Back to Journals » Infection and Drug Resistance » Volume 16
Clinical Diagnostic Value of Serum 25-Hydroxyvitamin D in Severe Fever with Thrombocytopenia Syndrome
Authors Liu T, Liu J , Wu J , Qin L, Shi Y, Qi Y
Received 3 January 2023
Accepted for publication 6 March 2023
Published 24 March 2023 Volume 2023:16 Pages 1715—1724
DOI https://doi.org/10.2147/IDR.S403482
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Ting Liu,1 Jiaxing Liu,2 Jing Wu,1 Linghan Qin,1 Yuru Shi,1 Yingjie Qi1
1Department of Laboratory Medicine, Infection Hospital Area of the First Affiliated Hospital of University of Science and Technology of China (Hefei Infectious Disease Hospital), Hefei, Anhui Province, 230022, People’s Republic of China; 2Department of Laboratory Medicine, Nanjing Drum Tower Hospital, The Affiliated Hospital of Nanjing University Medical School, Nanjing, Jiangsu Province, 210008, People’s Republic of China
Correspondence: Yingjie Qi, Department of Laboratory Medicine, Infection Hospital Area of the First Affiliated Hospital of University of Science and Technology of China (Hefei Infectious Disease Hospital), No. 218 Susong Road, Hefei, Anhui Province, 230022, People’s Republic of China, Email [email protected]
Purpose: Severe Fever with Thrombocytopenia Syndrome (SFTS) is an infectious disease with rapid onset and high case fatality rate. The study was to explore the clinical value by examining the serum level of 25-hydroxyvitamin D (25 (OH) D) in SFTS patients.
Methods: One hundred and five patients and 156 healthy controls were included. Univariate and multivariate regression analyses were performed to identify independent risk factors for disease progression. Subject operating characteristics (ROC) curves were drawn, and the corresponding area under the curve (AUC) was calculated to assess the sensitivity and specificity of the diagnostic disease.
Results: The 25 (OH) D level of disease group was lower than that of healthy control group (22.12 (18.43, 25.86) ng/mL vs 27.36 (23.20, 32.71) ng/mL; P< 0.05). The 25 (OH) D level of severe disease group was lower than that of mild disease group (20.55(16.30, 24.44) ng/mL vs 24.94(20.89, 31.91) ng/mL; P< 0.05). And there was no significant difference of 25 (OH) D level between the survival group and death group in severe disease group. Multivariate Logistic regression analysis showed that the 25 (OH) D level under 19.665 ng/mL was an independent risk factor for the development of SFTS (OR = 0.901, P=0.040). Furthermore, age more than 68.5 years old and lactate dehydrogenase (LDH) more than 1023.5U/L were independent risk factors for death in severe patients with SFTS.
Conclusion: Patients with SFTS have reduced 25 (OH) D level, and 25 (OH) D is a risk factor for disease severity in patients with SFTS. Vitamin D supplementation may be an effective measure to reduce the risk of infection and improve the prognosis.
