Back to Journals » Infection and Drug Resistance » Volume 16
Clinical Characteristics and Prognosis of Hospital-Acquired Klebsiella pneumoniae Bacteremic Pneumonia versus Escherichia coli Bacteremic Pneumonia: A Retrospective Comparative Study
Authors Li F , Zhu J, Hang Y, Chen Y, Gu S , Peng S , Fang Y, Hu L, Xiong J
Received 3 May 2023
Accepted for publication 26 July 2023
Published 2 August 2023 Volume 2023:16 Pages 4977—4994
DOI https://doi.org/10.2147/IDR.S419699
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Fuxing Li,1,* Junqi Zhu,1,* Yaping Hang,1 Yanhui Chen,1 Shumin Gu,1 Suqin Peng,1 Youling Fang,1 Longhua Hu,1 Jianqiu Xiong2
1Department of Jiangxi Provincial Key Laboratory of Medicine, Clinical Laboratory of the Second Affiliated Hospital of Nanchang University, Nanchang, Jiangxi, People’s Republic of China; 2Department of Nursing, the Second Affiliated Hospital of Nanchang University, Nanchang, Jiangxi, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Longhua Hu, Department of Jiangxi Provincial Key Laboratory of Medicine, Clinical Laboratory of the Second Affiliated Hospital of Nanchang University, Mingde Road No. 1, Nanchang, Jiangxi, 330006, People’s Republic of China, Email [email protected] Jianqiu Xiong, Department of Nursing, The Second Affiliated Hospital of Nanchang University, Mingde Road No. 1, Nanchang, Jiangxi, 330006, People’s Republic of China, Email [email protected]
Objective: This research aimed to investigate the variations in clinical features and prognosis of HABP caused by E. coli and K. pneumoniae. We also aimed to evaluate the risk variables related to 30-day death in the investigated groups.
Methods: A single-center retrospective cohort research lasting four years was performed. A total of 117 patients with HABP were involved in this research. The primary prognosis was 30-day death.
Results: Among 117 patients with HABP, 60 patients were infected with K. pneumoniae (KP-HABP), and 57 patients were infected with E. coli (E. coli-HABP). A higher proportion of males, ICU admission, undergoing tracheotomy and trachea cannulation, carbapenem-resistant strains, inappropriate empirical therapy (IET), immune compromise, diabetes mellitus, and sepsis were observed in the patients with KP-HABP (all P < 0.05). Meanwhile, the median SOFA score and Pitt score were significantly (P < 0.001) higher in the KP-HABP group compared to the E. coli-HABP group. The 30-day death was 48.33% in the KP-HABP group and 24.56% in the E. coli-HABP group (P = 0.008). After adjusting for the main covariates, the hazard ratios for 30-day mortality in KP-HABP were 1.58 (95% CI:0.80– 3.12), 3.24 (95% CI:1.48– 7.06), 5.67 (95% CI:2.00– 16.07), and 5.99 (95% CI:2.10– 17.06), respectively. Multivariate logistic regression models revealed that IET, hypoproteinaemia, cerebral vascular disease (CVD), and SOFA score ≥ 5.0 were the independent risk variables for 30-day death in KP-HABP. Simultaneously, SOFA score ≥ 4.0 and Pitt score ≥ 2.0 were independent risk factors for 30-day mortality in E. coli-HABP.
Conclusion: The clinical features of HABP vary depending on whether it is caused by Escherichia coli or K. pneumoniae. KP-HABP patients have higher 30-day mortality than E. coli-HABP patients. To ensure greater validity, it is necessary to further verify this conclusion using a larger sample size.
Keywords: Escherichia coli, Klebsiella pneumoniae, hospital-acquired pneumonia, bacteremic pneumonia, 30-day mortality
Introduction
The high incidence of hospital-acquired pneumonia (HAP) has a serious impact on the safety and prognosis of patients, which increases the economic burden on society and patients.1,2 Previous studies reported that the prevalence of HAP is estimated to be 0.5% to 1.0% and accounts for approximately 25% of all infectious diseases in the intensive care unit (ICU).3 Furthermore, hospital-acquired bacteremic pneumonia (HABP) poses a significant public health threat because of the high mortality rate, high cost, and high rate of detection of bacterial resistance.3–5
The leading etiological agents in HAP are Gram-negative bacteria. Opportunistic pathogens, which have the ability to colonize either the respiratory or intestinal tracts of humans or animals, have a tendency to infect individuals with compromised immune systems.6 Klebsiella pneumoniae (K. pneumoniae) and Escherichia coli (E. coli), as the two most representative bacteria of the Enterobacteriaceae family, are the two common pathogens of HABP.7 A large epidemiological study analyzed the pathogenic bacteria in HABP patients (31,436 episodes) and found that Gram-negative bacteria were the most common isolates, with Klebsiella pneumoniae (9.8%) and E. coli (6.9%) infections being the third and fourth most common, respectively.8 Notably, recently, due to clinical antibiotic abuse and other reasons, bacterial resistance has become increasingly severe,9 which has led to the evolution of these two bacteria into produced Extended-spectrum beta-lactamase (ESBL) and carbapenem-resistant (CR) strains, which certainly have great difficulty in the clinical therapy of HABP.10–12
In effect, it is critical to identify the causative pathogens as soon as possible for the treatment of HABP. Different bacteria have different pathogenic mechanisms,13 along with complex risk factors, comorbidities, and inappropriate empirical therapy. This contributes to prolonged hospitalizations and higher healthcare expenses, eventually leading to a worse prognosis for patients with HABP.8,14,15 Although numerous studies examined the differences in bloodstream infections induced by E. coli and K. pneumoniae,16–18 a comprehensive comparison of HABP caused by these two pathogens is still lacking.
