Back to Journals » Journal of Inflammation Research » Volume 16
Clinical Characteristics of Myasthenia Gravis Patients with COVID-19 in Guangxi, China: A Case–Control Study
Authors Zhou S , Wen Y, Liu C, Zhong J, Liang M, Wu Y, Lv S , Gong Z , Lao D, Li T , Lu T, Tang J, Mo X, Huang W
Received 29 April 2023
Accepted for publication 8 July 2023
Published 26 July 2023 Volume 2023:16 Pages 3157—3168
DOI https://doi.org/10.2147/JIR.S419307
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Shaodan Zhou,1 Yishuang Wen,1 Chao Liu,1 Jian Zhong,1 Manli Liang,1 Yu Wu,2 Sirao Lv,1 Zhuowei Gong,1 Dayuan Lao,1 Taiyan Li,1 Ting Lu,1 Jingqun Tang,1 Xuean Mo,1 Wen Huang1
1Department of Neurology, the First Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi, People’s Republic of China; 2University of Pittsburgh School of Medicine, Pittsburgh, PA, USA
Correspondence: Wen Huang, Department of Neurology, The First Affiliated Hospital of Guangxi Medical University, No. 6 Shuangyong Road, Nanning, Guangxi, 530021, People’s Republic of China, Tel +86-771-5356504, Fax +86-771-5350031, Email [email protected]
Purpose: With the adjustment of prevention strategies in December 2022, coronavirus disease 2019 (COVID-19) became widely prevalent in China. This study is aimed to describe the clinical characteristics of myasthenia gravis (MG) patients with COVID-19 and identify risk factors of exacerbation in MG patients with COVID-19 in Guangxi.
Patients and Methods: A total of 489 MG patients and 587 control subjects in Guangxi during the COVID-19 pandemic were enrolled in this case–control study. After contacting the participants, the clinical data of MG patients and the control group were analyzed. The clinical characteristics of MG patients with COVID-19 were described. Multivariable logistic regression analysis was used for discovering independent risk factors of MG exacerbation in the patients with MG and COVID-19.
Results: A total of 311 (75.30%) MG patients and 428 (72.91%) control subjects were infected with COVID-19, and 64.31% of MG patients with COVID-19 were women. The median age at the time of interview was 41 (IQR: 28, 54) years old, and median onset age was 36 (IQR: 24, 51), both of which were lower than those in MG patients without COVID-19. MG duration was 24 (IQR: 9, 72) months. About 44.69% of patients were generalized MG (GMG). About 11.90% of MG patients with COVID-19 showed severe COVID-19 symptoms and the duration of symptomatic COVID-19 was 9.57 ± 6.79 days, higher than those in the control group. About 35.69% MG patients with immunosuppressive drugs were infected with COVID-19, which is higher than those in the non-infected MG patients (21.57%). A total of 120 (38.59%) MG patients with COVID-19 had comorbidities. About 21 (20.19%) of the 104 MG patients without vaccination showed severe COVID-19 symptoms. Multivariable logistic regression analysis showed that baseline MG activities of daily living profile (MG-ADL, OR 1.280, 95% CI: 1.010– 1.621, p = 0.041), duration of COVID-19 (OR 1.158, 95% CI: 1.100– 1.220, p < 0.001), GMG (OR 2.331, 95% CI: 1.228, 4.426, p = 0.010), and lack of COVID vaccination (OR 2.075, 95% CI: 1.152, 3.738, p = 0.015) were independent factors of exacerbation in MG patients with COVID-19.
Conclusion: MG patients with immunosuppressive drugs, younger onset, longer MG duration, or comorbidities are more susceptible to COVID-19. The baseline MG-ADL, duration of symptomatic COVID-19, GMG, and lack of COVID-19 vaccination are independent risk factors of exacerbation in MG patients with COVID-19.
