Back to Journals » International Journal of Women's Health » Volume 14
Clinical Characteristics of Hyperandrogenism Include Hirsutism, Polycystic Ovary Syndrome, and Acne: Association with Psychiatric Disease in Women -A Nationwide Population-Based Cohort Study in Taiwan
Authors Wang TM , Chou CH, Lee YL, Chung CH , Huang YC , Lai XC , Sun CA, Kang CY , Wu GJ, Chien WC
Received 26 May 2022
Accepted for publication 10 August 2022
Published 27 August 2022 Volume 2022:14 Pages 1173—1189
DOI https://doi.org/10.2147/IJWH.S376244
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Tsan-Min Wang,1,2 Cheng-Hao Chou,1,2 Yi-Liang Lee,3,4 Chi-Hsiang Chung,1,5,6 Yao-Ching Huang,1,7 Xiao-Cheng Lai,8 Chien-An Sun,9,10 Chieh-Yi Kang,11 Gwo-Jang Wu,1,3,12 Wu-Chien Chien1,5,6,8
1Department of Medical Research, Tri-Service General Hospital, Taipei, Taiwan; 2Taipei Municipal Jianguo High School, Taipei, Taiwan; 3Department of Obstetrics and Gynecology, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan, Republic of China; 4Department of Obstetrics and Gynecology, Kang Ning Hospital, Taipei, Taiwan, Republic of China; 5School of Public Health, National Defense Medical Center, Taipei, Taiwan; 6Taiwanese Injury Prevention and Safety Promotion Association (TIPSPA), Taipei, Taiwan; 7Department of Chemical Engineering and Biotechnology, National Taipei University of Technology (Taipei Tech), Taipei, Taiwan; 8Graduate Institute of Life Sciences, National Defense Medical Center, Taipei, Taiwan; 9Department of Public Health, College of Medicine, Fu-Jen Catholic University, New Taipei City, Taiwan, Republic of China; 10Big Data Research Center, College of Medicine, Fu-Jen Catholic University, New Taipei City, Taiwan, Republic of China; 11Chi Mei Medical Center Gynecologic Oncologist Division, Department of Obstetrics & Gynecology, Tainan City, Taiwan, Republic of China; 12Graduate Institute of Medical Sciences, National Defense Medical Center, Taipei, Taiwan
Correspondence: Gwo-Jang Wu; Chieh-Yi Kang, Email [email protected]; [email protected]
Objective: Previous studies have shown an increased in psychiatric disorders in women with disorders associated with hyperandrogenism, but few nationwide cohorts have studied this phenomenon. Therefore, this study is aimed to examine the association between the clinical manifestations of hyperandrogenism and subsequent psychiatric disorders.
Methods: Based on the National Health Insurance Research Database, 49,770 enrolled participants were matched for age and index date between January 1, 2000, and December 31, 2015. Hirsutism, polycystic ovary syndrome, and acne are characterized by hyperandrogenism. After adjusting for confounding factors, we used Cox proportional analysis to compare the risk of psychiatric disorders during the 16 years of follow-up.
Results: Of all the participants, 1319 (13.25%) had psychiatric disorders in the study group, whereas only 3900(9.80%) had psychiatric disorders in the control group. After adjusting for age, and monthly income, the Cox regression analysis showed that the study patients were more likely to develop psychiatric disorders (hazard ratio [HR]: 2.004, 95% confidence interval [CI] = 1.327– 2.724, P < 0.001). The results demonstrated that women aged 20– 29 years had a more significant risk.
Conclusion: Women with clinical characteristics of hyperandrogenism have a higher risk of developing psychiatric disorders, especially those aged 20– 29 years.
Keywords: hyperandrogenism, psychiatric disorders, national health insurance research database, cohort study, women, Taiwan
Introduction
Previous literature has revealed that hirsutism, polycystic ovary syndrome (PCOS), and acne are linked by an association with hyperandrogenism.1–3 Heidelbaugh (2016) argues that hirsutism is characterized as excessive terminal hair, typically occurring in male growth patterns in the androgen-dependent regions of the female body.1 Moreover, PCOS has been defined using multifarious criteria, including hyperandrogenism, oligoovulation or anovulation, and polycystic ovaries.2,4 Additionally, acne is a characteristic of PCOS.2,3 Consequently, we used three clinical manifestations of hyperandrogenism, including hirsutism, PCOS, and acne, to represent the clinical characteristics of hyperandrogenism in this study.
In the previous research, hirsutism, PCOS, and acne have been linked to an increased risk for subsequent psychiatric disorders.5–8 Brutocao (2018) suggested that PCOS is linked to an increased risk of depression, anxiety, and bipolar disorders after including 57 studies reporting on 172,040 patients.5 A nationwide cohort study in the UK revealed acne is associated with an increased risk of depression.6 In his epidemiological cohort study, Morgan asserted that the prevalence of eating disorders in women with hirsutism has increased.7
In addition to psychological disorders, the present study used other disorders to analyze depression, anxiety, sleep disorders, and eating disorders. Further, we added suicide to the study list of the considered variables.9 Thus far, although numerous population-based studies have been published on the appearance characteristics of hyperandrogenism,10 There has been was a lack of direct analysis of large databases to verify the clinical manifestations of hyperandrogenism and subsequent psychiatric disorders. We hypothesized that a nationwide population-based cohort study utilizing the National Health Insurance Research Database (NHIRD) could examine women with clinical manifestations of hyperandrogenism and the possible risk of psychiatric disorders. Nonetheless, the main limitation of this study is the lack of exact androgen level data. This study aimed to demonstrate the correlation between hirsutism, PCOS, acne, and subsequent psychiatric disorders.
