Back to Journals » Risk Management and Healthcare Policy » Volume 16
Clinical Knowledge, Perceptions, and Communication Confidence Regarding the Development of Thyroid Cancer ——A Cross-Sectional Study of Clinical Medical Students in Chongqing, Southwest China
Authors Yang C, Feng X, Li J, Jiang Y, Zhang H, Gao Y, Tan J, Ran B
Received 2 June 2023
Accepted for publication 2 October 2023
Published 11 October 2023 Volume 2023:16 Pages 2101—2111
DOI https://doi.org/10.2147/RMHP.S424052
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Gulsum Kubra Kaya
Chuang Yang,1 Xing Feng,1,2 Junfeng Li,1 Yuchan Jiang,1 Huan Zhang,1 Yidan Gao,1 Jinxiang Tan,1 Bolin Ran3
1Department of Breast and Thyroid Surgery, the First Affiliated Hospital of Chongqing Medical University, Chongqing, 400016, People’s Republic of China; 2Department of Hepatobiliary, Breast and Thyroid Surgery, the People’s Hospital of Liangping District, Chongqing, 405200, People’s Republic of China; 3Department of Medical Laboratory Science, Laboratory of Traditional Chinese Medicine Hospital of Shizhu County, Chongqing, 409100, People’s Republic of China
Correspondence: Jinxiang Tan; Bolin Ran, Tel/Fax +86-23-89011496, Email [email protected]; [email protected]
Purpose: Medical students play an essential role in providing disease consultation for patients. Despite the rapid increase in thyroid disease, there are few data on how well Chinese medical students master the knowledge of thyroid diseases. This study aims to evaluate the clinical knowledge, perception, and clinical communication confidence of medical students on thyroid cancer (TC).
Patients and Methods: This cross-sectional study was carried out among medical students of Chongqing Medical University. An anonymous, self-administered questionnaire distributed from December 2022 to February 2023 included items on demographics and other information, the warning signs of cancer, perception regarding a person’s chance of developing cancer, and clinical communication confidence. Descriptive analysis, difference analysis, and correlation analysis were carried out.
Results: A total of 226 medical students participated in the survey. Most students (n=191, 84.5%) had heard of TC, while only a few (n=10, 4.4%) regularly performed thyroid self-examination. One hundred and eighty-four students (81.4%) agreed that an unexplained lump or swelling could be a sign of cancer. There were significant differences in thyroid clinical knowledge in relation to gender (P< 0.001), major (P=0.026), and thyroid disease (P=0.030). Clinical communication confidence showed significant differences in year of study (P=0.002), major (P=0.048), and graduate major (P< 0.001). There was a correlation between clinical confidence and year of study (r=0.261, P< 0.001).
Conclusion: Most medical students have sufficient clinical knowledge on TC prevention, but there are still misconceptions related to TC screening. In addition, medical students lack confidence in communicating with patients. Comprehensive communication training should be integrated into the medical curriculum and clinical activities should be initiated earlier.
Keywords: thyroid cancer, cancer warning signs, clinical communication confidence, communication skills training, medical students
Introduction
The thyroid is the body’s largest endocrine gland, and secretes hormones involved in metabolism. Thyroid disease is a common clinical disease, with thyroid cancer (TC) being the most severe. TC is the most common malignant tumor in the endocrine system.1 The International Agency for Research on Cancer estimated 567,000 new cases and 41,000 deaths worldwide in 2020.1 Although TC has a relatively good prognosis compared to other malignancies, its incidence has been steadily increasing in many parts of the world, particularly in high-income countries.2 In America, it is estimated that it will be the second leading cancer diagnosis in women in 2030.3 Previous data have shown that the prevalence of TC is generally high in Asian countries, especially in South Korea, China, and other regions.4 From 2000 to 2016, the prevalence of TC among Chinese women increased year by year.5 The increasing incidence of TC has been attributed to the widespread use of imaging techniques such as ultrasound, which has led to the detection of small, indolent thyroid nodules that may not have been diagnosed in the past.6
There are multiple risk factors for TC. Exposure to ionizing radiation is a well-established risk factor for TC.7 As future doctors, clinical medical students may be exposed to radiation from medical instruments in the medical environment. Therefore, evaluating their knowledge of the risk factors, symptoms, and signs of thyroid disease can help to inform regarding the progress of the disease.