Keywords: myasthenia gravis, COVID-19, exacerbation, vaccination, clinical characteristics
Introduction
Myasthenia gravis (MG) is an autoimmune neuromuscular disorder, which affects the neuromuscular junction. Autoantibodies against the acetylcholine receptor (AChR), muscle-specific tyrosine kinase (MuSK), low-density lipoprotein receptor-related protein 4 (LRP4), and ryanodine receptor (RyR) are found to be related to MG. Fatigability and muscle weakness which relieve after rest are the main clinical manifestations, sometimes accompanied by thymoma or thymic hyperplasia. The MG patients can be divided into ocular myasthenia gravis (OMG) and GMG, according to the clinical phenotype. A variable percentage of OMG patients can develop into GMG. Cholinesterase inhibitor, prednisolone, and immunosuppressive drugs are the primary treatments for MG. A recent study suggested that the incidence rate of MG in China was approximately 0.68 per 100,000 person-years, and admission death rate was about 14.69‰.1 Exacerbation of disease is frequent in MG patients. Myasthenic crisis occurs due to exacerbation of respiratory muscle weakness, which is the main cause of death in MG patients. On the other hand, research showed that infection was one of the major reasons for the exacerbation of MG symptoms.2,3
Coronavirus disease 2019 (COVID-19) is an acute infectious disease of the respiratory system caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The clinical manifestation of COVID-19 varies from mild to severe. The common symptoms include fever, fatigue, cough, weakness, pharyngalgia, muscular pain, etc. Severe patients may develop pneumonia or even respiratory failure.4 In addition to causing respiratory symptoms, studies had reported that SARS-CoV-2 had effects on the central and peripheral nervous system, such as multiple sclerosis (MS), MG, epilepsy, headache, Parkinson’s disease, Guillain-Barre syndrome, etc.5,6 Some studies had reported the impact of COVID-19 in MG patients and considered MG or immunosuppressive therapy in MG patients as risk factors for severe COVID-19.7 It was suggested that the infection of SARS-CoV-2 might increase the risk of MG exacerbation, MG onset, MG crisis, and respiratory failure.8 Nevertheless, the virus had been constantly variating since the global pandemic of COVID-19 in 2019, thus the characteristics of the virus have also changed. With the adjustment of prevention strategies since the beginning of December 2022, COVID-19 became widely prevalent in China from November 2022 to February 2023. In this study, MG patients in Guangxi (a province in Southern China) were investigated to describe the clinical characteristics of MG patients with COVID-19 and identify risk factors of MG exacerbation in MG patients during the infection of COVID-19.
Materials and Methods
Patients
This case–control study was conducted by the First Affiliated Hospital of Guangxi Medical University. A total of 489 MG patients who visited the outpatient clinic of Neurology from January 1st, 2022, to February 28th, 2023, were enrolled to the study, and 76 MG patients were excluded from the study for loss of contact. Meanwhile, 587 control subjects (age and sex matched) from the physical examination center or the outpatient clinic were randomly recruited in this study. Control subjects with immune diseases were excluded. Therefore, 413 MG patients and 587 control subjects were investigated in this study (Figure 1). MG diagnosis was based on typical clinical symptoms and one or more of the following: positive antibodies against AChR or MuSK, neural electrophysiological findings of decreased compound muscle action potential after repetitive nerve stimulation, positive response to the neostigmine test, according to Chinese guidelines for diagnosis and treatment of MG (2020). The Myasthenia Gravis Foundation of America (MGFA) clinical classification which divided MG patients into five groups was used to rank the severity of MG symptoms. In addition, the severity of disease was assessed by MG-ADL and Quantitative MG Score (QMGS). MG exacerbation was defined as deterioration according to the MGFA clinical classification, MG-ADL score increasing at least 2 points, or QMGS increasing at least 3 points.
 |
Figure 1 Study flowchart. Abbreviations: MG, myasthenia gravis; COVID-19, coronavirus disease 2019. |
The infection of COVID-19 was confirmed by positive results of nasopharyngeal swab polymerase chain reaction (PCR) testing for SARS-CoV-2, nasopharyngeal swab SARS-CoV-2 antigen testing, or typical clinical symptoms after close contact with COVID-19 patients. According to the severity of COVID-19 symptoms, we classified the patients with COVID-19 into 1 to 7 point scales.9 The severity of COVID-19 symptoms include: asymptomatic COVID-19 (1), isolated symptoms, such as anosmia, headache, dizzy, and pharyngalgia (2), mild infection symptoms, such as fever, cold, and cough (3), influenza-like infection without hospital admission (4), hospitalized patients with proven COVID-19 pneumonia requiring oxygen therapy (5), severe COVID-19 pneumonia with mechanical ventilation (6), and death due to COVID-19 (7).
The study was approved by the ethics committee of the First Affiliated Hospital of Guangxi Medical University (2023-E141-01).
Clinical Data Collection
The clinical data of MG patients before COVID-19 infection were obtained from their last visit records. The clinical data included demographics, MG symptoms, MGFA classification, clinical phenotype, antibodies against AChR or MuSK, treatments of MG (pyridostigmine, prednisolone and immunosuppressive drugs), baseline MG-ADL, baseline QMGS, thymus status, comorbidities (such as hypertension, diabetes, coronary heart disease, chronic lung disease, tumor, immune disease, hepatitis, gastritis), etc. All participants were contacted from January 1st to February 28th, 2023, by telephone, video call, or face-to-face interview. All questionnaires were not anonymous. The questionnaires included demographics, history of illness, smoking, vaccination status, the COVID-19 symptoms, duration, hospitalization, ICU admission, severity of COVID-19, MG symptoms during the COVID-19, treatments, MGFA class after the COVID-19, CT scans, MG-ADL, QMGS, outcomes, etc.
