Back to Journals » Journal of Inflammation Research » Volume 16
Clinical Features and Predictive Nomogram of Acute Kidney Injury in Aging Population Infected with SARS-CoV-2 Omicron Variant
Authors Zhang Y, Li X, Zhang S, Chen W, Lu J, Xie Y, Wu S, Zhuang F, Bi X, Chu M, Wang F, Huang Y, Ding F, Hu C, Pan Y
Received 18 April 2023
Accepted for publication 11 July 2023
Published 18 July 2023 Volume 2023:16 Pages 2967—2978
DOI https://doi.org/10.2147/JIR.S413318
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Tara Strutt
Yumei Zhang,1,* Xin Li,1,* Suning Zhang,2 Wei Chen,3 Jianxin Lu,1 Yingxin Xie,1 Shengbin Wu,1 Feng Zhuang,1 Xiao Bi,1 Mingzi Chu,1 Feng Wang,1 Yemin Huang,1 Feng Ding,1 Chun Hu,1 Yu Pan1
1Division of Nephrology, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China; 2Division of Emergency, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China; 3Division of Neurology, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yu Pan; Chun Hu, Division of Nephrology, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, 201900, People’s Republic of China, Tel +86-021-56691101, Email [email protected]; [email protected]
Background: Since little is known about the acute kidney injury (AKI) in aging population infected with SARS-CoV-2 Omicron variant, we investigated the incidence, clinical features, risk factors and mid-term outcomes of AKI in hospitalized geriatric patients with and without COVID-19 and established a prediction model for mortality.
Methods: A real-time data from the Shanghai Ninth People’s Hospital information system of inpatients with COVID-19 from 1 April 2022 to 30 June 2022 were extracted. Clinical spectrum, laboratory results, and clinical prognosis were included for the risk analyses. Moreover, Cox and Lasso regression analyses were applied to predict the 90-day death and a nomogram was established.
Results: A total of 1607 SARS-CoV-2 infected patients were enrolled; hypertension was the most common comorbidity, followed by chronic cardiovascular disease, diabetes mellitus, and lung disease. Most of the participants were non-vaccinated and the mean age of patients was 82.6 years old (range, 60– 103 years). The AKI incidence was higher in relatively older patients (16.29% vs 3.63% in patients older than 80 years and 60 to 80 years, respectively). Linear regression models identified some variables associated with the incidence of AKI, such as older age, clinical spectrum, D-dimer level, number of comorbidities, baseline eGFR, and antibiotic or corticosteroid treatment. In this cohort, 11 patients died in-hospital and 21 patients died at 90-day follow-up. The predictive nomogram of 90-day death achieved a good C-index of 0.823 by using 5 predictor variables: ICU admission, D-dimer, peak of serum creatinine, rate of serum creatinine decline and white blood cell count (WBC).
Conclusion: Older age, clinical spectrum, D-dimer level, number of comorbidities, baseline eGFR, and antibiotic or corticosteroid treatment are clinical risk factors for the incidence of AKI in geriatric COVID-19 patients. The prediction nomogram achieved an excellent performance at the prediction of 90-day mortality.
Keywords: COVID-19, Omicron, acute kidney injury, aging, predictive nomogram
Introduction
Since the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Omicron variant was identified in November 2021, it has become the main epidemic strains in multiple countries.1,2 The transmissibility of Omicron BA.2 is significantly enhanced compared to the earlier non-Omicron variants due to its immune escape ability.3–5 There were 626,863 Omicron infections reported by Shanghai Municipality between March 1 and June 4, 2022.6 Although it is suggested that Omicron is associated with significantly reduced severity and mortality compared with previous SARS-CoV-2 variants,7 the management of critically ill patients still remains a challenge. Given the tremendous transmissibility of Omicron, the clinical profile and prognosis of the huge population of Omicron infections would strongly influence the public health policies, including hospitalization and treatment strategies.8
Acute kidney injury (AKI) is one of the most frequent and significant complications in hospitalized patients with SARS-CoV-2.9 Observational studies demonstrated that patients who developed AKI were more likely to be admitted to an intensive care unit (ICU), require invasive mechanical ventilation and result in increased mortality.9–11 As we knew, the aging people are at increased risk of developing AKI following severe infection, while the AKI in geriatric patients infected with COVID-19 Omicron variant is not fully understood. Therefore, we conducted this single-center real-world study in Shanghai to analyze the clinical features and risk factors that would predict the mortality in hospitalized COVID-19 patients.
