Back to Journals » Orthopedic Research and Reviews » Volume 15
Clinical Effects of the End-Love Technique in the Treatment of Recurrent Lumbar Disc Herniation 1 Year After Surgery
Authors Li P, Li X, Ma L, He HY
Received 18 September 2023
Accepted for publication 9 November 2023
Published 16 November 2023 Volume 2023:15 Pages 225—236
DOI https://doi.org/10.2147/ORR.S433846
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Clark Hung
Peng Li, Xiang Li, Lin Ma, Hai Yi He
Spinal Surgery Department, Sanmenxia Central Hospital, Sanmenxia, Henan, People’s Republic of China
Correspondence: Hai Yi He, Spinal Surgery Department, Sanmenxia Central Hospital, Sanmenxia, Henan, People’s Republic of China, Email [email protected]
Background: The number of patients with lumbar disc herniation in China is increasing year by year. Percutaneous endoscopic lumbar discectomy (PELD) is currently the main surgical method for treating lumbar disc herniation (LDH). However, with the increase in the number of surgical cases, the number of patients with recurrent lumbar disc herniation (RLDH) is also increasing. Currently, the common method in China is lumbar fusion surgery, but this surgery would cause the loss of fusion segment mobility and considerable postoperative complications. In order to solve the problem above the following technique will be studied: the technique of posterior lumbar laminectomy and nucleus pulposus removal under fully visualized spinal endoscopy (ENDO-LOVE) to treat RLDH. Its clinical effects will be observed in this paper, too.
Methods: This series includes RLDH patients treated with ENDO-LOVE technology between January 2017 and January 2021. All patients will undergo at least three follow-up visits one year after surgery. The modified MacNab standard, VAS, JOA, and ODI scores will be used to evaluate clinical efficacy, observe for cerebrospinal fluid leak, nerve root injury, and surgical site infection, and evaluate clinical safety.
Results: All 29 patients completed the surgery successfully. Three patients had postoperative pain and numbness in the area of nerve root innervation, and all patients had no serious complications. The VAS, JOA scores and ODI indices of back pain and leg pain 1-day, 3-months, and 1-year postoperatively differed statistically significantly from the preoperative scores (p < 0.05). Efficacy evaluated at 1-year postoperatively using the modified MacNab criteria showed an excellent rate of 89.7%.
Conclusion: ENDO-LOVE technology has demonstrated good clinical efficacy and safety in the treatment of patients with RLDH. It should be considered for all patients with this condition.
Keywords: recurrent lumbar disc herniation, ENDO-LOVE technique, total spinal endoscopy
Introduction
Lumbar intervertebral disc protrusion is the result of degeneration of the nucleus, fibrous annulus, and terminal cartilage of the lumbar disc, superimposed by various endogenous and exogenous factors causing the nucleus and fibrous annulus to protrude, which locally produce inflammatory mediators and direct mechanical compression of the nerve roots, leading to lumbar and leg pain, and even to the emergence of muscle paralysis and atrophy, and the cauda equina, which has a serious impact on the quality of life of these patients. With the rapid development of the minimally invasive spine field in recent years, percutaneous endoscopic discectomy (PELD) has become an effective treatment for this disease.1,2 However, in view of the characteristics of this technique and the increase in the number of surgical cases over time, RLDH has gradually raised clinicians’ concerns, and the postoperative recurrence rate is currently reported to be 5% to 18%.3–6