Keywords: severe fever with thrombocytopenia syndrome, 25-hydroxyvitamin D, risk factor
Introduction
Severe Fever with Thrombocytopenia Syndrome (SFTS) is a notifiable infectious disease caused by SFTS virus (SFTSV),1 carried by ticks. SFTSV is a single stranded negative-strand RNA virus, a new member of the Phlebovirus genus of the Bunyaviridae family, which was renamed Dabie Banda virus by the International Committee on Taxonomy of Viruses in 2019. It is reported to be endemic in different parts of China. After the infection, the patient developed symptoms of fever, stomachache, gastrointestinal dysfunction, nausea, abdominal distension, vomiting, and thrombocytopenia.2,3 SFTS cases have also been identified in Korea, Japan and Vietnam,4 and similar diseases have occurred in the United States.5,6 In some endemic areas, the disease incidence is very high, with case-fatality rates of up to 30%, posing an increasing threat to global health. Vitamin D is a steroid derivative that can regulate the balance of calcium and phosphorus and promote the absorption of calcium and phosphorus, playing an essential role in human health.7 It can be obtained from several sources: diet, supplements or seasonal skin exposure to appropriate ultraviolet radiation from the sun through photochemical and thermal conversion of the cholesterol precursor 7-dehydrogenated cholesterol.8,9 Vitamin D exists in two natural forms, ergocalciferol (vitamin D2) and cholecalciferol (vitamin D3), depending on the number and location of the two-carbon carbon bonds. Vitamin D2 and D3 are metabolized in the liver to 25(OH)D by 25-hydroxylase, and then hydroxylated to 1,25 dihydroxyvitamin D3 (1,25 (OH)2D), which is most active in the kidney, but its anabolism is regulated by regulators such as phosphorus, calcium, parathyroid hormone, and fibroblast growth factor-23 (FGF23). Serum 25 (OH) D is the main circulating form of vitamin D, and can be used to evaluate the total level of vitamin D present in the body, reflecting the state of vitamin D in the body.10 In addition to its known role in maintaining bone health, vitamin D is involved in several biological functions, including antiproliferation, antiangiogenesis and immune system regulation.11–13 New evidence suggests that vitamin D can also prevent a variety of cancers. In the past two years, many studies have shown that Corona Virus Disease 2019 (COVID-19) is associated with low vitamin D levels.14,15 Therefore, we conducted this study, aiming to determine the association between serum 25 (OH) D level and the risk of SFTSV infection and the disease severity in patients with SFTS.
Materials and Methods
Research Subjects and Data Collection
Between April 2020 and August 2022, serum samples of 105 patients clinically diagnosed with SFTS and 156 healthy controls were collected from Infection Hospital Area of the First Affiliated Hospital of the University of Science and Technology of China. Clinical data of the two groups were also collected, including sex, age and other laboratory-related indicators: alanine aminotransferase (ALT), aspartate aminotransferase (AST), γ -glutamyltransferase (GGT), total protein (TP), albumin (ALB), lactate dehydrogenase (LDH), calcium (Ca), phosphorus (P), magnesium (Mg), creatine kinase (CK), creatine kinase isozymes CK-MB), amyloid A (SAA), white blood cells (WBC), neutrophils (Neu), platelets (PLT), CD3, CD4, CD8, CD4/CD8, C-reactive proteins (CRP), procalcitonin (PCT) and interleukin-6 (IL-6).
Inclusion and Exclusion Criteria
Inclusion Criteria included all patients met the diagnostic criteria for the Prevention and Treatment of Fever with thrombocytopenia Syndrome (2010) standard.16 The disease group was divided into mild and severe groups. The mild group included mild and normal types and the severe group included severe and critical types. Exclusion criteria: (1) with other viral infections; (2) with fungal, bacterial, or parasitic infections; (3) with vitamin drug supplements within nearly 1 month; (4) with other systemic diseases.
Instruments and Reagents
Instruments included: Antu A2000Plus automatic immune analyzer (Zhengzhou Antu biological engineering co., LTD.), Beckman AU 5800 automatic biochemical analyzer (Beckman Kurt biotechnology co., LTD.), Mindray BC6900 automatic blood cell analyzer (Shenzhen mrui biomedical electronics co., LTD.), Wanfu dry type fluorescence immunoanalyzer (Guangzhou wanfu biotechnology co., LTD.), Roche C411 automatic electrochemiluminometer (Hoffmann-La Roche), FACSCalibur Fully Automatic flow cytometer (Becton, Dickinson and Company). Reagents included alanine aminotransferase assay kit, aspartate aminotransferase assay kit, γ -glutamyl aminotransferase assay kit (Shanghai Fosun Diagnostic Technology Co., LTD.); total protein determination kit, albumin determination kit, lactate dehydrogenase determination kit (Anhui Tongzhi Biological Engineering Co., LTD.); creatine kinase assay kit, creatine kinase isoenzyme assay kit (Ningbo Tiankang Biotechnology Co., LTD.); amyloid A assay kit (Anhui Daqian Biological Engineering Co., Ltd.). Except for the reagents mentioned above, all the instrument supporting reagents were used.
