Back to Journals » Infection and Drug Resistance » Volume 15
Clinical Features and Outcomes of Spinal Tuberculosis in Central China
Authors Tang L , Fu CG, Zhou ZY, Jia SY, Liu ZQ, Xiao YX, Chen HD , Cai HL
Received 8 August 2022
Accepted for publication 3 November 2022
Published 11 November 2022 Volume 2022:15 Pages 6641—6650
DOI https://doi.org/10.2147/IDR.S384442
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Lei Tang,1,2,* Ce-Gang Fu,1,3,* Zhen-Yu Zhou,1,2 Si-Yu Jia,1 Zheng-Qiang Liu,1 Yun-Xiang Xiao,1 Hai-Dan Chen,1,2 Hui-Li Cai4
1Department of Spinal Surgery, Yichang Central People’s Hospital, China Three Gorges University, Yichang, People’s Republic of China; 2Graduate School, Ningxia Medical University, Yinchuan, People’s Republic of China; 3Department of Orthopedics, Haikou Orthopedic and Diabetes Hospital, Haikou Orthopedic and Diabetes Hospital of Shanghai Sixth People’s Hospital, Haikou, People’s Republic of China; 4Department of Hematology, Yichang Central People’s Hospital, China Three Gorges University, Yichang, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hai-Dan Chen, Department of Spinal Surgery, Yichang Central People’s Hospital, China Three Gorges University, 183 Yiling Road, Yichang, 443003, Hubei Province, People’s Republic of China, Tel +86 18086220025, Email [email protected] Hui-Li Cai, Department of Hematology, Yichang Central People’s Hospital, China Three Gorges University, 183 Yiling Road, Yichang, 443003, Hubei Province, People’s Republic of China, Email [email protected]
Purpose: The appropriate management of spinal tuberculosis (TB) is challenging for clinicians and the key to treat spinal TB. Surgery and long course anti-TB chemotherapy may not be necessary to all situations. This study aimed to characterize the clinical features and factors affecting treatment outcomes.
Patients and Methods: A retrospective study of patients with spinal TB over a 5-year period at a teaching hospital in central China was conducted. Features of patients with spinal TB who received different treatment modalities and factors associated with patient outcomes at the end of chemotherapy were analyzed.
Results: Forty-five patients (21 men and 24 women) with spinal TB were available for analysis. The mean age was 55.39 ± 14.94 years. The most common vertebral area involved was the lumbar (42.2%). The mean number of vertebrae involved was 2.20 ± 0.59. 27 patients (60.0%) received surgical treatment, of which 21 (77.8%) received radical surgical treatment. Thirty-five patients (77.8%) had achieved a favorable status. Statistically, there was no significant correlation between favorable status and surgery, but among 27 surgical patients with spinal tuberculosis, patients receiving radical surgery tended to achieve good prognosis (P = 0.010; odds ratio = 0.053; 95% confidence interval 0.006– 0.493). Moreover, there was no significant difference between long course and short course of anti-TB chemotherapy in prognosis in different treatment modalities.
Conclusion: Although the patients with spinal TB who needed surgical treatment often got a better prognosis when they had radical surgery, surgery was not actually a factor for the favorable outcomes of patients with spinal TB. In different treatment modalities, there was no additional benefit in longer anti-TB chemotherapy periods.