Recurrent lumbar disc herniation (RLDH) refers to the recurrence of low back pain in the same or opposite side of the originally responsible segment due to the herniation of the lumbar disc that led to low back pain and surgical treatment, and the recurrence of low back pain in the same or opposite side of the originally responsible segment due to the herniation of the nucleus pulposus of the intervertebral disc to compress and stimulate the nerve root.3 Studies have shown that smoking and obesity are the main factors associated with recurrence of the postoperative period in RLDH.7,8 At the same time, recurrence of the postoperative period is also the main reason for patient dissatisfaction.9 Most patients with RLDH have severe low back pain symptoms, and most of them need to be treated with fusion surgery, which is very traumatic and accelerates the next level.10 However, fusion surgery is very invasive, and it is recommended that patients with RLDH be treated with fusion surgery. Therefore, in 2002, Yeung first applied minimally invasive techniques to treat RLDH and achieved satisfactory clinical results, and then more academicians applied minimally invasive techniques to treat RLDH.11,12 However, due to previous surgical treatments, the surgical area is highly fibroplastic due to bleeding and inflammatory response stimulation, and severe adhesions to the dura mater and nerve roots often occur, and the localized adhesions and anatomical levels are not clear. As a result, it is difficult to recognize the nerve root, posterior longitudinal ligament, fibrous ring and dura mater during surgery, and the rate of intraoperative complications, such as cauda equina exposure and nerve root injury, is high. Meanwhile, severe intraoperative complications often necessitate intraoperative conversion to open decompression surgery.13,14 According to the statistics, the incidence of the above-mentioned severe complications in revision surgery is 0% to 34.6%, which is 2.5 to 5 times that of the original surgery.15–17 Thus, in revision surgery, it is necessary to obtain sufficient field of view. Thus, revision surgery requires adequate visual field exposure to distinguish tissue structures. Traditional “small opening window” nucleotomy (LOVE technique) has the advantages of good visual field, adequate neural decompression, and precise clinical results. However, the use of the LOVE technique causes greater musculoskeletal soft tissue damage in the posterior lumbar spine, which increases the risk of lumbar spine instability.18,19 Besides the advantages of the LOVE procedure, the ENDO-LOVE procedure has the advantages of a minimally invasive procedure, ie less damage to the posterior lumbar spinal column, adequate decompression, clear intraoperative visualization and full symptomatic relief. To this end, this study retrospectively analyzed 29 cases of RLDH patients admitted to our department who were treated with the ENDO-LOVE technique, and the therapeutic effects were satisfactory, which are now reported as follows.
Methods
General Information
Inclusion criteria: 1. patients whose initial surgery was a lateral approach or posterior spinal endoscopy; 2. patients with the same segment responsible for the initial surgery and who had been in symptomatic remission for more than 6 months after the initial surgery; 3. signs and symptoms consistent with imaging data; 4. patients who underwent at least 8 weeks of formal conservative treatment with poor outcome.
Exclusion criteria: 1. patients with preoperative lumbar imaging CT, MRI, and power for X-ray showing lumbar instability; 2. patients with massive herniation compressing the cauda equina nerve resulting in lower limb weakness, numbness, pain, urinary and fecal dysfunction, and sexual dysfunction; 3. patients with combined intervertebral infection, spinal tuberculosis, and tumor; 4. patients with symptomatic first-time lateral laminectomy; 5. patients with severe congestive heart failure and respiratory failure who cannot tolerate general anesthesia; 6. patients with severe anxiety and depression combined with psychiatric evaluation.
According to inclusion/exclusion criteria, 29 patients with RLDH were retrospectively analyzed for Endo-Love technique revision in our department from 01/2017 to 01/2021. Among them, 15 were male and 14 were female; age ranged from 24 to 52 years with a mean age of (38.8 ± 6.89) years; protrusion site: 10 for L4/5 patients, 19 for L5/S1 patients, 18 for patients on same side as first surgery, and 11 for patients on opposite side. The number of patients with a lateral foramen approach for the first surgery was 20, and the number of patients with a posterior interlaminar approach for the first surgery was 9.
