Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 12
Clinical characteristics of chronic bronchitic, emphysematous and ACOS phenotypes in COPD patients with frequent exacerbations
Authors Cheng YS, Tu XW, Pan LL, Lu S, Xing M, Li LL, Chen XW
Received 22 April 2017
Accepted for publication 19 June 2017
Published 18 July 2017 Volume 2017:12 Pages 2069—2074
DOI https://doi.org/10.2147/COPD.S140231
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Yusheng Cheng,* Xiongwen Tu,* Linlin Pan, Shuai Lu, Ming Xing, Linlin Li, Xingwu Chen
Department of Respiratory Medicine, Yijishan Hospital of Wannan Medical College, Wuhu, People’s Republic of China
*These authors contributed equally to this work
Purpose: Chronic bronchitis (CB), emphysematous (EM) and asthma–chronic obstructive pulmonary disease (COPD) overlap syndrome (ACOS) phenotypes in COPD are well recognized. This study aimed to investigate distinguishing characteristics of these phenotypes in COPD patients with frequent exacerbations (FE).
Patients and methods: A retrospective study was carried out. COPD patients with acute exacerbations were consecutively reviewed from November 2015 to October 2016. Patients were divided into FE and infrequent exacerbations (iFE) subgroups.
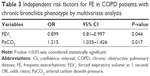
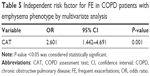
Results: A total of 142 eligible COPD subjects were reviewed. In the CB phenotype subgroup, age, body mass index, forced expiratory volume in 1 second (FEV1) % predicted, COPD assessment test (CAT), modified Medical Research Council breathlessness measurement (mMRC) dyspnea scale, emphysema scores and arterial carbon dioxide pressure (PaCO2) were significantly different in subjects with FE when compared to those in subjects with iFE of CB. In the EM phenotype subgroup, age, CAT, mMRC scores and history of COPD were different in subjects with FE when compared to those in CB subjects with iFE. Multivariate analysis indicated that FEV1% predicted (odds ratio [OR] =0.90, P=0.04) and PaCO2 (OR =1.22, P=0.02) were independent risk factors for FE in COPD with CB phenotype, and CAT (OR =2.601, P=0.001) was the independent risk factor for FE in COPD with EM phenotype. No significant differences in characteristics were observed in ACOS phenotype subgroups with FE or iFE.
Conclusion: In CB or EM phenotypes, COPD patients with FE present several differential clinical characteristics compared to patients with iFE, while the characteristics of ACOS phenotype in patients with FE need more investigation.
Keywords: chronic bronchitis, emphysema, ACOS, COPD, frequent exacerbations
Introduction
Chronic obstructive pulmonary disease (COPD) is a common and heterogeneous respiratory disease involving different pathophysiological changes and is a major cause of morbidity and mortality worldwide.1 Incompletely reversible airflow obstruction, the hallmark of COPD, presents as diverse clinical manifestations. Clinical phenotypes of COPD are differentiated by severity of systemic inflammation, quality of life, the degree of airway obstruction and the response of available medications.2 Chronic bronchitis (CB), emphysematous (EM) and asthma–COPD overlap syndrome (ACOS) are the three generally accepted clinical phenotypes.3–6 In an observational and multicenter study, it was reported that CB accounted for 44.7% of COPD patients, EM was 43.2% and ACOS was only 12.1%.6 COPD patients with CB showed greater chronic dyspnea and activity restriction than patients without CB.7 Compared to CB or ACOS phenotype, COPD patients with EM phenotype present with poorer pulmonary function and greater dyspnea.6 Notably, COPD patients with ACOS phenotype suffer more from obesity and atopic diseases, compared to COPD patients without ACOS phenotype.8 However, a subgroup of COPD patients experience frequent exacerbations (FE), which was clearly described in the ECLIPSE (Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints) study and was associated with accelerated deterioration of lung function, high economic burden and increased mortality.9,10
Around 16% of FE patients are of the EM phenotype.11 COPD patients with FE in the CB phenotype are the only patient group that benefits from treatment with phosphodiesterase-4 inhibitors.12 The ACOS phenotype is reported to be a predictor for FE in patients with COPD.13 Only limited prior work has been undertaken to evaluate these typical phenotypes in COPD patients with FE. The purpose of this study was to investigate differential characteristics of these phenotypes in COPD patients with FE, compared to those patients with infrequent exacerbations (iFE).