Materials and Methods
Data Source
This study used data from the NHIRD to investigate the association between the three clinical manifestations of hyperandrogenism and psychiatric disorders over a 16-year period.11 As a subset of the NHIRD, the Longitudinal Health Insurance Database of a two million randomized sampled population from 2000 to 2015 was used to study the association between clinical features of hyperandrogenism and the risk of psychiatric disorders.12
The National Health Insurance (NHI) program was launched in Taiwan in 1995. As of June 2009, it included contracts with 97% of medical providers with approximately 23 million beneficiaries or more than 99% of the population.13,14 The NHIRD, which contains all claims data of beneficiaries, uses the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes to record diagnoses.15 The details of the program were documented in a previous study.12
In this study, we used data from the NHIRD to investigate the association between patients with hirsutism (ICD-9-CM: 704.1), PCOS (ICD-9-CM:256.4 and 628.0), acne (ICD-CM:706.1), and psychiatric disorders (ICD-9-CM:290–319) over a 16-year period, from the total hospitalization Longitudinal Health Insurance Database in Taiwan (2000–2015).16
Study Design and Sampled Participants
This study used a population-based, matched-cohort design. This study was observational. Patients newly diagnosed with any of the three clinical manifestations of hyperandrogenism, including hirsutism, PCOS, and acne, were selected from the Longitudinal Health Insurance Database from January 1, 2000, to December 31, 2015. Patients with these diseases before 2000 were excluded from the study. This method could be viewed as a way to ensure that these diseases were recent-onset, with references from other studies on the association between clinical characteristics of hyperandrogenism and psychiatric health, utilizing the NHIRD.17
Additionally, the patients diagnosed with anxiety, depression, bipolar disorders, sleep disorders, posttraumatic stress disorders (PTSD) or acute stress disorders (ASD), dementia, eating disorders, substance-related disorders (SRD), psychotic disorders, autism, other mental disorders, suicide, before 2000, or before their first visit for any one of the three diseases mentioned above were also excluded.18 Of the total patients enrolled, 9954 participants with any of the three clinical manifestations of hyperandrogenism and 39,816 controls were matched for age and index date. Each enrolled participant was required to have made at least three outpatient visits or one inpatient episode in the 1-year study period for any of the three diseases mentioned above, according to the ICD-9-CM codes. Participants fulfilling any of clinical manifestation criteria were referred to the study group; participants without clinical features were referred to the control group (Figure 1).
 |
Figure 1 The flowchart of the study. |
Covariates
The covariates included age groups (≤ 19, 20–44, 45–64, and ≥ 65 years), geographical area of residence (north, center, south, and east of Taiwan), urbanization level of residence (levels 1–4), and monthly income (in New Taiwan Dollars [NT$]; < 18,000, 18,000–34,999,and ≥35,000). The urbanization level of a residence was defined according to the population and various indicators of the level of development.19 Level 1 was defined as a population of > 1,250,000 and a specific designation as political, economic, cultural, and metropolitan development. Level 2 was defined as populations between 500,000 and 1,249,999 and as playing an important role in politics, economy, and culture. Urbanization levels 3 and 4 were defined as a population between 149,999 and 499,999, and <149,999, respectively.20
Comorbidities
Baseline comorbidities included diabetes mellitus (DM; ICD-9-CM: 250), hypertension (HTN; ICD-9CM: 401–405), renal disease (ICD-9-CM: 580–589),hyperlipidemia (ICD-9-CM: 272), thyrotoxicosis (ICD-9-CM: 242), pneumonia (ICD-9-CM: 480–486), chronic liver disease (CLD; ICD-9-CM: 571), injury (ICD-9-CM: 800–999), tumor (ICD-9-CM: 140–208), and obesity (ICD-9-CM: 278.0–278.1). These comorbidities were based on previous population-based literature.21,22
Major Outcome
All study participants were tracked from the index date until the onset of anxiety disorders (ICD-9-CM:300), depression (ICD-9-CM:296.2–296.3, 300.4, and 311), bipolar disorders (ICD-9-CM 296.0, and 296.4–296.8), sleep disorders (ICD-9-CM:307.4 and 780.5), PTSD or ASD (ICD-9-CM:308,309.81), dementia (ICD-9-CM: 290.0, 290.10, 290.11, 290.12, 290.13, 290.20, 290.21, 290.3, 290.41, 290.42, 290.43, 290.8, 290.9, and 331.0), eating disorders (ICD-9-CM:307. 1, 307.5), SRD (ICD-9-CM:291–292, 303.3, 303.9, 304–305), psychotic disorders (ICD-9-CM: 295 and 297–298), autism (ICD-9-CM:299.0), other mental disorders (ICD-9-CM: 290–319 excluding listed above), suicide (ICD-9-CM: E950-E959), withdrew from the NHI program, or the end of 2015. Moreover, each psychiatric diagnosis was required to have made at least three outpatient visits within the 1-year study period for psychiatric disorders, according to the ICD-9-CM codes.15,23
Statistical Analyses
All statistical analyses were performed using SPSS Windows software version 22.0. χ2 and t-tests were used to evaluate the distributions of categorical and continuous variables, respectively.24 The results are presented as hazard ratios (HR) with 95% confidence intervals (CI).25,26 Differences in the risk of psychiatric disorders between the study and control groups were estimated using the Kaplan–Meier method with the Log rank test. Statistical significance was defined as a two-tailed p-value < 0.05.27
Results
Table 1 shows the age, comorbidities, urbanization, area of residence, and monthly insured premiums of the high-androgen females and controls. We identified 9954 patients with clinical manifestations of hyperandrogenism and 39,816 patients without hyperandrogenism. The difference between the two groups was not statistically significant in the distribution of age, renal disease, thyrotoxicosis, pneumonia, chronic liver disease (CLD), injury, tumor, obesity, or season of medical visits. Most patients were under 30 years of age (77.32% in the hyperandrogenism participant group and the non-hyperandrogenism control cohort). The hyperandrogenism cohort had more DM, HTN, and hyperlipidemia cases than the non-hyperandrogenism control cohort. Patients with clinical features of hyperandrogenism tended to pay a higher insurance premium, lived in the northern and central regions of Taiwan, had urbanization levels 1 and 2, and received medical care from hospital centers.