Surgical Method
After general anesthesia, the patient was placed in the prone position on the spinal surgical bed, and the responsible space was visualized using C-arm fluoroscopy. The puncture site was opened approximately 2 cm lateral to the symptomatic spinous process of the responsible space, the skin was soaked in complex iodine disinfectant for 10 minutes, deiodinated in alcohol, covered with sterile film and a homemade dam, and the puncture needle was placed percutaneously. In the lateral position, the puncture needle was positioned at the superior edge of the vertebral body. A 2 cm longitudinal incision was made along the puncture needle, and the guide wire, soft tissue expansion channel, and working cannula were placed in sequence. The tip of the working trocar was clearly located at the lateral edge of the vertebral plate under fluoroscopy. The endoscopic light source, irrigation saline, and camera system were connected, and the working channel placement was completed. The subscopic circular saw and lamellar forceps were used to remove part of the upper edge of the vertebral plate and part of the articular synovial joint to achieve opening and decompression of the vertebral plate space through endoscopic bipolar radiofrequency hemostasis and separation of soft tissues, medial exposure of the sphenoid root, exposure of the ligamentum flavum and the upper edge of the vertebral plate, and lateral exposure of the articular synovial joint. The extent of the opening was related to the preoperative CT and MRI prominence, the lamellar forceps and basket forceps were used to gradually bite away the ligamentum flavum from the normal tissue to the surgical area, and the dural sac was exposed, the adhesions were microscopically separated, the working trocar was rotated to push the nerve roots to the center, the working area was exposed, the herniated fibrous ring nucleus pulposus and scar tissue were removed, and no nucleus pulposus residue was seen in the axilla. The bipolar radiofrequency was sufficiently spotted to stop bleeding and ablate the coarse tissue at the edge of the fibrous ring, and the nerve root and dural sac were well pulsed microscopically. The endoscopic operating system was withdrawn after reexamination for obvious bleeding sites, local irrigation fluid was aspirated with a long needle, and the endoscopic operating system was withdrawn after local injection of 1 mL of Depo-Provera, and the surgical incision was sutured and sterilized and bandaged.
Evaluation Criteria
Clinical safety observations: duration of operation, intraoperative nerve root injury, dural injury, cerebrospinal fluid leakage, cauda equina injury, postoperative intracanalicular haematoma, intervertebral space infection, and more;
Observation index of clinical efficacy: 1-year postoperative follow-up, observing and recording changes in VAS score, JOA score, and ODI index at four time periods: preoperative, 1-day postoperative, 3-months, and 1-year postoperative; 1-year postoperative efficacy assessment using modified MacNab criteria [14], classified into 4 grades of excellent, good, acceptable, and poor, with excellent rate = (excellent + good)/total number of cases*100%.
Statistical methods
SPSS 19.0 software was used for statistical data analysis, and the collected data measures were expressed as mean±standard deviation (x±s), and pre and post-treatment data within group were compared by one-way repeated measures ANOVA, p<0.05 as statistically significant difference.
Results
Clinical Safety Observation results
All 29 patients successfully completed the surgery, and the operation time was 76 to 105 minutes, with a mean of (88.1 ± 8.3) minutes; the postoperative observation period in the hospital was 3 to 6 days, with a mean of (4.2 ± 1.1) days; three patients experienced postoperative pain and numbness in the area of nerve root innervation, and the inflammatory reaction of nerve root edema was taken into account, and symptomatic treatment with hormonal, nerve nutrition and dehydrating drugs was given for about 6 days. All patients had no intraoperative nerve root injury, dural injury, cerebrospinal fluid leakage, cauda equina injury, etc.; postoperative complications included spinal canal hematoma, intervertebral space infection, etc.
Clinical Efficacy Observation Indicators
ANOVA with repeated measures was used for VAS score, JOA score ODI index for different periods of time in patients with recurrent lumbar disc herniation treated with End-Love technique. The results showed that the difference was statistically significant (F=227.72 p=0.000) when comparing the VAS scores at preoperative (6.58±1.12), 1-day postoperative (2.21±0.54), 3-months postoperative (1.21±0.42), and 1-year postoperative (0.21±0.42), and the differences were statistically significant (F=227.72 p=0.000); preoperative (5.21±1.65), 1-day postoperative (20.68± 2.06), 3-months postoperatively (24.68±1.80), and 1-year postoperatively (25.16±1.74) JOA scores were compared and the difference was statistically significant (F=401.94 p=0.000); preoperatively (38.79±2.30), 1-day postoperatively (21.53±2.22), 3-months postoperatively (6.11±2.13), and 1-year postoperatively (2.32±1.00) ODI index scores were compared and the difference was statistically significant (F=1329.50 p=0.000); (Table 1).
 |
Table 1 Comparison of VAS, JOA Scores, and ODI Indices Before and After Surgery in 29 Patients ( |
One year after surgery, the overall result was evaluated according to the modified MacNab criteria. Among the 29 cases, 20 were excellent, 6 were good, and 3 were acceptable, with an excellent rate of 89.7%. The three patients with an efficacy of “1” had recurrence due to heavy physical labor in the short term after surgery, and finally improved after open fusion surgery after conservative treatment failed. Moreover, A case of a 32-year-old male patient with RLDH who was surgically treated with the END-LOVE technique, as shown in Figures 1–13.
