Back to Journals » Neuropsychiatric Disease and Treatment » Volume 11
Clinical preference for factors in treatment of geriatric depression
Authors Riepe M
Received 6 October 2014
Accepted for publication 20 November 2014
Published 22 December 2014 Volume 2015:11 Pages 25—31
DOI https://doi.org/10.2147/NDT.S75450
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Roger Pinder
Matthias W Riepe
Mental Health and Geriatric Psychiatry, Psychiatry II, Ulm University, Ulm, Germany
Abstract: Little is known about symptom preferences of clinical psychiatrists in the treatment of geriatric depression and preferences for avoiding adverse drug effects. Participants (board-certified psychiatrists) were recruited prior to a lecture on geriatric depression during a continuing education program. An analytic hierarchy process was performed and participants were asked for pairwise comparison of criteria guiding them in appraising therapeutic efficacy, and in avoiding toxicity and adverse events. Of the 61 participants from the continuing education program, 42 (69%) returned their data sheet. Avoidance of cardiotoxicity was regarded as more important than avoidance of hepatotoxicity or hematotoxicity. Concerning adverse events, highest preference was given to avoidance of falls and drug interactions, followed by avoidance of sedation, weight change, and impairment of sexual function. The most important preferences for appraisal of therapeutic efficacy were suicidality over ability to concentrate and sleep. Clinical psychiatrists have a hierarchy of preferences for treatment goals and avoidance of adverse events and toxicity. This raises the question for future research whether these preferences cause differences in prescription patterns in clinical practice even though a multitude of antidepressants are similarly effective when judged with instruments used in clinical trials.
Keywords: depressive disorder, symptoms, analytic hierarchy process, toxicity, adverse events, symptoms
Introduction
Depression is a disorder of the representation and regulation of mood and emotion.1 Clinically, as well as for clinical trials and research, the diagnostic process applies checklists as compiled for the International Classification of Diseases (ICD) or the Diagnostic and Statistical Manual of Mental Disorders (DSM). Interpretation on how to use these guidelines, however, has been subject to interpretation and change.2 Overall, inter-rater reliability in diagnosing depressive disorder remains low.3
Diagnosis of depressive disorder according to the fourth and fifth editions of the DSM (DSM-IV and DSM-V) requires the presence of five of the following nine symptoms: significant weight loss or weight gain; insomnia or hypersomnia; psychomotor agitation or retardation; fatigue or loss of energy; feelings of worthlessness or excessive or inappropriate guilt; diminished ability to think or concentrate or indecisiveness; recurrent thoughts of death or suicidal ideation, or suicide attempt or specific plan, including mandatorily either depressed mood or pervasive loss of interest or pleasure. The importance of these symptoms is ranked as equal in the diagnostic checklists. However, different degrees of association of clinical diagnosis of depressive disorder with specific items have been reported.4 Appraisal of change of severity of depressive disorder on treatment is guided by the same criteria used for the diagnosis.5 It is still under discussion in the literature whether late-life depression is characterized by a distinct pattern of symptoms compared to depression in young and middle-aged persons.6–8 In clinical practice, however, symptoms for diagnosis of depressive disorder are the same in adult and geriatric depression. Moreover, there is increasing awareness of the need to differentiate depressive disorder according to the clinical symptomatology and to choose antidepressive treatment accordingly.9 However, clear-cut criteria and guidelines are missing.
Multicriteria decision analysis is used to characterize and understand decision processes. These techniques have been applied to several health care issues to determine preferences for diagnosis and treatment. However, the topics addressed were mostly related to cancer care.10 One approach to establish a hierarchy of preferences in situations where several criteria contribute to an overall judgment is to perform an analytic hierarchy process (AHP). This method has been developed and brought into practice ever since the work of Saaty some 30 years ago.11 At the very heart of this method are comparison matrices resulting from pairwise comparisons of alternatives. With n alternatives, (n2 minus n)/2 choices have to be performed. For practical reasons, this limits the number of choices that can be targeted in a single study. It has been shown previously that preselection of alternatives may influence the result of the AHP.12 Two recent studies in small groups of patients and professionals reported use of the AHP method to appraise preferences of patients and professionals for treatment goals of depressive disorder.13,14 However, the criteria chosen in these studies comprised general criteria such as response to drug treatment and no relapse.13,14 It was the goal of the present study to gain a more detailed insight into what practicing psychiatrists aim at. To address symptom-oriented treatment goals in greater detail, we used symptoms from the ICD and DSM criteria for diagnosis of depression. Mandatory symptoms of depressed mood and pervasive loss of interest or pleasure were not included in the list of symptoms to be compared in the present study, as without these diagnosis of depressive disorder is at least uncertain if not impossible. Instead, the nonmandatory symptoms were used, namely ability to concentrate, feelings of worthlessness or guilt, psychomotor symptoms, sleep disturbance, suicidality, and weight.