This research objectives were to analyze the clinical features and outcome of HABP related to E. coli and K. pneumoniae and to assess the risk factors for 30-day death in each group separately, with the aim of providing a reference for clinical diagnosis, treatment, and rational use of antibiotics.
Methods
Study Subjects
This retrospective cohort research was conducted over four years (2016–2019). HAP and ventilator-associated pneumonia (VAP) have been identified based on the clinical practice standards of the Infectious Diseases Society of America and the American Thoracic Society.19 A total of 117 adults patients with HABP caused by E. coli or K. pneumoniae from the Second Affiliated Hospital of Nanchang University were involved herein (Figure 1). According to the different pathogens, patients with HABP were further classified into hospital-acquired Klebsiella pneumoniae (KP) bacteremic pneumonia (KP-HABP) group (n = 60) and hospital-acquired E. coli bacteremic pneumonia (E. coli-HABP) group (n = 57). Subsequently, patients with KP-HABP were split into two groups: death (n = 29) and survival (n = 31) based on their 30-day death. Similarly, patients with E. coli-HABP were divided into the survival group (n = 43) and the deceased group (n = 14). The inclusion criteria were: (1) Patients were aged 18 and above; (2) Patients with a minimum of one positive blood culture for Klebsiella pneumoniae or E. coli within 24 h of the diagnosis of HAP. The exclusion criteria were: (1) Polymicrobial infection; (2) Infections other than pneumonia at the time of admission; (3) Pregnant women and lactating females; (4) Patients with missing clinical data. For patients with multiple E. coli or K. pneumoniae blood culture isolations, only the initial isolation from each patient was incorporated herein.
 |
Figure 1 Flow chart of the inclusion of patients with KP-HABP and E. coli-HABP. |
Study Definitions and Treatment Outcomes
HAP was defined as pneumonia that does not exist at the time of hospitalization and is not in the incubation period of infection but occurs 48 h after hospitalization, including pneumonia acquired in the hospital and occurring within 48 h of discharge (including VAP).19 The current diagnosis of pneumonia is based on imaging showing a new pulmonary infiltrate and clinical evidence confirming that the infiltrate is due to infection, including new fever, pus sputum, leukocytosis, and decreased oxygenation.20 Polymicrobial infection was defined as more than one microorganism detected by blood culture or respiratory secretion specimens within 48 h of admission. At the time of hospitalization, immunocompromised patients are administered chronic glucocorticoids, biologic response modifiers, antimetabolites, or immunosuppressive transplant medicines.21 Inappropriate empirical antimicrobial therapy (IET) was defined as the isolates that were insusceptible (the susceptibility test results are interpreted as “resistant” (R) or “intermediate” (I)) to the prescribed antibiotics. The presence of infection, recurrence, or progression of disease after two weeks of appropriate antibiotic therapy was regarded as a 14-day therapeutic failure. The primary prognosis was 30-day mortality, and the secondary prognosis was 14-day treatment failure.
Data Collection
All patient data was acquired from digital medical data. Microsoft Excel (Excel for MacOS, 2020) was used for data collection of the clinical and laboratory information, including demographics, inpatient department, invasive procedures, underlying disease, microbiology-related data, infection-related indices, and the use of antibiotics, disease severity, and patient outcomes. Comorbidity was assessed using the age-adjusted Charlson comorbidity index (aCCI).22 Meanwhile, to evaluate the disease severity of patients with HABP, the Pitt bacteremia score (Pitt score)23 and the Sequential Organ Failure Assessment (SOFA) score24 were calculated on the day of admission.
Microbiological Analysis
KP and E. coli isolates were identified using mass spectrometry (MALDITOF MS, Vitek MS, BioMérieux, France) or the Vitek 2 automated System (BioMerieux®, Marcy IEtolie, France) according to the manufacturer’s instruction. Susceptibility tests were performed with the ATB System (bioMérieux, France) or Kirby-Bauer (KB) test. The minimal inhibitory concentration (MIC) was detected by the broth microdilution approach.25 The combined disc technique (ceftriaxone only and ceftriaxone-clavulanic acid) was used to detect ESBL production. Carbapenemase production was tested using the modified carbapenem inactivation method (mCIM) and the EDTA-modified carbapenem inactivation method (eCIM). Clinical Laboratory Standards Institutes (CLSI) standards (CLSI, 2016–2019) were used to interpret all susceptibility data.26–29
Statistics
SPSS v22.0 was employed to analyze the data (SPSS Inc.). GraphPad Prism 7.0 (GraphPad Software Inc.) and R software (R project) were employed to plot all figures. For data (in line with normal distribution) that was presented as mean ± standard deviation, a parameter test was used (One-way analysis of variance). The non-parametric Mann–Whitney U-test was performed for data that did not follow a normal distribution and was provided as a median and IQR. Percentages were calculated using the chi-square or Fisher’s exact test on the numerical data. Kaplan-Meier (KM) curve was plotted to assess survival outcomes between KP-HABP and E. coli-HABP. Following this, to assess the hazard ratios (HR) and 95% confidence interval (CI) of the correlation of HABP due to two pathogens with poor outcomes (14-day treatment failure and 30-day mortality), four Cox regression adjusted models were constructed. Model 1 was adjusted for age, sex, inpatient department (surgery ward, ICU), and invasive procedures (tracheotomy, trachea cannula). Model 2 was further adjusted for bacterial type. Model 3 was further adjusted for underlying disease (immune compromise, diabetes mellitus, and sepsis), Pitt score, and SOFA score. Model 4 was further adjusted for IET. Subsequently, the optima cut-off values of SOFA score, Pitt score, and aCCI score were calculated by receiver operating characteristic (ROC) curves and categorized using the optima cut-off values.
