Back to Journals » International Journal of Nanomedicine » Volume 17
Clinical Trials of Liposomes in Children’s Anticancer Therapy: A Comprehensive Analysis of Trials Registered on ClinicalTrials.gov
Authors Feng Z, Gu Y, Yuan M, Xiao R , Fei Z
Received 23 January 2022
Accepted for publication 12 April 2022
Published 26 April 2022 Volume 2022:17 Pages 1843—1850
DOI https://doi.org/10.2147/IJN.S359666
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Anderson Oliveira Lobo
Zhaosong Feng,1 Yuyang Gu,2 Mengping Yuan,3 Renzhong Xiao,4 Zhenghua Fei2
1Pharmacy Department, Jianhu People’s Hospital, Jianhu, Jiangsu Province, 224700, People’s Republic of China; 2Department of Oncology, the First Affiliated Hospital of Wenzhou Medical University, Wenzhou, Zhejiang Province, 325000, People’s Republic of China; 3Department of Gastroenterology, the Second Affiliated Hospital of Wenzhou Medical University, Wenzhou, Zhejiang Province, 325000, People’s Republic of China; 4R&D Center, Hunan Royal Pharmaceutical Technology Co., Ltd., Changsha, Hunan Province, 410000, People’s Republic of China
Correspondence: Renzhong Xiao, R&D Center, Hunan Royal Pharmaceutical Technology Co., Ltd., Changsha City, Hunan Province, 410000, People’s Republic of China, Email [email protected] Zhenghua Fei, Department of Oncology, the First Affiliated Hospital of Wenzhou Medical University, Wenzhou, Zhejiang Province, 325000, People’s Republic of China, Email [email protected]
Objective: Clinical trials have become essential for driving the development of medicine. However, little is known about the current status of clinical trials on liposomes in children’s anticancer therapy (LCAT). This study aimed to synthesize current finding from clinical trials of LCAT in ClinicalTrials.gov.
Methods: A cross-sectional descriptive study of clinical trials on LCAT was conducted, using studies registered on ClinicalTrials.gov through December 30, 2021.
Results: A total of 74 eligible trials were identified, accounting for 4.8% (74/1552) of all trials on liposomes for cancer therapy. Among these trials, 70 (94.6%) were interventional trials, and the remaining 4 (5.4%) were observational trials. Of the 70 interventional trials, 63 (90.0%) were for treatment, 48.6% were involving unlabeled allocations, 30.0% were randomized, 52.9% were single group assignment, 71.4% were without masking, 28.6% were Phase 3 trials, 30.0% were Phase 1 trials, and 24.3% were Phase 2 trials. Furthermore, 17 liposomal drugs for 123 types of cancer were investigated in the interventional trials, and these were mainly focused on organic chemicals (43/70, 61.4%). Of these cancers, the highest proportion was leukemia (15.4%), followed by lymphoma (9.8%) and ovarian cancer (8.9%).
Conclusion: High quality, adequately powered, masked, appropriately sized, and randomized clinical trials represent the critical priorities for conducting a high-quality clinical trial. However, most of these trials for LCAT were non-randomized, single group assignment, and non-blinded interventional trials of small scale, with various eligibility criteria and outcome measures. Our analysis highlights the need for improvement in the completeness of study designs curated on clinicalTrials.gov. We urge for decision-makers to avoid adopting entrenched positions about the study design of cancer clinical trials to avoid this problem. As such, tackling the problematic challenges related to cancer and designing efficient trials for cancer requires developing and applying new approaches and multiple strategies.