Beyond therapeutic efficacy, treatment of elderly persons with depressive symptoms requires careful attention to issues of toxicity and side effects. Multidecision criteria analyses have been performed regarding patient preferences concerning adverse events.15,16 These studies, however, did not unfold side effects or toxicity in greater detail, but rather asked for preferences concerning overall treatment efficacy and overall adverse events.
It was the goal of the present study to analyze preferences of clinical psychiatrists judging on therapeutic efficacy and adverse events and toxicity in the treatment of geriatric depression.
Methods
The study was performed according to institutional guidelines and the principles outlined in the Declaration of Helsinki.
Participants
In the context of continuing medical education certified by the state board of physicians of the state of Saxonia in Germany, 61 board-certified psychiatrists from all over Germany participated in a symposium organized by Servier GmbH. Prior to a lecture on geriatric depression delivered by the author, a survey with alternative choices concerning symptoms and adverse events was distributed. Participants were asked to choose which symptoms they regarded as most important when appraising therapeutic efficacy and which adverse events they tried to avoid during treatment using an analytic hierarchy process.
AHP criteria and analysis
Analytic hierarchy process is a multiple criteria decision-making method that was developed some 30 years ago.11 It is used in multiple settings to determine preferences among a set of alternative choices. The method rests on preference ratings using pairwise comparisons. For this study, it was the goal to study preferences for symptoms to appraise therapeutic efficacy on antidepressive treatment and for avoiding certain types of toxicity and adverse events (Figure 1).
  | Figure 1 Prioritization of goals in the treatment of elderly patients with depressive disorder. |
Answers were to be given on a five-step scale of preferences, with higher numerical values indicating higher relevance of the item (see sample items in Figure 2). The questionnaire on toxicity comprised three items (cardiotoxicity, hepatotoxicity, and hematotoxicity). AHP yields three pairwise comparisons to be made (cardiotoxicity vs hepatotoxicity, cardiotoxicity vs hematotoxicity, and hepatotoxicity vs hematotoxicity). The questionnaires on adverse events and therapeutic targets comprised five (drug interactions, sedation, falls, weight change, and sexual dysfunction) and six (ability to concentrate, feeling worthless, suicidality, psychomotor symptoms, sleep, and weight) items, thus requiring 10 and 15 pairwise comparisons, respectively. For methodological reasons, the number of inconsistent respondents increases with the number of choices to be made (Figure 2).
  | Figure 2 Sample items for determining the preferences. |
For each participant, the individual judgments were used to calculate the comparison matrices in a spreadsheet file. Preference weights as well as their consistency ratio were calculated using the formulas provided by Saaty.11 With this method, all pairwise choices are integrated to calculate the overall preference. For the present investigation, the comparisons had to be done on a five-step scale from 1 (equal importance of the alternatives) to 6 (extreme preference for one of the alternatives) rather than on an eight-step scale from 1 (equal importance) to 9 (extreme preference for one of the alternatives). While Saaty’s eight-step scale is used most frequently, scales with other numbers of steps may be used depending on the context.17,18 The reason why a five-step scale was chosen in the present study was that this scale resembles more what is used in psychometric and medical contexts.
Responses from participants with a consistency ratio >0.1 were excluded from the final analysis. To evaluate overall group differences, a one-way analysis of variance (ANOVA) was calculated with post hoc Bonferroni testing for difference between alternatives (SPSS version 17.0, SPSS, Chicago, IL, USA).
Results
Forty-two participants responded. The average time after board certification of these participants was 9.7±6.5 years (mean ± standard deviation). The prioritization of treatment issues was performed on grounds of analyzing avoidance of toxicity, avoidance of adverse events, and targeting treatment appraisal.