Keywords: surgical treatment, duration of anti-TB chemotherapy, retrospective study, outcome, spine, tuberculosis
Introduction
Spinal tuberculosis (TB), also referred to as Pott’s disease, was first modernly described by Percivall Pott in 1779.1,2 Bone and joint TB may account for 15–35% of patients with extrapulmonary TB, and for 1–5% of all cases of TB. Spinal TB accounts for approximately half of patients with bone and joint TB.3 The lower thoracic and the lumbar are the most commonly involved area. The most threatening complication of spinal tuberculosis is paraplegia, which can be onset early or late.4 Therefore, early diagnosis and treatment is the key to the treatment of spinal TB. However, the optimal treatment of spinal TB remains controversial, particularly surgical treatment and the duration of chemotherapy.5
In the past, 12–18 months of anti-TB chemotherapy were advocated for bone and joint TB.6 The prolonged anti-TB chemotherapy is likely to provoke the infection of drug-resistance Mycobacterium tuberculosis (MTB), interruption of treatment, or modification of the regimen during the chemotherapy. In addition, prolonged anti-TB chemotherapy may lead to decreasing patient compliance and increasing the difficulty of case supervision.7 More recently, some studies have shown that shorter anti-TB regimens than the standard are as effective as standard anti-TB regimens.8–10 Consequently, extensive attention has been given to shortening anti-TB chemotherapy to eliminate adverse consequences during tuberculosis management.11
Surgical treatment for spinal TB was proven to be effective,12–14 and some studies have shown that surgical treatment was a favorable factor for the prognosis of patients with spinal TB.15,16 And some studies advocated aggressive surgery for spinal TB.17 However, some studies reported that spinal TB patients with surgery or not had equally favorable outcome,18 This may imply that surgery may not be necessary to all situations.11,16,19
Due to these controversies regarding the surgical treatment and duration of anti-TB chemotherapy of spinal TB, we conducted a retrospective study at a teaching hospital over a 5-year period. This study aimed to determine the factors for favorable outcomes in patients with spinal TB, in terms of surgical treatment and duration of anti-TB chemotherapy in central China.
Materials and Methods
Study Design and Population
From January 1, 2016 to December 31, 2021, patients with a diagnosis of spinal TB were reviewed at a teaching hospital in Central China. Only patients older than 10 years with clinical evidence of spinal TB were included in the study.
A diagnosis of spinal TB was made in patients had one of the following criteria: (1) Patients had microbiologic or histopathological evidence (caseating granuloma or granulomatous inflammation with or without positive AFB smear) of TB infection; (2) Patients had typical radiographic or clinical features; (3) Patients had symptoms and signs compatible with spinal TB and a good reaction to anti-TB therapy. Exclusion criteria: (1) Irregular use of anti-TB drugs; (2) death from non-spinal TB; (3) still on treatment at the time of data analysis.
We collected the patient’s demographics, clinical features at presentation, laboratory results and radiographic findings, histological findings, microbiological results, treatment modality and anti-TB drugs used, duration of treatment, and patient outcome at the end of treatment. Then, we analyzed features of patients with spinal TB who received different treatment modalities and factors associated with patient outcomes at the end of chemotherapy.
Definitions
Based on the duration of anti-TB chemotherapy as triple therapy (isoniazid, rifampin, and ethambutol) or quadruple therapy (isoniazid, rifampin, pyrazinamide and ethambutol), the treatment duration was classified into two groups: (1) a short course defined of less than 12 months or equal to 12 months; (2) a long course defined of more than 12 months.
Patient outcome at the end of chemotherapy was classified into two groups: (1) favorable status: full physical activity at work, no evidence of central nervous system involvement, no remaining sinus or abscess that was clinically or radiologically detectable, and radiological evidence of healing of the spinal lesion; (2) unfavorable status: not radiographically quiescent, limited physical activity, clinically evident abscess or sinus present, myelopathy with functional impairment, a need for additional chemotherapy for spinal disease, or death associated with spinal disease.
Based on anti-TB chemotherapy, treatment was classified as non-surgery and surgery. (1) Surgery was defined as diagnostic operations, abscess drainage or curettage, debridement, anterior decompression, anterior or posterior stabilization with bone graft or instrumentation, vertebral curettage, laminectomy, and discectomy. (2) Non-surgery was defined as patient did not have surgery we defined above.
The type of surgical procedure was classified as radical or non-radical.16 (1) A radical surgery was defined as patient had vertebral curettage with or without decompression or bone fusion with instrumentation. (2) Nonradical surgery was defined as diagnostic operations, abscess drainage or curettage, debridement, anterior decompression, laminectomy, or discectomy et al.
Statistical Analysis
All statistical calculations were done using the SPSS version 15.0 (SPSS Inc., Chicago, IL, USA). P values were calculated using the x2 or Fisher exact test for categorical variables and by the Student t test for continuous variables. Odds ratio (OR) and 95% confidence intervals (CIs) were calculated for each variable by logistic regression analysis. Values of P < 0.05 were considered statistically significant.
Results
Baseline Characteristics
From January 1, 2016 to December 31, 2021, a 5-year period, 131 patients with bone and joint tuberculosis were admitted to our hospital and 51 patients with spinal TB were selected to follow-up, of which 6 were lost to irregular medication and non-tuberculosis causes of death in total and 45 were included in the analysis.