Study Variables
One hundred and five patients were divided into mild group (34 cases) and severe group (71 cases); Patients in the severe group were divided into survival group (51 cases) and death group (20 cases) according to the final outcome. Antu A2000Plus was used to detect 25(OH)D; AU 5800 was performed for testing for ALT, AST, GGT, TP, AL B, LDH, CK, CK-MB, SAA, Ca, P, Mg; Mindray BC6900 test for CRP, WBC, Neu; Roche C411 Fully Automatic Electrochemiluminometer for Detection of IL-6; PCT was detected by Wanfu dry-type fluorescence immunoassay; CD3, CD4, CD8 and CD4/CD8 were detected by flow cytometry. The general data and laboratory examinations including the level of 25 (OH) D of the patients in different groups were retrospectively analyzed and compared. The relevant factors that may affect the prognosis were evaluated.
Statistical Analysis
We analyzed all data using SPSS software version 22 (SPSS, Inc., Chicago, IL, USA). For normal distribution measurement data, we expressed by mean ± SD and t-test was used for comparison between groups. For non-normal distribution measurement data, we described as M (P25, P75) percentiles and Mann–Whitney U-test was used for comparison between groups. Counting data were compared using chi-square test. Pearson correlation analysis was used to analyze the correlation of continuous variables. Multivariate Logistic regression was used to analyze the influencing factors of SFTS severity, and ROC curve was used to evaluate the predictive value of 25(OH)D. It is generally believed that the model with area under curve (AUC) >0.7 has clinical application value, and a P-value of <0.05 is considered to have statistical significance.
Results
Comparison of Laboratory Indicators Between Disease Group and Healthy Control Group
Among the 105 patients, 49 were males and 56 were females and the average age was 64.47±9.88 years old. In healthy control group, there were 72 cases of males and 84 cases of females and the average age was 60.01±6.40 years old. There was no significant difference in gender between the two groups, but age of the two groups was statistically different. Laboratory indicators including ALT, AST, GGT, TP, ALB, LDH, Ca, P, Mg, CK, CK-MB, SAA, CRP, WBC, Neu, PLT, CD3, CD4, CD8, CD4/CD8, PCT and IL-6 had statistical differences (P<0.05), as shown in Table 1.
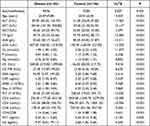 |
Table 1 Comparison of Laboratory Indicators Between Disease Group and Healthy Control Group |
Comparison of Laboratory Indicators Between Mild Disease Group and Severe Disease Group
In mild disease group, there were 17 males and 17 females, with an average age of 61.94±10.89 years old. In severe disease group, there were 32 males and 39 females, with an average age of 65.69±9.20 years old. There was no statistical difference in age and gender between the two groups. There were statistical differences of laboratory indicators including ALT, AST, LDH, CK, CK-MB, PLT, CD4/CD8, PCT and IL-6 between the two groups (P<0.05), as shown in Table 2.
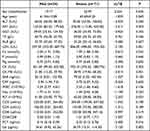 |
Table 2 Comparison of Laboratory Indicators Between Mild Disease Group and Severe Disease Group |
Comparison of Laboratory Indicators Between Death Group and Survival Group
There were 22 males and 29 females in survival group with an average age of 63.45±8.79 years old. In death group, there were 10 males and 10 females with an average age of 71.40±7.78 years old. There was a statistical difference in age between the two groups (P<0.05). There were statistical differences of ALT, AST, LDH, Ca, CK, CK-MB, PLT, PCT and IL-6 (P < 0.05), as shown in Table 3.
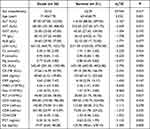 |
Table 3 Comparison of Laboratory Indicators Between Death Group and Survival Group |
Comparison of 25 (OH) D Level Between Disease Group and Healthy Control Group
The 25(OH)D level was 22.12 (18.43, 25.86) ng/mL in disease group and 27.36 (23.20, 32.71) ng/mL in healthy control group, and there was a statistical difference between the two groups (P<0.05), as shown in Figure 1.
 |
Figure 1 Comparison of 25 (OH) D levels between disease group and healthy control group. |
Comparison of 25 (OH) D Level Between Mild Disease Group and Severe Disease Group
The 25(OH)D level was 24.94 (20.89, 31.91) ng/mL in mild disease group and 20.55 (16.30, 24.44) ng/mL in severe disease group, and there was a statistical difference between the two groups (P<0.05), as shown in Figure 2.
 |
Figure 2 Comparison of 25 (OH) D levels between mild disease group and severe disease group. |
Comparison of 25 (OH) D Level Between Death Group and Survival Group
The 25(OH)D level was 20.29 (16.07, 22.87) ng/mL in death group and 21.38 (17.64, 24.61) ng/mL in survival group, with no statistically significant difference between the two groups (P>0.05), as shown in Figure 3.