Statistical Analysis
Numerical variables conforming to the normal distribution are described as mean and standard deviation, otherwise as the median and interquartile range (IQR). Categorical variables are described as n (%). Categorical data were analyzed by using Chi-squared test or Fisher’s exact test, while numerical data using independent-t test or Mann-Whitney test. P values <0.5 were considered significant. In addition, multivariable logistic regression analysis was performed with MG exacerbation in MG patients with COVID-19 as the outcome. The significant factors (including vaccination status, clinical type, antibody status, MGFA class pre-COVID-19, baseline MG-ADL, baseline QMGS, COVID-19 duration, age at the time of interview, and age at onset) associated with MG exacerbation were used as model predictors to determine which variables were independent risk factors of exacerbation in MG patients with COVID-19. Statistical analyses were performed using SPSS 21 and GraphPad prism 8.0.
Results
Characteristics of COVID-19 Infection in MG Patients
The characteristics of COVID-19 infection in MG patients were shown in Table 1. Among 413 MG patients and 587 control subjects, 311 (75.30%) MG patients and 428 (72.91%) control subjects were infected with COVID-19 (p = 0.391). Two hundred of 311 (64.31%) MG patients with COVID-19 were women. There was no statistical significance in demographics between MG patients with COVID-19 and the control group. The course of COVID-19 was 9.57 ± 6.79 days in MG patients, which was longer than that in the control group (7.79 ± 5.59, p < 0.001). Of the 311 MG patients with COVID-19, 25 (8.04%) showed scores 1–2 of the severity of COVID-19 infection, 249 (80.06%) were scores 3–4, and 37 (11.90%) were scores more than 4. In the control group, 56 (13.08%) participants were scores 1–2, 369 (86.22%) were scores 3–4, and only 3 (0.70%) were scores more than 4; this is significantly different from MG patients (p < 0.001). More MG patients with COVID-19 (11.90%, 37/311) were hospitalized, compared to control subjects with COVID-19 (0.70%, 3/428, p < 0.001). However, there was no significant difference in the length of hospital stays (p = 0.106) between the MG patients (14.46± 8.39) and the control group (6.33± 1.15). Of 311 MG patients with COVID-19, 15 (4.92%) MG patients were admitted to the ICU, 14 (4.50%) needed mechanical ventilation, and 3 (0.96%) died of respiratory failure.
 |
Table 1 Characteristics of COVID-19 Infection in MG Patients |
Baseline Clinical Characteristics of MG Patients with COVID-19
The baseline clinical characteristics of MG patients with COVID-19 were shown in Table 2. In MG patients, there was no significant difference in smoking history and demographics (except age at the time of interview and age at onset) between the patients with or without COVID-19. The median age at the time of interview was 41 years old (IQR: 28, 54) and the median age at onset was 36 years old (IQR: 24, 51) in MG patients with COVID-19. The median age at the time of interview and the median age at onset in MG patients without COVID-19 was 52 (IQR: 35, 61.25) and 48 (IQR: 33, 58). The median MG duration of patients with COVID-19 was 24 months (IQR: 9, 72), which was significantly higher than those without COVID-19 (meidan13.5, IQR: 6, 48, p = 0.013). In terms of clinical phenotype, as well as antibody, vaccination, and thymus status, there was no significant difference between the two groups. In the MG treatments before COVID-19, 235 (75.56%) MG patients with COVID-19 were treated with pyridostigmine, 158 (50.80%) with prednisolone, and 111 (35.69%) with immunosuppressive drugs (62 with azathioprine, 5 with mycophenolate mofetil, 45 with tacrolimus). In the non-infected group, 76 (74.51%) MG patients were treated with pyridostigmine, 59 (57.84%) with prednisolone, and only 22 (21.57%) with immunosuppressive drugs (10 with azathioprine, 3 with mycophenolate mofetil, 9 with tacrolimus). The number of patients using immunosuppressive therapy in the infected group was significantly higher than that in patients without infection (p = 0.008). More MG patients (19.94%, 62/311) with COVID-19 were on azathioprine (AZA), compared to patients without COVID-19 (10.87%, 10/102, p = 0.046). About 38.59% (120/311) of MG patients with comorbidities were infected with COVID-19. This percentage was higher than that in MG patients without COVID-19 (27.45%, 28/102, p = 0.044). The baseline MG-ADL and QMGS were 2.55± 2.35 and 3.44± 3.40 in MG patients with COVID-19, whereas they were 2.75± 2.54 and 4.02± 3.73 in MG patients without COVID-19. There is no significant difference between these two groups (p > 0.05).