All 45 patients were available for assessment of end-of-treatment outcomes. All patients received antituberculosis chemotherapy, including 3 or 4 drugs containing isoniazid, rifampicin, pyrazinamide, and ethambutol. Demographic characteristics and clinical features of the 45 patients with spinal tuberculosis are shown in Table 1. There were 21 (46.7%) males and 24 (53.3%) females, with the mean age (± standard deviation [SD]) of 55.39 years (± 14.94). The most common vertebra involved was the lumbar (42.2%), followed by the thoracic (28.9%) and the lumbosacral (13.3%). The mean number of vertebra (± SD) involved was 2.20 (± 0.59). 84.4% of patients had one or two vertebrae involved. The other 15.6% of patients had 3 vertebrae involved or more. No patients had sinus. 24 patients (53.3%) had abscesses visible by Computed Tomography (CT) or Magnetic Resonance Imaging (MRI). 26 patients (57.8%) had symptoms of neurological compression. The mean duration of anti-TB chemotherapy (± SD) was 21.24 months (± 15.26) in 45 patients.
 |
Table 1 Demographic Characteristics and Clinical Features of Patients with Spinal TB |
Clinical Features in Different Treatment Modalities
Of the 45 patients with spinal tuberculosis, 27 (60.0%) underwent surgical treatment. The other 18 patients underwent non-surgical treatment. The clinical characteristics of surgical versus non-surgical patients with spinal TB are shown in Table 2. Surgical patients had more involvement of the lumbar (40.7% vs. 44.4%; P = 0.038; OR = 0.215; 95% CI 0.050–0.919), abscess (66.7% vs. 33.3%; P = 0.032; OR = 4.000; 95% CI 1.129–14.175) and neural compression (74.1% vs. 33.3%; P = 0.009; OR= 5.714; 95% CI 1.551–21.058).
 |
Table 2 Clinical Characteristics of Patients with Spinal TB with Surgery versus Non-Surgery |
Of the 27 surgical patients, 21 underwent radical surgical treatment. The other 6 patients underwent non-radical surgical treatment. The clinical characteristics of patients with spinal TB treated with non-radical surgery versus those treated with radical surgery are shown in Table 3. According to univariate logistic analysis, there was no statistical difference between radical surgical patients and non-radical surgical patients in terms of age (P = 0.062), radiologic site of lesion (P = 0.093), number of involved vertebrae (P = 0.303), duration of chemotherapy (P = 0.677), or symptoms of neural compression (P = 0.143).
 |
Table 3 Clinical Characteristics of Patients with Spinal TB Treated with Radical versus Nonradical Surgery |
At the end of chemotherapy, 16 patients were on the short course regimen. 29 patients were treated on the long course regimen. The clinical characteristics of patients on the short course regimen versus the long course regimen are shown in Table 4. There were no statistically significant differences in age (P = 0.603), surgery or not (P = 0.376), or surgical type (P = 0.677) in spinal TB patients with the long course regimen compared to the short one.
 |
Table 4 Clinical Characteristics of Patients with Short versus Long Course of Spinal TB |
Analysis of Outcome
The prognosis of the patients at the end of chemotherapy was compared, as shown in Table 5. 35 patients had a favorable outcome and 10 patients had an unfavorable outcome. Among patients with spinal TB had surgery, those with radical surgery had a significantly better outcome than those with non-radical surgery (P = 0.010; OR= 0.053; 95% CI 0.006–0.493). However, for all patients with spinal tuberculosis, there was no statistically significant difference in favorable outcome between surgical and non-surgical treatment (P = 1.000), nor in radiologic site of lesion (P = 0.378), number of vertebrae involved (P = 0.168), and duration of chemotherapy (P = 0.740).
 |
Table 5 Comparison of Prognosis of Patients with Spinal TB at the End of Antituberculosis Chemotherapy |
Multiple logistic regression analysis of 45 patients with spinal TB (Table 6) did not reveal any factor of favorable outcome in terms of age, sex, duration of chemotherapy, or whether surgery was performed. However, multivariate logistic regression analysis of 27 patients with spinal TB had surgical treatment (Table 7) suggested that the type of surgery was significantly associated with a favorable outcome (P = 0.033; OR= 0.052; 95% CI 0.003–0.786). In the surgical patients with spinal TB, the patients had radical surgery were used to have a favorable outcome, but surgery was not a factor of favorable outcome for all patients with spinal TB.
