Back to Journals » Journal of Pain Research » Volume 16
Clinical Efficacy Evaluation of Ultrasound-Guided C2 Dorsal Root Nerve Pulsed Radiofrequency Combined with Stellate Ganglion Block in the Treatment of Cervicogenic Headache: A Retrospective Cohort Study
Authors Hua L, Sha K , Lu H, Han Y , Ou C , Wang JL , Zhang Y
Received 28 March 2023
Accepted for publication 26 July 2023
Published 28 July 2023 Volume 2023:16 Pages 2655—2663
DOI https://doi.org/10.2147/JPR.S409226
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Alexandre F DaSilva
Lu Hua,1,2,* Kaiyuan Sha,1,2,* HongCheng Lu,1,2 Ying Han,1,2 Cehua Ou,1,2 Jiang-Lin Wang,1 Yue Zhang1,2
1Department of Pain Management, The Affiliated Hospital of Southwest Medical University, Luzhou, People’s Republic of China; 2Anesthesiology and Critical Care Medicine Key Laboratory of Luzhou Southwest Medical University, Luzhou, Sichuan Province 646000 People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jiang-Lin Wang; Yue Zhang, Department of Pain Management, The Affiliated Hospital of Southwest Medical University, Luzhou, People’s Republic of China, Email [email protected]; [email protected]
Purpose: To explore the therapeutic effect of C2 dorsal root ganglion pulsed radiofrequency (PRF) combined with stellate ganglion block (SGB) in patients with cervicogenic headache (CEH).
Patients and Methods: We retrospectively reviewed 90 patients diagnosed with CEH who were admitted to our hospital between May 2019 and May 2022. All patients were divided into three groups (n = 30 each) according to the actual treatment method used: ultrasound-guided SGB, ultrasound-guided C2 dorsal root ganglion PRF treatment, and ultrasound-guided C2 dorsal root ganglion PRF combined with SGB treatment. Patients’ pain intensity, sleep, and mood changes were assessed by statistically analyzing their pain visual analog scale (VAS), Pittsburgh Sleep Quality Inventory (PSQI), and short-form McGill Pain Questionnaire affective item scores before and after treatment.
Results: The post-treatment VAS, PSQI, and McGill scores were significantly decreased in all patients (P < 0.05), and all three scores in ultrasound-guided C2 dorsal root ganglion PRF combined with SGB were lower than those in ultrasound-guided SGB alone and ultrasound-guided C2 dorsal root ganglion PRF alone (P < 0.05).
Conclusion: The use of ultrasound-guided C2 dorsal root ganglion PRF combined with SGB in patients with CHE is effective in alleviating pain and improving sleep, and deserves to be replicated in the clinic.
Keywords: cervicogenic headache, C2 dorsal root ganglion, pulsed radiofrequency, stellate ganglion block
Introduction
Cervicogenic headache (CEH) refers to head pain that arises from organic or functional lesions in the neck; the pain is often predominant in the unilateral cervical-occipital region and may be accompanied by pain in the frontal and temporal regions.1 With changes in people’s lifestyles, the number of patients with CEH is increasing.2 The International Headache Society stated that the prevalence of CEH is 2.2% in the healthy population and 15–20% in headache sufferers.3 Although the pathogenesis of CEH is unclear, it is considered to be due to pathological changes in the synovial joints of the upper cervical spine with disorders of the superior cervical nerve (C1-C3).4 Currently, CEH has many treatment options, including pharmacological treatment, scalpel treatment, acupuncture treatment, nerve block treatment, pulsed radiofrequency (PRF) treatment, and cervical surgery.4,5 Surgical treatment is generally not recommended unless CEH is refractory and conservative treatment is ineffective. Therefore, patients with CEH who are not well treated with medication alone can be treated with nerve blocks and PRF. PRF acts as a modulator of the nerve by delivering high-intensity pulses. Studies have shown that ultrasound-guided PRF of the C2 dorsal root nerve combined with nerve block therapy has good efficacy for CEH.6,7 Stellate ganglion block (SGB) can improve head and facial pain, potentially via the improvement of blood flow due to direct blockade of afferent nociceptive impulses through sympathetic pathways.8 SGB is also widely recognized in the prevention and treatment of CEH.9 However, whether the two have synergistic effects for better treatment of CEH remains unknown. Therefore, we explored the effectiveness of ultrasound-guided C2 dorsal root ganglion PRF combined with SGB in the treatment of CEH.