As the leading role in the medical diagnosis and treatment process, doctors play an important role in providing assistance and treatment plans for patients. Previous studies have shown that more engagement in emotional exchanges can lead to better patient prognosis and satisfaction.8 At present, communication skills training (CST) has been internationally recognized as an important component of medical education, which is reflected in the clinical process. A 2021 report among doctors in China showed that they are pessimistic about the doctor-patient relationship and there are obstacles in doctor-patient communication.9 Compared with other developed countries, China’s medical higher education is relatively backward. In addition, in the field of medical education, the curriculum system and curriculum development of communication skills in Chinese medical schools are not ideal, which can be attributed to the neglect of training in doctor-patient communication skills.10 Thus, it is necessary to improve the communication ability of medical students.
At present, the investigation of thyroid diseases in China is mainly aimed at the public, while research on the cognition and communication confidence of medical students on thyroid diseases is lacking. Also, the quality of self-made questionnaires in existing studies has not been assessed.11 In this study, a professional scale was used to measure clinical medical students’ knowledge of TC and to assess their current or future confidence in doctor-patient communication.
Research Questions
How well do medical students master the knowledge of TC?
Do medical students feel confident enough to communicate with patients?
Are there differences among different medical students in TC knowledge and clinical communication confidence?
Methods
Setting and Participants
This cross-sectional study involved an anonymous questionnaire survey that lasted for three months from December 2022 to February 2023. The subjects included undergraduate and graduate students in clinical medicine and non-clinical medical students (including nursing, laboratory medicine, imaging medicine, and other medical majors) from Chongqing Medical University. Undergraduate clinical medicine students in mainland China need to study for five years to obtain a bachelor’s degree. They spend the first four years of academic study in school and the fifth year in hospital clinical practice. Clinical graduate students need three years of standardized residency training to obtain a master’s degree, and they must choose an interested department as their research direction during the master’s degree period.12,13 All undergraduate and graduate students have their communication group, where online questionnaires are distributed and students are asked to complete them voluntarily. Participants need to complete all the questions before submitting the questionnaire to ensure a 100% completion rate, and the questionnaire cannot be added to after submission. Participants provided informed consent before completing the questionnaire.
The required sample size for this study was calculated by the Rao soft sample size calculator (http://www.raosoft.com/samplesize.html.) with a 95% confidence level, a pre-determined margin of error of 5%, and a 50% response distribution. We calculated a sample size of 306 students, and as the questionnaire was completed voluntarily, a total of only 226 students finally participated.
Survey Questionnaire
Parts of the questionnaire are shown in Figure 1. This questionnaire was based on early similar research,8,14,15 and adjusted according to our research purposes. Cancer Awareness Measure Scale (CAM) was cited in the questionnaire to evaluate the degree of medical students’ knowledge on cancer. We used Physician Confidence in the Medical Interview Scale (PCMI) to measure medical students’ confidence in communicating with patients. The first draft of the questionnaire was reviewed by experts; then, 37 medical students were randomly selected to conduct semi-structured interviews and complete a pre-survey questionnaire. Based on the pre-survey data, reliability analysis was conducted on the questions included in the questionnaire to evaluate the reliability of the scale items. We prepared a formal questionnaire according to the preliminary survey and interview results. The formal questionnaire consisted of four parts, I: Demographic and other information; II: The warning signs of cancer; III: Perception regarding a person’s chance of developing cancer; IV: Clinical communication confidence. We stipulated that pre-survey data were not included in the formal survey.
 |
Figure 1 Medical students’ clinical knowledge, perceptions, and communication confidence questionnaire on thyroid cancer. |
Part I: Demographic information included the age, gender, major, year of study, and thyroid status of the respondents. Other information also included the awareness and clinical information of TC.
Part II: This part asked participants: “The following may or may not be warning signs for cancer. Do you think X is a warning sign for cancer?” It lists nine possible signs of cancer. These questions were designed to measure how many warning signs a respondent could recognize when prompted. The options were yes, no, or do not know. The correct answer to this question was that all of the warning signs and symptoms listed could be warning signs of cancer.
Part III: Similar to Part II, the students were asked “These are some of things that can increase a person’s chance of developing cancer. How much do you agree that each of these can increase a person’s chance of developing cancer?” Eleven questions related to cancer risk were then listed. These closed questions were designed to measure a respondent’s level of agreement with the 11 risk factors. The correct answer to this question was that all of the risk factors listed could increase the chance of developing cancer.