 |
Table 6 Logistic Regression Analysis of Variable Factors on Outcome of 45 Patients with Spinal TB |
 |
Table 7 Logistic Regression Analysis of Variable Factors on Outcome of 27 Surgical Patients with Spinal TB |
The analysis of the outcome in relation to the duration of chemotherapy and treatment modality is shown in Table 8. In the radical surgical treatment group, 9 patients received short-term chemotherapy and eight of them (88.9%) had a favorable outcome. 11 patients (91.7%) who received a long-term chemotherapy regimen also had a favorable outcome. However, there was no statistically significant difference between long and short courses under radical surgical treatment (P = 0.686). Similarly, there was no statistically significant difference between long and short courses under non-surgical (P = 0.701) and non-radical surgical treatment (P = 0.400). It indicates that there is no advantage in the long course of anti-tuberculosis treatment for patients with spinal TB in different treatment modalities.
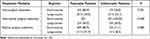 |
Table 8 Analysis of Patient Prognosis with Duration of Chemotherapy and Treatment Modality |
Discussion
In the present study, we characterized the clinical features of patients with spinal TB in different treatment modalities and analyzed the factors influencing the prognosis of patients with spinal TB. Surgical patients with spinal TB had more involvement of the lumbar, abscesses and neural compression, compared to non-surgical patients with spinal TB. But there was no statistical difference between radical and non-radical surgical patients with spinal TB, or short- and long-course regimen. As for outcome, the patients with spinal TB who needed surgical treatment often got a better prognosis when they had radical surgery. However, surgery is not actually a factor for the favorable outcomes of patients with spinal TB. And in different treatment modalities, there is no additional benefit in longer treatment periods.
In contrast to the approach of our study, which emphasized surgical type grouping (radical and non-radical surgery groups) in the retrospective study by Park et al16 and whether surgical treatment (drug-only and surgery-combined drug groups) in the retrospective study by Su et al,15 our study approach combined both grouping concepts and compared the groups separately in the spinal TB patients we studied. Besides, we expanded definition of radical surgery based on the study of Park et al. Because we believe that vertebral curettage is the key to radical surgery, not decompression or bone fusion. In the Korean findings, radical surgical patients with spinal TB were characterized by neurological compression symptoms and thoracic involved,16 Similarly, in our study, we also found surgical patients with spinal TB had symptoms of neural compression, but often accompanied by abscesses and more often involved in the lumbar, not thoracic. Furthermore, there were no significant differences in the clinical characteristics of patients with spinal TB in the duration of anti-TB chemotherapy and surgical type.
Surgery is an important adjunct to the treatment of spinal tuberculosis,20,21 but the necessity of surgical treatment for patients with spinal tuberculosis is controversial.22,23 Park et al16 retrospectively analyzed 137 patients with spinal TB and concluded that radical surgery combined with antituberculosis chemotherapy was a significant favorable prognostic factor. However, in a Cochrane review of randomized controlled trials, it believed there was no significant benefit to apply surgery in the treatment of spinal TB.18 And according to Zhang et al20 in their meta-analysis similarly concluded that surgery or not had no significant effect on the prognosis of patients with spinal TB. In the present study, we also believed surgery was not a favorable prognostic factor for patients with spinal TB, but we unexpectedly found the patients with spinal TB who needed surgical treatment often got a better prognosis when they had radical surgery. We speculate it may be an explanation for the controversy about whether surgery is a favorable prognostic factor for patients with spinal TB. By reason of surgical treatment of spinal TB exists to address complications, such as abscesses, nerve injuries, and spinal deformities.24,25 If patients do not have these complications or these complications can be managed by the organism, standardized anti-tuberculosis chemotherapy is the key to the treatment of spinal TB.26,27 On the other hand, if the organism is not able to manage these complications, the patient who choose radical surgery are more likely to have a favorable outcome.11 In clinical practice, it has a certain guiding role in the application of surgical treatment in spinal TB.