Until now, most studies focused on AKI in COVID-19 adopted the traditional Kidney Disease Improving Global Outcomes (KDIGO) definition, which defined as a rise in serum creatinine, either by 26.5μmol/L in 48 hours or by 50% from baseline over a 7-day period.12 This definition is appropriate to diagnose AKI occurs during hospitalization; however, it could fail to identify cases developed in the community and had recovered partially by the time the patients were admitted to the hospital, thereby underestimate the true incidence of AKI. To address this limitation, the International Society of Nephrology (ISN) 0by25 studies added a commensurate fall in serum creatinine to their definition of AKI making it a more comprehensive and inclusive definition.13–15 Extended KDIGO (eKDIGO) AKI was defined by a fall in serum creatinine by 26.5μmol/l within 48 hours or a fall to more than 1.5 times the baseline serum creatinine within 7 days. The eKDIGO definition can identify AKI not only during its development but also in its recovery phase, which would help us to get more closer to the actual incidence of AKI. In this case, the integration of this additional criterion to identify kidney injury has also been highlighted as one of the research priorities in recent KDIGO report on controversies in AKI.16 Given the global impact of SARS-CoV-2 infection combined with the potentially burden of AKI in community, we adopted both KDIGO and eKDIGO definition to identify AKI patients with COVID-19 in our study and hypothesized that the additional cases identified by this extended criterion would result in poorer outcomes compared with those non-AKI patients. And then comparisons between the subgroups of KDIGO AKI, eKDIGO AKI and non-AKI were made to analyze the clinical features of AKI in the aging population infected with Omicron. Furthermore, multivariate regression was used to screen the risk factors of AKI occurrence. Cox and Lasso regression analyses were applied to predicting 90-day mortality and a nomogram to predict the 90-day death of AKI patients was established.
Materials and Methods
Study Design
This single-center real-world study required no change to clinical management. The clinical classification and treatment was conducted according to the standards of the Chinese Diagnosis and Treatment of Pneumonia Caused by New Coronavirus Infection (ninth version).17 Patients with mild clinical symptoms and no pneumonia manifestation in imaging were classified into the mild group, while patients with mild clinical manifestations and pneumonia imaging were grouped as moderate. Participants were classified to severe Omicron infection when SpO2≤93% in resting state. Viral clearance was confirmed when two consecutive negative nucleic acids of SARS CoV-2 real-time polymerase reaction chain (RT-PCR) test were reported (cycle threshold value large than 35 in both ORF1ab and N genes), with interval of 24 hours at least. The length of nucleic acid positive was defined as the first day of positive nucleic acid test to the date of the first negative test of the consecutive negative results. This study was approved by the hospital ethics committee of Shanghai Ninth People’s Hospital, School of Medicine, Shanghai Jiaotong University (approval number:SH9H-2022-T402-1). All of the experimental protocols were implemented in accordance with the relevant guidelines and regulations. In accordance with the Declaration of Helsinki, patients or their legal guardians had obtained written informed consent prior to participation.
Inclusion and Exclusion Criteria
All the individuals recruited in our hospital with Omicron infection from April 18, 2022, to June 5, 2022, confirmed by SARS-CoV-2 RT-PCR tests were included (Figure 1). Patients younger than 60 years and those on renal replacement therapy (RRT; dialysis or transplantation) were excluded. Patients with less than two serum creatinine measurements during the admission and those with incomplete laboratory data were also excluded. 1607 patients were recorded in this study and 346 patients were included in the final analysis cohort (Figure 1). Ethical approval was obtained from the ethics committee of Shanghai Ninth People’s Hospital.