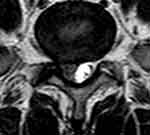 |
Figure 1 Lumbar spine coronal MRI showed a right-sided disc herniation. |
 |
Figure 2 MRI T2 image of lumbar spine in sagittal position shows L5/S1 disc protruding to the posterior side. |
 |
Figure 3 Pre-operative lumbar spine 3-D CT showed intact vertebral plate. |
 |
Figure 4 In the figure, the tip of the vascular clamp points to the location of the puncture. |
 |
Figure 5 Orthostatic X-ray images of the lumbar spine were taken after placement of the working channel. |
 |
Figure 6 Lateral X-ray images of the lumbar spine taken after placement of the working channel. |
 |
Figure 7 Removal of ligamentum flavum by microscopic occlusion with medullary forceps. |
 |
Figure 8 Exposure of the fibrous ring was seen to be unruptured and the scar healed. |
 |
Figure 9 At the completion of the operation, the nucleus pulposus was completely removed and the nerve root and dural sac were clearly visible and flaccid. |
 |
Figure 10 The left side shows the bone removed intraoperatively; the right side shows the nucleus pulposus and fibrous ring tissue removed intraoperatively. |
 |
Figure 11 Post-operative lumbar coronal MRI showed that herniated disc tissue had been removed with adequate nerve decompression. |
 |
Figure 12 Postoperative lumbar spine sagittal MRI T2 image showed that the dural sac compression had been relieved and the nerve decompression was adequate. |
 |
Figure 13 Post-operative 3-dimensional CT clearly shows the bone of the vertebral plate removed by intraoperative decompression. |
Discussion
LOVE technique is posterior lumbar plate opening nucleus pulposus removal, which was firstly reported by Prof. Love J G in 1939, and it is the main procedure for treating lumbar disc herniation in the era of traditional surgery. Over the years, endoscopic spine surgery has evolved to become an important surgical technique in spine surgery. Minimally invasive percutaneous endoscopic nucleus pulposus removal (PELD) is currently an effective means of treating lumbar disc herniation,1,2 which can achieve the same clinical results as traditional open surgery, and it mainly includes two modalities: lateral transforaminal approach (PETD) and posterior transforaminal interlaminar approach (PEID). With the wide application of spinal endoscopy in the clinic, the maturity of its technology is on the rise, and it is gradually being applied to patients with RLDH.11,12 The Endo-Love technique belongs to the category of interlaminar approach, which is a combination of the advantages of total spinal endoscopy technology and LOVE technology, and its main features are more in line with the spinal surgeon’s habit of posterior approach, and the anatomical level of surgical access tissues is basically the same as that of conventional open surgery. In short, it is the endoscopic operation of traditional open window decompression and nucleus pulposus removal, and it makes up for the blind spot of PETD technology.
RLDH is often caused by bleeding irritation from the initial surgery resulting in severe dural adhesions in the operative area. Use of conventional PETD technique and PEID technique for revision surgery is often due to the narrow field of view, effective surgical space, and the risk of intraoperative cerebrospinal fluid leakage and nerve root injury is significantly increased compared with the initial surgery.20 As the skill of operation increases, Endo-Love technique treatment has obvious advantages in treating patients with RLDH, and its technical points are as follows.
1. Fluoroscopic localization: a common localization plate is used for marking, which is positioned at the junction of the inferior articular eminence and the superior vertebral plate, similar to the V-point of the cervical spine. The 1-level guide rod is inserted squarely into the bone, so that the junction between the tip of the inferior articular eminence and the superior margin of the inferior vertebral plate is found, and the mirror is less likely to get lost.
2. Place the working trocar and perform fluoroscopy once again: Place the dilatation tube step by step along the guide rods and place the external protection trocar. Use fluoroscopy to judge the position of the trocar in the orthogonal position. The best position for common surgical procedures is that the head end of the trocar is located at the junction of the inferior articular process and the superior lamina in the anterior position, and in the lateral position, the head end of the trocar is located near the dorsal aspect of the articular process of the lamina, and the direction is generally toward the intervertebral space.