Toxicity
Three participants had to be excluded for reasons of an inconsistency ratio >0.1. For the remaining 39 participants, a one-way ANOVA was calculated for group effect showing highly significant group difference (F2,114=74.41, P<0.001). Pairwise comparisons between cardiotoxicity and both hepatotoxicity and hematotoxicity were highly significant (P<0.001). No difference was observed between preference for hepatotoxicity and hematotoxicity (Figure 3).
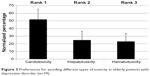  | Figure 3 Preferences for avoiding different types of toxicity in elderly patients with depressive disorder (n=39). |
Adverse events
Three participants had to be excluded for reasons of inconsistency ratio >0.1. For the remaining 39 participants, a one-way ANOVA was calculated showing a highly significant group difference (F4,190=81,154, P<0.001). All pairwise comparisons were highly significant (P<0.001) except drug interactions and falls, which were equally important (Figure 4).
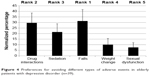  | Figure 4 Preferences for avoiding different types of adverse events in elderly patients with depressive disorder (n=39). |
Symptoms
Ten of the 42 participants had a consistency ratio >0.1. For the remaining 32 participants, a one-way ANOVA was calculated for group effect showing a highly significant group difference (F5,186=95,656, P<0.001). Suicidality was rated with the highest preference compared to all other symptoms (P<0.001). Ability to concentrate, feelings of worthlessness/guilt, psychomotor changes, and weight were of next highest preference, rated less important than suicidality (P<0.001) but more important than sleep.
In a separate analysis, the preferences of those that were excluded from the final analysis were averaged and compared with those fulfilling Saaty’s consistency criterion. In none of the domains were any statistical significant differences observed between the whole group and the group excluded for reasons of inconsistency (Figure 5).
Discussion
The present study examined three different aspects determining therapeutic decisions in elderly subjects with depressive disorder; ie, avoidance of toxicity, avoidance of adverse events, and targeting specific symptoms. It is a common belief that psychiatrists use sophisticated forms of clinical judgment that are suitable for clinical challenges but are not addressed by current research strategies.9 The current study aimed at analyzing these somewhat hidden preferences of psychiatrists for the avoidance of toxicity and adverse events and targeting symptoms with an established method of analyzing preferences in a situation where multiple criteria contribute to the overall assessment.
Compared to other reports targeting the analysis of the relative importance of different symptoms for diagnosis and severity assessment of depressive disorder by means of an AHP, the group of professionals is much larger in the present study.13,14 While the study sample in the present study is small compared to the number of practicing psychiatrists and thus may be influenced by several confounders (eg, the setting in which they practice), the number is much larger than in the previous studies using AHP in health professionals.13,14 The present study used established endpoints of toxicity and adverse events. The symptoms used to determine the preferences for treatment goals are those symptoms used to characterize depressive disorder in the diagnostic classification system of the DSM and ICD. Thus, on grounds of these results, some light can be shed on the ranking of symptoms in clinical practice. Using established symptoms of depressive disorder, the present study avoids arbitrary labeling and choice of symptoms used in prior studies.13,14 Moreover, it determines preferences concerning toxicity, side effects, and symptoms in separate questionnaires, thus avoiding the mingling of target symptoms and side effects in prior studies.13,14
In the literature, toxic events on treatment with antidepressants refer to cardiac toxicity as a fairly frequent event and hepatotoxicity and hematotoxicity as rare but serious events.19–23 In the present study, avoidance of cardiotoxicity was rated more important than avoidance of both hepatotoxicity and hematotoxicity. Most likely, this results from the impression that cardiotoxicity may be associated with an immediate threat of death. Possibly, warnings concerning some antidepressants of the SSRI-type in recent years contributed to this assessment also.24 Cardiotoxicity is the most frequent form of toxicity during treatment with antidepressants.19 Practicing physicians thus may be more aware of cardiotoxicity compared to the serious but rare events of hepatotoxicity or hematotoxicity.
Overall tolerability is an important factor in the selection of antidepressive treatments and patient compliance, even though no clear-cut guidelines exist.25,26 In the present study, drug interactions and falls were considered to be the most important side effects to avoid. Even though sedation is known to be a risk factor for falls, avoidance of sedation is ranked as less important than avoidance of falls and drug interactions. Possibly this results from sedation being a therapeutic goal sometimes; eg, in depressed patients with suicidality where some extent of sedation is a therapeutic goal as long as it can be achieved without increasing the risk of falls. Similarly, weight change in some situations with reduced weight and appetite is a therapeutic goal, while in other situations on long-term treatment it is clearly an adverse event increasing the risk of metabolic syndrome. Overall, the results reflect clinical common sense, with highest preference for avoiding potentially health-threatening effects (eg, drug interactions) or immediate health risks (eg, falls).