 |
Figure 1 Flow diagram of the study. HIS: Hospital Information System. |
AKI Definition and Diagnosis
Diagnosis and stage of AKI were defined according to both KDIGO and eKDIGO criteria. Patients’ serum creatinine levels throughout the admission were used to classify them as (i) non-AKI, not having AKI; (ii) eKDIGO AKI, having AKI according to the extended KDIGO (eKDIGO) criteria; or (A) KDIGO AKI, AKI according to the traditional KDIGO definition and (B) eKDIGO AKI. AKI was classified accordingly as staging criteria for each definition.15 A moving window of 48 hours and 7 days was applied during the entire length of admission, the minimum serum creatinine within that window was deemed as the baseline, the maximum serum creatinine within that window became the highest stage. Urine volume criteria were not used for either definition as patients’ urine volume was not routinely collected.
Data Collection and Analyses
Data collection for Covid-19 patients commenced on April 18, 2022. Information was collected for the duration of a patient’s admission by visual inspection of hospital information system, included characteristics, treatments, complications, and outcomes. Clinical prognosis included oxygen saturation and AKI stage. Outcomes contained use of invasive mechanical ventilation, all-cause death in-hospital or 90-day death after AKI events, and length of nucleic acid positive. The frequency of serum creatinine test was discretion of attending physicians. Mortality at 90 days after AKI event was identified by telephone follow-up. Incidence, characteristics, treatment and outcome of AKI and non-AKI patients were evaluated respectively; univariate and multivariate regression were used to select the risk factors of AKI occurrence; lasso analysis was used to establish a nomogram to predict the death of AKI patients 90 days after AKI events accordingly.
Statistical Analysis
For continuous variables, characteristics were reported as mean values ± standardized deviation if they were Gaussian distribution by Kolmogorov–Smirnov test. Otherwise, they were expressed as medians and interquartile ranges (IQRs) and the Mann–Whitney U-test was applied. Categorical variables were reported as counts and percentages and analysed by Pearson chi-squared test. A multivariate regression was fitted to assess the factors influencing eKDIGO AKI incidence. Univariate Cox logistic regression was used to select the clinical index associated with AKI mortality. Collinearity indicators were screened out by lasso regression. The final variables obtained by lasso regression were subsequently used to construct a random forest classifier. The data were randomly split into a training set selected in a ratio of 0.5, 0.6, 0.7, 0.8, and a validation set containing the remaining patients. The discriminatory ability of the nomogram was validated by using receiver operating characteristics (ROC) curves. The process was conducted 1000 times at random. The area under the curve (AUC) of the 1000 verifications was Calculated with the R package and the sampling proportion of training set and validation set was selected with the highest AUC. The proposed method of Mean Decrease Accuracy (MDA) calculated the relative contributions of each significant clinical index within this classification process. Statistical analyses were performed with SPSS (version 26, IBM, Armonk, NY, USA), and R software (version 4.1.1; http://www.r-project.org). P <0.05 was considered statistically significant.
Results
Characteristics of the Total Population and the Adopted Population
In our research, 38.2% of the Omicron infected patients were older than 80 years (Table 1), and the oldest was 103 years old. Hypertension was the most common comorbidity (63.0%), followed by chronic cardiovascular disease, diabetes mellitus and lung disease (Table 2). Among these patients, 86.1% were unvaccinated and most SARS-CoV-2 clinical spectrum was moderate (76.9%). It is demonstrated that clinical spectrum, comorbidities, and treatment at admission were very similar in the aging population whether they were over or under 80 years old (Supplementary Table 1). According to the eKDIGO definition, additional 136 patients were diagnosed with AKI. Matching (1:2) based on propensity score was applied to achieve a balanced baseline by age, gender and Cov-SARS-2 clinical spectrum. One hundred and thirty-three AKI patients and 213 non-AKI patients were included for the final analysis. The peak stages of AKI with eKDIGO definition were the following: stage 1: 86.5%; stage 2: 6.8% and stage 3: 6.8% (Table 2).