Antituberculosis chemotherapy remains the mainstay of treatment for spinal tuberculosis,28 but the duration of antituberculosis chemotherapy for patients with spinal tuberculosis has been heated one of the controversies.22,29 The definitions of long and short courses of anti-TB chemotherapy are not entirely consistent in different studies, which may result from the application of different anti-TB guidelines for different countries or regions. The American Thoracic Society recommends 6 months of anti-TB chemotherapy for adults and 12 months for children.30 The British Thoracic Society recommends daily use of rifampicin and isoniazid for 6 months.31 However, Chinese and Indian guidelines recommend a total course of anti-TB chemotherapy between 12 and 18 months.32,33 Recent studies also recommend at least 12 months of treatment for patients with spinal TB.33 Therefore, in our study, instead of setting the short course of anti-TB chemotherapy at 6 or 9 months,29,32,34 or even an ultra-short course of 3 months,35 as in other studies, the short course of treatment was set at less than or equal to 12 months. We believe this is more in line with the characteristics of the course of anti-TB treatment for Chinese patients under Chinese guidelines.
Efficacy of anti-TB chemotherapy has been validated, but long-term anti-TB chemotherapy leads to an increase in drug-resistant MTB and frequency of anti-TB drug side effects.19,33 Many studies have validated and explored the possibility of shortening the course of anti-TB chemotherapy,32,34,36 and the MRC study showed that the prognosis of patients treated with 6 or 9 months of antituberculosis chemotherapy was favorable and did not differ significantly from one of 18 months of antituberculosis treatment.11,37 However, it has also been suggested that 6 months of treatment may not be sufficient for the treatment of bone and joint TB, including spinal TB.33 In our results (Table 8), it was further suggested that short course (≤12 months) versus long course (>12 months) in patients with spinal TB was also not significantly associated in different treatment modalities.
However, we acknowledge the present study has several obvious limitations. First, it was a single-center retrospective study and the sample size was small. Some confounders, such as the change in the length of anti-TB chemotherapy, and practices of follow-up as mentioned above, could not be evaluated. Although there were significant differences in comparisons of several variables associated with outcome, the statistical power is adequate for drawing certain conclusions. Second, we enrolled cases not diagnosed by microbiology and histopathology, because of difficulty in diagnosis of TB, especially extrapulmonary TB. However, such cases were also enrolled in other studies.15,16 Third, we did not analyze the causes of unfavorable outcome such as the infection of drug-resistant MTB, In the present study, the patients involved in our study did not have the infection of drug-resistant MTB before the follow-up. We only evaluated the outcomes in the follow-up, and did not detect drug-resistant MTB in patients with unfavorable outcome. Hence, it needs more multi-center and well-designed studies to substantiate the present findings.
Conclusion
The present study demonstrated surgical treatment of spinal tuberculosis did not improve the clinical outcome of patients with spinal TB, but radical surgery improved the clinical outcome of patients who need surgery. And in different treatment modalities, there is no additional benefit in longer treatment periods. These findings suggested the directions to application of operation in patients with spinal TB and feasibility of shortening the course of anti-TB chemotherapy in different treatment modalities, which need to be verified by more studies.
Abbreviations
TB, Tuberculosis; MTB, Mycobacterium tuberculosis; CT, Computed Tomography; MRI, Magnetic Resonance Imaging; SD, standard deviation; OR, Odds ratio; CIs or CI, confidence intervals.
Patient Consent and Ethics Statement
This project was approved by the Ethics Committee of Yichang Central People’s Hospital (202112401). The need to obtain individual informed consent was waived for this study utilized existing data collected from the hospital information system and did not pose any additional risks to the patients. The study was conducted in accordance with the Declaration of Helsinki.