Part IV: The last part of the questionnaire was related to medical students’ current confidence in clinical communication, which is subjective and has no correct answer.
The options for the second part of the questionnaire were as follows: Yes, No, and Do not Know. The knowledge score for warning signs of cancer was calculated for each item by allocating “one” to the correct answer and “zero” to the wrong answer. A five-point Likert scale was used for the third and fourth parts of the questionnaire, which ranged from 1 = strongly disagree to 5 = strongly agree. Then, Part II and Part III scores were added together as an evaluation of the knowledge of TC, which ranged from 11 to 64. Similarly, the clinical communication confidence score in Part IV ranged from 5 to 25.
Data Analysis
An online questionnaire platform was used to distribute questionnaires and collect information. The online questionnaire was imported into Excel, and the data were imported into SPSS for statistical analysis. Cronbach’s alpha coefficients were calculated to examine the internal consistency of the scale. Descriptive statistical analysis was carried out using frequencies and percentages (Including demographic information and TC knowledge). To verify the hypothesis, the Mann–Whitney test, Kruskal–Wallis test and bivariate linear correlation analysis were used with the correlation coefficient and P value. The test level was α = 0.05 in all statistical tests.
Ethical Consideration
This study was conducted according to the ethical guidelines of the Helsinki Declaration. The First Affiliated Hospital of Chongqing Medical University ethics committee ethically approved the study protocol (Approval No: K2023-165). As the survey was conducted anonymously, written informed consent was not necessary.
Results
Reliability Analysis
The Cronbach alpha of the total scale was 0.749, and the Cronbach alpha of each dimension was between 0.784 and 0.955, indicating that the scale had good reliability and high internal consistency among items.
Demographic and other information
The mean age of the 226 participants was 21.5, ranging from 17 to 28 years, with 150 (66.4%) females, and 76 (33.6%) males. One hundred and seventy (75.2%) were undergraduate (Year 1 to Year 5), and 56 (24.8%) were master (Year 6 to Year 8). One hundred and seventy (75.2%) were clinical medicine students, and 56 (24.8%) were non-clinical medicine students. Of the 56 graduate students, 16 (7.1%) majored in thyroid disease research. Forty-four (19.5%) indicated that they or their relatives had thyroid disease.
Most (n=191, 84.5%) had heard of TC, while only a few (n=10, 4.4%) regularly performed thyroid self-examination. When asked where they obtained their knowledge of the thyroid (Figure 2), most of them (n=153, 67.7%) thought it was from medical college courses, nearly half of them (n=109, 48.2%) chose the media, followed by consult books and articles (n=65, 28.8%), and others had suffered from thyroid disease (n=53, 23.5%). Eighty-one (35.8%) thought biopsy was the most common diagnostic method for screening TC when examining a thyroid nodule, while others did not know (n=71, 31.4%), followed by thyroid ultrasonography (n=59, 26.1%), computed tomography (n=9, 4.0%), and magnetic resonance imaging (n=6, 2.7%), (Table 1).
 |
Table 1 Demographic and Other Information (N=226) |
 |
Figure 2 Sources of thyroid knowledge for medical students. |
Table 2 describes participants’ attitudes toward cancer symptoms and signs. Most students agreed that these signs were related to cancer. One hundred and eighty-four (81.4%) agreed that an unexplained lump or swelling could be a sign of cancer.
 |
Table 2 Clinical Medical Students’ Knowledge Regarding Warning Signs of Cancer (N=226) |
The participants’ attitudes regarding cancer risk are shown in Table 3. The results indicated that they were more inclined towards a supportive attitude. The majority of students agreed that smoking (85.9%) and exposure to smoke (83.2%) can cause cancer. More than two-thirds (76.6%) believed that drinking more than 1 unit of alcohol a day can increase a person’s chance of developing cancer. Approximately 65.9% agreed that being overweight (BMI over 25) can increase the risk of cancer and 56.6% agreed that sunburn more than once as a child can cause cancer. Furthermore, more than half of the students agreed being over 70 years old (73.9%), having a close relative with cancer (75.2%), and infection with HPV (Human Papillomavirus) (62.8%) may also increase the likelihood of developing cancer.