 |
Table 1 AKI Incidence in Aging Population |
 |
Table 2 The Characteristics of the Adopted Population, Including AKI and Non-AKI Participants |
Comparisons Between AKI Participants and Non-AKI Participants
Comparisons of the collected variables were performed among patients with eKDIGO AKI and non-AKI. Baseline characteristics of demographics, Cov-SARS-2 clinical spectrum, vaccination, complications, and laboratory results are provided in Table 2. Non-vaccination was associated with an increased risk of AKI (91.7% vs 82.6%, p = 0.042). Patients developed AKI presented with worse Cov-SARS-2 clinical spectrum compared to those without AKI and accompanied with more comorbidities. Chronic cardiovascular disease (CVD), cerebrovascular disease, hypertension, and liver disease were significantly more frequent in AKI patients (Table 2). AKI patients with decreased plasma albumin level were accompanied with lower oxygen saturation, estimated glomerular filtration rate (eGFR, estimated with CKD-EPI equation) and peripheral CD3+CD8+ T cells, compared to those without AKI. Increased levels of serum D-dimer, high-sensitivity C-reactive protein (CRP), interleukin 6 (IL-6) and tumor necrosis factor-α (TNF-α) were also presented in AKI patients, which suggested that the inflammation responses and coagulopathy were more severe in AKI patients. Moreover, administration of antibiotic and antifungal agents, corticosteroid, low-molecular-weight heparin (LMW heparin), nutrition support was also more common among AKI patients compared to non-AKI patients (Table 3). Meanwhile, the duration of positive nucleic acid was longer in AKI patients [11.2±5.47 vs 9.1±3.86, p = 0.000]. The AKI patients had worse outcomes, higher rates of invasive mechanical ventilation support (14.3% vs 4.2%, p = 0.001), increased in-hospital mortality (6.0% vs 0.9%, p = 0.006) and 90-day mortality (10.5% vs 3.3%, p = 0.006), therefore, increased the health care costs than those without AKI (p-value < 0.001) (Table 3).
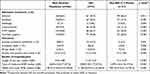 |
Table 3 The Treatment and Outcome of the Population with AKI and Non-AKI |
Linear Regression Models for Risk Factors of AKI Occurrence
Multivariable linear regression model with an enter process was applied to reveal the risk factors associated with the incidence of AKI. Our data demonstrated that older age, moderate or severe clinical spectrum, more kinds of comorbidities, lower baseline eGFR, higher D-dimer level, ICU admission and antibiotic agents contributed to the incidence of AKI (Table 4).
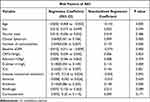 |
Table 4 Linear Regression Models for Risk Factors of AKI Occurrence |
Characteristics of the Adopted Population and Comparison eKDIGO AKI Patients with Non-AKI Participants
In this study, there were 35 AKI patients diagnosed by KDIGO definition and an additional 98 AKI patients according to the eKDIGO definition. The clinical features were compared between eKDIGO-AKI patients and non-AKI patients (Supplementary Table 2). The AKI patients presented with more underlying comorbidities, especially chronic cardiovascular disease, cerebrovascular disease, chronic kidney disease and hypertension. Levels of D-dimer, CRP, IL-6 and TNF-α was significantly increased in AKI patients compared to those without AKI. Accordingly, administration of antibiotic agents, corticosteroid, LMW heparin, nutrition support was more frequent among AKI patients than non-AKI individuals and more common in KDIGO AKI than eKDIGO AKI. (Supplementary Table 3). Furthermore, the hospitalization was remarkably prolonged in the eKDIGO-AKI group [11.3±5.60 vs 9.1±4.29, p = 0.000] and the costs of medicine and health care were significantly increased compared with the non-AKI patients.