 |
Table 2 Baseline Clinical Characteristics of MG Patients with or Without COVID-19 |
Features of MG Exacerbation in MG Patients with COVID-19
The features of MG exacerbation in MG patients with COVID-19 were shown in Table 3. The deterioration of MG symptoms had occurred in 105 (33.76%, 105/311) patients with COVID-19. There was no significant difference between the patients with exacerbation and without exacerbation in demographics, MG treatment, thymus status, comorbidities, and MG duration. In the group of MG patients who experienced an exacerbation of symptoms, 45.71% (48/105) were not vaccinated. The proportion was significantly higher than in MG patients without exacerbation (27.18%, 56/206). More MG patients (64.76%, 68/105) with exacerbation were classified as GMG, compared to MG patients without exacerbation (34.47%, 71/206, p < 0.001). Positive antibodies against AChR (82.52%, 85/105) or MuSK (7.77%, 8/105) in MG patients with exacerbation were significantly higher than those in MG patients without exacerbation (AChRab+: 76.24%, 154/206; MuSKab+: 2.97%, 6/206; p = 0.013). The baseline MG-ADL (3.41 ± 2.84) and QMGS (4.68 ± 4.05) in MG patients with exacerbation were significantly higher than MG-ADL (2.12 ± 1.92) and QMGS (2.82 ± 2.83) in MG patients without exacerbation (p < 0.001). According to the MGFA clinical classification classes, 11.43% MG patients with exacerbation were class III or more before COVID-19, significantly higher than those without exacerbation (4.37%, 9/206, p = 0.019). The course of symptomatic COVID-19 in MG patients with exacerbation was 13.61 ± 8.09 days, almost twice of that (7.53 ± 4.91) in MG patients without exacerbation (p < 0.001).
 |
Table 3 Features of MG Exacerbation in MG Patients with COVID-19 |
In addition, multivariable logistic regression analysis showed that baseline MG-ADL (OR 1.280, 95% CI: 1.010–1.621, p = 0.041), duration of symptomatic COVID-19 (OR 1.158, 95% CI: 1.100–1.220, p < 0.001), GMG (OR 2.331, 95% CI: 1.228, 4.426, p = 0.010), and lack of COVID-19 vaccination (OR 2.075, 95% CI: 1.152, 3.738, p = 0.015) were the independent risk factors of MG exacerbation in MG patients with COVID-19 (Table 4).
 |
Table 4 Multivariable Logistic Regression Analysis of Predictors for Exacerbation in MG Patients with COVID-19 |
Impact of COVID-19 Vaccination in MG Patients with the COVID-19
Impact of COVID-19 vaccination in MG patients with COVID-19 was shown in Table 5. MG patients with COVID-19 were divided into two groups: those with and without COVID-19 vaccination. Of the 104 MG patients without vaccination, 21 (20.19%) showed severe symptoms of COVID-19 and were admitted to the hospital, of which 8 (7.64%) were admitted to ICU. The rate of hospitalization was higher than that in MG patients with vaccination (p = 0.001). However, the ICU admission rate in patients with vaccination was not significantly different from those in patients without vaccination (p = 0.094). The length of hospitalization stays, ICU stays, and duration of symptomatic COVID-19 infection were not significantly different between the two groups.
 |
Table 5 Impact of Vaccination in MG Patients with the COVID-19 |
Characteristics of Hospitalized MG Patients with COVID-19
Characteristics of hospitalized MG patients with COVID-19 were shown in Table 6. The median age at onset was 44 years old (IQR: 29, 53.5) in the MG patients who were hospitalized, significantly higher than those in non-hospitalized patients (35, IQR: 23, 50.5, p = 0.041). The duration of symptomatic COVID-19 was 13.60 ± 8.09 days in the hospitalized group, which was higher than non-hospitalized patients (7.53 ± 4.91, p < 0.001). Among 37 hospitalized MG patients with COVID-19, 20 (54.05%) had comorbidities, which was significantly different from the non-hospitalized group (36.90%, 100/274, p = 0.040). MG symptoms of 33 (89.19%) hospitalized MG patients with COVID-19 worsened during the pandemic. Seven (18.92%) hospitalized patients were classified as MGFA class III or more before the pandemic. The baseline MG-ADL (3.97 ± 3.11) and QMGS (5.84 ± 4.69) of hospitalized MG patients were significantly higher than those in the non-hospitalized group (MGFA class ≥ class III: 5.11%, MG-ADL: 2.36 ± 2.17, QMGS: 3.12 ± 3.06, p < 0.05). Of 37 hospitalized MG patients with COVID-19, 3 (8.11%, 3/37) died after admission to the ICU.