Moreover, univariate and multivariate logistic regression analyses were employed to detect independent risk variables for 14-day treatment failure and 30-day death in patients with KP-HABP and E. coli-HABP, respectively. Then, variables with P < 0.10 (with potentially statistically significant) in the multivariate logistic analyses for 30-day mortality were included for nomogram construction. The Hosmer-Lemeshow test was employed to analyze the nomogram’s calibration and determine its accuracy.30 Finally, the nomogram was assessed utilizing the ROC curve, calibration curve, and decision curve analysis (DCA). A P-value smaller than 0.05 (P < 0.05) was considered statistically significant.
Results
The Initial Demographics and Clinical Features of Subjects with KP-HABP and E. Coli-HABP
Table 1 depicts the clinical features of patients with KP-HABP and E. coli-HABP. In total, 117 patients were diagnosed with KP-HABP or E. coli-HABP, with a mean age of 57.88 ± 16.06 years, and 69 (58.97%) males. A total of 60 patients were from the KP-HABP group, and 57 were from the E. coli-HABP group. No statistically significant variation was observed in age, the proportion of patients admitted to internal medicine, invasive procedures (including surgery, venous catheterization, wound drainage tube, indwelling urinary catheter, bone marrow aspiration, lumbar puncture, and thoracentesis), underlying disease (including cerebral vascular disease, hypertension, pleural effusion, hypoproteinaemia, and leukemia), aCCI score, empiric therapy (including third-generation cephalosporins, β-lactam-β-lactamase inhibitor, carbapenems, and aminoglycoside), antibiotics ≥3 during hospitalization and hospitalization duration between the two groups (all P > 0.05). Nevertheless, in comparison to the E. coli-HABP group, patients with KP-HABP included more male patients, were more frequently admitted to the ICU, less frequently admitted to the surgery ward, and were more likely to undergo tracheotomy and trachea cannulation. Moreover, the KP-HABP group exhibited a higher proportion of carbapenem-resistant strains and inappropriate empirical therapy, a higher prevalence of concomitant immune compromise, diabetes mellitus, and sepsis, higher Pitt and SOFA scores, and a higher proportion of 14-day therapeutic failure and 30-day mortality (all P < 0.05). Table 2 presents the antimicrobial susceptibility features of 60 K. pneumoniae, and 57 E. coli isolates. Compared to K. pneumoniae, E. coli was sensitive to more antibiotics, including amikacin, cefoxitin, imipenem, and piperacillin (all P < 0.05).
 |
Table 1 Characteristics of the KP-HABP and E. Coli-HABP Cohorts |
 |
Table 2 Antimicrobial Resistance of Klebsiella Pneumoniae and Escherichia Coli Isolated from Patients with KP-HABP and E. Coli-HABP |
The Hazard Ratio for 30-Day Mortality According to KP-HABP and E. Coli-HABP
The 30-day mortality was 48.33% (29/60) in the KP-HABP group compared to 24.56% (14/57) in the E. coli-HABP group (P = 0.008). Subsequently, Kaplan-Meier survival analysis was performed to assess the relationship between the bacterial type of hospital-acquired pneumonia and survival outcomes (Figure 2). Similar to the results above, patients with KP-HABP presented a significant increase in 30-day mortality (P < 0.001). Then, to evaluate possible determinants of 30-day mortality from KP-HABP and E. coli-HABP, four multivariate Cox regression models were developed (Table 3). After adjusting for age, sex, inpatient department (surgery ward, ICU), and invasive procedures (tracheotomy, trachea cannula), the HR for 30-day mortality comparing KP-HABP to E. coli-HABP was 1.58 (95% CI [0.80–3.12], P = 0.187, model 1). Further analyses adjusted for bacterial type, revealing a statistically significant adjusted HR (HR = 3.24, 95% CI [1.48–7.06], P = 0.003, model 2). Moreover, HR remained statistically significant after adjustment for underlying disease (immune compromise, diabetes mellitus, sepsis), Pitt score and SOFA score (HR = 5.67, 95% CI [2.00–16.07], P = 0.001, model 3), and after further adjustment for inappropriate empirical therapy (HR = 5.99, 95% CI [2.10–17.06], P = 0.001, model 4). However, there was a greater proportion of 14-day treatment failure in the KP-HABP group compared E. coli-HABP group (66.67% vs 33.33%), even though the variation was non-statistically significant after adjusting by models (Table 3).
 |
Table 3 Hazard Ratio for Outcomes According to KP-HABP and E. Coli-HABP |
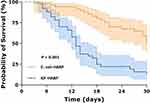 |
Figure 2 Kaplan-Meier curve of 30-day mortality in patients with HABP caused by Klebsiella pneumoniae and Escherichia coli. |
The Risk Variables for 14-Day Treatment Failure and 30-Day Death in Patients with KP-HABP
Patients with KP-HABP were classified into survival (n = 31) or non-survival group (n = 29) based on the prognosis of patients at 30 days. Table 4 shows the different features of the death group and survival group. In comparison to the survival group, the death group showed an increased rate of tracheotomy, was more susceptible to carbapenem-resistant strains infection, and had higher numbers of subjects with cerebral vascular disease and hypoproteinaemia, higher Pitt score, higher SOFA score, and aCCI score. Meanwhile, the death group exhibited a greater proportion of inappropriate empirical therapy, antibiotics ≥3 during hospitalization, and 14-day treatment failure.