Keywords: liposomes, liposomal drug, cancer, children anticancer therapy, clinical trials
Introduction
Recently nanoscale drugs become an area of intense novel drug research.1,2 Several nanocarriers, including liposomes, have been utilized for cancer therapies.3,4 Among these, liposomes have attracted the most attention because of their potency of side effects,5 prolonged the retention-time for encapsulated payloads in cancer cells,6 effectively resolving some of the problems of off-target effects of anticancer drugs by improving the pharmacokinetic profiles and pharmacological properties of several agents.7,8
Clinical trials are the most effective strategy for evaluating the efficacy of a drug on a specific disease9,10 and are a critical step in the successful development of more effective drugs.11 Thus, exploring clinical trials, especially analyzing registered clinical trials, has become an important facet of research to help future clinical practice. ClinicalTrials.gov is a public trial registry provided by the US National Library of Medicine and the US Food and Drug Administration. Zarin et al12 postulated that the number of clinical trials in ClinicalTrials.gov accounted for more than 80% of all studies in the World Health Organization’s International Clinical Trials Registry Platform. This proportion will likely expand with further implementation of the Food and Drug Administration Amendments Act (FDAAA 801), which expands the scope of mandatory clinical trial registration.13 Moreover, a joint statement from all International Committee of Medical Journal Editors (ICMJE) member journals indicated that clinical trials must be publicly registered in trials registries before they are considered for publication. Therefore, to better evaluate the breadth of liposome treatments for pediatric cancers, we performed a cross-sectional study to investigate the characteristic of registered trials in ClinicalTrials.gov regarding liposomes in children’s anticancer therapy.
Materials and Methods
A cross-sectional, descriptive study of clinical trials for LCAT registered on the ClinicalTrials.gov database was conducted. The trials were obtained from ClinicalTrials.gov using the advanced search function with the search term “cancer” for “condition or disease” and the term “liposome” for “Other terms” on December 30, 2021. All of the identified clinical trials were assessed to obtain records of all studies. Intervention and observation studies were all included. We used the age field as a filter, and we included trials explicitly designed for the child (birth – 17 years of age). Next, we manually reviewed all of the trials and selected those using liposomal drugs for children’s anticancer therapy. Trials utilizing non-liposomal drugs were excluded. The following information and data were extracted: registered number, title, study type, conditions, interventions, locations, start date, the status of the trial, study results, study samples, participant ages, primary sponsor, location, primary purpose, phases of each trial, allocation, intervention model, masking and intervention. All trials were then further subclassified according to their study type. We used descriptive statistics to characterize trial categories. Frequencies and percentages were provided for categorical data. All analyses were performed using Microsoft Excel (Microsoft Office Excel 2010, Microsoft Corporation).
Results
Screening and Included Trials
The initial search identified 1552 clinical trials on liposomes in cancer therapy registered on the ClinicalTrials.gov database through December 30, 2021. After using the age field (child; birth – 17 years of age) as a filter, 352 trials focusing on liposomes in children’s anticancer therapy were included. After carefully reviewing all the information, 278 trials were not liposomal drugs and were excluded. Thus, a total of 74 registered trials focusing on liposomes in children’s anticancer therapy were subsequently included, including four observational studies and 70 intervention trials (Figure 1).
 |
Figure 1 Flowchart of trial selection. |
Basic Characteristics of Included Trials
The basic characteristics of the included trials are shown in Table 1. Among the 74 eligible trials, 70 (94.6%) were interventional trials, and the 4 (5.4%) were observational trials. Half of these trials were initiated prior to 2007. Every five years, the number of initiated trials changed a little from 2007 to 2021. Most of the included trials (47.3%) have been completed, although only 23.0% of trials had available results in this database. The sources of funding were indicated for 40.5% of trials. The National Institutes of Health (NIH) was the second-largest contributor, accounting for 36.5% of included trials. North America was the most frequently identified study location (68.9%), followed by Europe (14.9%), Asia (12.2%), and other (4.1%).
 |
Table 1 Characteristics of All Included Trials |
Characteristics of Study Design
Of the four observational trials, two were retrospective, and two trials were prospective. Of the 70 interventional trials, 63 (90.0%) were for treatment, 3 (4.3%) were for supportive care, 2 (2.9%) were for diagnostic, and 2 (2.9%) were for prevention. The allocation concealment was not clear in 48.6% of these studies. 21 (30.0%) trials were randomized, and 15 (21.4%) trials were non-randomized. More than half of the intervention models were single group assignments (52.9%), followed by parallel assignments (22.9%), and unknown (21.4%). Among the 70 interventional trials, the majority of trials (50, 71.4%) were without masking, 13 (18.6%) were with unknown masking, and 7 (10.0%) were with masking (1 single masking, 4 double maskings, and 2 quadruple maskings). 20 (28.6%) were phase 3 trials, 21 (30.0%) were phase 1 trials, and 17 (24.3%) were phase 2 trials. More than half of the trials recruited less than 50 participants, 12 trials (17.1%) recruited 100–500 individuals, and 12 trials (17.1%) did not indicate the number of participants. The study design characteristics of interventional trials are displayed in Table 2.