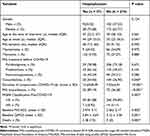 |
Table 6 Characteristics of Hospitalized MG Patients with the COVID-19 |
Discussion
Though the COVID-19 pandemic has lasted for 3 years, knowledge about MG patients infected with COVID-19 is still insufficient. There are few studies on the infection of COVID-19 in MG patients in China after the adjustment of prevention strategies since the beginning of December 2022. A cohort study showed that MG may be a high-risk factor for serious COVID-19 infections.10 However, Businaro had discovered that the infection rate of COVID-19 in MG patients was similar to the general population in Italy in 2020.11 In our study, there was no significant difference in the incidence rate of COVID-19 infection between MG patients and the control group, which is consistent with previous studies. However, the course of symptomatic COVID-19 was longer and the symptoms were more serious in MG patients. The rates of hospitalization and ICU admission were 11.90% and 4.92%, respectively, which were higher than those in the control group. Although there was no statistical difference in hospitalization stays between MG patients and the control group, hospitalization stays in MG patients were longer. Unfortunately, 3 of 37 (8.11%) hospitalized MG patients with COVID-19 died of respiratory failure after admission to the ICU. The results of our study are in accordance with the Chinese Center for Disease Control and Prevention, which declared that MG patients with SARS-CoV-2 were more likely to be admitted to the hospital or the ICU, and have a higher mortality rate than the general population.7 However, previous studies in 2020 showed that 87% hospitalized MG patients with COVID-19 were admitted to the ICU and 30% died, indicating a mortality rate higher than in our study (8.11%).12 The probable cause of this phenomenon is that the virus has been constantly variating. In this most recent variant, the pathogenicity of SARS-CoV-2 reduced and the symptoms were milder than the earlier variants.13,14
Our study found that MG patients whose onset age is younger or have longer MG duration were more susceptible to SARS-CoV-2 and more likely to develop symptomatic COVID-19, which is in accordance with a previous study in 2021.15 The most possible explanation is that younger patients have more active immune systems, which are easier to be activated and initiate cytokine storms. A number of studies suggested that COVID-19 patients had increased levels of inflammatory cytokines during SARS-CoV-2 infection, which was closely related to the development and progression of COVID-19 syndrome.16–18 In our study, some (35.69%) MG patients treated with immunosuppressive agents before infection were more susceptible to COVID-19, but immunosuppressive agents were not related to MG exacerbation and hospitalization. However, previous studies11,19–21 showed that immunosuppressive drugs had no impact on the infection of SARS-CoV-2. Some guidelines suggested that existing immunosuppressive agents were probably safe and should not be stopped when MG patients were infected with COVID-19.22,23 Sole found that immunosuppressive agents were not an independent high-risk factor for COVID-19, although it was significant in single-factor analysis.24 A possible reason is that the types of immunosuppressive drugs used in MG patients in our study were different from these studies. Among 311 MG patients infected with SARS-CoV-2 in the current study, 45 (14.47%) were undergoing treatment with tacrolimus. However, few patients used tacrolimus in previous studies. Furthermore, some studies showed that immunosuppressive drugs were associated with higher mortality rate in chronic immune diseases with COVID-19 infection.10,25 The impact of immunosuppressive therapy on COVID-19 is uncertain, so individualized treatment plans should be used for MG patients during the COVID-19 pandemic. Of 311 MG patients with COVID-19, 120 (38.59%) had comorbidities, including cancer, immune diseases, hypertension, diabetes, coronary heart disease, hepatitis, chronic obstructive pulmonary disease, etc. The rate of comorbidities in MG patients with COVID-19 was higher than MG patients without COVID-19. This is consistent with previous studies,11,26 which had found that MG patients with comorbidities were more likely to be infected with COVID-19. On the other hand, we found that comorbidities were not related to hospitalization and exacerbation in MG patients during the pandemic, which is consistent with Karimi’s study.27
In our study, 48 (45.71%) of 105 patients with MG exacerbation were not vaccinated before infection with COVID-19, higher than those in the patients without MG exacerbation. A further analysis showed that vaccination status was related to the severity of COVID-19. The multivariable logistic regression analysis showed that lack of COVID-19 vaccination was an independent risk factor for the exacerbation in MG patients with COVID-19 (OR 2.075, 95% CI: 1.152, 3.738, p = 0.015). COVID-19 vaccination is a possible protective factor for exacerbation and hospitalization of MG patients during COVID-19 pandemic. Our results are consistent with a study in Greece,28 which had found that vaccines might reduce hospitalization rate of MG patients with COVID-19. Nevertheless, our study found that vaccination cannot reduce the length of hospitalization and ICU stay. Studies had confirmed the safety and effectiveness of the COVID-19 vaccine in MG patients. Therefore, it is recommended that MG patients should be vaccinated, if they have no contraindications.23,29–31 Our study showed that MG symptoms of the patients classified as