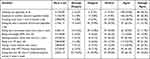 |
Table 3 Clinical Medical Students’ Perception Regarding a Person’s Chance of Developing Cancer |
However, less than half of the students agreed that other behaviors increase cancer risk. 38.9% believed eating less than 5 portions of fruit and vegetables a day can cause cancer while eating red or processed meat once a day or more will increase the risk of cancer. Similarly, 36.5% of the students thought that doing less than 30 mins of moderate physical activity 5 times a week was a risk factor.
The scores based on demographic information are summarized in Table 4. The average score for participants’ knowledge was 47.07. There were significant differences in TC knowledge scores in terms of gender (P<0.001), major (P=0.026), and thyroid disease (P=0.030), while there were no significant differences in years of study (P=0.223), and graduate major (P=0.159). The mean clinical communication confidence score was 12.85. Clinical communication confidence showed significant differences in years of study (P=0.002), major (P=0.048), and graduate major (P<0.001), and clinical confidence was correlated with years of study (r=0.261, P<0.001). There was no significant difference in gender (P=0.118) and thyroid disease (P=0.694).
 |
Table 4 Association Between the Students’ Knowledge and Clinical Communication Confidence Score Levels and Demographics |
To verify our hypothesis, we calculated the correlation between TC knowledge, clinical communication confidence and years of study (Table 5).
 |
Table 5 The Correlation Between Thyroid Cancer Knowledge, Clinical Communication Confidence and Years of Study |
Discussion
TC, as an endocrine system tumor, has gradually received attention from the public due to a rise in incidence. We conducted our study at a Chinese Medical University. This appears to be the first time a professional scale has been used to evaluate the knowledge of TC among Chinese medical students. In addition, it also assessed students’ confidence in communicating with patients. The research results indicate that the majority of participants have comprehensive prevention knowledge on TC, but lack correct awareness of thyroid screening. Furthermore, it is worth noting that a lack of clinical communication confidence among medical students seems to be common.
Although this study shows that most of the participants had a good knowledge level of TC, few of them (4.4%) regularly performed thyroid self-examination. We do not recommend thyroid testing for other populations. However, due to their profession, medical students need to know the screening process. In this survey, 84.5% of participants knew about TC, and the majority (67.7%) of them learned about thyroid disease through medical courses. This demonstrated the importance of theoretical teaching in medical education. Unexpectedly, quite a few students (35.8%) thought biopsy was the most common diagnostic method for screening TC when examining thyroid nodules, while others (26.1%) chose thyroid ultrasonography. The accuracy was lower than that in the survey in both Saudi Arabia and China.11,15 This shows that medical students lack knowledge regarding TC screening.
Encouragingly, most of the participants had good knowledge on cancer prevention, and quite a few medical students could identify the typical symptoms of TC, such as neck lump (81.4%), hoarseness (67.3%), and difficulty swallowing (76.5%). These results are much higher than those of a study carried out in Saudi Arabia, which reported that an unexplained lump or swelling (65.24%), a persistent cough or hoarseness (43.97%), and persistent difficulty in swallowing (54.6%) as the early signs of TC.15 Consistent with previous studies, most believed that smoking or exposure to second-hand smoke increases the risk of TC.15 It is easy to agree that smoking is a major risk factor for various types of cancer and a poor prognosis, but a recent cohort study showed that current smoking was associated with a reduced risk of TC in Korean men.16 In addition, there is evidence that smoking leads to higher levels of thyroid hormones, which causes the development of hyperthyroidism or other thyroid diseases.17 Although this is a controversial topic, we cannot deny that smoking cessation has more benefits overall.
Similar to other studies, our investigation found that females have significantly higher TC knowledge scores.15 Studies have shown that female medical students have better learning plans and higher learning motivation.18,19 On the other hand, it is a fact that the global incidence and mortality rate of TC is higher in women than in men.20 Therefore, it is not surprising that female medical students have a deeper understanding and pay greater attention to TC. Our results showed that there was a statistically significant difference in TC knowledge in terms of major, with clinical medicine majors having more knowledge. A survey conducted by other medical schools in China may explain this phenomenon. The authors concluded that receiving clinical teaching can significantly improve the cognitive level of TC among medical students, and clinical medical students have more opportunities to interact with patients.11 In addition, we found that participants who chose “others around those who had suffered from the disease” had higher TC knowledge scores, and most of them (79.3%) agreed that having a close relative with cancer would increase the risk of developing cancer. Therefore, they may be more alert to enhancing disease prevention.