Materials and Methods
The study was clinically ethically registered in the University Medical Research Archive Registry and approved by the Clinical Trials Ethics Committee of the Affiliated Hospital of Southwestern Medical University (Grant No. KY2023011). Because this study is retrospective, the Clinical Trials Ethics Committee specifically waived the requirement for informed consent. All methods in the study were carried out in accordance with the Helsinki guidelines and declaration. This is a retrospective cohort study comprising 90 patients diagnosed with CEH in the pain department of the Affiliated Hospital of Southwest Medical University from May 2020 to May 2022. We collected basic information, including gender, age, weight, and duration of disease, of the patients through the electronic medical file.
Study Design and Participants
The inclusion criteria were: (1) all patients were diagnosed in accordance with the diagnostic criteria for CEH established in ICHD-3;10 (2) pharmacological treatment alone is ineffective in accordance with the expert consensus of the Chinese Medical Association’s pain division;4 (3) patients had completed the treatment protocol set in this study and co-operated with follow-up. The exclusion criteria were: (1) patients whose actual treatment regimen did not meet or did not fully comply with the setting of this study; (2) patients who were lost to follow-up; (3) patients with cognitive impairment and unclear language expression. After screening according to the inclusion and exclusion criteria, the patients were divided into three groups according to their actual treatment modality: ultrasound-guided SGB treatment group (group A), ultrasound-guided C2 dorsal root PRF treatment group (group B), and ultrasound-guided C2 dorsal root PRF + SGB treatment group (group C).
Procedures
Ultrasound-Guided Stellate Ganglion Block (Group A)
Patients were placed in a supine position with a thin pillow behind the neck and face turned to the opposite side to fully expose the neck. A high-frequency probe was selected for scanning to the level of the (C6/C7) transverse process, and the common carotid artery, internal jugular vein, and longus colli muscle were identified as the stellate ganglion with a slightly thickened moderate to strong echo in the inferior lateral aspect of the common carotid artery and anterior medial aspect of the longissimus dorsi (as shown in Figure 1). After routine disinfection and spreading of the towel, the in-plane approach was chosen, and care was taken to avoid the adjacent vessels. After breaking through the prevertebral fascia, the blood was retracted, 5 mL of 1% lidocaine was slowly injected, and the drug was spread between the long carotid muscle and the carotid artery. The patient was then observed for Horner syndrome manifestations such as ipsilateral pupil narrowing and eyelid ptosis, and complications such as hoarseness and numbness of the upper limbs. The treatment cycle was once a day for 10 consecutive days.
Ultrasound-Guided C2 Dorsal Root Ganglion Pulsed Radiofrequency (Group B)
Patients were positioned in lateral recumbency, the neck and posterior occipital region were fully exposed (the occipital area needed to be prepared with skin), and the towel was routinely disinfected. A low-frequency probe was selected for longitudinal scanning, and bony structures such as occipital bone, C2 spinous process, and C3 spinous process were observed. The probe was rotated, and the two ends of the probe were placed at the position of the C2 spinous process and the C1 transverse process, respectively. The inferior oblique muscle of the head, vertebral artery, and spinal cord were fully exposed, and 1% lidocaine local anesthesia was administered slowly through an in-plane puncture into the needle (radiofrequency set needle cervical segment length was 10 cm and the bare end was 5 mm). The needle tip was accurately positioned at the target site (as shown in Figure 2) after conducting a radiofrequency sensory test at 50 Hz and 0.4 V or less and testing for induction of the original pain area hyperesthesia. After determining the target location, the PRF was conducted at 2 Hz and 1 V or less (which did not induce local muscle twitching) as follows: 2 cycles at 40 °C for 180 s, and 2 cycles at 42 °C for 180 s. After the PRF procedure, 3 mL of a compound solution (2 mL of 2% lidocaine + 0.5 mg methylcobalamin + 5 mg dexamethasone + saline added to make the total volume 10 mL) was injected into the target area. The treatment cycle was once every three days, twice for a course of treatment.
Ultrasound-Guided C2 Dorsal Root Nerve Pulsed Radiofrequency Combined with Stellate Ganglion Block (Group C)
The treatment mode was as described above. The treatment cycle comprised SGB treatment once a day for 10 days and C2 dorsal root ganglion PRF performed once every three days, two times for a course of treatment.
Clinical Assessment
The relevant scores before and after treatment were obtained from the patient’s respective supervising physician’s medical records and follow-up records. The scores assessed included the visual analog scale (VAS) of pain before and at 1 week, 1 month, 3 months, and 6 months after treatment, Pittsburgh sleep quality index (PSQI) score, and McGill Pain Questionnaire affective item scores.