 |
Table 4 Characteristics of 30-Day Survivors and Non-Survivors |
Due to Pitt, SOFA, and aCCI scores being non-normal data, the cut-off values of these parameters were calculated with the ROC curve analysis (Table 5). The best cut-off levels of Pitt, SOFA, and aCCI scores were 3.0, 5.0, and 5.0, respectively. After dichotomous transformation, univariable and multivariable logistic regression analyses were carried out to assess the 14-day treatment failure and 30-d mortality-related risk factors in patients with KP-HABP (Figure 3). Subsequently, multivariable logistic regression showed carbapenem-resistant strains, cerebral vascular disease and higher SOFA score (≥ 5.0) were potential predictors of 14-day treatment failure (P < 0.10, with potentially statistically significant) (Figure 3B), and inappropriate empirical therapy (IET), hypoproteinaemia, cerebral vascular disease (CVD) and higher SOFA score (≥ 5.0) were related significantly to 30-day deaths in patients with KP-HABP (P < 0.05) (Figure 3D).
 |
Table 5 ROC Analysis of Illness Severity Scores for Predicting the Prognosis of Patients with KP-HABP and E. Coli-HABP |
Furthermore, the nomogram was constructed by incorporating five predictors, which were linked to 30-day death (Figure 4). The scores corresponding to the nomogram were 87.5 for CVD, 90 for hypoproteinaemia, 100 for SOFA score ≥ 5.0, 72.5 for aCCI score ≥ 5.0, and 97.5 for IET, respectively, with predicted probabilities between 0.05–0.99 for total integrals between 65–430. The AUC of the nomogram was 0.888 (95% CI: 0.800–0.977), with 82.8% sensitivity and 87.1% specificity, which had high accuracy (Figure 5A). The calibration curve was approximately diagonal, and the Hosmer-Lemeshow test P-value for the model’s goodness-of-fit was 0.491, which is not statistically significant (Figure 5B). Finally, the clinical decision curve (DCA) for the 30-day mortality prediction model was presented in Figure 5C, which showed great clinical application value.
The Risk Variables for 14-Day Treatment Failure and 30-Day Mortality in Patients with E. Coli-HABP
The patient cohort diagnosed with E. coli-HABP was divided into two distinct groups based on their survival status at 30 days post-admission: survival (n = 43) and death (n = 14) (Table 4). The percentage of tracheotomy and trachea cannula was higher in the death group than in the survival group. Concerning sepsis severity, patients in the death group showed significantly higher Pitt and SOFA scores. In addition, Patients in the death group were significantly more likely to receive inappropriate empirical therapy and to have treatment failure at the 14-day point. Meanwhile, based on Youden’s index, the best cut-off value of the Pitt score to anticipate 30-day death in patients with E. coli-HABP was determined as 2.0. The optimal cut-off value of the SOFA score was 4.0 (Table 5), and then binary classification was performed. Next, we performed logistic regression analysis (Figure 6). Multivariate logistic regression analysis identified high SOFA score (≥ 4.0) and trachea cannula were associated significantly with 14-day treatment failure (Figure 6B). High SOFA score (≥ 4.0) and high Pitt score (≥ 2.0) were independent risk variables of 30-day mortality in patients with E. coli-HABP (all P < 0.05) (Figure 6D). A nomogram was further constructed based on IET, SOFA score and Pitt score (Figure 7), with predicted probabilities between 0.05–0.80 for total integrals between 48–248. Next, we validated the performance of the nomogram in patients with E. coli-HABP (Figure 8). The AUC of prediction model was 0.888 (95% CI: 0.776–0.956), with 78.6% sensitivity and 88.4% specificity (Figure 8A). The Hosmer-Lemeshow test was used to determine whether or not the regression model was a good fit yielded a significant result (P = 0.536), and the calibration curve demonstrated that the model prediction was consistent with the observed field data (Figure 8B). Moreover, DCA confirmed the clinical practicability of three risk factors to predict 30-d mortality in patients with E. coli-HABP (Figure 8C).
 |
Figure 7 Nomogram for predicting the prognosis of E. coli-HABP patients. |
Discussion
There were significant variations in the initial clinical features of KP-HABP patients and those with E. coli-HABP. Consistent with previous reports,31 male patients were more susceptible to KP-HABP, which may be attributed to the differences between male and female lifestyles. Epidemiological studies also found that men were generally more susceptible to infection with diverse pathogens than women.32,33 However, further investigation is required in light of the restricted sample size. Furthermore, numerous studies confirmed that HAP is the main reason for hospital-acquired infection in the ICU.34,35 Simultaneously, KP is mainly isolated from respiratory specimens. Some studies confirmed that K. pneumoniae was the most frequent reason for HAP,36 which provided plausible explanations for our study’s findings that KP-HABP patients were more frequently admitted to the ICU than E. coli-HABP patients.