 |  |  |
Table 1 Characteristics of Study in the Baseline |
Of the total 49,770 participants, 1319 were from 9954 (13.25%) in the hyperandrogenism cohort, compared to 3900 from the 39,816 (9.80%) non-hyperandrogenism cohort. Kaplan-Meier survival analysis revealed that the difference in the development of psychiatric disorders was statistically significant (log-rank, p<0.001). (Figure 2)
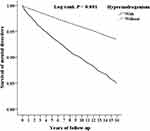 |
Figure 2 Kaplan-Meier for survival of mental disorders among aged 15–49 women stratified by hyperandrogenism with Log rank test. |
Table 2 shows the results of the COX regression analysis: the incidence of psychiatric disorders was higher in the hyperandrogenism group than that in the non-hyperandrogenism control cohort (13.25% vs 9.80%). The Cox regression revealed that the crude HR was 2.267 (95% CI = [1.385,2.916], p < 0.001), and the adjusted HR was 2.004 (95% CI = [1.327, 2.724], p < 0.001) in the risk of psychiatric disorders after adjusting for age, comorbidities, geographical area of residence, urbanization level of the residence, and monthly income. For the subgroup of participants aged 20–29 years, the risk of psychiatric disorders was 1.878 times that of the age group ≤19 years. The results show that those with DM, HTN, renal disease, CLD, injury, and tumors are more likely to suffer from subsequent psychiatric disorders. Additionally, the mean years from clinical features of hyperandrogenism diagnosis to psychiatric disorders were 5.82 ± 5.69 years in the participant group, shorter than 6.06 ± 5.92 years for the control group from tracking the course of psychiatric disorders. (Table 3)
 |
Table 2 Factors of Mental Disorders by Using Cox Regression |
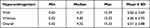 |
Table 3 Years to Mental Disorders |
We analyzed the data by stratifying factors, such as age, urbanization level, geographic areas of residence, seasons of medical visits, monthly insured premiums, and levels of care from medical service providers. We found that different urbanization levels, residence areas, seasons of medical visits, insured premiums, and levels of care were associated with an increased risk of psychiatric disorders. Patients with clinical characteristics of hyperandrogenism between the ages of 20 and 29 years had an increased risk of developing psychiatric disorders Tables 4 and 5 shows the adjusted HR of anxiety with adjusted HR: 2.196, p < 0.001, depression with adjusted HR: 2.389, p < 0.001, bipolar disorders adjusted HR: 2.047, p < 0.001; SRD adjusted HR: 1.933, p <0.001; psychotic disorders adjusted HR: 1.768 p < 0.001, and other mental disorders adjusted HR: 1.997, p <0.001 in patients with three clinical manifestations of hyperandrogenism when compared to the patients without clinical characteristics of hyperandrogenism. Surprisingly, we found that eating disorders were significant. Nonetheless, there was no statistical significance when the first year was excluded, and there was statistically a significant difference when the first five years were excluded.
 |
Table 4 Factors of Mental Disorders Stratified by Variables Listed in the Table by Using Cox Regression |
 |
Table 5 Factors of Mental Disorders Subgroups by Using Cox Regression |
Overall, the differences between people with and without psychiatric disorders, including hirsutism, PCOS, and acne were statistically significant. Nevertheless, the difference in the hirsutism and acne subgroups was not statistically significant; the p-values for hirsutism and acne were 0.342 and 0.053 respectively. The adjusted HR values of all subgroups, including hirsutism and acne, were greater than 1. For PCOS, the adjusted HR values were 3.165. (Table 6)
 |
Table 6 Factors of Mental Disorders Among Different Hyperandrogenism Subgroups by Using Cox Regression |
Discussions
This study examined the association between three clinical manifestations of hyperandrogenism and the risk of psychiatric disorders. After adjusting for covariates, the adjusted HR was 2.004 for the participants (95% CI = 1.327–2.724, p < 0.001) compared to the control group. Kaplan–Meier analysis demonstrated that the study participants had a significantly higher 16-year psychiatric disorders-free survival rate than controls.