Statistical Analysis
Statistical software R system for statistical computing (R Core Team 2022, version 4.1.1) was used for data analysis and description. Data are expressed as the mean ± standard deviation. As PSQI, VAS, and McGill scores were repeatedly measured before treatment and post-treatment, a linear mixed model was used to detect the interaction and within-group effect. One-way analysis of variance (ANOVA) and post-hoc Tukey’s test were used to compare the average PSQI, VAS, and McGill scores between groups A, B, and C within each time point. P-values < 0.05 were interpreted as statistically significant differences.
Results
Characteristics of the Included Patients
A total of 90 patients were included in the final analysis with an average age of 44.02 ± 8.77 years. Among the patients, 55 (61.1%) were male and 45 (38.9%) were female. There was no significant difference in the basic characteristics between the groups (Table 1).
 |
Table 1 Comparison of Basic Characteristics Between Groups |
Pain Assessment
The interaction effect between time and group was significant (t = −3.976, P < 0.001). The post-treatment VAS scores significantly descended at week 1, month 1, month 3, and month 6 in all patients (P < 0.05). The post-treatment VAS scores at each time point were lower in group C compared to those in groups A and B (P < 0.05) (Table 2 and Figure 3).
 |
Table 2 Comparison of Visual Analog Scale Scores Between Groups at Each Time Point |
 |
Figure 3 The comparison of visual analog scale (VAS) scores between groups at each time point. |
PSQI Scores
Results from the linear mixed model demonstrated that the interaction effect between time and group was significant (t = 2.070, P = 0.039 for the time and group B interaction, and t = −1.986, P = 0.048 for the time and group C interaction). Furthermore, the time-dependent trend for the PSQI scores is different between groups A, B, and C. Group A had lower PSQI scores than groups B and C at 3 months and 6 months post-treatment. In groups A and B, except for the comparison between 1 month post-treatment and 1 week post-treatment, all the remaining comparisons between time points showed significant differences. In group C, The PSQI score at each time point after treatment was lower than the PSQI score at the corresponding time point before treatment. (Table 3 and Figure 4).
 |
Table 3 The Comparison of Pittsburgh sleep quality index Between Groups at Each Time Point |
 |
Figure 4 The comparison of Pittsburgh Sleep Quality Index (PSQI) scores between groups at each time point. |
McGill Scores
The interaction effect between time and group was significant (t = −3.414, P = 0.001 for the time and group C). Furthermore, significant differences in McGill scores were detected between groups at 1 month, 3 months, and 6 months post-treatment. In within-group comparison, except for the comparison between 1 month post-treatment vs 1 week post-treatment, all the remaining comparisons between time points showed significant differences in groups A and B. In group C, the post-treatment McGill scores at each time point were lower than that at the previous time point (Table 4 and Figure 5).
 |
Table 4 The Comparison of McGill Scores Between Groups at Each Time Point |
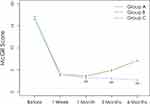 |
Figure 5 The comparison of McGill scores between groups at each time point. |
No major complications occurred in all patients in this retrospective study.
Discussion
The World Health Organization ranks headaches as one of the top 10 disabling diseases in the world, having serious adverse physical, psychological, and social effects on patients.11 Among the more common secondary headaches, CEH is a chronic headache caused by mechanical compression of the cervical spine and related soft tissues and other pathological factors. In CEH, neck and occipital pain are more common, while some patients may also show forehead and temporal pain.10 The prevalence of CEH in the general population is uncertain and varies according to the diagnostic criteria used. CEH accounts for 17.8% of all severe headaches.12 It is considered that CEH may be caused by pathological changes in the articular process of the upper cervical vertebra, leading to the disorder of the superior cervical nerve (C1-C3). The pathophysiological mechanism leading to subsequent pain is complex and may be closely related to inflammatory edema, nerve convergence, mechanical stimulation, central sensitization, sympathetic nerve, and other mechanisms. Thus, CEH is caused by the interaction of various mechanisms. Long-term chronic persistent pain can seriously affect the quality of life of patients, and even lead to emotional changes such as anxiety and depression. Pain and emotions interact with each other, resulting in a vicious circle.13 The treatment of CHE mainly includes drug therapy, nerve block, minimally invasive intervention, and cervical surgery. With the development of technology, minimally invasive treatment such as PRF has gradually become the mainstream.6