Further analysis found that patients with KP-HABP had more comorbidities (immune compromise, diabetes mellitus, and sepsis) than patients with E. coli-HABP, and most patients with KP-HABP were treated with endotracheal intubation and mechanical ventilation, resulting in significantly higher disease severity (Pitt and SOFA scores) in patients with KP-HABP. It is worth noting that the extensive utilization of carbapenems has led to a significant rise in the identification of carbapenem-resistant K. pneumoniae (CRKP), owing to the resulting enhanced selective pressure,37,38 combined with inappropriate empiric therapy, which significantly limits effective clinical treatment and leads to poor outcomes (14-day treatment failure and 30-day mortality). Overall, the synergy of the above factors ultimately led to higher 30-day mortality in KP-HABP patients than in E. coli-HABP patients (48.33% vs 24.56%, P = 0.008). The variances in pathogenesis between K. pneumoniae and E. coli necessitate an investigation into the potential impact of microbial type on clinical outcomes. The present study aimed to conduct a comparative analysis of the clinical outcomes of HABP in relation to microorganisms, specifically K. pneumoniae and E. coli. The findings of this study may contribute novel insights into the field of clinical diagnosis and treatment. Similar problems were described in other clinical comparative studies,17,18,39–42 but comprehensive comparative studies of HABP caused by these two pathogens are still lacking. Although previous reports indicated no difference in short-term mortality between liver abscesses due to E. coli and K. pneumoniae,17,42 a study found that community-onset monomicrobial bacteremia due to E. coli and K. pneumoniae had similar 28-d mortality rates (12.4% vs 14.0%, P = 0.59).39 However, the results of some studies were in line with our findings. In a comparative research of community-onset E. coli and K. pneumoniae bacteremia, patients admitted with K. pneumoniae bacteremia exhibited elevated 30-day deaths compared to patients admitted with E. coli bacteremia (14.44% vs 8.8%, P = 0.008).18 Moreover, acute cholangitis (AC) caused by two pathogens showed a higher 30-day mortality rate for K. pneumoniae infection than E. coli infection (20.7% vs 6.3%, P = 0.017).41 Remarkably, after we found a variation in 30-day death between the two groups, KM analysis yielded similar conclusions (Figure 2) and further supported our results after correction for confounders (Table 3). Indeed, our findings can be explained by the following reasons: (i) KP-HABP group had a higher number of critical illnesses on admission, along with more invasive operations during hospitalization, which resulted in a worse prognosis for KP-HABP patients. (ii) K. pneumoniae caused more severe bacteremia than E. coli in patients having severe underlying health issues, resulting to an elevated probability of death.13,18 (iii) The higher 30-d mortality rate in patients with KP-HABP may be related to virulence factors, biofilm formation, and antimicrobial resistance of K. pneumoniae.41,43 Admittedly, the small sample size limits the reliability and generalizability of results; this remains to be confirmed by a more extensive study.
Alarmingly, the rates of carbapenem resistance in K. pneumoniae are on the rise.44–46 In retrospective research performed in a tertiary care hospital in China, 68.8% of patients diagnosed with HAP were identified with CRKP infection, and 25% died within 28 days.47 Meanwhile, the data on the evolution of drug resistance of K. pneumoniae to imipenem and meropenem in CHINET tertiary hospitals from 2005 to 2019 showed that their resistance rates had elevated quickly from 3.0% and 2.9% in 2005 to 25.3% and 26.8% in 2019, respectively.48 The resistance rates are on the rise, which were essentially similar to our results. Our study found that the detection rate of CRKP strains in KP-HABP patients was 41.67%, while the 30-day mortality rate was 48.33%. Moreover, a study conducted in Taiwan found that among HABP patients, the detection rate of CRKP strains, up to 58.2%, showed a 28-day death rate of 60.2%,31 further supporting our results. Another concern was that using carbapenem antibiotics in the empirical therapy of KP-HABP patients is up to 50%, which undoubtedly increased the detection rate of CRKP strains. Therefore, the rational use of antibiotics to reduce the production of drug-resistant strains is essential to improve the prognosis of patients with KP-HABP. Besides, current studies have identified several risk factors for prognosis in patients with KP infection, including advanced age, high APACHEII score/SOFA score, infectious shock, granulocytopenia or deficiency, mechanical ventilation, central venous catheterization, insensitive anti-infective therapy.49–53 In our study, further multiple logistic regression confirmed that inappropriate empirical therapy (IET), hypoproteinaemia, cerebral vascular disease (CVD), and higher SOFA score (≥ 5.0) were independent risk factors for 30-day mortality in patients with KP-HABP. Based on the potential risk factors, the constructed nomogram demonstrates good prognostic performance (Figures 4 and 5). In a word, these findings suggested that clinicians need to be alert to the risk factors associated with KP-HABP patients and that timely intervention and avoidance of disease progression are critical to improving the prognosis of patients.
Differently from patients with KP-HABP, more ESBL-producing strains were detected in E. coli-HABP patients (18.33% vs 50.88%). Combined with our drug sensitivity experiments (Table 2), most E. coli strains were resistant to quinolones and sulfonamides antibiotics, which may be related to the presence of multi-drug resistance genes, including quinolone and sulfonamide antibiotics on the plasmid, besides the reduced permeability of bacterial outer membrane proteins.54 Notably, E. coli susceptibility to amikacin, imipenem, and piperacillin exceeded 90% in patients with E. coli-HABP. Therefore, for antibiotic selection in patients with E. coli-HABP, carbapenems can be the first choice, while amikacin and piperacillin-tazobactam can be used as alternative or combination regimens when appropriate, and quinolones and β-lactam antibiotics are not recommended, which provided a theoretical reference for clinicians to use antibiotics rationally. In parallel, E. coli-HABP patients exhibited a 30-day mortality of 24.56%. A study found a 14% hospital mortality rate in community-acquired pneumonia (CAP) caused by E. coli,55 which may be due to the fact that more patients with HAP occur in the ICU and the greater chance of infection with drug-resistant bacteria. Furthermore, inappropriate empiric therapy, SOFA score ≥ 4.0, and Pitt score ≥ 2.0 were independent risk factors for 30-day mortality in patients with E. coli-HABP, which had been confirmed in previous studies.55–57 Finally, we tried to construct the nomogram with the potential risk factors and again demonstrated good prognostic performance (Figures 7 and 8).