3. Full visible endoscopic exposure of surgical anatomy: Access to the endoscopic system, cleaning of the soft tissues between the intervertebral articular processes, and combination with preoperative imaging to find the following anatomical structures: the lower edge of the superior vertebral plate, the upper edge of the inferior vertebral plate, the apical portion of the inferior articular process, the ligamentum flavum between the plates, and the root of the spinous process.
4. Open vertebral plate: According to the operator’s habit, the vertebral plate can be opened by the use of microscopic ring saw, microscopic forceps and vertebral plate forceps. The author primarily used the ring saw to remove bone from the transition between the lower articular process and the lower edge of the vertebrae. Depending on whether the disc is prolapsing superiorly or inferiorly, the amount of bone removed on the cephalad and caudal sides of the annulus may vary. For example, a supraspinatus and anterior shoulder type herniation may be more cephalad, while an axillary type herniation that prolapses caudally may be more caudal. Caution notes (1) Rather than using a full saw, try to see half of the bone and half of the ligamentum flavum in the saw, which will not only help judge the depth of the saw but will also prevent too much ring removal from compromising stability; (2) Ring removal of bone should generally not be more than the medial edge of the vertebral arch root connecting the line, to avoid damaging the lateral bone column of the vertebral arch, resulting in an isthmus fracture; (3) There is a certain learning curve in using the ring saw to avoid ring sawing too deeply, protruding into the spinal canal, and damaging the nerves.
5. Removal of the Ligamentum Flavum: Removal of the clavicular ligament can be easily done, even in one piece, if the plate bone is removed to the cephalocaudal stop of the clavicular ligament. Of course, the general Endo-Love surgery will not reach the cephalocaudal stop of the ligamentum flavum. At that time, there are many ways to remove the ligamentum flavum into the spinal canal. Currently, the common ways to break the ligamentum flavum: (1) directly rotate the trocar to break the ligamentum flavum, with the tip of the trocar pushed to the ventral side of the repeatedly rotated to break the ligamentum flavum; (2) using the blue forceps and nucleus pulposus forceps to break the ligamentum flavum, which is also the commonly used way to break the ligamentum flavum. This approach is safe, can be performed under general anesthesia, and can achieve the necessary dissection of the ligamentum flavum, completely expose the nerve structures in the spine, and provide a comprehensive anatomic field of view for the next step of ventral decompression of the nerve. Warning: If the primary surgery is a posterior approach and the scar at the ligamentum flavum defect can be seen microscopically to be adhering to the dura mater, it is suggested that the vertebral plate bone be removed to the cephalo-caudal stop of the ligamentum flavum, and the ligamentum flavum be gradually bitten off to the area of adherence to avoid damaging the dura mater to avoid damaging the dura mater and cauda equina.
6. Removal of ventral herniated disc nucleus pulposus tissue: after removing the ligamentum flavum, the fatty tissue on the surface of the nerve can be seen, further clamp the fatty tissue, or radiofrequency head electrocautery to separate it, the edge of the dural sac and the traveled nerve root can be seen, and the shoulder and axilla where the nerve bifurcates can be seen. Depending on the location of the herniation, a ventral herniation is localized. It is removed using a nerve probe hook and trocar rotational block. For the anterior, shoulder-side, axillary type of herniation, a reverse hand scope is preferred, which will significantly reduce nerve root irritation. Avoid forceful removal of larger prolapsed medulla or even accompanying endplate cartilage tissue. Forceful removal is prone to nerve injury and is difficult to tolerate, especially in patients under local anesthesia. It can be pulled in a ventral parallel direction to begin with, and pulled and released like fishing while removing. Particularly large tissues may need to be removed with the outer sheath. When the decompression is complete, it can be seen that the nerve root is relaxed, that there is some space on the ventral side, and that there is no pressure-causing material to be seen, so the procedure can be completed. Draining is usually not necessary. For the novice surgeon, a negative pressure tube may be placed in the original incision if there is insufficient hemostasis at the microscopic level.