Patients and methods
Study subjects
This was a retrospective study which was approved by the Institutional Ethics Committee of Wan Nan Medical College. Due to the retrospective nature of the study all patient data were strictly confidential and the committee waived the need for written informed consent from the subjects. COPD subjects with acute exacerbations, admitted to the Department of Respiratory Medicine, Yijishan Hospital of Wannan Medical College, were reviewed from November 2015 to October 2016. Patients with CB, EM or ACOS phenotype were included. Patients with comorbidities of pulmonary tuberculosis, pulmonary fibrosis, bronchiectasis, lung cancer, pulmonary embolism or other organ failures were excluded. The definition of acute exacerbations of COPD followed the guideline of Global Initiative for Chronic Obstructive Lung Disease (GOLD). FE was defined by the presence of at least two exacerbations (an increase in, or new onset of, ≥2 respiratory symptoms, such as cough, sputum, dyspnea, wheezing and chest tightness, with ≥1 symptom lasting for ≥3 days and requiring treatment with antibiotics and/or systemic steroids or hospitalization) in the previous year and separated by at least 4 weeks (or 6 weeks from the previous exacerbation that did not receive treatment). Others were categorized into the iFE group.14 The definition of CB was chronic phlegm alone for most days, 3 months a year, for 2 years. EM was defined as no chronic cough and sputum, but having typical clinical and radiologic manifestations of EM. The ACOS definition was based on dyspnea at rest and wheezing episodes, with post-bronchodilator forced expiratory volume in 1 second (FEV1)/forced vital capacity (FVC) <0.7 and bronchodilator responsiveness (increase in FEV1 ≥12% and ≥200 mL increase over baseline value).15
Clinical parameters
All clinical parameters were collected and appraised during 24 hours after patients’ admission. Demographic and clinical data including age, gender, body mass index (BMI), smoking index and medical history were collected from medical databases in our hospital. Pulmonary function tests and results of routine hematological examination (white blood cell counts, neutrophils, neutrophil-to-lymphocyte ratio [NLR], C-reactive protein and arterial blood gas) were also collected. The COPD assessment test (CAT) and the modified Medical Research Council breathlessness measurement (mMRC) dyspnea scale were assessed as previously described. Thoracic high-resolution computed tomography (HRCT) was performed with a Philips Brilliance 16-slice spiral CT scanner. Sequential scanning was performed continuously from the apex to the diaphragm at maximal inspiration with a slice thickness of 1 mm and a layer distance of 10 mm. HRCT images were visualized on coronal and sagittal planes to assess the heterogeneity of emphysema by two independent pulmonologists blinded to the patients’ clinical information. The distribution of emphysema was qualitatively assessed by a modified 5-point visual scoring system as follows: a score of 1 indicated obvious predominance of emphysema in upper lung; 2, somewhat predominance of emphysema in upper lung; 3, equal extent of emphysema in upper and lower lung; 4, somewhat predominance of emphysema in lower lung and 5, obvious predominance of emphysema in lower lung.16 A simplified CT scoring system was used to assess bronchial wall thickening for each patient: 0= absent; 1= mild (air wall thickness equal to adjacent vessel); 2= moderate (air wall thickening > adjacent vessel, but ≤2× the diameter of adjacent vessel), and 3= severe (airway wall thickening >2× diameter of adjacent vessel).17
Statistical analysis
Data were expressed as mean ± standard deviation or number (n). Categorical variables were compared between groups using chi-square testing. Continuous variables were evaluated by Student’s t-test. Multivariate analysis was used to assess risk factors for FE in different phenotypes. Odds ratios (OR) and 95% CIs were presented. A P-value <0.05 was considered statistically significant. Statistical analyses were done using SPSS 17.0.