Limitations
There were some limitations to this study. First, this study was a single-center retrospective study, and the size of included cases was too small, which might impact on accuracy and punctuality of statistical analysis. At the same time, we did not perform sample size estimation, so the results should be interpreted and used with caution. However, due to the small number of related studies, our study still has a certain reference value. We look forward to multi-center collaboration to further confirm our findings. Second, selection bias could not be avoided due to the retrospective study design. For example, HAP patients with undiagnosed bacteremia were not included. Third, in this study, we did not detect and analyze the molecular characteristics of drug-resistant strains so as to know the prevalence of strains causing HABP in our region. Finally, after exploring the risk factors for 30-day mortality in HABP caused by two pathogens separately, we attempted to construct a nomogram, which, although we performed internal validation, was, however, a tentative exercise and was not externally validated, which will be the focus of our subsequent study.
Conclusion
In conclusion, our study showed differences in clinical features between HABP caused by E. coli and K. pneumoniae. The 30-day mortality of HABP caused by Klebsiella pneumoniae was significantly higher than that of E. coli. Among patients with KP-HABP, inappropriate empirical therapy, hypoproteinaemia, cerebral vascular disease (CVD), SOFA score ≥ 5.0, and aCCI score ≥ 5.0 were independent risk factors for 30-day mortality. Meanwhile, inappropriate empiric therapy, SOFA score ≥ 4.0, and Pitt score ≥ 2.0 were closely related to the prognosis of patients with E. coli-HABP. Moreover, the detection rate of carbapenem-resistant and ESBL-producing strains was high in patients with HABP, and the problem of bacterial resistance is still severe. Therefore, antimicrobial drugs should be used rationally in the clinic, and antimicrobial drugs should be selected in combination with resistance characteristics and resistance in the region.
Data Sharing Statement
All data generated or analysed during this study are included in this published article.
Ethics Approval and Consent to Participate
Informed consent was acquired from each participant included in the study. This study conformed to the guidelines of the Helsinki Declaration. Ethics approval was obtained by the Research Ethics Committee of the Second Affiliated Hospital of Nanchang University.
Consent for Publication
Written informed consent for publication was obtained from all participants.
Acknowledgments
The authors would like to thank Home for Researchers for English language editing services.
Author Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the Natural Science Foundation of Jiangxi Province for Young Scholars (No. 20202BAB2160), Science and Technology Research Project of Education Department of Jiangxi Province (No. GJJ180154) and the Medical Health Science and Technology Project of Jiangxi Provincial Health Commission (No. 20201034).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lanks CW, Musani AI, Hsia DW. Community-acquired pneumonia and hospital-acquired pneumonia. Med Clin North Am. 2019;103(3):487–501. doi:10.1016/j.mcna.2018.12.008
2. Myrianthefs P, Ioannidis K, Baltopoulos G, et al. Treatment of hospital-acquired pneumonia. Lancet Infect Dis. 2011;11(10):729–730. doi:10.1016/S1473-3099(11)70263-8
3. Rosenthal VD, Maki DG, Mehta Y, et al. International Nosocomial Infection Control Consortium (INICC) report, data summary of 43 countries for 2007–2012. Device-associated module. Am J Infect Control. 2014;42(9):942–956. doi:10.1016/j.ajic.2014.05.029
4. Magill SS, O’Leary E, Janelle SJ, et al. Changes in prevalence of health care–associated infections in U.S. hospitals. N Engl J Med. 2018;379(18):1732–1744. doi:10.1056/NEJMoa1801550
5. Bart SM, Rubin D, Kim P, et al. Trends in hospital-acquired and ventilator-associated bacterial pneumonia trials. Clin Infect Dis. 2021;73(3):e602–e8. doi:10.1093/cid/ciaa1712
6. Gupta R, Malik A, Rizvi M, et al. Epidemiology of multidrug-resistant Gram-negative pathogens isolated from ventilator-associated pneumonia in ICU patients. J Glob Antimicrob Resist. 2017;9:47–50. doi:10.1016/j.jgar.2016.12.016
7. Wang M, Earley M, Chen L, et al. Clinical outcomes and bacterial characteristics of carbapenem-resistant Klebsiella pneumoniae complex among patients from different global regions (CRACKLE-2): a prospective, multicentre, cohort study. Lancet Infect Dis. 2022;22(3):401–412. doi:10.1016/S1473-3099(21)00399-6
8. Jones RN. Microbial etiologies of hospital-acquired bacterial pneumonia and ventilator-associated bacterial pneumonia. Clin Infect Dis. 2010;51 Suppl 1:S81–7. doi:10.1086/653053
9. Algammal A, Hetta HF, Mabrok M, et al. Editorial: emerging multidrug-resistant bacterial pathogens “superbugs”: a rising public health threat. Front Microbiol. 2023;14:1135614. doi:10.3389/fmicb.2023.1135614
10. Xu A, Zheng B, Xu YC, et al. National epidemiology of carbapenem-resistant and extensively drug-resistant Gram-negative bacteria isolated from blood samples in China in 2013. Clin Microbiol Infect. 2016;22(1):S1–8. doi:10.1016/j.cmi.2015.09.015