Using the two million NHIRD with the advantage of a larger dataset, our study confirmed the association between three clinical manifestations of hyperandrogenism and the increased risk of depressive disorder, bipolar disorder, anxiety disorders, and sleep disorders. Our study excluded patients and controls with psychiatric disorders before the follow-up period. Patients with clinical characteristics of hyperandrogenism were associated with a higher risk of overall psychiatric disorders than the control group, especially anxiety, depression, bipolar disorders, SRD, and other mental disorders. In this group, hyperandrogenism was associated with an increased risk of overall psychiatric disorders, especially depression and anxiety. Therefore, regular psychiatric follow-up may be vital for patients with hyperandrogenism.10,28
Our study did not find an association between the clinical characteristics of hyperandrogenism and suicide, which may be due to several reasons. Suicidal ideation occurs more frequently in women than in men; nevertheless, men are more likely to commit suicide than woman.29,30 Utilizing the NHIRD, we could not count patients with suicidal ideation, which may have affected the results of this study. A previous article suggested that androgens in men are a risk factor for completed suicide.30,31 However, our study included only women, which may be a critical reason for the lack of statistical significance due to sex differences. The underlying association between androgens and suicide requires clarification in future research. Most previous population-based studies on psychiatric morbidity were related to patients with hirsutism, PCOS, or acne.10 Therefore, to the best of our knowledge, this is the first population‐based study on the incidence of psychiatric disorders with clinical manifestations of hyperandrogenism.
A crucial question is whether the increased risk of psychiatric disorders after exposure to high androgen levels is associated with high androgen levels. Previous animal studies have shown that supraphysiological doses of androgens contribute to neurodegeneration, decreased brain-derived neurotrophic factors, increased inflammation, and increased neuronal density, which may correspond to changes in mood, cognition, and aggression.32 Neural alterations likely play a role in the common mental health problems in patients with high androgen levels.33 The total cerebral cortex volume of people with high androgen levels was more compact than that of controls.34 A trophy of the cerebral cortex is a risk factor. Specifically, the brain neurons of patients with high androgen levels may have become atrophied.35 Although the mechanism between the atrophied brain and high androgen levels is yet to be clarified, there is a dose-response relationship.32 Further, patients with high androgen levels are more likely to develop cerebrovascular problems.36 Epidemiological studies have confirmed high comorbidity between cerebrovascular problems and psychiatric disorders, particularly depression. Comorbidity is bidirectional, and the mechanisms responsible are complex and multifaceted.37 One study indicated that high androgen levels demonstrated more attention-deficit hyperactivity disorder (ADHD) symptoms; however, we do not emphasize this section in this study.38
Table 6 demonstrates that the p-value of hirsutism is 0.342, which is far from the significance standard, although there is an association between hirsutism and psychiatric disorders in previous studies.39 The number of patients with hirsutism is far less than that of patients with PCOS, which may be an important influencing factor of the p-value. Despite their clinical importance, the prevalence of different pathological conditions associated with androgen excess is not apparent.10 The most recognizable clinical feature of androgen excess may be hirsutism. However, not all patients with hirsutism have overt evidence of androgen excess, with some women suffering from what we understand to be idiopathic hirsutism.40 Nevertheless, the mechanisms underlying idiopathic hirsutism are not completely known.1,41 Alternatively, not all patients with an androgen excess disorder have hirsutism, as in Asian patients with PCOS.42 East Asian females have fewer hirsute compared to Caucasians.42,43 Thus, owing to ethnic differences, it is important to discuss different standards.
Women aged 20–29 years had the highest risk for psychiatric disorders, followed by those aged 30–39 years. In previous studies, compared to females aged >40 years, females aged 20–40 years produced more androgens and testosterone, a type of androgen.44 Women aged 20–29 years secreted more significant amounts of androgens than those between the ages of 30 and 39 years in most previous studies.45 Furthermore, psychiatric disorders were associated with age.46 Although females’ physical function worsens with age; they simultaneously feel less stressed.47 Another reason is that women aged 20–40 years may face the task of reproduction and may come down with psychiatric disorders during this experience.48,49 The mechanisms associated with androgen and psychiatric disorders have not been completely confirmed; consequently, age may be an influencing factor leading to this result.