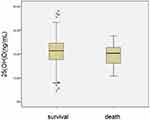 |
Figure 3 Comparison of 25 (OH) D levels between death group and survival group. |
Binary Logistics Regression Analysis
The status of severe disease in the disease group was taken as the dependent variable, and the variables with P-value <0.05 of the above laboratory test indicators in the univariate analysis were taken as the independent variable. The binary Logistic regression analysis showed that the lower the level of 25(OH)D was, the greater the possibility of developing into severe disease was, as shown in Table 4. Survival status in severe disease group was taken as the dependent variable, and the variables with P-value <0.05 of the above laboratory test indicators were taken as independent variables in the univariate analysis. The binary logistic regression analysis showed that the higher the LDH level, the older the age, the higher the risk of death, as shown in Table 5.
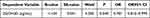 |
Table 4 The Logistics Regression Analysis of Disease Group |
 |
Table 5 The Logistics Regression Analysis of Severe Disease Group |
The Value of 25(OH)D Level for Developing Severe Disease in SFTS Patients by ROC Curve
We used ROC curve analysis to analyze the predictive value of 25(OH)D level for developing severe disease. The optimal critical value was 19.665 ng/mL, with a sensitivity of 0.577 and specificity of 0.606 (AUC = 0.725, P<0.05), as shown in Figure 4.
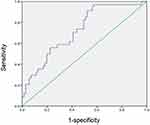 |
Figure 4 ROC curve of mild disease group and severe disease group. |
ROC Curve Evaluation of Death-Related Factors in SFTS Patients
The two variables of age and LDH that could lead to increased risk of death in the above binary logistic regression analysis were included in ROC curve analysis, in which the optimal critical value of age to predict the risk of death was 68.5 years old, with a sensitivity of 0.684 and a specificity of 0.700 (AUC = 0.747, P<0.05). The optimal threshold for LDH to predict the risk of death was 1023.5U/L, with a sensitivity of 0.789 and a specificity of 0.760 (AUC = 0.784, P<0.05), as shown in Figure 5.
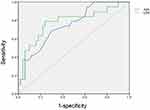 |
Figure 5 ROC curve of death group and survival group. |
Discussion
SFTS is a tick-borne infectious disease caused by SFTSV, and related cases have been reported worldwide, which can lead to fever, gastrointestinal reactions, thrombocytopenia and other symptoms, and in severe cases, multiple organ failure and eventually death. In recent years, the number of SFTS patients in East Asian countries has increased every year,17 which may be due to: (1) Greenhouse effect. The most suitable temperature for tick growth and activity is 25–30°C. As the global temperature increases year by year, the number of days with the temperature above 25°C increases, thus increasing the chance of contact with ticks and increasing the incidence. (2) The sensitivity of the detection method is improved. Now, reverse transcription-cross primer thermostatic amplification technique (RTCPA) technology combined with vertical flow visualization detection technology18 and reverse transcription real-time fluorescent quantitative polymerase chainR The reaction (RT-PCR) detection technique,19 Huang et al20 developed reverse transcription-loop mediated isothermal amplification (RT-LAMP) of SFTSV nucleotide sequences consistent with that of Chinese, the rapid development of RT-LAMP technology and metagenome sequencing (MGS), a hot topic in recent years, enable SFTSV infection to be detected earlier. There were 20 died cases among the 105 patients, with a case fatality rate of 19.04%. SFTS has become a serious public health problem, posing a great threat to human life and health. In this study, the levels of ALT, AST, GGT, LDH, CK, CK-MB, SAA, CRP, PCT, IL-6 in disease group were significantly higher than those in healthy control group, while the levels of TP, ALB, WBC, Neu, PLT, Ca, P, Mg, CD3, CD4, CD8, CD4/CD8 were significantly lower than those in healthy control group. The levels of ALT, AST, LDH, CK, CK-MB, PCT and IL-6 in severe disease group were significantly higher than those in mild disease group, while the levels of PLT and CD4/CD8 were significantly lower than those in mild disease group. ALT, AST, LDH, CK, CK-MB, PCT and IL-6 levels in death group were significantly higher than those in survival group, while Ca and PLT levels were significantly lower than those in survival group. This indicates that SFTV infection can cause multi-system damage, resulting in abnormal biochemical and blood routine indexes.