GMG or higher MGFA class were more likely to face exacerbation of MG when they were infected with SARS-CoV-2. The baseline MG-ADL scores and QMGS of MG patients with exacerbation during the COVID-19 pandemic were higher than those in MG patients without exacerbation. The course of symptomatic COVID-19 was prolonged in MG patients with exacerbation. Previous studies had shown that MG exacerbation was significantly related to infection of COVID-19.15,24,32 The multivariable logistic regression analysis in our study showed that baseline MG-ADL, duration of symptomatic COVID-19, GMG, and lack of COVID-19 vaccination were the independent risk factors of the MG exacerbation in patients infected with COVID-19. MG-ADL, QMGS and MGFA class are frequently used to evaluate the severity of MG. Higher scores of MG-ADL, QMGS, and MGFA class indicate more serious cases of MG. MG is an autoimmune neuromuscular disease and characterized by muscular weakness. Severe MG may possibly include respiratory muscle weakness and dysregulation of the immune system. Similarly, severe COVID-19 may also cause muscular weakness and dysregulation of immune system. For patients with severe MG, cytokine storms caused by COVID-19 infection may have aggravated their immune system disorder.8 In the exacerbation group, antibodies against AChR were positive in 82.52% of MG patients and antibodies against MuSK were positive in 7.77% of MG patients, higher than those in MG patients without exacerbation. The most possible explanation for this phenomenon is the potential antigenic similarity of AChR and the receptors of SARS-CoV-2. A sequence of SARS-CoV-2 spike protein is similar to neurotoxins, which can bind nicotinic acetylcholine receptors (nAChR) and disrupt the activity of the cholinergic system.33 Furthermore, there are studies that reported new onset MG following the infection of SARS-CoV-2 or vaccination of COVID-19.34,35 This new onset MG is usually accompanied by hyperthyroidism, thymoma, or thymic hyperplasia. Patients with new onset of MG might already have existing immune system disorders. After the infection of COVID-19, cytokine storms from the infection may have exacerbated these pre-existing disorders.
The analysis of the characteristics of hospitalized MG patients with the COVID-19 showed that 37 (11.9%) MG patients were admitted to the hospital. Of these, 20 (54.05%) had comorbidities and 33 (89.19%) had MG exacerbation, which is a higher percentage than those in non-hospitalized patients. Moreover, MGFA class before infection, baseline MG-ADL, and QMGS were also higher in hospitalized patients. These results suggested that the severity of MG before COVID-19 infection is related to with hospitalization after infection of COVID-19, being in accordance with previous studies.15,32 The course of symptomatic COVID-19 in hospitalized MG patients was prolonged. Therefore, age at onset, comorbidities, course of COVID-19, MGFA class, MG-ADL, QMGS before COVID-19, and MG exacerbation during COVID-19 might be related to hospitalization of MG patients with COVID-19.
Limitations
Our study has some limitations. Firstly, all subjects in our study came from the same hospital in Guangxi. Secondly, there were few cases of MG patients with COVID-19 in Guangxi before this pandemic, so this study will not be able to compare the characteristics of different variants of COVID-19. Moreover, the study lacks long-term follow-up of MG patients with COVID-19.
Conclusions
There was no significant difference between MG patients and the control group in the incidence rate of COVID-19 infection. However, MG patients with COVID-19 faced more severe symptoms. They had longer course of COVID-19, higher hospitalization rate, and higher ICU admission rate. Immunosuppressive therapy, onset age, MG duration, and comorbidities were related to higher infection rate of COVID-19. COVID-19 vaccination can possibly protect MG patients from severe COVID-19 and MG exacerbation, while reducing hospitalization rate during infection of COVID-19. Some MG patients with COVID-19 developed severe symptoms and were admitted to the hospital, even requiring ICU admission and mechanical ventilation. Most patients showed outcomes of recovery, but 3 (0.96%) of 311 MG patients with COVID-19 died of the respiratory failure. The baseline MG-ADL, duration of symptomatic COVID-19, GMG, and lack of COVID-19 vaccination were the independent risk factors of MG exacerbation in patients with COVID-19.
Abbreviations
MG, myasthenia gravis; COVID-19, coronavirus disease 2019; ICU, intensive care unit; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; MG-ADL, myasthenia gravis activities of daily living profile; GMG, generalized myasthenia gravis; OR, odds ratio; CI, confidence interval; AChR, acetylcholine receptor; MuSK, muscle-specific tyrosine kinase; LRP4, low-density lipoprotein receptor-related protein 4; RyR, ryanodine receptor; OMG, ocular myasthenia gravis; MS, multiple sclerosis; MGFA, Myasthenia Gravis Foundation of America; QMGS, Quantitative myasthenia gravis Score; PCR, polymerase chain reaction; IQR, interquartile range; AChRab+, anti-acetylcholine receptor antibody positive; MuSKab+, anti-muscle-specific tyrosine kinase positive; AZA, azathioprine; MMF, mycophenolate mofetil.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
This study was approved by the Medical Ethics Committee of the First Affiliated Hospital of Guangxi Medical University, Guangxi, China (2023-E141-01). All procedures were performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Written informed consents were obtained from all the participants enrolled in this study.