Hirsutism, PCOS, and acne are risk factors that influence patients’ mental health.50–55 A Poor prognosis included psychiatric disorders and suicide in this study. Women with hirsutism have an increased risk of depression linked to their circulating active testosterone levels.50 Similarly, in Derogatis’ research, the findings indicate that depression in hirsute women is more likely to be affected by a malfunctioning neuroendocrine system than by psychosocial factors.51 The underlying mechanisms of psychopathology are needed to clarify the underlying mechanisms of psychopathology. Daisung et al’s meta-analysis observed a 26% increase risk of suicide deaths and a 17% increase risk of suicide attempts after concluding 32 papers.52 Yin argues that women with PCOS tend to experience a low quality of life and suffer from depression and anxiety after conducting a meta-analysis of 46 studies.53 Cesta suggests that PCOS in women might be a risk factor for psychiatric disorders and attempted suicide.54 However, concerning completed suicide, the estimate attenuates, and the significance disappears when adjusting for comorbid psychiatric disorders.54 Conversely, the results of this study demonstrate that the three clinical manifestations of hyperandrogenism could be a risk factor for completed suicide. Due to the limitations of the NHIRD, suicide in this study only included completed suicide. Hull maintained that acne may have considerable psychological influence, including anxiety, depression, and suicide.55
Concerning the laboratory testing for hirsutism, screening for serum testosterone and 17-hydroxyprogesterone levels is sufficient in most cases.56 In 2003, new guidelines for the diagnosis of PCOS were suggested by the European Society for Human Reproduction and Embryology and the American Society of Reproductive Medicine to replace the guidelines for the diagnosis of PCOS launched by the National Institutes of Health.57 PCOS should be diagnosed when at least two of the following three characteristics are present: oligoovulation or anovulation, clinical or biochemical signs of hyperandrogenism, and polycystic ovaries.4 Furthermore, new guidelines concerning the diagnosis of PCOS were launched at the 2018 European Society for Human Reproduction and Embryology meeting in Barcelona.58 However, this cohort study were conducted between 2000 and 2015; hence, the latest principle is not applicable. Acne can be diagnosed by a simple visual inspection.59 Nevertheless, a dermatologist may recommend a blood test to determine if the progesterone and androgen levels are low.59
Hyperandrogenism is a defining feature of PCOS.60 As such, patients with PCOS have a higher risk of psychiatric disorders and vice versa.61 PCOS is a common heterogeneous endocrine disorder characterized by irregular menses, hyperandrogenism, and polycystic ovaries.2 Moreover, the negative influence on body image may contribute to subsequent psychiatric disorders.62,63 Research in the United States maintains that women with PCOS are more likely to have low body image stress scores and the lower BIS scores, which may be associated with anxiety and depression.62 A cross-sectional study suggests that PCOS is correlated with lower satisfaction with body images, which may lead to sexual dysfunction, anxiety, and depression.63
Hirsutism, PCOS, and acne were not separated. Thus, clarifying the mechanisms underlying the interaction between these diseases and hyperandrogenism is necessary.
First, one of the primary strengths of this study is the set of ICD-9 codes, and several studies have demonstrated the accuracy and validity of several diagnoses in the NHIRD, including cancer and central nervous system diseases, such as stroke or comorbidity.64,65 Some studies have also demonstrated concordance between Taiwan’s National Health Survey and the NHIRD for various diagnoses.64,66 Second, the relatively long-term observation period allowed for more credibility compared with similar studies to propose mechanisms and plausible hypotheses. Third, we attempted to explain the lack of statistical significance when people experience hirsutism. Fourth, and most importantly, we attempted to explain the mutual biological and psychological mechanisms between the three clinical manifestations of hyperandrogenism and psychiatric disorders. Finally, for the first time, we found that clinical manifestations of hyperandrogenism are associated with an increased risk of psychiatric disorders using a nationwide population-based cohort study design, which to the best of our knowledge, has not been established in previous studies.
The present study had several limitations that warrant consideration. First, we did not use the test results for the exact amount of androgens as the basis for the discussion. Therefore, the results may have been inaccurate. Only three diseases have been used to explain this phenomenon. Second, other genetic, psychosocial, and environmental factors were not considered. Third, the lack of data on the severity of psychiatric disorders limits the generalizability of the results. Fourth, the NHI program started in 1995; however, in this study, the NHIRD that we used contained a database of only 16 years. We strongly recommend a more comprehensive follow-up study in the future. Fifth, some individuals with characteristics of hyperandrogenism during development may not express any of these traits. These patients were not included in our study. Finally, the results of this study were limited to Taiwan and may not necessarily represent other countries or regions. Hence, further studies are needed to investigate the association between the three clinical manifestations of hyperandrogenism and the risk of psychiatric disorders.
Conclusions
The results showed an association between the clinical characteristics of hyperandrogenism and psychiatric disorders. Additionally, this study demonstrated that women aged 20–29 years were more likely to develop subsequent psychiatric disorders. Nevertheless, this study is limited by the lack of exact data on serum androgen levels, as the three clinical symptoms are inferred from hyperandrogenism. Further studies are needed to elucidate the underlying pathophysiological mechanisms of the relationship between hyperandrogenism and psychiatric disorders in women. These findings should be timely reminders for clinicians to pay attention to women who might suffer from psychiatric disorders.
Data Sharing Statement
Data are available from the National Health Insurance Research Database (NHIRD) published by the Taiwan National Health Insurance (NHI) Administration. Due to legal restrictions imposed by the government of Taiwan concerning the “Personal Information Protection Act”, data cannot be made publicly available. Data requests can be sent as formal proposals to the NHIRD (http://www.mohw.gov.tw).
Ethics Approval
The study was conducted per the Declaration of Helsinki guidelines and approved by the Institutional Review Board of the Tri-Service General Hospital at the National Defense Medical Center in Taipei, Taiwan (TSGH IRB No.B-111-15).
Acknowledgments
The National Health Insurance Research Database was provided by the Health and Welfare Data Science Center, Ministry of Health and Welfare (HWDC,MOHW), Taiwan (NHIRD).
Funding
The study was supported by the Medical Affairs Bureau, the Ministry of Defense of Taiwan (MND-MAB-D–111134), the Tri-Service General Hospital Research Foundation (TSGH-B-111018; TSGH-A-111012), and research grants from the Chi Mei Medical Center (CMNDMC10208; CMNDMC10304), which has no role in the study design, data collection and analysis, preparation of the manuscript, and decision to publish.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Heidelbaugh JJ. Endocrinology update: Hirsutism. FP Essent. 2016;451:17–24.