In addition to playing an important role in the skeletal system, vitamin D also has a variety of other biological functions, such as immune regulation and cancer prevention. Studies have shown that 25(OH)D is associated with a variety of infectious diseases in children.21,22 Beard et al reported that 1,25 (OH) 2D may stimulate cathelicidin release, regulate toll-like receptor expression and NK cell function, and inhibit proinflammatory cytokine overexpression, exert antiviral activity and regulate the inflammatory response of viral infection.23 Analyzing data from a total of 1368 COVID-19 positive patients, Ruhul Munshi24 concluded that low vitamin D levels were significantly associated with more severe symptoms and prognosis in patients. Vitamin D and its receptors play roles in both the primitive and adaptive immune system and mitigate anti-microbial and anti-inflammatory processes in the body. Vitamin D targets many immune cells, including monocytes, macrophages, T lymphocytes and B lymphocytes. Vitamin D can play an important role in some autoimmune diseases by enhancing the release of cytokines, promoting the polarization of T lymphocytes, and inducing Th1 to Th2 transition.25 It has been shown that patients with autoimmune or immune-mediated diseases have significantly lower serum vitamin D levels than healthy individuals.26 Giuseppe Lassandro et al reported that 80% of the 30 children they studied with immune thrombocytopenia (ITP) had serum vitamin D deficiency but there was no significant difference in vitamin D levels between newly diagnosed ITP and chronic ITP.27 It is suggested that vitamin D deficiency may not play a role in the progression of ITP, and further studies are needed to reveal the role of vitamin D in the pathogenesis of ITP. In addition, the level of 25(OH)D, the main form of vitamin D and a precursor of 1,25 (OH) 2D, can be used to assess the total level of vitamin D in the body.
In this study, the average 25(OH)D level of healthy control group was 27.36 (23.20, 32.71) ng/mL, while the average 25(OH)D level of disease group was 22.12 (18.43, 25.86) ng/mL, showing a statistical difference. The average 25(OH)D level of mild disease group was 24.94 (20.89, 31.91) ng/mL, while the average 25(OH)D level of severe disease group was 20.55 (16.30, 24.44) ng/mL, which was significantly different from that of mild disease group. This suggests that vitamin D deficiency may be related to the onset and development of SFTS. This may be because vitamin D can activate the apoptosis of activated B cells and inhibit the secretion of plasma cell immunoglobulin,28,29 thus increasing the risk of infection. In addition, there was no significant difference in the level of 25(OH)D between death group and survival group, which may be related to the fact that the number of included cases was not enough and the sample size was limited. In logistics regression analysis, 25(OH)D level is the only risk factor that can determine the development of severe disease, suggesting that serum 25(OH)D level has a direct impact on the severity of SFTS infection, and vitamin D supplementation may be a protective factor to prevent the progression of SFTS.
In summary, 25(OH)D level is one of the risk factors for severe SFTS, with predictive value, and timely supplementation of vitamin D at the early stage of the disease may effectively prevent the progression of the disease. There are still limitations in this study: (1) The included SFTS patients are generally middle-aged and elderly, and their 25(OH)D level itself may be lower than that of healthy people. However, there is no statistical difference in age between mild and severe patients, and the 25(OH)D level between the two groups is still statistically different. (2) Due to the limited sample size, no statistical difference in 25(OH)D level was found between survival group and death group. Therefore, it is necessary to expand the sample size and improve the evaluation methods in future studies, so as to effectively and accurately study the predictive value of 25(OH)D level for the survival status of severe SFTS patients. (3) This study is a retrospective study, and the impact of vitamin D deficiency on disease severity has not been demonstrated by prospective studies. Therefore, in future studies, the differences in disease development and survival status between patients in the vitamin D supplement group and those without vitamin D supplement group can be compared by taking different treatment measures to evaluate the clinical predicting value of vitamin D in SFTS.