11. Martin-Loeches I, Rodriguez AH, Torres A. New guidelines for hospital-acquired pneumonia/ventilator-associated pneumonia: USA vs. Europe. Curr Opin Crit Care. 2018;24(5):347–352. doi:10.1097/MCC.0000000000000535
12. Karampatakis T, Tsergouli K, Behzadi P. Carbapenem-resistant Klebsiella pneumoniae: virulence factors, molecular epidemiology and latest updates in treatment options. Antibiotics. 2023;12(2). doi:10.3390/antibiotics12020234
13. Scheuerman O, Schechner V, Carmeli Y, et al. Comparison of predictors and mortality between bloodstream infections caused by ESBL-Producing Escherichia coli and ESBL-producing Klebsiella pneumoniae. Infect Control Hosp Epidemiol. 2018;39(6):660–667. doi:10.1017/ice.2018.63
14. Masterton RG, Galloway A, French G, et al. Guidelines for the management of hospital-acquired pneumonia in the UK: report of the working party on hospital-acquired pneumonia of the British Society for Antimicrobial Chemotherapy. J Antimicrob Chemother. 2008;62(1):5–34. doi:10.1093/jac/dkn162
15. Masterton R, Craven D, Rello J, et al. Hospital-acquired pneumonia guidelines in Europe: a review of their status and future development. J Antimicrob Chemother. 2007;60(2):206–213. doi:10.1093/jac/dkm176
16. Song P, Wei Y, Yu X, et al. The comparison analysis of bloodstream infection caused by Klebsiella pneumoniae versus Escherichia coli: incidence, clinical distribution and drug resistance. Minerva Med. 2022;113(5):879–881. doi:10.23736/S0026-4806.22.08010-7
17. Kang CI, Kim SH, Park WB, et al. Bloodstream infections due to extended-spectrum beta-lactamase-producing Escherichia coli and Klebsiella pneumoniae: risk factors for mortality and treatment outcome, with special emphasis on antimicrobial therapy. Antimicrob Agents Chemother. 2004;48(12):4574–4581. doi:10.1128/AAC.48.12.4574-4581.2004
18. Sung HS, Lee JW, Bae S, et al. Comparison of antimicrobial resistances and clinical features in community-onset Escherichia coli and Klebsiella pneumoniae bacteremia. Korean J Intern Med. 2021;36(2):433–440. doi:10.3904/kjim.2019.272
19. Kalil AC, Metersky ML, Klompas M, et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the infectious diseases society of America and the American thoracic society. Clin Infect Dis. 2016;63(5):e61–e111. doi:10.1093/cid/ciw353
20. Aliberti S, Dela Cruz CS, Amati F, et al. Community-acquired pneumonia. Lancet. 2021;398(10303):906–919. doi:10.1016/S0140-6736(21)00630-9
21. Goepfert RP, Hutcheson KA, Lewin JS, et al. Complications, hospital length of stay, and readmission after total laryngectomy. Cancer. 2017;123(10):1760–1767. doi:10.1002/cncr.30483
22. Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8
23. Paterson DL, Ko WC, Von Gottberg A, et al. International prospective study of Klebsiella pneumoniae bacteremia: implications of extended-spectrum beta-lactamase production in nosocomial Infections. Ann Intern Med. 2004;140(1):26–32. doi:10.7326/0003-4819-140-1-200401060-00008
24. Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European society of intensive care medicine. Intensive Care Med. 1996;22(7):707–710. doi:10.1007/BF01709751
25. Lee J, Hwang JS, Hwang IS, et al. Coprisin-induced antifungal effects in Candida albicans correlate with apoptotic mechanisms. Free Radic Biol Med. 2012;52(11–12):2302–2311. doi:10.1016/j.freeradbiomed.2012.03.012
26. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; 26th informational supplement. CLSI Document M100-S26. Wayne, PA: Clinical and Laboratory Standards Institute; 2016.
27. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; 27th informational supplement. CLSI Document M100-S27. Wayne, PA: Clinical and Laboratory Standards Institute; 2017.
28. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; 28th informational supplement. CLSI Document M100-S28. Wayne, PA: Clinical and Laboratory Standards Institute; 2018.
29. Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; 29th informational supplement. CLSI Document M100-S29. Wayne, PA: Clinical and Laboratory Standards Institute; 2019.
30. Lemeshow S, Hosmer DW Jr. A review of goodness of fit statistics for use in the development of logistic regression models. Am J Epidemiol. 1982;115(1):92–106. doi:10.1093/oxfordjournals.aje.a113284
31. Chen IR, Lin SN, Wu XN, et al. Clinical and microbiological characteristics of bacteremic pneumonia caused by Klebsiella pneumoniae. Front Cell Infect Microbiol. 2022;12:903682. doi:10.3389/fcimb.2022.903682
32. Ingersoll MA. Sex differences shape the response to infectious diseases. PLoS Pathog. 2017;13(12):e1006688. doi:10.1371/journal.ppat.1006688
33. Silveyra P, Fuentes N, Rodriguez Bauza DE. Sex and gender differences in lung disease. Adv Exp Med Biol. 2021;1304:227–258. doi:10.1007/978-3-030-68748-9_14
34. Gill CM, Nicolau DP; Group E-PGS. Carbapenem-resistant Pseudomonas aeruginosa: an assessment of frequency of isolation from ICU versus non-ICU, phenotypic and genotypic profiles in a multinational population of hospitalized patients. Antimicrob Resist Infect Control. 2022;11(1):146. doi:10.1186/s13756-022-01187-8
35. Lakbar I, Medam S, Ronfle R, et al. Association between mortality and highly antimicrobial-resistant bacteria in intensive care unit-acquired pneumonia. Sci Rep. 2021;11(1):16497. doi:10.1038/s41598-021-95852-4