 |
Table 2 Study Design Elements of Interventional Trials (n = 70) |
Overview of Investigated Drugs
A total of 70 interventional trials investigated 17 liposomal drugs, mainly focused on organic chemicals (43/70, 61.4%). 32 trials (45.7%) investigated liposomal doxorubicin. Of these trials for liposomal drugs, the highest proportion was testing liposomal doxorubicin (45.7%), followed by liposomal vincristine (17.1%) and liposomal cytarabine (5.7%). Three trials investigated liposomal complex compounds, of which two trials were liposomal daunorubicin-cytarabine, and one trial was liposomal doxorubicin-daunorubicin. A summary of studied liposomal drugs for prevention is provided in Table 3.
 |
Table 3 Overview of Drugs for Prevention |
Overview of Cancer Type for Prevention
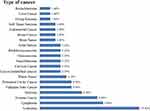
A total of 70 interventional trials investigated 17 liposomal drugs for 123 types of cancer. Of these cancers, the highest proportion was leukemia (15.4%), followed by lymphoma (9.8%) and ovarian cancer (8.9%). Detailed data is shown in Figure 2.
Discussion
Liposomes have been extensively investigated for overcoming cancer drug resistance,14 cancer-targeted therapy,15 and as a sustained and controlled release drug delivery system.16 However, liposomes do have limited clinical utility due to properties such as uncontrollable drug release, instability in storage, and insufficient drug loading.17 Specifically, due to their small aqueous internal volumes, liposomes have a relatively low encapsulation efficacy for water-soluble drugs.18 Meanwhile, large-scale liposomes production with low batch-to-batch differences is a challenge for the industry, which ultimately delays the clinical translation of new products.19 In addition, recruitment of children is a persistent challenge for researchers seeking to include these populations in clinical trials.20 First, societal concerns and parental emotional involvement can act to delay or prevent certain types of paediatric research.20,21 Second, medical ethics and clinical trial design for children need further refinement.22 Thus, the number of trials of liposomes in children’s anticancer therapy has not increased significantly over time and clinical trials focusing on liposomes account for only about 4.77% (74/1552) of clinical trials on liposomes in cancer therapy. Liposomally-delivered drugs have predominantly been organic chemicals (43/70, 61.4%). For example, 32 trials (45.7%) investigated liposomal doxorubicin. These results were following previous literature reports on the efficacy of delivering doxorubicin this way. To enhance the solubility of a hydrophobic substance, lipid-based drug delivery systems, especially liposomes, are among the best candidates.23–25
In this study, the highest proportion of cancer type for prevention in a children was leukemia (15.4%), and the highest proportion of liposomal drug was in liposomal doxorubicin (45.7%), followed by liposomal vincristine (17.1%) and liposomal cytarabine (5.7%). For decades, the standard of care for treating acute myeloid leukemia (AML) has been the combination of a nucleoside analog with an anthracycline.26,27 Vincristine and cytarabine are nucleoside, and doxorubicin is a type of anthracycline. This indicated that liposomal doxorubicin combined with vincristine or cytarabine for childhood leukemia is an important future direction for liposomes in children’s anticancer therapy.
High quality, adequately powered, masked, appropriately sized, and appropriately sized, and randomized clinical trials represent a critical priority for high-quality clinical trials.28–30 However, only 30.0% of trials studied here were randomized, and the majority of trials (71.4%) were without masking. Previously, it has been suggested that efficient trial designs are essential for rare malignancies has randomized trials are less feasible.31 To address this, there are multiple strategies for, such using as a Bayesian posterior predictive approach,32 or using complex innovative design,33 a novel multi-arm, multi-stage (MAMS) design.34 Hearn et al35 discussed in depth this issue highlighting the need for decision-makers to avoid adopting entrenched positions about the nature of the trial design.
Disclosure
The authors declare there are no conflicts of interest regarding the publication of this paper.