Acknowledgments
The authors cordially thank the participants and their families.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the National Natural Science Foundation of China (82060236) and the Natural Science Foundation of Guangxi Province (CN) (2017GXNSFAA198042, 2019GXNSFDA245032).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Chen J, Tian DC, Zhang C, et al. Incidence, mortality, and economic burden of myasthenia gravis in China: a nationwide population-based study. Lancet Reg Health West Pac. 2020;5:100063. doi:10.1016/j.lanwpc.2020.100063
2. Gummi RR, Kukulka NA, Deroche CB, Govindarajan R. Factors associated with acute exacerbations of myasthenia gravis. Muscle Nerve. 2019;60(6):693–699. doi:10.1002/mus.26689
3. Nelke C, Stascheit F, Eckert C, et al. Independent risk factors for myasthenic crisis and disease exacerbation in a retrospective cohort of myasthenia gravis patients. J Neuroinflammation. 2022;19(1):89. doi:10.1186/s12974-022-02448-4
4. Umakanthan S, Sahu P, Ranade AV, et al. Origin, transmission, diagnosis and management of coronavirus disease 2019 (COVID-19). Postgrad Med J. 2020;96(1142):753–758. doi:10.1136/postgradmedj-2020-138234
5. Dewanjee S, Vallamkondu J, Kalra RS, et al. Emerging COVID-19 neurological manifestations: present outlook and potential neurological challenges in COVID-19 pandemic. Mol Neurobiol. 2021;58(9):4694–4715. doi:10.1007/s12035-021-02450-6
6. Shah SMI, Yasmin F, Memon RS, et al. COVID-19 and myasthenia gravis: a review of neurological implications of the SARS-COV-2. Brain Behav. 2022;12(12):e2789. doi:10.1002/brb3.2789
7. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in china: summary of a report of 72 314 cases from the Chinese center for disease control and prevention. JAMA. 2020;323(13):1239–1242. doi:10.1001/jama.2020.2648
8. Tugasworo D, Kurnianto A, Andhitara Y, et al. The relationship between myasthenia gravis and COVID-19: a systematic review. Egypt J Neurol Psychiatr Neurosurg. 2022;58(1):83. doi:10.1186/s41983-022-00516-3
9. Jakubikova M, Tyblova M, Tesar A, et al. Predictive factors for a severe course of COVID-19 infection in myasthenia gravis patients with an overall impact on myasthenic outcome status and survival. Eur J Neurol. 2021;28(10):3418–3425. doi:10.1111/ene.14951
10. Kassardjian CD, Widdifield J, Paterson JM, et al. Serious infections in patients with myasthenia gravis: population-based cohort study. Eur J Neurol. 2020;27(4):702–708. doi:10.1111/ene.14153
11. Businaro P, Vaghi G, Marchioni E, et al. COVID-19 in patients with myasthenia gravis: epidemiology and disease course. Muscle Nerve. 2021;64(2):206–211. doi:10.1002/mus.27324
12. Camelo-Filho AE, Silva AMS, Estephan EP, et al. Myasthenia Gravis and COVID-19: clinical Characteristics and Outcomes. Front Neurol. 2020;11:1053. doi:10.3389/fneur.2020.01053
13. Fan Y, Li X, Zhang L, et al. SARS-CoV-2 Omicron variant: recent progress and future perspectives. Signal Transduct Target Ther. 2022;7(1):141. doi:10.1038/s41392-022-00997-x
14. Suzuki R, Yamasoba D, Kimura I, et al. Attenuated fusogenicity and pathogenicity of SARS-CoV-2 Omicron variant. Nature. 2022;603(7902):700–705. doi:10.1038/s41586-022-04462-1
15. De Leon AM, Aban I, McPherson T, et al. Impact of the COVID-19 pandemic on patients with myasthenia gravis: a survey of the myasthenia gravis foundation of America MG patient registry. Muscle Nerve. 2023;67(1):25–32. doi:10.1002/mus.27743
16. Zanza C, Romenskaya T, Manetti AC, et al. Cytokine Storm in COVID-19: immunopathogenesis and Therapy. Medicina. 2022;58(2). doi:10.3390/medicina58020144
17. Tutal Gursoy G, Yuksel H, Mulkem Simsek I, et al. Neurological presentations in patients with COVID-19 in cytokine storm. Can J Neurol Sci. 2023;50(1):89–95. doi:10.1017/cjn.2021.247