The symptom given the highest weight by practicing psychiatrists was suicidality, in good accordance with the judgments on avoidance of life-threatening adverse effects or toxicity. Nevertheless, this is somewhat surprising, since it was reported that suicidality is less central to the diagnosis of depression than vegetative symptoms.27 However, the present study asked for symptom preferences concerning depressive disorder in elderly patients. This group of patients has a particularly high rate of suicide, so that the preference from the group of psychiatrists in this study is in good harmony with the actual risk of the target group of patients.28 The present study demonstrates that vegetative symptoms (ie, weight and sleep) are weighted with different preference. Sleep is considered to be more important than weight. Thus, it can be questioned whether it is useful to combine symptoms of sleep and symptoms of weight change into one area labeled as “vegetative” in scales for the assessment of severity of major depression as in the Montgomery–åsberg Depression Scale or the Hamilton Depression Rating Scale.29,30 Similar to the preference of psychiatrists in the present study, it was reported recently that targeting sleep problems is one of the most important symptoms for older male patients with depressive disorder.15 Future studies will need to address whether this holds in different settings (eg, hospital vs. outpatients) and patient or physician contexts. It is one of the limitations of the present study that several factors of the respondents are unknown (eg, setting, years of practice, and sex).
Inability to concentrate is just one out of many symptoms in the diagnostic checklists of the DSM and ICD. However, together with weight and feeling worthless, it belongs to the group of symptoms considered second most important after suicidality. Clinical practice thus seems to already have recognized that cognition is an important aspect of depressive disorder, even though this only recently has begun to be addressed in greater detail in academic research.31 Considering the impact of impaired ability to concentrate on everyday function, the current study supports to look out for these and other cognitive symptoms more specifically in future.
Even though some studies suggest the importance of sexual dysfunction for the elderly more so than for younger patients, impairment thereof as an important side effect in treatment of depressed elderly seems to be neglected in everyday practice.32 Probably this reflects that elderly patients rarely talk about sexual issues, and therefore it not a frequent topic discussed between physician and patient.
The results of the present study raise the question for future research whether the preferences of clinical psychiatrists for specific symptoms cause differences in prescription patterns although a multitude of antidepressants are similarly effective when judged with instruments used in clinical trials. Future studies will also need to address the preferences of psychiatrists in appraising therapeutic efficacy, cross-culturally.
Acknowledgment
The author serves on advisory and speakers’ boards of drug companies developing and selling antidepressants (Lundbeck GmbH, Servier).
Disclosure
The author reports no conflicts of interest in this work.
References
Davidson RJ, Pizzagalli D, Nitschke JB, Putnam K. Depression: perspectives from affective neuroscience. Annu Rev Psychol. 2002;53:545–574. | ||
Maj M. “Clinical judgment” and the DSM-5 diagnosis of major depression. World Psychiatry. 2013;12(2):89–91. | ||
Regier DA, Narrow WE, Clarke DE, et al. DSM-5 field trials in the United States and Canada, Part II: test-retest reliability of selected categorical diagnoses. Am J Psychiatry. 2013;170(1):59–70. | ||
Zimmerman M, McGlinchey JB, Young D, Chelminski I. Diagnosing major depressive disorder I: A psychometric evaluation of the DSM-IV symptom criteria. J Ner Ment Dis. 2006;194(3):158–163. | ||
Fava M. Assessing response to treatment and recognizing residual depressive symptoms. J Clin Psychiatry. 2014;75(1):e01. | ||
Grayson L, Thomas A. A systematic review comparing clinical features in early age at onset and late age at onset late-life depression. J Affect Disord. 2013;150(2):161–170. | ||