Development of a Predictive Nomogram for the 90-Day Death of AKI Patients in Aging Population Infected with Cov-SARS-2 Omicron Variant
To explore the risk factors of the 90-day mortality in AKI patients, we performed discrete and 90-day mortality enrichment analyses, respectively. Seventeen discrete measures were associated with 90-day mortality events (Figure 2). Based on the coefficient of AKI risk index was not 0 obtained from lasso regression (as shown in Supplementary Table 4), we used a random forest algorithm to collect samples in the training set with the sampling ratio of 0.5, 0.6, 0.7, and 0.8, respectively and used the remaining samples as the validation set to construct the classifier and verify (Supplementary Figure 1). This training and validation cycle is 1000 times as shown in Supplementary Table 4. The area under curve (AUC) of each time was calculated, and the AUC results of each sampling ratio were compared (Figure 1). Considering that the sampling ratio of 0.8 was with the highest AUC (Figure 2), the contribution of each indicator to the classifier prediction (Mean Decreasing AUC, MDA) was calculated based on 1000 cycles under the sampling ratio of 0.8. The ranking of the contribution degree of each index is shown in Figure 2. Due to the contribution of ICU admission, D-dimer, peak of serum creatinine, rate of serum creatinine decline, and white blood cell level to 90-day mortality, they were used to construct the prediction nomogram for 90-day death. The C-statistic was 0.823 (Figure 3).
Discussion
To our knowledge, this study is the first and most extensive collection until recently to describe the occurrence of AKI in the geriatric COVID-19 patients in real-world practice based on the data from Shanghai. In this cohort of geriatric patients with COVID-19, an increased incidence of AKI was observed and a worse mid-term outcome was developed in AKI patients compared with those without AKI.
As reported by early studies, AKI was quite frequent among the hospitalized patients with COVID-19, especially the geriatric individuals and increased the risk of mortality.9,18 As far as we are concerned, this is the first study focused on the patients older than 80 years in China. Xu and colleagues reported the incidence of AKI in older adults with COVID-19 was 29% in a Swedish cohort of hospitalized geriatric patients.19 And a study from Italy reported that 233 (aged 73.5±11.9 years old) of 1701 COVID-19 patients (13.7%) developed AKI.20 While in studies from New York, among the old patients with mean age from 64 to 66 years old, the incidence of AKI varies from 29% to 56.9%.21,22 Meanwhile, in other studies, which enrolled mainly elderly patients from China (with ≥70% patients with mean age ≥60 years old), the incidence of AKI varies from 50.6% in critically ill patients23 to 5.3–31.7% (with a mean incidence of 13.3%, 73 of 549) in non-critical ill patients,24 which support our findings.
As we know, the traditional KDIGO definition could fail to identify patients for whom hospitalization coincides with recovery of AKI as manifested by a decrease in serum creatinine. These AKI cases might be the consequences of early rehydration caused by gastrointestinal fluid losses, fever or treatment with ACE-inhibitors or ARBs before admission.25,26 Therefore, we applied an eKDIGO definition, adapted from the international Society of Nephrology (ISN) 0by25 studies27 and got a remarkable increased detection rate as expected (35 vs 98 patients by traditional KDIGO definition and eKDIGO definition, respectively). Moreover, we also demonstrated a significant increased incidence of AKI in COVID-19 patients who ≥80 years old compared with patients under 80 years old. And these AKI patients diagnosed by eKDIGO definition resulted in worse outcomes in a 3-month follow-up, which was consistent with the report of ISARIC Clinical Characterisation Group.27
Since our study is a real-world study, the patients enrolled in our study are older, having more medical comorbidities and more challenging social demographic issues compared to the patients included in RCTs. Therefore, it can provide scientific information on how factors such as clinical setting influence the treatment effects and outcomes for decision-making in clinical practice.28
As far as we know, there are only a few studies investigated the mid-term outcomes of AKI in elderly COVID 19 patients. Zhang and colleagues reported that most of the new-set AKI during hospitalization of elderly COVID-19 patients (with a median age of 64 years) recovered 4 months after discharge (130 of 143).29 While in a study reported by Chan, on a follow-up at a median of 21(IQR, 8–38) days after hospital discharge, 212 of 1835(12%) patients developed AKI during their hospitalization and 77 of 212(36%) patients discharged with AKD. Of these 77 patients, only 28 patients (36%) had recovery of AKD during the follow-up.9 In another study, during a 6-month follow-up of 1733 COVID-19 patients, Huang and colleagues found that there were some patients developed persistent renal dysfunctions.30 They also showed that there were 13% of patients with normal eGFR at the acute phase had decreased eGFR at follow-up. In our study, the results suggest that even most elderly patients who developed AKI have recovered after discharge, the outcomes in 3-months follow-up were still worse compared to the patients without AKI. Some potential mechanisms might play essential roles in the pathogenesis.