Among the 29 patients with RLDH in our group who underwent revision using the Endo-Love total spine endoscopic technique, the VAS, JOA, and ODI scores improved to different degrees after surgery compared with the preoperative scores, and the difference was statistically significant (p < 0.05). The excellent rate was 89.7%, and only 3 patients had “acceptable” efficacy. Only three patients in the “acceptable” effectiveness group recurred because of heavy work in the short term after surgery, pre-operative MRI of the lumbar spine showed that the patient had stage I endplate inflammation, which improved after open fusion surgery, Intraoperative prolapse of lumbar endplate cartilage with nucleus pulposus tissue from the first revision area. Meanwhile, in this study, the method of removal of vertebral plate and articular protrusion bone was adopted, and the scar adherent tissues were peeled off from the bone edge without forceful separation of scar adherent tissues, so there was no CSF leakage, nerve root dissection and cauda equina injury with serious complications in this group of cases.21,22 The above results show that the Endo-Love technique for the treatment of patients with RLDH can achieve a satisfactory clinical result with high surgical safety.
In summary, Endo-Love technique is clinically effective in patients with RLDH. Intraoperative fluoroscopy is less, radiation damage is low, and resection of the lamina, ligamentum flavum and articular eminence under direct vision is safe with good stability of the lumbar spine.23 At the same time, the operation begins with the removal of the vertebral plate. This avoids serious complications such as damage to the dura mater and cauda equina due to the direct removal of the ligamentum flavum from adhesions. This technique belongs to the traditional PEID method, which is more in keeping with spine surgeons’ surgical habits and is easy to learn and master. However, this study is a retrospective study, with a small number of cases and a lack of a control group, so the long-term effects need to be further studied.
Conclusion
Use of End-Love technology to treat RLDH has the advantages of minimal traumatization and good clinical outcome, with good clinical safety and efficacy, and is worthy of adoption.
Ethics Approval and Consent to Participate
This study was approved by the Ethics Committee of Sanmenxia Central Hospital. The privacy and personal identity of all participants were protected, and written informed consent was obtained from all participants. This study adhered to the tenets of the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Li X, Hu Z, Cui J, et al. Percutaneous endoscopic lumbar discectomy for recurrent lumbar disc herniation. Int J Surg. 2016;27:8–16. doi:10.1016/j.ijsu.2016.01.034
2. Chen HC, Lee CH, Wei L, Lui TN, Lin TJ. Comparison of percutaneous endoscopic lumbar discectomy and open lumbar surgery for adjacent segment degeneration and recurrent disc herniation. Neurol Res Int. 2015;2015:791943. doi:10.1155/2015/791943
3. Lee JK, Amorosa L, Cho SK, Weidenbaum M, Kim Y. Recurrent lumbar disk herniation. J Am Acad Orthop Surg. 2010;18(6):327–337. doi:10.5435/00124635-201006000-00005
4. Shimia M, Babaei-Ghazani A, Sadat BE, Habibi B, Habibzadeh A. Risk factors of recurrent lumbar disk herniation. Asian J Neurosurg. 2013;8(2):93–96. doi:10.4103/1793-5482.116384
5. Suk KS, Lee HM, Moon SH, Kim NH. Recurrent lumbar disc herniation: results of operative management. Spine. 2001;26(6):672–676. doi:10.1097/00007632-200103150-00024
6. Camino Willhuber G, Kido G, Mereles M, et al. Factors associated with lumbar disc hernia recurrence after microdiscectomy. Factores asociados a recidiva de hernia de disco lumbar luego de una microdiscectomía. Rev Esp Cir Ortop Traumatol. 2017;61(6):397–403. doi:10.1016/j.recot.2017.07.002