Data Sharing Statement
All data and materials were in full compliance with the journal’s policy.
Ethics Approval and Informed Consent
Our study was approved by the Institutional Review Board of the First Affiliated Hospital of University of Science and Technology of China and the IRB number was 2021-BE(H)-005. We could not obtain written informed consent from the patients who have been discharged from hospital because this study is a retrospective study. But we obtained oral informed consent from all participants during telephone follow-up and the approval of the Institutional Review Board of the First Affiliated Hospital of the University of Science and Technology of China. We insure that all data that could indicate the identity of the patients were kept strictly confidential in this study. Work on human beings is conducted in accordance with the Declaration of Helsinki.
Acknowledgments
Thanks to all authors for their contributions to this study.
Funding
This study was supported by “Development and Clinical Application of A Novel Bunyavirus IgM/IgG Antibody Detection Kit (Time-Resolved Fluorescence Immunochromatography)” (fund project no. GWLM202012).
Disclosure
All authors declare that they have no conflicts of interest in this work.
References
1. Li P, Tong Z-D, Li K-F, Tang A, Dai Y-X, Yan J-B. Seroprevalence of severe fever with thrombocytopenia syndrome virus in China: a systematic review and meta-analysis. PLoS One. 2017;12(4):e0175592. doi:10.1371/journal.pone
2. Zhang L, Liu Y, Ni D, et al. Nosocomial transmission of human granulocytic anaplasmosis in China. JAMA. 2008;300:2263–2270. doi:10.1001/jama.2008.626
3. Xu B, Liu L, Huang X, et al. Metagenomic analysis of fever, thrombocytopenia and leukopenia syndrome (FTLS) in Henan Province, China: discovery of a new bunyavirus. Plos Pathog. 2011;7(11):e1002369. doi:10.1371/journal.ppat.1002369
4. Tran XC, Yun Y, Van An L, et al. Endemic severe fever with thrombocytopenia syndrome, Vietnam. Emerg Infect Dis. 2019;25(5):1029–1031. doi:10.3201/eid2505.181463
5. Kim KH, Yi J, Kim G, et al. Severe fever with thrombocytopenia syndrome, South Korea. Emerg Infect Dis. 2012;19:1892–1894.
6. Takahashi T, Maeda K, Suzuki T, et al. The first identification and retrospective study of severe fever with thrombocytopenia syndrome in Japan. J Infect Dis. 2014;209:816–827. doi:10.1093/infdis/jit603
7. Abbasnezhad A, Amani R, Hasanvand A, et al. Association of serum Vitamin D concentration with clinical symptoms and quality of life in patients with irritable bowel syndrome. J Am Coll Nutr. 2019;38(4):327–333. doi:10.1080/07315724.2018.1510349
8. Botelho J, Machado V, Proenca L, Delgado AS, Mendes JJ. Vitamin D deficiency and oral health: a comprehensive review. Nutrients. 2020;12(5):1471. doi:10.3390/nu12051471
9. Charoenngam N, Holick MF. Immunologic effects of vitamin D on human health and disease. Nutrients. 2020;12:2097. doi:10.3390/nu12072097
10. Rosen CJ. Clinical practice. Vitamin D insufficiency. N Engl J Med. 2011;364(3):248–254. doi:10.1056/NEJMcp1009570
11. Lee SJ, Kang BH, Choi BS. Vitamin D serum levels in children with allergic and vasomotor rhinitis. Korean J Pediatr. 2015;58(9):325–329. doi:10.3345/kjp.2015.58.9.325
12. Keles¸ E, Ozkara S, Ilhan N, et al. The relationship between Th1/Th2 balance and 1a, 25dihydroxyvitamin D3 in patients with allergic rhinitis. Turk Arch Otorhinolaryngol. 2015;53(4):139–143. doi:10.5152/tao.2015.1187
13. Esposito S, Lelii M. Vitamin D and respiratory tract infections in childhood. BMC Infect Dis. 2015;15:487. doi:10.1186/s12879-015-1196-1
14. Fouad MN, Ruffiffiffin J, Vickers SM. COVID-19 is out of proportion in African Americans. this will come as no surprise. Am J Med. 2020;10:30411–30413.