Results
Baseline characteristics of COPD patients with FE or iFE
A total of 142 eligible COPD subjects were reviewed: 60 subjects were categorized as FE and 82 with iFE. As shown in Table 1 – which summarizes clinical data without subphenotyping – subjects with FE were on average substantially older than those with iFE (P=0.001). Subjects with FE had longer history of COPD than subjects with iFE (P=0.001). Smoking index, pulmonary function testing, CAT score, mMRC, bronchial thickening score and PaCO2 in subjects with FE shared significant differences with those in subjects with iFE. However, the proportion of CB, emphysema and ACOS phenotypes, and other characteristics in subjects with FE did not differ from those in subjects with iFE (Table 1).
Characteristics of the CB phenotype in COPD patients with FE
As indicated in Table 2, CB phenotype COPD subjects with FE were significantly older than subjects with iFE (P=0.003). BMI, FEV1% predicted, FEV1/FVC (%), CAT, mMRC, emphysema scores and PaCO2 in CB phenotype subjects with FE shared significant differences with those in subjects with iFE. By multivariate analysis, we found that FEV1% predicted (OR =0.899, P=0.044) and PaCO2 (OR =1.215, P=0.017) were two independent risk factors for CB phenotype subjects with FE (Table 3).
Characteristics of the emphysema phenotype in COPD patients with FE
As shown in Table 4, the age of EM phenotype subjects with FE was greater than subjects with iFE (P=0.012). A longer history of COPD was observed in EM phenotype subjects with FE than in subjects with iFE. Similar to CB phenotype subjects, lower FEV1/FVC (%) and higher CAT and mMRC scores were found in EM phenotype subjects with FE. However, there was no statistical difference in other variables, including BMI, FEV1% predicted and arterial blood PaCO2. Using multivariate analysis, CAT (OR =2.601, P=0.001) proved to be an independent risk factor for FE in COPD patients with the EM phenotype (Table 5).
Characteristics of the ACOS phenotype in COPD patients with FE
As shown in Table 6, arterial pH value was somewhat lower in the ACOS phenotype of COPD with FE than in the iFE subgroup (7.40±0.03 vs 7.42±0.03; P=0.032). However, there were no statistically significant differences in other characteristics between ACOS phenotype COPD subjects with FE and subjects with iFE.
Discussion
In line with previous reports,4,18–22 we revealed that COPD patients with FE showed significantly older age, longer history of disease, greater smoking index, worse lung function (FEV1% predicted, FEV1/FVC%), higher CAT, mMRC and bronchial thickening score, PaCO2 and more comorbidities (coronary heart disease and diabetes) than COPD patients with iFE. Higher bronchial thickening score is also associated with COPD patients with FE.20,23
Previous studies suggested that NLR (examining together the influences of neutrophilia and lymphopenia) reflected systemic inflammatory status in COPD, which was one of the independent predictors of future exacerbations.24,25 However, we found that NLR did not associate with FE in COPD in our study.