First of all, comorbidities are common in elderly individuals. Su and colleagues demonstrated that there is evidence of glomerular and vascular changes indicative of underlying diabetic of hypertensive disease besides the invasion of COVID-19 virus by analyzing 26 kidney abnormalities in 26 autopsies of patients with COVID-19.31 This is consistent with the risk factors we identified which are associated with AKI in this study, including hypertension, diabetes and chronic vascular disease.
Secondly, the immunosenescence of the geriatric patients contributes a lot to the pathogenesis of AKI. As we know, the hallmarks of aging, such as immunosenescence, inflammation, adaptive immunosenescence, likely contribute to the increased pathophysiological responses to SARS-CoV-2 among older adults.32 Previous research demonstrated that Coronaviruses can activate both NLRP3 inflammasome and NF-κB pathway.33 While some proinflammatory cytokines including interleukin (IL)-6, tumor necrosis factor-α (TNF-α) are key players in NF-κB pathway. Meanwhile, there is a furin-like cleavage site in SARS-CoV-2, which stimulates both NLRP3 and NF-κB inflammatory pathways.34 On the other side, with aging, the capacity for antigen recognition, production and activity of CD8+ T cells and NK cells are decreased. In our study, the CD3+ CD8+ T cells are decreased in older patients with AKI compared to non-AKI group and the relative younger patients. That would result in failing to eliminate the virus and induce cytokines released from CD4+ T effector cells which augment the inflammatory responses.35 As IL-6 and TNF-α were significantly increased in the AKI group, we speculate that cytokine storm in these patients leads to more severe injury and organ dysfunction.
In addition, multi-organ involvement has been documented since the emergence of COVID-19, such as lung, brain, heart, liver, and so on. There are increasing reports of persistent and prolonged effects after acute COVID-19 which will worsen the long-term outcomes.36 Consistent with these studies, our findings demonstrate that early interventions should be considered to prevent these potentially devastating complications of COVID-19.
It is well known that the main target of SARS-CoV-19 in kidney is the proximal tubules since the angiotensin converting enzyme 2 is expressed in the apical brush borders of the proximal tubules, that could mediate the entry of SARS-CoV-2 into epithelial cells and induce cytotoxicity.37,38 Along with these injuries, abundant erythrocytes were observed obstructing peritubular capillary lumens with ensuing endothelial damage, which indicated that endothelial dysfunction contributed to COVID-19-associated coagulopathy, characterized by increased D-dimer levels and microvascular damage. Besides D-dimer, Li and colleagues reported some other key factors in the coagulation pathway were elevated in COVID-19 patients, including factor III, von Willebrand factor, and SERPINE1.39 These findings are in accordance with our results that D-dimer is an essential risk factor of AKI with COVID-19.
There are several limitations in our study. Above all, our study was conducted in a single center which make the selection bias of extrapolation is inevitable. In addition, some risk factors, such as KIM-1, NGAL were not available during the pandemic. It would improve our predictive precision with these factors included. Thirdly, the specific causes of death for many patients have not been recorded; however, it is highly speculative that cardio-cerebrovascular diseases are the most common cause.
In conclusion, the incidence of AKI is increased among the geriatric COVID-19 patients. Therefore, we developed a predictive tool to improve the detection of AKI in elderly patients with this real-world data. Moreover, our findings demonstrated that AKI in COVID-19 may substantially affect the mid-term endpoints even after recovery of the renal function. Accordingly, awareness of kidney disease in elderly patients with COVID-19 needs to be emphasised among clinicians and maximizing the recovery of renal function should be the goal of AKI prevention and treatment strategy in COVID-19.