15. Dietz W, Santos-Burgoa C. Obesity and its implications for COVID-19 mortality. Obesity. 2020;28:1005. doi:10.1002/oby.22818
16. Yuan YM, Cui N, Yuan C, et al. Recommendations for nominating, clinical staging and typing of fever with thrombocytopenia syndrome. Chin J Infect Dis. 2016;34(1):57–58.
17. Li JC, Wang Y, Zhao J, et al. Progress in the epidemiological study of fever with thrombocytopenia syndrome. Chin J Epidemiol. 2021;42(12):2226–2233. doi:10.3760/cma.j.cn112338-20210529-00439
18. Cui L, Ge Y, Qi X, et al. Detection of severe fever with thrombocytopenia syndrome virus by reverse transcription-cross-priming amplification coupled with vertical flow visualization. J Clin Microbiol. 2012;50(12):3881–3885. doi:10.1128/JCM.01931-12
19. Sun Y, Liang M, Qu J, et al. Early diagnosis of novel SFTS bunyavirus infection by quantitative real-time RT-PCR assay. J Clin Virol. 2012;53(1):48–53. doi:10.1016/j.jcv.2011.09.031
20. Huang XY, Hu XN, Ma H, et al. Detection of new bunyavirus RNA by reverse transcription-loop-mediated isothermal amplification. J Clin Microbiol. 2014;52(2):531–535. doi:10.1128/JCM.01813-13
21. Zhang XY, ChX L, ZhA O, et al. Analysis of serum vitamin D, calcium, phosphorus, and parathyroid hormone levels in children with mild rotavirus enteritis and benign convulsions. CJCHC. 2019;27(6):684–686.
22. Chen YM, Lu S, Wang ZHP, et al. Correlation between serum 25-hydroxyvitamin D levels and respiratory infections in children. Mater Child Health Care China. 2018;33(19):117–119.
23. Beard JA, Bearden A, Striker R. Vitamin D and the anti-viral state. J Clin Virol. 2011;50:194–200. doi:10.1016/j.jcv.2010.12.006
24. Munshi R, Hussein MH, Toraih EA, et al. Vitamin D insufficiency as a potential culprit in critical COVID‐19 patients. J Med Virol. 2021;93(2):733–740. doi:10.1002/jmv.26360
25. Bizzaro G, Antico A, Fortunato A, Bizzaro N. Vitamin D and autoimmune diseases: is Vitamin D Receptor (VDR) polymorphism the culprit? Isr Med Assoc J. 2017;19(7):438–443. PMID:28786260.
26. Antico A, Tampoia M, Tozzoli R, Bizzaro N. Can supplemen-tation with vitamin D reduce the risk or modify the course of autoimmune diseases? A systematic review of the literature. Autoimmun Rev. 2012;12(2):127–136. doi:10.1016/j.autrev.2012.07.007
27. Lassandro G, Carriero F, Palmieri V, et al. Serum vitamin D levels in children with immune thrombocytopenia. Endocr Metab Immune Disord Drug Targets. 2020;20(2):221–226. doi:10.2174/1871530319666190614152709
28. Chen S, Sims GP, Chen XX, Gu YY, Chen S, Lipsky PE. Modulatory effects of 1,25-dihydroxyvitamin D3 on human B cell differentiation. J Immunol. 2007;179(3):1634–1647. doi:10.4049/jimmunol.179.3.1634
29. Heine G, Anton K, Henz BM, Worm M. 1alpha,25-dihydroxyvitamin D3 inhibits anti-CD40 plus IL-4-mediated IgE production in vitro. Eur J Immunol. 2002;32(12):3395–3404. doi:10.1002/1521-4141(200212)32:12<3395::AID-IMMU3395>3.0.CO;2-#
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