References
1. Jiang X, Zheng Y-W, Bao S, et al. Drug discovery and formulation development for acute pancreatitis. Drug Deliv. 2020;27(1):1562–1580. doi:10.1080/10717544.2020.1840665
2. Guo S, Liang Y, Liu L, et al. Research on the fate of polymeric nanoparticles in the process of the intestinal absorption based on model nanoparticles with various characteristics: size, surface charge and pro-hydrophobics. J Nanobiotechnol. 2021;19(1):32. doi:10.1186/s12951-021-00770-2
3. Qi -S-S, Sun J-H, Yu H-H, Yu S-Q. Co-delivery nanoparticles of anti-cancer drugs for improving chemotherapy efficacy. Drug Deliv. 2017;24(1):1909–1926. doi:10.1080/10717544.2017.1410256
4. Kim K, Khang D. Past, present, and future of anticancer nanomedicine. Int J Nanomedicine. 2020;15:5719–5743. doi:10.2147/IJN.S254774
5. Fenske DB, Cullis PR. Liposomal nanomedicines. Expert Opin Drug Deliv. 2008;5(1):25–44. doi:10.1517/17425247.5.1.25
6. Suntres ZE. Liposomal antioxidants for protection against oxidant-induced damage. J Toxicol. 2011;2011:152474. doi:10.1155/2011/152474
7. Landi-Librandi AP, Chrysostomo TN, Caleiro Seixas Azzolini AE, Marzocchi-Machado CM, de Oliveira CA, Lucisano-Valim YM. Study of quercetin-loaded liposomes as potential drug carriers: in vitro evaluation of human complement activation. J Liposome Res. 2012;22(2):89–99. doi:10.3109/08982104.2011.615321
8. Mignet N, Seguin J, Chabot GG. Bioavailability of polyphenol liposomes: a challenge ahead. Pharmaceutics. 2013;5(3):457–471. doi:10.3390/pharmaceutics5030457
9. Feizabadi M, Fahimnia F, Mosavi Jarrahi A, Naghshineh N, Tofighi S. Iranian clinical trials: an analysis of registered trials in International Clinical Trial Registry Platform (ICTRP). J Evid Based Med. 2017;10(2):91–96. doi:10.1111/jebm.12248
10. Chen L, Su Y, Quan L, Zhang Y, Du L. Clinical trials focusing on drug control and prevention of ventilator-associated pneumonia: a comprehensive analysis of trials registered on ClinicalTrials.gov. Original research. Front Pharmacol. 2019;9. doi:10.3389/fphar.2018.01574
11. Jacobsen PB, Wells KJ, Meade CD, et al. Effects of a brief multimedia psychoeducational intervention on the attitudes and interest of patients with cancer regarding clinical trial participation: a multicenter randomized controlled trial. J Clin Oncol. 2012;30(20):2516–2521. doi:10.1200/JCO.2011.39.5186
12. Zarin DA, Ide NC, Tse T, Harlan WR, West JC, Lindberg DAB. Issues in the registration of clinical trials. JAMA. 2007;297(19):2112–2120. doi:10.1001/jama.297.19.2112
13. Tse T, Williams RJ, Zarin DA. Reporting “basic results” in ClinicalTrials.gov. Chest. 2009;136(1):295–303. doi:10.1378/chest.08-3022
14. Bai F, Yin Y, Chen T, et al. Development of liposomal pemetrexed for enhanced therapy against multidrug resistance mediated by ABCC5 in breast cancer. Int J Nanomedicine. 2018;13:1327–1339. doi:10.2147/IJN.S150237
15. Riaz MK, Riaz MA, Zhang X, et al. Surface functionalization and targeting strategies of liposomes in solid tumor therapy: a review. Int J Mol Sci. 2018;19(1):195. doi:10.3390/ijms19010195
16. Yue P-J, He L, Qiu SW, et al. OX26/CTX-conjugated PEGylated liposome as a dual-targeting gene delivery system for brain glioma. Mol Cancer. 2014;13:191. doi:10.1186/1476-4598-13-191
17. Wicki A, Witzigmann D, Balasubramanian V, Huwyler J. Nanomedicine in cancer therapy: challenges, opportunities, and clinical applications. J Control Release. 2015;200:138–157. doi:10.1016/j.jconrel.2014.12.030
18. Akbarzadeh A, Rezaei-Sadabady R, Davaran S, et al. Liposome: classification, preparation, and applications. Nanoscale Res Lett. 2013;8(1):102. doi:10.1186/1556-276x-8-102