2. Sirmans SM, Pate KA. Epidemiology, diagnosis, and management of polycystic ovary syndrome. Clin Epidemiol. 2013;6:1–13. doi:10.2147/clep.S37559
3. Rodriguez-Paris D, Remlinger-Molenda A, Kurzawa R, et al. Psychiatric disorders in women with polycystic ovary syndrome [Występowanie zaburzeń psychicznych u kobiet z zespołem policystycznych jajników]. Psychiatr Pol. 2019;53(4):955–966. doi:10.12740/PP/OnlineFirst/93105
4. Azziz R. Controversy in clinical endocrinology: diagnosis of polycystic ovarian syndrome: the Rotterdam criteria are premature. J Clin Endocrinol Metab. 2006;91(3):781–785. doi:10.1210/jc.2005-2153
5. Brutocao C, Zaiem F, Alsawas M, Morrow AS, Murad MH, Javed A. Psychiatric disorders in women with polycystic ovary syndrome: a systematic review and meta-analysis. Endocrine. 2018;62(2):318–325. doi:10.1007/s12020-018-1692-3
6. Vallerand IA, Lewinson RT, Parsons LM, et al. Risk of depression among patients with acne in the U.K.: a population-based cohort study. Br J Dermatol. 2018;178(3):e194–e195. doi:10.1111/bjd.16099
7. Morgan J, Scholtz S, Lacey H, Conway G. The prevalence of eating disorders in women with facial hirsutism: an epidemiological cohort study. Int J Eat Disord. 2008;41(5):427–431. doi:10.1002/eat.20527
8. Toffol E, Koponen P, Luoto R, Partonen T. Pubertal timing, menstrual irregularity, and mental health: results of a population-based study. Arch Womens Ment Health. 2014;17(2):127–135. doi:10.1007/s00737-013-0399-y
9. Chien WC, Chung CH, Lin FH, et al. The risk of injury in adults with attention-deficit hyperactivity disorder: a nationwide, matched-cohort, population-based study in Taiwan. Res Dev Disabil. 2017;65:57–73. doi:10.1016/j.ridd.2017.04.011
10. Azziz R, Sanchez LA, Knochenhauer ES, et al. Androgen excess in women: experience with over 1000 consecutive patients. J Clin Endocrinol Metab. 2004;89(2):453–462. doi:10.1210/jc.2003-031122
11. Lin LY, Warren-Gash C, Smeeth L, Chen PC. Data resource profile: the National Health Insurance Research Database (NHIRD). Epidemiol Health. 2018;40:e2018062. doi:10.4178/epih.e2018062
12. Tzeng NS, Chang HA, Chung CH, et al. Risk of psychiatric disorders in Guillain-Barre syndrome: a nationwide, population-based, cohort study. J Neurol Sci. 2017;381:88–94. doi:10.1016/j.jns.2017.08.022
13. Hsieh CY, Su CC, Shao SC, et al. Taiwan’s National Health Insurance research database: past and future. Clin Epidemiol. 2019;11:349–358. doi:10.2147/clep.S196293
14. Ho Chan WS. Taiwan’s healthcare report 2010. Epma j. 2010;1(4):563–585. doi:10.1007/s13167-010-0056-8
15. Yang YJ, Chien WC, Chung CH, et al. Risk of erectile dysfunction after traumatic brain injury: a nationwide population-based Cohort study in Taiwan. Am J Mens Health. 2018;12(4):913–925. doi:10.1177/1557988317750970
16. Hsu DY, Chien WC, Chung CH, et al. Risk of anxiety and depression in patients with lichen planus: a nationwide population-based study. J Affect Disord. 2022;300:255–262. doi:10.1016/j.jad.2021.12.127
17. Tzeng NS, Chung CH, Chang SY, et al. Risk of psychiatric disorders in pulmonary embolism: a nationwide cohort study. J Investig Med. 2019;67(6):977–986. doi:10.1136/jim-2018-000910
18. Kung LY, Li TI, Chung CH, et al. Risk of depression in patients with oral cancer: a nationwide cohort study in Taiwan. Sci Rep. 2021;11(1):23524. doi:10.1038/s41598-021-02996-4
19. Hung CT, Chiang CP, Chung CH, Tsao CH, Chien WC, Wang WM. Risk of psychiatric disorders in rosacea: a nationwide, population-based, cohort study in Taiwan. J Dermatol. 2019;46(2):110–116. doi:10.1111/1346-8138.14705
20. Chang CY, Chen WL, Liou YF, et al. Increased risk of major depression in the three years following a femoral neck fracture–a national population-based follow-up study. PLoS One. 2014;9(3):e89867. doi:10.1371/journal.pone.0089867
21. Tzeng NS, Chung CH, Lin FH, et al. Anti-herpetic medications and reduced risk of dementia in patients with herpes simplex virus infections-a nationwide, population-based Cohort Study in Taiwan. Neurotherapeutics. 2018;15(2):417–429. doi:10.1007/s13311-018-0611-x
22. Gilbert EW, Tay CT, Hiam DS, Teede HJ, Moran LJ. Comorbidities and complications of polycystic ovary syndrome: an overview of systematic reviews. Clin Endocrinol (Oxf). 2018;89(6):683–699. doi:10.1111/cen.13828
23. Yeh TC, Chien WC, Chung CH, et al. Psychiatric disorders after traumatic brain injury: a nationwide population-based Cohort Study and the Effects of Rehabilitation Therapies. Arch Phys Med Rehabil. 2020;101(5):822–831. doi:10.1016/j.apmr.2019.12.005
24. Wang SC, Chien WC, Chung CH, Tzeng NS, Liu YP. Posttraumatic stress disorder and the risk of erectile dysfunction: a nationwide cohort study in Taiwan: PTSD and erectile dysfunction. Ann Gen Psychiatry. 2021;20(1):48. doi:10.1186/s12991-021-00368-w