It is considered that CEH may be caused by pathological changes in the articular process of the upper cervical vertebra, leading to the disorder of the superior cervical nerve (C1-C3). The pathophysiological mechanism leading to subsequent pain is complex and may be closely related to inflammatory edema, nerve convergence, mechanical stimulation, central sensitization, sympathetic nerve, and other mechanisms. Studies have shown that the C2 dorsal root ganglion is the most easily stimulated nerve, from which it can be inferred that the C2 dorsal root ganglion is closely related to the occurrence of CEH.10 The DRG is the site of aggregation of primary pseudomonopolar neuronal cells associated with somatic and visceral nociceptive transmission, and it plays an important role in the transmission and processing of sensory signals.14 Furthermore, the DRG is relatively easy to be approached anatomically and is a more commonly used therapeutic target for CEH.14 Studies have shown that nerve block therapy of the C2 dorsal heel ganglion can treat a variety of headaches15 and is also effective for CEH.16 However, nerve block therapy is only effective in the short term and is not durable. In contrast, PRF therapy can have a long-term effect on patients with CEH. PRF uses high-frequency current to generate a magnetic field, which can activate the brainstem downstream inhibitory system, inhibit the injurious sensory afferents of class C nerve fibers, regulate the activity of inflammatory factors, and activate substances such as neurotrophic factors to produce long-lasting pain relief. Concurrently, C2 dorsal root ganglion PRF can relieve the muscle spasm of the posterior cervical region, improve blood circulation, and reduce the symptoms caused by nerve entrapment. Moreover, PRF does not cause radiofrequency destruction as its needle tip temperature generally does not exceed 42 °C; thus, PRF mainly plays a regulatory role on nerves without causing any permanent damage and thermal injury to neurons.17
SGB is a sympathetic ganglion located in the neck and is closely related to the regulation of immune, endocrine, and vegetative functions of the body. SGB mainly refers to cervicothoracic sympathetic ganglion block, thus achieving the effect of blocking preganglionic and postganglionic nerve fibers and cervical sympathetic trunk and its innervated head and neck blood vessels, sweat glands, and many other organs.18 Long-term poor lifestyle habits predispose an individual to muscle spasms in the neck, poor local blood circulation, and aseptic inflammation. The accumulation of inflammatory factors leads to the production and release of painful substances, which cause stiffness and pain in the head and neck, forming a vicious cycle of “headache-muscle ischemia-inflammatory substance accumulation-headache”. SGB improves cervicogenic pain by improving blood circulation in the head and neck, relieving muscle tension, and increasing the efficiency of sterile inflammation and other mediators without affecting cerebral perfusion and cerebral regulation.19,20
Our study demonstrates that the use of ultrasound-guided C2 dorsal root ganglion PRF combined with SGB was more effective in improving pain, sleep, and mood in patients with CHE, with effects lasting longer than with C2 dorsal root ganglion PRF alone or SGB alone. The strengths of our study are that it carried out a structured evaluation and follow-up of patients by the same physician and there were no losses to follow-up. To the best of our knowledge, this study will be the first to investigate the efficacy of ultrasound-guided C2 dorsal root ganglion PRF combined with SGB in patients with CHE. However, our study also has some limitations. First, it comprised a small sample size, and future studies with a larger cohort should be carried out. Second, our study only followed patients for 6 months. A longer follow-up can provide insights into the long-term outcomes and effects of the combined treatment in patients with CHE. Addressing these limitations can better guide clinical practice.
Conclusion
Patients’ pain intensity, sleep, and mood changes were assessed by statistically analyzing their VAS, PSQI, and McGill scores before and after treatment. Our results suggest that the use of ultrasound-guided cervical 2 dorsal root ganglion PRF combined with SGB in patients with CHE is more effective in improving pain, sleep, and mood and deserves to be replicated in the clinic.
Ethics Approval and Informed Consent
The study was clinically ethically registered in the University Medical Research Archive Registry and approved by the Clinical Trials Ethics Committee of the Affiliated Hospital of Southwestern Medical University (Grant No. KY2023011). Because this study is retrospective, the Clinical Trials Ethics Committee specifically waived the requirement for informed consent. All methods in the study were carried out in accordance with the Helsinki guidelines and declaration.
Acknowledgment
We thank the patients who enrolled in this study.
Funding
This study was supported by a grant from the Natural Science Foundation of Sichuan Province (No. 2022NSFSC1479), the joint foundation of the Luzhou government and Southwest Medical University (No. 2021LZXNYD-J29), strategic cooperation project between Hejiang County People’s Government and Southwest Medical University (No. 2020-HJXNYD-4).
Disclosure
The authors declare that they have no conflict of interest.