19. Al-Amin MD, Bellato F, Mastrotto F, et al. Dexamethasone loaded liposomes by thin-film hydration and microfluidic procedures: formulation challenges. Int J Mol Sci. 2020;21(5):1611. doi:10.3390/ijms21051611
20. Cunningham-Erves J, Deakings J, Mayo-Gamble T, Kelly-Taylor K, Miller ST. Factors influencing parental trust in medical researchers for child and adolescent patients’ clinical trial participation. Psychol Health Med. 2019;24(6):691–702. doi:10.1080/13548506.2019.1566623
21. Rentea RM, Oyetunji TA, Peter SDS. Ethics of randomized trials in pediatric surgery. Pediatr Surg Int. 2020;36(8):865–867. doi:10.1007/s00383-020-04665-5
22. Nicholl A, Evelegh K, Deering KE, et al. Using a Respectful Approach to Child-centred Healthcare (ReACH) in a paediatric clinical trial: a feasibility study. PLoS One. 2020;15(11):e0241764. doi:10.1371/journal.pone.0241764
23. Nik ME, Malaekeh-Nikouei B, Amin M, et al. Liposomal formulation of Galbanic acid improved therapeutic efficacy of pegylated liposomal Doxorubicin in mouse colon carcinoma. Sci Rep. 2019;9(1):9527. doi:10.1038/s41598-019-45974-7
24. Laverman P, Boerman OC, Storm G, Oyen WJG. (99m)Tc-labelled Stealth liposomal doxorubicin (Caelyx) in glioblastomas and metastatic brain tumours. Br J Cancer. 2002;86(4):659–661. doi:10.1038/sj.bjc.6600093
25. Wang G, Wang J, Wu W, Tony To SS, Zhao H, Wang J. Advances in lipid-based drug delivery: enhancing efficiency for hydrophobic drugs. Expert Opin Drug Deliv. 2015;12(9):1475–1499. doi:10.1517/17425247.2015.1021681
26. Chen EC, Fathi AT, Brunner AM. Reformulating acute myeloid leukemia: liposomal cytarabine and daunorubicin (CPX-351) as an emerging therapy for secondary AML. Onco Targets Ther. 2018;11:3425–3434. doi:10.2147/OTT.S141212
27. Preisler HD, Anderson K, Rai K, et al. The frequency of long-term remission in patients with acute myelogenous leukaemia treated with conventional maintenance chemotherapy: a study of 760 patients with a minimal follow-up time of 6 years. Br J Haematol. 1989;71(2):189–194. doi:10.1111/j.1365-2141.1989.tb04253.x
28. Zwierzyna M, Davies M, Hingorani AD, Hunter J. Clinical trial design and dissemination: comprehensive analysis of ClinicalTrials.gov and PubMed data since 2005. BMJ. 2018;361:k2130. doi:10.1136/bmj.k2130
29. Zhang C, Kwong JSW, Yuan R-X, et al. Effectiveness and tolerability of different recommended doses of PPIs and H(2)RAs in GERD: network meta-analysis and GRADE system. Sci Rep. 2017;7:41021. doi:10.1038/srep41021
30. Oh ES, Fong TG, Hshieh TT, Inouye SK. Delirium in older persons: advances in diagnosis and treatment. JAMA. 2017;318(12):1161–1174. doi:10.1001/jama.2017.12067
31. Italiano A, Nanda S, Briggs A, et al. Larotrectinib versus prior therapies in tropomyosin receptor kinase fusion cancer: an intra-patient comparative analysis. Cancers. 2020;12(11):3246. doi:10.3390/cancers12113246
32. Dutton P, Love S, Faleti A, Hassan B. The use of Bayesian design in two trials in rare cancers. Trials. 2015;16(Suppl 2):P213. doi:10.1186/1745-6215-16-S2-P213
33. Blagden SP, Billingham L, Brown LC, et al. Effective delivery of Complex Innovative Design (CID) cancer trials-A consensus statement. Br J Cancer. 2020;122(4):473–482. doi:10.1038/s41416-019-0653-9
34. Sydes MR, Parmar MKB, Mason MD, et al. Flexible trial design in practice - stopping arms for lack-of-benefit and adding research arms mid-trial in STAMPEDE: a multi-arm multi-stage randomized controlled trial. Trials. 2012;13:168. doi:10.1186/1745-6215-13-168
35. Hearn J, Keat N, Law K, Sharpe R. How cancer research UK is adapting to adaptive designs. Trials. 2011;12(Suppl 1):A6. doi:10.1186/1745-6215-12-S1-A6
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.