7. Siccoli A, Staartjes VE, Klukowska AM, Muizelaar JP, Schröder ML. Overweight and smoking promote recurrent lumbar disk herniation after discectomy. Eur Spine J. 2022;31(3):604–613. doi:10.1007/s00586-022-07116-y
8. Yaman ME, Kazancı A, Yaman ND, Baş F, Ayberk G. Factors that influence recurrent lumbar disc herniation. Hong Kong Med J. 2017;23(3):258–263. doi:10.12809/hkmj164852
9. Fu TS, Lai PL, Tsai TT, Niu CC, Chen LH, Chen WJ. Long-term results of disc excision for recurrent lumbar disc herniation with or without posterolateral fusion. Spine. 2005;30(24):2830–2834. doi:10.1097/01.brs.0000190393.15369.94
10. Dower A, Chatterji R, Swart A, Winder MJ. Surgical management of recurrent lumbar disc herniation and the role of fusion. J Clin Neurosci. 2016;23:44–50. doi:10.1016/j.jocn.2015.04.024
11. Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: surgical technique, outcome, and complications in 307 consecutive cases. Spine. 2002;27(7):722–731. doi:10.1097/00007632-200204010-00009
12. Kogias E, Franco Jimenez P, Klingler JH, Hubbe U. Minimally invasive redo discectomy for recurrent lumbar disc herniations. J Clin Neurosci. 2015;22(9):1382–1386. doi:10.1016/j.jocn.2015.02.028
13. Ahn Y, Lee SH, Park WM, Lee HY, Shin SW, Kang HY. Percutaneous endoscopic lumbar discectomy for recurrent disc herniation: surgical technique, outcome, and prognostic factors of 43 consecutive cases. Spine. 2004;29(16):E326–E332. doi:10.1097/01.brs.0000134591.32462.98
14. Kim CH, Chung CK, Sohn S, Lee S, Park SB. The surgical outcome and the surgical strategy of percutaneous endoscopic discectomy for recurrent disk herniation. J Spinal Disord Tech. 2014;27(8):415–422. doi:10.1097/BSD.0b013e3182a180fc
15. Deer T, Sayed D, Michels J, Josephson Y, Li S, Calodney AK. A Review of Lumbar Spinal Stenosis with Intermittent Neurogenic Claudication: disease and Diagnosis. Pain Med. 2019;20(Suppl 2):S32–S44. doi:10.1093/pm/pnz161
16. Palma L, Carangelo B, Muzii VF, Mariottini A, Zalaffi A, Capitani S. Microsurgery for recurrent lumbar disk herniation at the same level and side: do patients fare worse? Experience with 95 consecutive cases. Surg Neurol. 2008;70(6):619–621. doi:10.1016/j.surneu.2007.12.020
17. Vinas-Rios JM, Sanchez-Aguilar M, Medina Govea FA, Von Beeg-Moreno V, Meyer F, Registry-group DWG. Incidence of early postoperative complications requiring surgical revision for recurrent lumbar disc herniation after spinal surgery: a retrospective observational study of 9310 patients from the German Spine Register. Patient Saf Surg. 2018;12:9. doi:10.1186/s13037-018-0157-1
18. Cinotti G, Gumina S, Giannicola G, Postacchini F. Contralateral recurrent lumbar disc herniation. Results of discectomy compared with those in primary herniation. Spine. 1999;24(8):800–806. doi:10.1097/00007632-199904150-00012
19. Chen Z, Zhao J, Liu A, Yuan J, Li Z. Surgical treatment of recurrent lumbar disc herniation by transforaminal lumbar interbody fusion. Int Orthop. 2009;33(1):197–201. doi:10.1007/s00264-008-0531-1
20. Le H, Sandhu FA, Fessler RG. Clinical outcomes after minimal-access surgery for recurrent lumbar disc herniation. Neurosurg Focus. 2003;15(3):E12. doi:10.3171/foc.2003.15.3.12
21. Shin KH, Chang HG, Rhee NK, Lim KS. Revisional percutaneous full endoscopic disc surgery for recurrent herniation of previous open lumbar discectomy. Asian Spine J. 2011;5(1):1–9. doi:10.4184/asj.2011.5.1.1
22. Ruetten S, Komp M, Merk H, Godolias G. Recurrent lumbar disc herniation after conventional discectomy: a prospective, randomized study comparing. Clin Spine Surgery. 2009;22(2):122
23. Lee DY, Shim CS, Ahn Y, Choi YG, Kim HJ, Lee SH. Comparison of percutaneous endoscopic lumbar discectomy and open lumbar microdiscectomy for recurrent disc herniation. J Korean Neurosurg Soc. 2009;46(6):515–521. doi:10.3340/jkns.2009.46.6.515
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