Compared to CB phenotype COPD subjects with iFE, clinical characteristics of subjects with FE were older age, lower BMI, more severe airway obstruction (lower FEV1% predicted, FEV1/FVC), increases of CAT and mMRC score, elevated PaCO2 in arterial blood and higher emphysema scores, compared to subjects with iFE. Low BMI is recognized as a marker for predicting future exacerbations among patients with COPD.26,27 Mucus hypersecretion in CB subjects causes distal airway collapse and air trapping, leading to increased residual volume and hyperinflation-emphysema. The ECLIPSE study has identified emphysema as a strong predictor for physiological decline in patients with COPD.1 We found that FEV1% predicted and PaCO2 were two independent risk factors for CB phenotype COPD presenting with FE. The association between FEV1% predicted and CB phenotype with FE has been well documented.28,29 CB phenotype COPD patients with FE present with increased sputum production and bronchial mucosal edema leading to bronchial obstruction, decreased pulmonary ventilation and, consequently, increased arterial PaCO2.30 Similar to the CB phenotype, FE patients with EM phenotype also were older, had a longer history of COPD, lower FEV1/FVC (%), higher CAT and mMRC scores, compared to iFE subjects. Consistent with previous reports, FEV1% predicted in EM subjects with FE did not differ from iFE subjects, supporting that FEV1% predicted is a poor clinical predictor for FE.31 Indeed, a group of COPD patients with high FEV1% predicted commonly experience FE.32 Clearly, FEV1% predicted does not reflect the complexity of COPD, nor alone adequately assess treatment effect in patients with COPD.33,34 Thus, other factors in COPD patients, such as clinical variables, biological indicators and history of exacerbations, need to be evaluated. The associations between emphysema and FE in patients with COPD were inconsistent in previous publications, though we pointed out that emphysema score shared no difference between FE and iFE.20,23,35 Using multivariate analysis, we identified CAT score was an independent risk factor for FE in EM phenotype COPD. This is consistent with previous studies.36,37 The CAT score – which includes 8 questions with scores ranging from 0 to 40 for evaluating symptoms of patients with COPD – is able to more comprehensively capture the impact of COPD symptoms on the daily life and physical and mental health of patients. Clinical symptoms of COPD may provide important information, which should be comprehensively considered for predicting future COPD exacerbations.38,39
Unlike in CB or EM phenotypes, clinical characteristics in ACOS phenotype subjects with FE were not particularly distinguishable from those with iFE. Other factors relating to the asthma, such as atopy, environmental exposures and airway inflammation, may help to identify contributors to FE in the ACOS phenotype.
Some limitations exist in the present study. First, this was a retrospective study and the sample size was small. Second, other phenotypes or endotypes were not appraised in this study. Finally, the underlying mechanisms resulting in differences between the FE risks among the phenotypes were not clarified.
Conclusion
Our study identified differential clinical characteristics in the CB, EM and ACOS phenotypes of COPD patients with FE, compared with patients with iFE. We demonstrated related risk factors for the existence of FE in patients with CB or EM phenotype. An understanding of FE in ACOS phenotype patients will require more investigation.
Acknowledgments
Support for this work has been awarded to Chen Xingwu by the Anhui Provincial Natural Science Foundation (1608085 MH192) and the Scientific Research Foundation of Yijishan Hospital of Wannan Medical College for the Introduction of Talent (YR201401), and to Cheng Yusheng by the Anhui Provincial Key projects of Natural Science Foundation for Colleges and Universities (KJ2017A264) and Key projects of Wannan Medical College (KY22340150).