18. Nasrollahi H, Talepoor AG, Saleh Z, et al. Immune responses in mildly versus critically ill COVID-19 patients. Front Immunol. 2023;14:1077236. doi:10.3389/fimmu.2023.1077236
19. Dotan A, David P, Arnheim D, Shoenfeld Y. The autonomic aspects of the post-COVID19 syndrome. Autoimmun Rev. 2022;21(5):103071. doi:10.1016/j.autrev.2022.103071
20. Octaviana F, Yugo HP, Safri AY, et al. Case series: COVID-19 in patients with mild to moderate myasthenia gravis in a National Referral Hospital in Indonesia. eNeurologicalSci. 2021;23:100332. doi:10.1016/j.ensci.2021.100332
21. Stascheit F, Grittner U, Hoffmann S, et al. Risk and course of COVID-19 in immunosuppressed patients with myasthenia gravis. J Neurol. 2023;270(1):1–12. doi:10.1007/s00415-022-11389-0
22. Zupanic S, Lazibat I, Rubinic Majdak M, Jelicic M. Treatment of myasthenia gravis patients with Covid-19: review of the literature. Acta Clin Croat. 2022;60(3):496–509. doi:10.20471/acc.2021.60.03.21
23. Jacob S, Muppidi S, Guidon A, et al.; International MGC-WG. Guidance for the management of myasthenia gravis (MG) and Lambert-Eaton myasthenic syndrome (LEMS) during the COVID-19 pandemic. J Neurol Sci. 2020;412:116803. doi:10.1016/j.jns.2020.116803
24. Sole G, Mathis S, Friedman D, et al. Impact of coronavirus disease 2019 in a French cohort of myasthenia gravis. Neurology. 2021;96(16):e2109–e2120. doi:10.1212/WNL.0000000000011669
25. Ward D, Gortz S, Thomson Ernst M, et al. The effect of immunosuppressants on the prognosis of SARS-CoV-2 infection. Eur Respir J. 2022;59(4):2100769. doi:10.1183/13993003.00769-2021
26. Ejaz H, Alsrhani A, Zafar A, et al. COVID-19 and comorbidities: deleterious impact on infected patients. J Infect Public Health. 2020;13(12):1833–1839. doi:10.1016/j.jiph.2020.07.014
27. Karimi N, Fatehi F, Okhovat AA, et al. Clinical features and outcomes of patients with myasthenia gravis affected by COVID-19: a single-center study. Clin Neurol Neurosurg. 2022;222:107441. doi:10.1016/j.clineuro.2022.107441
28. Bakirtzis C, Boziki MK, Karakasi MV, Moysiadis T, Grigoriadis N. The impact of SARS-CoV −2 immunization on COVID −19 disease course in people with myasthenia gravis. Muscle Nerve. 2023;67:412–416. doi:10.1002/mus.27805
29. Ruan Z, Tang Y, Li C, et al. COVID-19 vaccination in patients with myasthenia gravis: a single-center case series. Vaccines. 2021;9(10). doi:10.3390/vaccines9101112
30. Lupica A, Di Stefano V, Iacono S, et al. Impact of COVID-19 in AChR myasthenia gravis and the safety of vaccines: data from an Italian cohort. Neurol Int. 2022;14(2):406–416. doi:10.3390/neurolint14020033
31. Farina A, Falso S, Cornacchini S, et al. Safety and tolerability of SARS-Cov-2 vaccination in patients with myasthenia gravis: a multicenter experience. Eur J Neurol. 2022;29(8):2505–2510. doi:10.1111/ene.15348
32. Aktoz G, Boz C, Zengin S, et al. Clinical course and outcome of Covid-19 in patients with myasthenia gravis. Neurol Res. 2023:1–7. doi:10.1080/01616412.2023.2167536
33. Kopanska M, Batoryna M, Bartman P, Szczygielski J, Banas-Zabczyk A. Disorders of the cholinergic system in COVID-19 Era-A review of the latest research. Int J Mol Sci. 2022;23(2). doi:10.3390/ijms23020672
34. Sriwastava S, Tandon M, Kataria S, Daimee M, Sultan S. New onset of ocular myasthenia gravis in a patient with COVID-19: a novel case report and literature review. J Neurol. 2021;268(8):2690–2696. doi:10.1007/s00415-020-10263-1
35. Abicic A, Sitas B, Adamec I, Bilic E, Habek M. New-onset ocular myasthenia gravis after booster dose of COVID-19 vaccine. Cureus. 2022;14(7):e27213. doi:10.7759/cureus.27213
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