25. Yao WC, Chen HJ, Leong KH, et al. The risk of fibromyalgia in patients with iron deficiency anemia: a nationwide population-based cohort study. Sci Rep. 2021;11(1):10496. doi:10.1038/s41598-021-89842-9
26. Tsai SY, Chen HJ, Chen C, et al. Increased risk of chronic fatigue syndrome following psoriasis: a nationwide population-based cohort study. J Transl Med. 2019;17(1):154. doi:10.1186/s12967-019-1888-1
27. Hung HH, Lai JN, Chen WC, Chen YH, Chiu LT, Chen HY. Evaluation of the efficacy of traditional Chinese medicine for the reproductive and pregnancy outcomes in women with endometriosis: a nationwide population-based study. Taiwan J Obstet Gynecol. 2021;60(4):685–689. doi:10.1016/j.tjog.2021.05.017
28. O’Driscoll JB, Mamtora H, Higginson J, Pollock A, Kane J, Anderson DC. A prospective study of the prevalence of clear-cut endocrine disorders and polycystic ovaries in 350 patients presenting with hirsutism or androgenic alopecia. Clin Endocrinol (Oxf). 1994;41(2):231–236. doi:10.1111/j.1365-2265.1994.tb02535.x
29. Nock MK, Borges G, Bromet EJ, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008;192(2):98–105. doi:10.1192/bjp.bp.107.040113
30. Thiblin I, Runeson B, Rajs J. Anabolic androgenic steroids and suicide. Ann Clin Psychiatry. 1999;11(4):223–231. doi:10.1023/a:
31. Lenz B, Röther M, Bouna-Pyrrou P, Mühle C, Tektas OY, Kornhuber J. The androgen model of suicide completion. Prog Neurobiol. 2019;172:84–103. doi:10.1016/j.pneurobio.2018.06.003
32. Scarth M, Bjørnebekk A. Androgen abuse and the brain. Curr Opin Endocrinol Diabetes Obes. 2021;28(6):604–614. doi:10.1097/med.0000000000000675
33. Zelleroth S, Nylander E, Örtenblad A, et al. Structurally different anabolic androgenic steroids reduce neurite outgrowth and neuronal viability in primary rat cortical cell cultures. J Steroid Biochem Mol Biol. 2021;210:105863. doi:10.1016/j.jsbmb.2021.105863
34. Kaufman MJ, Kanayama G, Hudson JI, Pope HG
35. Bjørnebekk A, Kaufmann T, Hauger LE, Klonteig S, Hullstein IR, Westlye LT. Long-term Anabolic-Androgenic steroid use is associated with deviant brain aging. Biol Psychiatry Cogn Neurosci Neuroimaging. 2021;6(5):579–589. doi:10.1016/j.bpsc.2021.01.001
36. Sadaie MR, Farhoudi M, Zamanlu M, et al. What does the research say about androgen use and cerebrovascular events? Ther Adv Drug Saf. 2018;9(8):439–455. doi:10.1177/2042098618773318
37. Halaris A. Inflammation-Associated Co-morbidity Between Depression and Cardiovascular Disease. Curr Top Behav Neurosci. 2017;31:45–70. doi:10.1007/7854_2016_28
38. James WH. Further evidence that some male-based neurodevelopmental disorders are associated with high intrauterine testosterone concentrations. Dev Med Child Neurol. 2008;50(1):15–18. doi:10.1111/j.1469-8749.2007.02001.x
39. Ekbäck MP, Lindberg M, Benzein E, Årestedt K. Health-related quality of life, depression and anxiety correlate with the degree of hirsutism. Dermatology. 2013;227(3):278–284. doi:10.1159/000355356
40. Azziz R, Carmina E, Sawaya ME. Idiopathic hirsutism. Endocr Rev. 2000;21(4):347–362. doi:10.1210/edrv.21.4.0401
41. Yilmaz B, Yildiz BO. Endocrinology of Hirsutism: from androgens to androgen excess disorders. Front Horm Res. 2019;53:108–119. doi:10.1159/000494907
42. Carmina E, Koyama T, Chang L, Stanczyk FZ, Lobo RA. Does ethnicity influence the prevalence of adrenal hyperandrogenism and insulin resistance in polycystic ovary syndrome? Am J Obstet Gynecol. 1992;167(6):1807–1812. doi:10.1016/0002-9378(92
43. Huang Z, Yong EL. Ethnic differences: is there an Asian phenotype for polycystic ovarian syndrome? Best Pract Res Clin Obstet Gynaecol. 2016;37:46–55. doi:10.1016/j.bpobgyn.2016.04.001
44. Goodman NF, Cobin RH, Futterweit W, Glueck JS, Legro RS, Carmina E. American Association of Clinical Endocrinologists, American College of Endocrinology, and Androgen Excess and Pcos Society Disease State Clinical Review: guide to the best practices in the evaluation and treatment of polycystic ovary syndrome–Part 1. Endocr Pract. 2015;21(11):1291–1300. doi:10.4158/ep15748.Dsc
45. Reis SL, Abdo CH. Benefits and risks of testosterone treatment for hypoactive sexual desire disorder in women: a critical review of studies published in the decades preceding and succeeding the advent of phosphodiesterase type 5 inhibitors. Clinics. 2014;69(4):294–303. doi:10.6061/clinics/2014(04)11
46. Skoog I. Psychiatric disorders in the elderly. Can J Psychiatry. 2011;56(7):387–397. doi:10.1177/070674371105600702
47. Ito M, Hatazawa J, Yamaura H, Matsuzawa T. Age-related brain atrophy and mental deterioration–a study with computed tomography. Br J Radiol. 1981;54(641):384–390. doi:10.1259/0007-1285-54-641-384
48. Levey L, Ragan K, Hower-Hartley A, Newport DJ, Stowe ZN. Psychiatric disorders in pregnancy. Neurol Clin. 2004;22(4):863–893. doi:10.1016/j.ncl.2004.07.003
49. Petersen KB. Individual fertility assessment and counselling in women of reproductive age. Dan Med J. 2016;63(10):1–26.