36. Wang C, Yuan Z, Huang W, et al. Epidemiologic analysis and control strategy of Klebsiella pneumoniae infection in intensive care units in a teaching hospital of People’s Republic of China. Infect Drug Resist. 2019;12:391–398. doi:10.2147/IDR.S189154
37. Zeng M, Xia J, Zong Z, et al. Guidelines for the diagnosis, treatment, prevention and control of infections caused by carbapenem-resistant gram-negative bacilli. J Microbiol Immunol Infect. 2023. doi:10.1016/j.jmii.2023.01.017
38. Bengoechea JA, Sa Pessoa J. Klebsiella pneumoniae infection biology: living to counteract host defences. FEMS Microbiol Rev. 2019;43(2):123–144. doi:10.1093/femsre/fuy043
39. Kuo TH, Yang CY, Lee CH, et al. Propensity score matched analysis comparing the clinical outcome of Klebsiella pneumoniae and Escherichia coli causing community-onset monomicrobial bacteremia. Medicine. 2017;96(26):e7075. doi:10.1097/MD.0000000000007075
40. Chen SC, Wu WY, Yeh CH, et al. Comparison of Escherichia coli and Klebsiella pneumoniae liver abscesses. Am J Med Sci. 2007;334(2):97–105. doi:10.1097/MAJ.0b013e31812f59c7
41. Chan KS, Shelat VG. Klebsiella pneumoniae bacteremia is associated with higher mortality in acute calculous cholangitis as compared to Escherichia coli bacteremia. World J Surg. 2022;46(7):1678–1685. doi:10.1007/s00268-022-06559-0
42. Shelat VG, Chia CL, Yeo CS, et al. Pyogenic liver abscess: does Escherichia coli cause more adverse outcomes than Klebsiella pneumoniae? World J Surg. 2015;39(10):2535–2542. doi:10.1007/s00268-015-3126-1
43. Ahmadi M, Ranjbar R, Behzadi P, et al. Virulence factors, antibiotic resistance patterns, and molecular types of clinical isolates of Klebsiella Pneumoniae. Expert Rev Anti Infect Ther. 2022;20(3):463–472. doi:10.1080/14787210.2022.1990040
44. Chi X, Meng X, Xiong L, et al. Small wards in the ICU: a favorable measure for controlling the transmission of carbapenem-resistant Klebsiella pneumoniae. Intensive Care Med. 2022;48(11):1573–1581. doi:10.1007/s00134-022-06881-0
45. Luterbach CL, Chen L, Komarow L, et al. Transmission of carbapenem-resistant Klebsiella pneumoniae in US hospitals. Clin Infect Dis. 2023;76(2):229–237. doi:10.1093/cid/ciac791
46. Liu C, Dong N, Chan EWC, et al. Molecular epidemiology of carbapenem-resistant Klebsiella pneumoniae in China, 2016–20. Lancet Infect Dis. 2022;22(2):167–168. doi:10.1016/S1473-3099(22)00009-3
47. Pang F, Jia XQ, Zhao QG, et al. Factors associated to prevalence and treatment of carbapenem-resistant Enterobacteriaceae infections: a seven years retrospective study in three tertiary care hospitals. Ann Clin Microbiol Antimicrob. 2018;17(1):13. doi:10.1186/s12941-018-0267-8
48. Hu FP, Guo Y, Zhu DM, et al. CHINET surveillance of bacterial resistance across tertiary hospitals in 2019. Chinese J Infect Chemother. 2020;20(3):233–243. doi:10.16718/j.1009-7708.2020.03.001
49. Daikos GL, Tsaousi S, Tzouvelekis LS, et al. Carbapenemase-producing Klebsiella pneumoniae bloodstream infections: lowering mortality by antibiotic combination schemes and the role of carbapenems. Antimicrob Agents Chemother. 2014;58(4):2322–2328. doi:10.1128/AAC.02166-13
50. Kim D, Park BY, Choi MH, et al. Antimicrobial resistance and virulence factors of Klebsiella pneumoniae affecting 30 day mortality in patients with bloodstream infection. J Antimicrob Chemother. 2019;74(1):190–199. doi:10.1093/jac/dky397
51. Brescini L, Morroni G, Valeriani C, et al. Clinical and epidemiological characteristics of KPC-producing Klebsiella pneumoniae from bloodstream infections in a tertiary referral center in Italy. BMC Infect Dis. 2019;19(1):611. doi:10.1186/s12879-019-4268-9
52. Tumbarello M, Viale P, Viscoli C, et al. Predictors of mortality in bloodstream infections caused by Klebsiella pneumoniae carbapenemase-producing K. pneumoniae: importance of combination therapy. Clin Infect Dis. 2012;55(7):943–950. doi:10.1093/cid/cis588
53. Zarkotou O, Pournaras S, Tselioti P, et al. Predictors of mortality in patients with bloodstream infections caused by KPC-producing Klebsiella pneumoniae and impact of appropriate antimicrobial treatment. Clin Microbiol Infect. 2011;17(12):1798–803. 10.1111/j.1469–0691.2011.03514.x.
54. Loncaric I, Beiglbock C, Fessler AT, et al. Characterization of ESBL- and ampc-producing and fluoroquinolone-resistant Enterobacteriaceae isolated from mouflons (Ovis orientalis musimon) in Austria and Germany. PLoS One. 2016;11(5):e0155786. doi:10.1371/journal.pone.0155786
55. John TM, Deshpande A, Brizendine K, et al. Epidemiology and outcomes of community-acquired Escherichia coli pneumonia. Open Forum Infect Dis. 2022;9(1):ofab597. doi:10.1093/ofid/ofab597
56. Luo H, Xiao Y, Hang Y, et al. Comparison of therapy with beta-lactam/beta-lactamase inhibitor combinations or carbapenems for bacteraemia of nonurinary source caused by ESBL-producing Escherichia coli or Klebsiella pneumoniae. Ann Clin Microbiol Antimicrob. 2021;20(1):63. doi:10.1186/s12941-021-00471-6
57. Kim YC, Choi H, Kim YA, et al. Risk factors and microbiological features of recurrent Escherichia coli bloodstream infections. PLoS One. 2023;18(1):e0280196. doi:10.1371/journal.pone.0280196
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