Acknowledgments
These studies were supported by National Natural Science Foundation of China (No.81870490 to P.Y., No.: 81870462, 82070789 to F.D.), Sponsored by Shanghai Pujiang Program (22PJ1409300 to P.Y), Shanghai Huangpu Industry Support Grant (XK2020002 to F.D.), Collaborative Innovation Center for Clinical and Translational Science by Chinese Ministry of Education & Shanghai (CCTS-2022206 to F.D.).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Cai J, Deng X, Yang J, et al. Modeling transmission of SARS-CoV-2 Omicron in China. Nat Med. 2022;28(7):1468–1475.
2. WHO Coronavirus (COVID-19) Dashboard. Available from: https://covid19.who.int/.
3. Cui Z, Liu P, Wang N, et al. Structural and functional characterizations of infectivity and immune evasion of SARS-CoV-2 Omicron. Cell. 2022;185(5):860–871 e13.
4. Iketani S, Liu L, Guo Y, et al. Antibody evasion properties of SARS-CoV-2 Omicron sublineages. Nature. 2022;604(7906):553–556.
5. Jingwen A, Wang X, Xinyi H, et al. Antibody evasion of SARS-CoV-2 Omicron BA.1, BA.1.1, BA.2, and BA.3 sub-lineages. Cell Host Microbe. 2022;30(8):1077–1083 e4.
6. Information Office of Shanghai Municipality. Shanghai reports on the prevention and control of COVID-19; 2022. Available from: https://www.shio.gov.cn/TrueCMS/shxwbgs/2022n_6y/2022n_6y.html.
7. Wolter N, Jassat W, Walaza S, et al. Early assessment of the clinical severity of the SARS-CoV-2 omicron variant in South Africa: a data linkage study. Lancet. 2022;399(10323):437–446.
8. Karunanithi S. Omicron and the NHS: we need to look beyond hospital care to solve the pressures. BMJ. 2022;376:o185.
9. Chan L, Chaudhary K, Saha A, et al. AKI in Hospitalized Patients with COVID-19. J Am Soc Nephrol. 2021;32(1):151–160.
10. Cheng Y, Luo R, Wang K, et al. Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney Int. 2020;97(5):829–838.
11. Ng JH, Hirsch JS, Hazzan A, et al. Outcomes Among Patients Hospitalized With COVID-19 and Acute Kidney Injury. Am J Kidney Dis. 2021;77(2):204–215 e1.
12. Kellum JA, Norbert Lameire PA, Barsoum RS, et al. Kidney disease: improving global outcomes (KDIGO) acute kidney injury work group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012;2(1):138.
13. Mehta RL, Burdmann EA, Cerdá J, et al. Recognition and management of acute kidney injury in the International Society of Nephrology 0by25 Global Snapshot: a multinational cross-sectional study. Lancet. 2016;387(10032):2017–2025.
14. Eckardt K-U, Kasiske BL. Kidney disease: improving global outcomes. Nat Rev Nephrol. 2009;5(11):650–657.
15. Macedo E, Hemmila U, Kumar Sharma S, et al. Recognition and management of community-acquired acute kidney injury in low-resource settings in the ISN 0by25 trial: a multi-country feasibility study. PLoS Med. 2021;18(1):e1003408.
16. Ostermann M, Bellomo R, Burdmann EA, et al. Controversies in acute kidney injury: conclusions from a Kidney Disease: improving Global Outcomes (KDIGO) Conference. Kidney Int. 2020;98(2):294–309.
17. NHCotPsRo C. Notice on printing and distributing the COVID-19 pneumonia diagnosis and treatment plan (ninth trial version) 2022; 2022. Available from: http://www.nhc.gov.cn/yzygj/s7653p/202203/b74ade1ba4494583805a3d2e40093d88.shtml.
18. D’ascanio M, Innammorato M, Pasquariello L, et al. Age is not the only risk factor in COVID-19: the role of comorbidities and of long staying in residential care homes. BMC Geriatr. 2021;21(1):63.
19. Hong X, Garcia-Ptacek S, Annetorp M, et al. Acute kidney injury and mortality risk in older adults with COVID-19. J Nephrol. 2021;34(2):295–304.