50. Shulman LH, DeRogatis L, Spielvogel R, Miller JL, Rose LI. Serum androgens and depression in women with facial hirsutism. J Am Acad Dermatol. 1992;27(2 Pt 1):178–181. doi:10.1016/0190-9622(92)70166-d
51. Derogatis LR, Rose LI, Shulman LH, Lazarus LA. Serum androgens and psychopathology in hirsute women. J Psychosom Obstet Gynaecol. 1993;14(4):269–282. doi:10.3109/01674829309084450
52. Jang D, Elfenbein HA. Menstrual cycle effects on mental health outcomes: a meta-analysis. Arch Suicide Res. 2019;23(2):312–332. doi:10.1080/13811118.2018.1430638
53. Yin X, Ji Y, Chan CLW, Chan CHY. The mental health of women with polycystic ovary syndrome: a systematic review and meta-analysis. Arch Womens Ment Health. 2021;24(1):11–27. doi:10.1007/s00737-020-01043-x
54. Cesta CE, Månsson M, Palm C, Lichtenstein P, Iliadou AN, Landén M. Polycystic ovary syndrome and psychiatric disorders: Co-morbidity and heritability in a nationwide Swedish cohort. Psychoneuroendocrinology. 2016;73:196–203. doi:10.1016/j.psyneuen.2016.08.005
55. Hull PR, D’Arcy C. Acne, depression, and suicide. Dermatol Clin. 2005;23(4):665–674. doi:10.1016/j.det.2005.05.008
56. Mimoto MS, Oyler JL, Davis AM. Evaluation and Treatment of Hirsutism in Premenopausal Women. JAMA. 2018;319(15):1613–1614. doi:10.1001/jama.2018.2611
57. Carmina E. Diagnosis of polycystic ovary syndrome: from NIH criteria to ESHRE-ASRM guidelines. Minerva Ginecol. 2004;56(1):1–6.
58. Hoeger KM, Dokras A, Piltonen T. Update on PCOS: consequences, challenges, and guiding treatment. J Clin Endocrinol Metab. 2021;106(3):e1071–e1083. doi:10.1210/clinem/dgaa839
59. Titus S, Hodge J. Diagnosis and treatment of acne. Am Fam Physician. 2012;86(8):734–740.
60. Rodriguez Paris V, Bertoldo MJ. The mechanism of androgen actions in PCOS etiology. Med Sci. 2019;7(9). doi:10.3390/medsci7090089
61. Greenwood EA, Pasch LA, Cedars MI, Legro RS, Eisenberg E, Huddleston HG. Insulin resistance is associated with depression risk in polycystic ovary syndrome. Fertil Steril. 2018;110(1):27–34. doi:10.1016/j.fertnstert.2018.03.009
62. Alur-Gupta S, Chemerinski A, Liu C, et al. Body-image distress is increased in women with polycystic ovary syndrome and mediates depression and anxiety. Fertil Steril. 2019;112(5):930–938.e1. doi:10.1016/j.fertnstert.2019.06.018
63. Kogure GS, Ribeiro VB, Lopes IP, et al. Body image and its relationships with sexual functioning, anxiety, and depression in women with polycystic ovary syndrome. J Affect Disord. 2019;253:385–393. doi:10.1016/j.jad.2019.05.006
64. Cheng CL, Chien HC, Lee CH, Lin SJ, Yang YH. Validity of in-hospital mortality data among patients with acute myocardial infarction or stroke in National Health Insurance Research Database in Taiwan. Int J Cardiol. 2015;201:96–101. doi:10.1016/j.ijcard.2015.07.075
65. Yang CC, Chen PC, Hsu CW, Chang SL, Lee CC. Validity of the age-adjusted Charlson comorbidity index on clinical outcomes for patients with nasopharyngeal cancer post radiation treatment: a 5-year nationwide cohort study. PLoS One. 2015;10(1):e0117323. doi:10.1371/journal.pone.0117323
66. Tzeng NS, Chang HA, Chung CH, et al. Increased risk of psychiatric disorders in Allergic Diseases: a nationwide, population-based, Cohort Study. Front Psychiatry. 2018;9:133. doi:10.3389/fpsyt.2018.00133
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