It should be noted that medical students are viewed as trusted sources of health-related information. To some extent, the communication confidence of medical students will affect the doctor-patient relationship. Our research found that clinical communication confidence was correlated with years of study, and this ability varied in different years of study with an upward trend from year 1 to year 8 (P<0.05, R=0.261). This may be due to the accumulation of medical knowledge and clinical experience. Therefore, compared with non-thyroid surgery students, it is easy to understand that thyroid surgery students have higher communication confidence. Compared with postgraduate students, undergraduates were weak in clinical communication. In recent years, some medical colleges in China have set up CST elective courses for clinical medicine undergraduates to improve their communication skills and confidence. However, it should be emphasized that there is no systematic and comprehensive CST in compulsory courses, and students’ enthusiasm for elective courses is low.21 Diversified compulsory courses should be included in the training plan in the future curriculum. The Chinese undergraduate medical education standards-clinical medicine issued by the Ministry of Education stipulates that medical schools must ensure students acquire comprehensive clinical skills. It is recommended that undergraduate medical students begin clinical practice as soon as possible.13 Furthermore, our research found that senior students who engage in clinical work earlier have higher communication confidence. We suggest that schools offer clinical courses and practical activities earlier to enhance students’ clinical communication confidence. A recent study in the Chinese Mainland showed that a majority of Chinese physicians were trained in communication skills and showed a highly positive attitude towards CST.22 Generally speaking, graduate students seem to lack such training. In earlier years, three years of standardized residency training were implemented to compensate for weaknesses in undergraduate clinical education by the Chinese government.12 In fact, many hospitals lack systematic training in their communication skills but rely more on social experience from communicating with patients. To adapt to the clinical environment and improve communication initiatives, hospitals need to develop CST programs for graduate students and introduce professional communication assessment tools.21,23,24
There are some limitations in the present study. Our investigation was limited to Chongqing Medical University, which cannot represent all medical schools in China. We expect to expand our research scope in the future. At the same time, the results were based on an online self-completed questionnaire, which may have increased the possibility of social desirability bias and underestimated medical students’ true ability for cancer awareness and communication skills. Furthermore, our research shows that graduate students have high confidence in clinical communication. Thus, training measures are more applicable to undergraduate students. Despite its limitations, we emphasize that medical students at different stages do not completely grasp the knowledge on thyroid diseases. We believe that our study can provide ideas for the future reform of CST courses.
Data Sharing Statement
The raw data supporting the conclusions of this article will be made available by the corresponding authors, without undue reservation.
Ethics Approval and Informed Consent
The studies involving human participants were reviewed and approved by the First Affiliated Hospital of Chongqing Medical University.
Consent for Publication
The authors agree to publish any information about the article.
Acknowledgments
The authors of the study extend their appreciation to the Chongqing Medical University, China, for supporting this work.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There was no funding and financial support for this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sung H, Ferlay J, Siegel R, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–249. doi:10.3322/caac.21660
2. Lim H, Devesa S, Sosa J, Check D, Kitahara C. Trends in Thyroid Cancer Incidence and Mortality in the United States, 1974-2013. JAMA. 2017;317(13):1338–1348. doi:10.1001/jama.2017.2719
3. Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014;74(11):2913–2921. doi:10.1158/0008-5472.CAN-14-0155
4. Deng Y, Li H, Wang M, et al. Global Burden of Thyroid Cancer From 1990 to 2017. JAMA Netw Open. 2020;3(6):e208759. doi:10.1001/jamanetworkopen.2020.8759
5. Zheng RS, Zhang SW, Zeng HM. Cancer incidence and mortality in China, 2016. J National Cancer Center. 2022;2022:
6. Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA. 2006;295(18):2164–2167. doi:10.1001/jama.295.18.2164
7. Han MA, Kim JH. Diagnostic X-Ray Exposure and Thyroid Cancer Risk: systematic Review and Meta-Analysis. Thyroid. 2018;28(2):220–228. doi:10.1089/thy.2017.0159
8. Ishikawa H, Eto M, Kitamura K, Kiuchi T. Resident physicians’ attitudes and confidence in communicating with patients: a pilot study at a Japanese university hospital. Patient Educ Couns. 2014;96(3):361–366. doi:10.1016/j.pec.2014.05.012
9. Department of Sociology, Tsinghua University, Chinese Social Survey and Research Center, Academy of Social Sciences, Tsinghua University, Humanistic Medicine Committee of Chinese Medical Doctor Association. 2021 Chinese Physician Survey Report. 2021. Available from: https://www.soc.tsinghua.edu.cn/__local/8/23/F8/634DECF776A7FCEC495B3F7AD93_AC9AC79B_114EF0.pdf.
