abnormalities in clozapine-treated patients: a cross-sectional study. Psychiatry Investig. 2011;8(4):372-376. | ||
Chung SJ, Jeong SH, Ahn YM, et al. A retrospective study of clozapine and electroencephalographic abnormalities in schizophrenic patients. Prog Neuropsychopharmacol Biol Psychiatry. 2002;26(1):139–144. | ||
Gross A, Joutsiniemi SL, Rimon R, Appelberg B. Clozapine-induced QEEG changes correlate with clinical response in schizophrenic patients: a prospective, longitudinal study. Pharmacopsychiatry. 2004;37(3):119-122. | ||
Knott V, Labelle A, Jones B, Mahoney C. EEG hemispheric asymmetry as a predictor and correlate of short-term response to clozapine treatment in schizophrenia. Clin Electroencephalogr. 2000;31(3):145-152. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.