Funding
This study received no funding.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Tuli SM. Tuberculosis of the spine: a historical review. Clin Orthop Relat Res. 2007;460:29–38. doi:10.1097/BLO.0b013e318065b75e
2. Wang B, Wang Y, Hao D. Current study of medicinal chemistry for treating spinal tuberculosis. Curr Med Chem. 2021;28(25):5201–5212. doi:10.2174/0929867328666201222125225
3. Davies PD, Humphries MJ, Byfield SP, et al. Bone and joint tuberculosis. A survey of notifications in England and Wales. J Bone Joint Surg Br. 1984;66(3):326–330. doi:10.1302/0301-620X.66B3.6427232
4. Moon MS, Moon JL, Moon YW, et al. Pott’s paraplegia in patients with severely deformed dorsal or dorsolumbar spines: treatment and prognosis. Spinal Cord. 2003;41(3):164–171. doi:10.1038/sj.sc.3101366
5. Nene A, Bhojraj S. Results of nonsurgical treatment of thoracic spinal tuberculosis in adults. Spine J. 2005;5(1):79–84. doi:10.1016/j.spinee.2004.05.255
6. Nussbaum ES, Rockswold GL, Bergman TA, Erickson DL, Seljeskog EL. Spinal tuberculosis: a diagnostic and management challenge. J Neurosurg. 1995;83(2):243–247. doi:10.3171/jns.1995.83.2.0243
7. Sun G, Wang Q, Liang Q, et al. Clinical efficacy and safety of ultra-short-course chemotherapy in treatment of spinal tuberculosis after complete debridement: an observational study. J Int Med Res. 2021;49(2):300060520967611. doi:10.1177/0300060520967611
8. Merle CS, Fielding K, Sow OB, et al. A four-month gatifloxacin-containing regimen for treating tuberculosis. N Engl J Med. 2014;371(17):1588–1598. doi:10.1056/NEJMoa1315817
9. Darbyshire J. Controlled trial of short-course regimens of chemotherapy in the ambulatory treatment of spinal tuberculosis. Results at three years of a study in Korea. Twelfth report of the Medical research council working party on tuberculosis of the spine. J Bone Joint Surg Br. 1993;75(2):240–248. doi:10.1302/0301-620X.75B2.8444944
10. Nene AM, Patil S, Kathare AP, Nagad P, Nene A, Kapadia F. Six versus 12 months of anti tubercular therapy in patients with biopsy proven spinal tuberculosis: a single center, open labeled, prospective randomized clinical trial-A pilot study. Spine. 2019;44(1):E1–E6. doi:10.1097/BRS.0000000000002811
11. Pandita A, Madhuripan N, Pandita S, Hurtado RM. Challenges and controversies in the treatment of spinal tuberculosis. J Clin Tuberc Other Mycobact Dis. 2020;19:100151. doi:10.1016/j.jctube.2020.100151
12. Luan H, Liu K, Wang Y, et al. Efficacy of anterior debridement and bone grafting with fusion using internal fixation combined with anti-tuberculosis chemotherapy in the treatment of subaxial cervical tuberculosis. BMC Surg. 2022;22(1):150. doi:10.1186/s12893-022-01606-y
13. Bai J, Xia Q, Miao J. Combined anteroposterior approaches in lateral position treatment of lumbosacral tuberculous in single-stage. BMC Surg. 2022;22(1):154. doi:10.1186/s12893-022-01612-0
14. Du X, Ou Y, Luo W, Jiang G, Qin W, Zhu Y. Evaluation of the efficacy of OLIF combined posterior internal fixation for single-segment lumbar tuberculosis: a single-center retrospective cohort study. BMC Surg. 2022;22(1):54. doi:10.1186/s12893-022-01492-4
15. Su SH, Tsai WC, Lin CY, et al. Clinical features and outcomes of spinal tuberculosis in southern Taiwan. J Microbiol Immunol Infect. 2010;43(4):291–300. doi:10.1016/S1684-1182(10)60046-1
16. Park DW, Sohn JW, Kim EH, et al. Outcome and management of spinal tuberculosis according to the severity of disease: a retrospective study of 137 adult patients at Korean teaching hospitals. Spine. 2007;32(4):E130–135. doi:10.1097/01.brs.0000255216.54085.21
17. Chen WJ, Chen CH, Shih CH. Surgical treatment of tuberculous spondylitis. 50 patients followed for 2–8 years. Acta Orthop Scand. 1995;66(2):137–142. doi:10.3109/17453679508995507
18. Jutte PC, van Loenhout-Rooyackers JH. Routine surgery in addition to chemotherapy for treating spinal tuberculosis. Cochrane Database Syst Rev. 2006;5:CD004532. doi:10.1002/14651858.CD004532.pub2