10. Hu Z. Study on the Value of Clinical Medicine Professional Certification in Promoting Reform on the Teaching Model of Doctor-Patient Communication. Chine Health Service Manage. 2018;35(04):296–297.
11. Liu P, Lin J, Nie Y, Cao Z, Xu X. Awareness of thyroid cancer among medical students: a questionnaire-based study. Sci Prog. 2021;104(2):311994150. doi:10.1177/00368504211023654
12. Zhu J, Li W, Chen L. Doctors in China: improving quality through modernisation of residency education. Lancet. 2016;388(10054):1922–1929. doi:10.1016/S0140-6736(16)00582-1
13. Wang W. Medical education in China: progress in the past 70 years and a vision for the future. BMC Med Educ. 2021;21(1):453. doi:10.1186/s12909-021-02875-6
14. Cancer Research UK UCL, Kings College London, and University of Oxford Cancer Awareness Measure (CAM). 2007-2008. Available from: www.cancerresearchuk.org/sites/default/files/health_professional_cancer_awareness_measure_toolkit_version_2.1_09.02.11.pdf.
15. Syed W, Samarkandi OA, Alsadoun A, Harbi M, Al-Rawi M. Evaluation of clinical knowledge and perceptions about the development of thyroid cancer-An observational study of healthcare undergraduates in Saudi Arabia. Front Public Health. 2022;10:912424. doi:10.3389/fpubh.2022.912424
16. Alhazmi RA, Alobaid AM, Althunayyan SM, Syed W, Al-Rawi M. A cross-sectional assessment of knowledge, awareness of risk factors, and perceptions of thyroid disease (TD) among adults living in Saudi Arabia - A community based study. Front Public Health. 2022;10:1041745. doi:10.3389/fpubh.2022.1041745
17. Asvold BO, Bjøro T, Nilsen TI, Vatten LJ. Tobacco smoking and thyroid function: a population-based study. Arch Intern Med. 2007;167(13):1428–1432. doi:10.1001/archinte.167.13.1428
18. Demirören M, Turan S, Öztuna D. Medical students’ self-efficacy in problem-based learning and its relationship with self-regulated learning. Med Educ Online. 2016;21:30049. doi:10.3402/meo.v21.30049
19. Busch A, Rockenbauch K, Schmutzer G, Brähler E. Do medical students like communication? Validation of the German CSAS (Communication Skills Attitude Scale). GMS Z Med Ausbild. 2015;32(1):Doc11. doi:10.3205/zma000953
20. Pizzato M, Li M, Vignat J, et al. The epidemiological landscape of thyroid cancer worldwide: GLOBOCAN estimates for incidence and mortality rates in 2020. Lancet Diabetes Endocrinol. 2022;10(4):264–272. doi:10.1016/S2213-8587(22)00035-3
21. Liu X, Rohrer W, Luo A, Fang Z, He T, Xie W. Doctor-patient communication skills training in mainland China: a systematic review of the literature. Patient Educ Couns. 2015;98(1):3–14. doi:10.1016/j.pec.2014.09.012
22. Du J, Mayer G, Posenato E, et al. Communication Skills (CS) training of physicians in China and its role in actual challenges of patient-physician relationship: a cross-sectional survey. BMC Med Educ. 2022;22(1):783. doi:10.1186/s12909-022-03830-9
23. Nakagawa S, Fischkoff K, Berlin A, Arnell TD, Blinderman CD. Communication Skills Training for General Surgery Residents. J Surg Educ. 2019;76(5):1223–1230. doi:10.1016/j.jsurg.2019.04.001
24. Schumm MA, Ohev-Shalom R, Nguyen DT, Kim J, Tseng CH, Zanocco KA. Measuring patient perceptions of surgeon communication performance in the treatment of thyroid nodules and thyroid cancer using the communication assessment tool. Surgery. 2021;169(2):282–288. doi:10.1016/j.surg.2020.08.019
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