Heun R, Kockler M, Papassotiropoulos A. Distinction of early- and late-onset depression in the elderly by their lifetime symptomatology. Int J Geriatr Psychiatry. 2000;15(12):1138–1142. | ||
Korten NC, Comijs HC, Lamers F, Penninx BW. Early and late onset depression in young and middle aged adults: differential symptomatology, characteristics and risk factors? J Affect Disord. 2012;138(3):259–267. | ||
Tomba E, Fava GA. Treatment selection in depression: the role of clinical judgment. Psychiatr Clin North Am. 2012;35(1):87–98. | ||
Adunlin G, Diaby V, Montero AJ, Xiao H. Multicriteria decision analysis in oncology. Health Expect. 2014. | ||
Saaty TL. The analytic hierarchy process: planning, priority setting, resource allocation. New York: McGraw-Hill; 1980. | ||
Ijzerman MJ, van Til JA, Bridges JF. A comparison of analytic hierarchy process and conjoint analysis methods in assessing treatment alternatives for stroke rehabilitation. Patient. 2012;5(1):45–56. | ||
Hummel MJ, Volz F, van Manen JG, et al. Using the analytic hierarchy process to elicit patient preferences: prioritizing multiple outcome measures of antidepressant drug treatment. Patient. 2012;5(4):225–237. | ||
Danner M, Hummel JM, Volz F, et al. Integrating patients’ views into health technology assessment: Analytic hierarchy process (AHP) as a method to elicit patient preferences. Int J Technol Assess Health Care. 2011;27(4):369–375. | ||
Dwight Johnson M, Apesoa-Varano C, Hay J, Unutzer J, Hinton L. Depression treatment preferences of older white and Mexican origin men. Gen Hosp Psychiatry. 2013;35(1):59–65. | ||
Zimmermann TM, Clouth J, Elosge M, et al. Patient preferences for outcomes of depression treatment in Germany: a choice-based conjoint analysis study. J Affect Disord. 2013;148(2–3):210–219. | ||
Melillo P, Delle Donne A, Improta G, Cozzolino S, Bracale M, eds. Assessment of patient satisfaction using an AHP model: an application to a service of pharmaceutical distribution. In: Proceedings of the International Symposium on the Analytic Hierarchy Process; June 15–18, 2011; Sorrento, Naples, Italy. | ||
Deshmukh A, Millet I. An analytic hierarchy process approach to assessing the risk of management fraud. J Appl Business Res. 1999;15(1):87–102. | ||
Mago R, Mahajan R, Thase ME. Medically serious adverse effects of newer antidepressants. Curr Psychiatry Rep. 2008;10(3):249–257. | ||
Lucena MI, Carvajal A, Andrade RJ, Velasco A. Antidepressant-induced hepatotoxicity. Expert Opin Drug Saf. 2003;2(3):249–262. | ||
Flanagan RJ, Dunk L. Haematological toxicity of drugs used in psychiatry. Hum Psychopharmacol. 2008;23 Suppl 1:27–41. | ||
Stübner S, Grohmann R, Engel R, et al. Blood dyscrasias induced by psychotropic drugs. Pharmacopsychiatry. 2004;37 Suppl 1:S70–S78. | ||
Voican CS, Corruble E, Naveau S, Perlemuter G. Antidepressant-induced liver injury: a review for clinicians. Am J Psychiatry. 2014;171(4):404–415. | ||
Marcum ZA, Vande Griend JP, Linnebur SA. FDA drug safety communications: a narrative review and clinical considerations for older adults. Am J Geriatr Pharmacother. 2012;10(4):264–271. | ||
Ginsberg LD. Impact of drug tolerability on the selection of antidepressant treatment in patients with major depressive disorder. CNS Spectr. 2009;14(12 Suppl 12):8–14. | ||
Roose SP. Compliance: the impact of adverse events and tolerability on the physician’s treatment decisions. Eur Neuropsychopharmacol. 2003;13 Suppl 3:S85–S92. | ||
Buchwald AM, Rudick-Davis D. The symptoms of major depression. J Abnorm Psychol. 1993;102(2):197–205. | ||
Erlangsen A, Nordentoft M, Conwell Y, et al; International Research Group on Suicide Among the Elderly. Key considerations for preventing suicide in older adults: consensus opinions of an expert panel. Crisis. 2011;32(2):106–109. | ||
Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389. | ||
Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatr. 1960;23:56–62. | ||
Papakostas GI. Cognitive symptoms in patients with major depressive disorder and their implications for clinical practice. J Clin Psychiatry. 2014;75(1):8–14. | ||
Hybels CF, Blazer DG, Pieper CF, Landerman LR, Steffens DC. Profiles of depressive symptoms in older adults diagnosed with major depression: latent cluster analysis. Am J Geriatr Psychiatry. 2009;17(5):387–396. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