20. Scarpioni R, Valsania T, Albertazzi V, et al. Acute kidney injury, a common and severe complication in hospitalized patients during the COVID-19 pandemic. J Nephrol. 2021;34(4):1019–1024.
21. Lee JR, Silberzweig J, Akchurin O, et al. Characteristics of Acute Kidney Injury in Hospitalized COVID-19 Patients in an Urban Academic Medical Center. Clin J Am Soc Nephrol. 2021;16(2):284–286.
22. Fisher M, Neugarten J, Bellin E, et al. AKI in Hospitalized Patients with and without COVID-19: a Comparison Study. J Am Soc Nephrol. 2020;31(9):2145–2157.
23. Xia P, Wen Y, Duan Y, et al. Clinicopathological Features and Outcomes of Acute Kidney Injury in Critically Ill COVID-19 with Prolonged Disease Course: a Retrospective Cohort. J Am Soc Nephrol. 2020;31(9):2205–2221.
24. Lin L, Wang X, Ren J, et al. Risk factors and prognosis for COVID-19-induced acute kidney injury: a meta-analysis. BMJ Open. 2020;10(11):e042573.
25. Bell JS, James BD, Al-Chalabi S, et al. Community- versus hospital-acquired acute kidney injury in hospitalised COVID-19 patients. BMC Nephrol. 2021;22(1):269.
26. Pan Y, Wang W, Jinwei W, et al. Incidence and Risk Factors of in-hospital mortality from AKI after non-cardiovascular operation: a nationwide Survey in China. Sci Rep. 2017;7(1):13953.
27. Wainstein M, MacDonald S, Fryer D, et al. Use of an extended KDIGO definition to diagnose acute kidney injury in patients with COVID-19: a multinational study using the ISARIC-WHO clinical characterisation protocol. PLoS Med. 2022;19(4):e1003969.
28. Sherman RE, Anderson SA, Dal Pan GJ, et al. Real-World Evidence - What Is It and What Can It Tell Us? N Engl J Med. 2016;375(23):2293–2297.
29. Zhang N-H, Cheng Y-C, Luo R, et al. Recovery of new-onset kidney disease in COVID-19 patients discharged from hospital. BMC Infect Dis. 2021;21(1):397.
30. Huang C, Huang L, Wang Y, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet. 2021;397(10270):220–232.
31. Hua S, Yang M, Wan C, et al. Renal histopathological analysis of 26 postmortem findings of patients with COVID-19 in China. Kidney Int. 2020;98(1):219–227.
32. Shabnam Salimi M, John M, Hamlyn P. COVID-19 and Crosstalk With the Hallmarks of Aging. J Gerontol a Biol Sci Med Sci. 2020;75(9):e34–e41.
33. Wang W, Chen J, Xueqing Y, et al. Signaling mechanisms of SARS-CoV-2 Nucleocapsid protein in viral infection, cell death and inflammation. Int J Biol Sci. 2022;18(12):4704–4713.
34. Coutard B, Valle C, de Lamballerie X, et al. The spike glycoprotein of the new coronavirus 2019-nCoV contains a furin-like cleavage site absent in CoV of the same clade. Antiviral Res. 2020;176:104742.
35. van de Sandt CE, Bárcena M, Koster AJ, et al. Human CD8+ T Cells Damage Noninfected Epithelial Cells during Influenza Virus Infection In Vitro. Am J Respir Cell Mol Biol. 2017;57(5):536–546.
36. Nalbandian A, Sehgal K, Gupta A, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27(4):601–615.
37. Diao B, Wang C, Wang R, et al. Human kidney is a target for novel severe acute respiratory syndrome coronavirus 2 infection. Nat Commun. 2021;12(1):2506.
38. Vabret N, Britton GJ, Gruber C, et al. Immunology of COVID-19: current State of the Science [review]. Immunity. 2020;52(6):910–941.
39. Yijia L, Schneider AM, Mehta A, et al. SARS-CoV-2 viremia is associated with distinct proteomic pathways and predicts COVID-19 outcomes. J Clin Invest. 2021;131(13):e148635.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