References
1. Sjaastad O, Saunte C, Hovdahl H, et al. ”Cervicogenic” headache. An hypothesis. Cephalalgia. 1983;3(4):249–256. doi:10.1046/j.1468-2982.1983.0304249.x
2. Xu Y, Gao Y, Jiang L, et al. Global trends in research on cervicogenic headache: a bibliometric analysis. Front Neurol. 2023;14:1169477. doi:10.3389/fneur.2023.1169477
3. Svensson J, Hermansen A, Wibault J, et al. Neck-related headache in patients with cervical disc disease after surgery and physiotherapy: a 1-year follow-up of a prospective randomized study. Spine. 2020;45(14):952–959. doi:10.1097/BRS.0000000000003430
4. Xiao H, Peng B, Ma K, et al. The Chinese Association for the Study of Pain (Casp): expert consensus on the cervicogenic headache. Pain Res Manag. 2019;2019:9617280. doi:10.1155/2019/9617280
5. Raposio G, Raposio E. Principles and techniques of migraine surgery. Eur Rev Med Pharmacol Sci. 2022;26:6110–6113. doi:10.26355/eurrev_202209_29628
6. Lee H-J, Cho H, Nahm S, et al. Pulsed radiofrequency ablation of the C2 dorsal root ganglion using a posterior approach for treating cervicogenic headache: a retrospective chart review. Headache. 2020;60(10):2463–2472. doi:10.1111/head.13759
7. Wu B, Yue L, Sun F, et al. The feasibility and efficacy of ultrasound-guided C2 nerve root coblation for cervicogenic headache. Pain Med. 2019;20(6):1219–1226. doi:10.1093/pm/pny227
8. Noma N, Kamo H, Nakaya Y, et al. Stellate ganglion block as an early intervention in sympathetically maintained headache and orofacial pain caused by temporal arteritis. Pain Med. 2013;14(3):392–397. doi:10.1111/pme.12040
9. Goldberg ME, Schwartzman RJ, Domsky R, et al. Deep cervical plexus block for the treatment of cervicogenic headache. Pain Phys. 2008;11(6):849–854. doi:10.36076/ppj.2008/11/849
10. Olesen J. Headache classification committee of the International Headache Society (IHS) the international classification of headache disorders, 3rd edition. Cephalalgia. 2018;38(1):1–211.
11. Stovner L, Hagen K, Jensen R, et al. The global burden of headache: a documentation of headache prevalence and disability worldwide. Cephalalgia. 2007;27(3):193–210. doi:10.1111/j.1468-2982.2007.01288.x
12. Evers S. Comparison of cervicogenic headache with migraine. Cephalalgia. 2008;28(Suppl 1):16–17. doi:10.1111/j.1468-2982.2008.01609.x
13. Juang KD, Yang C-Y. Psychiatric comorbidity of chronic daily headache: focus on traumatic experiences in childhood, post-traumatic stress disorder and suicidality. Curr Pain Headache Rep. 2014;18(4):405. doi:10.1007/s11916-014-0405-8
14. Berger A, Liu Y, Possoit H, et al. Dorsal root ganglion (Drg) and chronic pain. Anesthesiol Pain Med. 2021;11(2):e113020. doi:10.5812/aapm.113020
15. Lim HB, Hunt K. Anesthetic management for surgical placement of greater occipital nerve stimulators in the treatment of primary headache disorders. J Neurosurg Anesthesiol. 2007;19(2):120–124. doi:10.1097/ANA.0b013e31802ba10f
16. Naja M, El-Rajab M, Al-Tannir MA, et al. Occipital nerve blockade for cervicogenic headache: a double-blind randomized controlled clinical trial. Pain Pract. 2006;6(2):89–95. doi:10.1111/j.1533-2500.2006.00068.x
17. Van Zundert J, Lamé E, De Louw A, et al. Percutaneous pulsed radiofrequency treatment of the cervical dorsal root ganglion in the treatment of chronic cervical pain syndromes: a clinical audit. Neuromodulation. 2003;6(1):6–14. doi:10.1046/j.1525-1403.2003.03001.x
18. Narouze S. Ultrasound-guided stellate ganglion block: safety and efficacy. Curr Pain Headache Rep. 2014;18(6):424. doi:10.1007/s11916-014-0424-5
19. Lipov E, Gluncic V, Lukić K, et al. How does stellate ganglion block alleviate immunologically-linked disorders? Med Hypotheses. 2020;144:110000. doi:10.1016/j.mehy.2020.110000
20. T-T L, Wan Q, Zhang X, et al. Stellate ganglion block reduces inflammation and improves neurological function in diabetic rats during ischemic stroke. Neural Regen Res. 2022;17(9):1991–1997. doi:10.4103/1673-5374.335162
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