19. Zhang Z, Luo F, Zhou Q, Dai F, Sun D, Xu J. The outcomes of chemotherapy only treatment on mild spinal tuberculosis. J Orthop Surg Res. 2016;11(1):49. doi:10.1186/s13018-016-0385-y
20. Zhang X, Ji J, Liu B. Management of spinal tuberculosis: a systematic review and meta-analysis. J Int Med Res. 2013;41(5):1395–1407. doi:10.1177/0300060513498023
21. Waheed G, Soliman M, Ali AM, Aly MH. Spontaneous spondylodiscitis: review, incidence, management, and clinical outcome in 44 patients. Neurosurg Focus. 2019;46(1):E10. doi:10.3171/2018.10.FOCUS18463
22. Medical Research Council Working Party on Tuberculosis of the Spine. A controlled trial of six-month and nine-month regimens of chemotherapy in patients undergoing radical surgery for tuberculosis of the spine in Hong Kong. Tenth report of the medical research council working party on tuberculosis of the spine. Tubercle. 1986;67(4):243–259. doi:10.1016/0041-3879(86)90014-0
23. Shembekar A, Babhulkar S. Chemotherapy for osteoarticular tuberculosis. Clin Orthop Relat Res. 2002;398:20–26. doi:10.1097/00003086-200205000-00004
24. Sae-Jung S, Wongba N, Leurmprasert K. Predictive factors for neurological deficit in patients with spinal tuberculosis. J Orthop Surg. 2019;27(3):2309499019868813. doi:10.1177/2309499019868813
25. Reisener MJ, Pumberger M, Shue J, Girardi FP, Hughes AP. Trends in lumbar spinal fusion-a literature review. J Spine Surg. 2020;6(4):752–761. doi:10.21037/jss-20-492
26. Bakhsh A. Medical management of spinal tuberculosis: an experience from Pakistan. Spine. 2010;35(16):E787–791. doi:10.1097/BRS.0b013e3181d58c3c
27. Lan X, Xu JZ, Luo F, Liu XM, Ge BF. 脊柱结核术后复发原因分析及再手术疗效观察 [Analysis of postoperative recurrence reason and observation of reoperation outcome for spinal tuberculosis]. Zhongguo Gu Shang. 2013;26(7):536–542. Chinese.
28. Divya A, Shukla DP, Bahubali VH, et al. Consumption of spine by tuberculosis in the era of directly observed treatment, short-course and genomic diagnosis. Indian J Tuberc. 2021;68(1):73–79. doi:10.1016/j.ijtb.2020.08.017
29. Lin L, Ke Z, Cheng S. Efficacy and safety of short-term chemotherapy for patients with spinal tuberculosis undergoing surgery in Chinese population: a meta-analysis. J Orthop Surg Res. 2021;16(1):229. doi:10.1186/s13018-021-02375-9
30. Joint T. Chemotherapy and management of tuberculosis in the United Kingdom: recommendations 1998. Joint Tuberculosis Committee of the British Thoracic Society. Thorax. 1998;53(7):536–548.
31. Sharma SK, Ryan H, Khaparde S, et al. Index-TB guidelines: guidelines on extrapulmonary tuberculosis for India. Indian J Med Res. 2017;145(4):448–463. doi:10.4103/ijmr.IJMR_1950_16
32. Ramachandran S, Clifton IJ, Collyns TA, Watson JP, Pearson SB. The treatment of spinal tuberculosis: a retrospective study. Int J Tuberc Lung Dis. 2005;9(5):541–544.
33. Khanna K, Sabharwal S. Spinal tuberculosis: a comprehensive review for the modern spine surgeon. Spine J. 2019;19(11):1858–1870. doi:10.1016/j.spinee.2019.05.002
34. Park CS, Lee JY, Choi HY, et al. Gallic acid attenuates blood-spinal cord barrier disruption by inhibiting Jmjd3 expression and activation after spinal cord injury. Neurobiol Dis. 2020;145:105077. doi:10.1016/j.nbd.2020.105077
35. Qiao J, Yang L, Feng J, Dai X, Xu F, Xia P. Analysis of efficacy and safety of linezolid-based chemotherapeutic regimens for patients with postoperative multidrug-resistant spinal tuberculosis. Int J Infect Dis. 2022;118:264–269. doi:10.1016/j.ijid.2022.03.020
36. van Loenhout-Rooyackers JH, Verbeek AL, Jutte PC. Chemotherapeutic treatment for spinal tuberculosis. Int J Tuberc Lung Dis. 2002;6(3):259–265.
37. Darbyshire J. Five-year assessment of controlled trials of short-course chemotherapy regimens of 6, 9 or 18 months’ duration for spinal tuberculosis in patients ambulatory from the start or undergoing radical surgery. Fourteenth report of the Medical Research Council Working Party on Tuberculosis of the Spine. Int Orthop. 1999;23(2):73–81. doi:10.1007/s002640050311
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