Author contributions
All authors contributed toward data analysis, drafting and critically revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Vestbo J, Agusti A, Wouters EF, et al. Should we view chronic obstructive pulmonary disease differently after ECLIPSE? A clinical perspective from the study team. Am J Respir Crit Care Med. 2014;189(9):1022–1030. | ||
Allen-Ramey FC, Gupta S, DiBonaventura MD. Patient characteristics, treatment patterns, and health outcomes among COPD phenotypes. Int J Chron Obstruct Pulmon Dis. 2012;7:779–787. | ||
de Oca MM, Halbert RJ, Lopez MV, et al. The chronic bronchitis phenotype in subjects with and without COPD: the PLATINO study. Eur Respir J. 2012;40:28–36. | ||
Oh YM, Sheen SS, Park JH, et al. Emphysematous phenotype is an independent predictor for frequent exacerbation of COPD. Int J Tuberc Lung Dis. 2014;18(12):1407–1414. | ||
Gelb AF, Christenson SA, Nadel JA. Understanding the pathophysiology of the asthma-chronic obstructive pulmonary disease overlap syndrome. Curr Opin Pulm Med. 2016;22(2):100–105. | ||
Izquierdo-Alonso JL, Rodriguez-Gonzalezmoro JM, de Lucas-Ramos P, et al. Prevalence and characteristics of three clinical phenotypes of chronic obstructive pulmonary disease (COPD). Respir Med. 2013;107(5):724–731. | ||
Elbehairy AF, Raghavan N, Cheng S, et al. Physiologic characterization of the chronic bronchitis phenotype in GOLD grade IB COPD. Chest. 2015;147(5):1235–1245. | ||
Caillaud D, Chanez P, Escamilla R, et al. Asthma-COPD overlap syndrome (ACOS) vs ‘pure’ COPD: a distinct phenotype? Allergy. 2017;72(1):137–145. | ||
Miravitlles M, Calle M, Soler-Cataluna JJ. Clinical phenotypes of COPD: identification, definition and implications for guidelines. Arch Bronconeumol. 2012;48(3):86–98. | ||
Hurst JR, Vestbo J, Anzueto A, et al. Susceptibility to exacerbation in chronic obstructive pulmonary disease. N Engl J Med. 2010;363(12):1128–1138. | ||
Blasi F, Neri L, Centanni S, et al. Clinical characterization and treatment patterns for the frequent exacerbator phenotype in chronic obstructive pulmonary disease with severe or very severe airflow limitation. COPD. 2017;14(1):15–22. | ||
Miravitlles M, Soler-Cataluna JJ, Calle M, et al. Treatment of COPD by clinical phenotypes: putting old evidence into clinical practice. Eur Respir J. 2013;41(6):1252–1256. | ||
Wan ES, DeMeo DL, Hersh CP, et al. Clinical predictors of frequent exacerbations in subjects with severe chronic obstructive pulmonary disease (COPD). Respir Med. 2011;105(4):588–594. | ||
Soler-Cataluna JJ, Rodriguez-Roisin R. Frequent chronic obstructive pulmonary disease exacerbators: how much real, how much fictitious? COPD. 2010;7(4):276–284. | ||
Soler-Cataluna JJ, Cosio B, Izquierdo JL, et al. Consensus document on the overlap phenotype COPD-asthma in COPD. Arch Bronconeumol. 2012;48(9):331–337. | ||
Chae EJ, Seo JB, Song JW, et al. Slope of emphysema index: an objective descriptor of regional heterogeneity of emphysema and an independent determinant of pulmonary function. AJR Am J Roentgenol. 2010;194(3):W248–W255. | ||
da Silva SM, Paschoal IA, De Capitani EM, et al. COPD phenotypes on computed tomography and its correlation with selected lung function variables in severe patients. Int J Chron Obstruct Pulmon Dis. 2016;11:503–513. | ||
McGarvey L, Lee AJ, Roberts J, et al. Characterisation of the frequent exacerbator phenotype in COPD patients in a large UK primary care population. Respir Med. 2015;109(2):228–237. | ||
Aziz ZA, Wells AU, Desai SR, et al. Functional impairment in emphysema: contribution of airway abnormalities and distribution of parenchymal disease. AJR Am J Roentgenol. 2005;185(6):1509–1515. | ||
Han MK, Kazerooni EA, Lynch DA, et al. Chronic obstructive pulmonary disease exacerbations in the COPDGene study: associated radiologic phenotypes. Radiology. 2011;261(1):274–282. | ||
Donaldson GC, Hurst JR, Smith CJ, et al. Increased risk of myocardial infarction and stroke following exacerbation of COPD. Chest. 2010;137(5):1091–1097. | ||
Divo M, Cote C, de Torres JP, et al. Comorbidities and risk of mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;186(2):155–161. | ||
Han MK, Bartholmai B, Liu LX, et al. Clinical significance of radiologic characterizations in COPD. COPD. 2009;6(6):459–467. | ||
Lee H, Um SJ, Kim YS, et al. Association of the neutrophil-to-lymphocyte ratio with lung function and exacerbations in patients with chronic obstructive pulmonary disease. PLoS One. 2016;11(6):e0156511. | ||
Gunay E, Sarinc Ulasli S, Akar O, et al. Neutrophil-to-lymphocyte ratio in chronic obstructive pulmonary disease: a retrospective study. Inflammation. 2014;37(2):374–380. | ||
Motegi T, Jones RC, Ishii T, et al. A comparison of three multidimensional indices of COPD severity as predictors of future exacerbations. Int J Chron Obstruct Pulmon Dis. 2013;8:259–271. | ||
Alexopoulos EC, Malli F, Mitsiki E, et al. Frequency and risk factors of COPD exacerbations and hospitalizations: a nationwide study in Greece (Greek Obstructive Lung Disease Epidemiology and health ecoNomics: GOLDEN study). Int J Chron Obstruct Pulmon Dis. 2015;10:2665–2674. | ||
Sundh J, Johansson G, Larsson K, et al. The phenotype of concurrent chronic bronchitis and frequent exacerbations in patients with severe COPD attending Swedish secondary care units. Int J Chron Obstruct Pulmon Dis. 2015;10:2327–2334. | ||
Donaldson GC, Mullerova H, Locantore N, et al. Factors associated with change in exacerbation frequency in COPD. Respir Res. 2013;14(1):79. | ||
Bates ML, Farrell ET, Eldridge MW. Abnormal ventilatory responses in adults born prematurely. N Engl J Med. 2014;370(6):584–585. | ||
Kirby SE, Dennis SM, Jayasinghe UW, et al. Patient related factors in frequent readmissions: the influence of condition, access to services and patient choice. BMC Health Serv Res. 2010;10(1):216. | ||
Thomsen M, Ingebrigtsen TS, Marott JL, et al. Inflammatory biomarkers and exacerbations in chronic obstructive pulmonary disease. JAMA. 2013;309(22):2353–2361. | ||
Bhavani S, Tsai CL, Perusich S, et al. Clinical and immunological factors in emphysema progression. Five-year prospective longitudinal exacerbation study of chronic obstructive pulmonary disease (LES-COPD). Am J Respir Crit Care Med. 2015;192(10):1171–1178. | ||
Hesselbacher SE, Ross R, Schabath MB, et al. Cross-sectional analysis of the utility of pulmonary function tests in predicting emphysema in ever-smokers. Int J Environ Res Public Health. 2011;8(5):1324–1340. | ||
Tulek B, Kivrak AS, Ozbek S, et al. Phenotyping of chronic obstructive pulmonary disease using the modified Bhalla scoring system for high-resolution computed tomography. Can Respir J. 2013;20(2):91–96. | ||
Feliz-Rodriguez D, Zudaire S, Carpio C, et al. Evolution of the COPD Assessment Test score during chronic obstructive pulmonary disease exacerbations: determinants and prognostic value. Can Respir J. 2013;20(5):e92–e97. | ||
Miravitlles M, Garcia-Sidro P, Fernandez-Nistal A, et al. The chronic obstructive pulmonary disease assessment test improves the predictive value of previous exacerbations for poor outcomes in COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:2571–2579. | ||
Kerkhof M, Freeman D, Jones R, et al. Predicting frequent COPD exacerbations using primary care data. Int J Chron Obstruct Pulmon Dis. 2015;10:2439–2450. | ||
Pasquale MK, Xu Y, Baker CL, et al. COPD exacerbations associated with the modified Medical Research Council scale and COPD assessment test among Humana Medicare members. Int J Chron Obstruct Pulmon Dis. 2016;11(1):111–121. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.