Back to Journals » Infection and Drug Resistance » Volume 16
Clinical Characteristics and Associated Factors for Infection and in-Hospital Mortality in Inpatients with Polymyositis/Dermatomyositis in China: A Retrospective Study
Authors Lao M , Ouyang H, Li N, Li H, Dai P, Zhan Z, Chen D
Received 2 November 2022
Accepted for publication 6 January 2023
Published 17 January 2023 Volume 2023:16 Pages 289—299
DOI https://doi.org/10.2147/IDR.S392585
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Minxi Lao,1,2,* Hui Ouyang,3,* Nannan Li,1 Hao Li,1 Peiyin Dai,1 Zhongping Zhan,1 Dongying Chen1
1Department of Rheumatology, the First Affiliated Hospital of Sun Yat-sen University, Guangzhou, People’s Republic of China; 2Department of Geriatrics, the First Affiliated Hospital of Sun Yat-sen University, Guangzhou, People’s Republic of China; 3Department of Digestive Medicine Center, the Seventh Affiliated Hospital of Sun Yat-Sen University, Shenzhen, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Dongying Chen; Zhongping Zhan, Department of Rheumatology, the First Affiliated Hospital of Sun Yat-sen University, 58 Zhongshan 2 nd Road, Guangzhou, 510080, People’s Republic of China, Email [email protected]; [email protected]
Purpose: To investigate the clinical features of infection, and associated factor for in-hospital mortality in a southern Chinese cohort with polymyositis/dermatomyositis (PM/DM).
Patients and Methods: Clinical data were retrospectively reviewed from 2015 to 2022 from a tertiary hospital in southern China. Associated factors for infection and in-hospital mortality were analyzed by multivariate logistic regression analysis.
Results: A total of 554 patients with PM/DM were included, and 35.6% (197/554) of them developed 404 episodes of infection. Half of the patients developed infection within 4 months after disease onset. Bacterial infection was predominant (249/404, 61.6%). Lung was the most involved (242/404, 59.9%). Gram-negative bacteria the leading pathogens (64/84, 76.2%). Patients with anti-MDA5 positive were prone to develop severe infections (35.1% vs 16.4%, P< 0.001) and had higher mortality (11.7% vs 3.4%, P=0.01). The in-hospital mortality was 6.5% (36/554). Infection was the leading cause of death (20/36, 55.6%). Older age (adjusted odds ratio (OR): 1.05, 95% confidential interval (CI): 1.02– 1.09, P=0.004), ILD (adjusted OR: 2.76, 95% CI: 1.11– 6.84, P=0.03), number of episodes of infection (adjusted OR: 1.91, 95% CI: 1.53– 2.38, P< 0.001), and elevated serum creatinine (Scr) (adjusted OR: 6.83, 95% CI: 1.77– 26.40, P=0.01) were associated with in-hospital mortality.
Conclusion: Infection is an early complication in PM/DM with a high proportion of lung involvement and predominance of gram-negative bacteria. It is a major contributor to in-hospital mortality. Older age, ILD, and number of episodes of infection are associated with poor prognosis.
Keywords: dermatomyositis, polymyositis, infection, MDA5, mortality
Introduction
Polymyositis/dermatomyositis (PM/DM) is an autoimmune disease characterized by muscular inflammation and weakness. The acute onset of the disease, sometimes with rapid progression, calls for intensive anti-inflammatory treatment including high doses of glucocorticoids (GC) and immunosuppressants. In return, visceral involvement such as interstitial lung disease (ILD) and intensive treatment renders patients with PM/DM more vulnerable to infection.
Infection remains to be a paramount concern in the management of PM/DM. A population-based retrospective study including 15,407 hospitalizations with PM/DM in the USA revealed infection is the strongest predictor of hospital mortality in PM/DM, leading to 4.2-fold increase in the odds of death.1 A Chinese study analyzing 63 deceased patients with PM/DM showed that pulmonary infection alone accounted for 34.9% of the cases, and 25.4% of the patients died of pulmonary infection combined with ILD exacerbation.2 Despite of concerted efforts to mitigate the infection risk, infection remains to be a major cause of death in PM/DM. In this study, we performed a retrospective study in a large sample of patients, aiming to investigate the clinical features and identify the associated factors for infection and in-hospital mortality in PM/DM.
Patients and Methods
Study Design
We performed a retrospective study on consecutive inpatients admitted to the First Affiliated Hospital of Sun Yat-Sen University from January 1st, 2015, to January 1st, 2022. Discharge diagnosis was screened by the 10th version International Classification of Disease 10 (ICD-10) for PM/DM (Appendix 1). Medical records were reevaluated by two independent investigators (N. Li & P. Dai). Patients aged over 18 years old and diagnosed as probable or definite idiopathic inflammatory myopathy (IIM) according to the 2017 EULAR/ACR criteria3,4 were included. Patients were further categorized as DM or PM in the presence or absence of typical rash such as heliotrope rash, Gottron’s papules, or Gotton’s sign. Patients with or without infection were further compared. Deceased patients during hospitalization were recorded and the in-hospital mortality rate (I-HMR) was analyzed. Patients who were diagnosed with overlap syndrome, pregnant, or admitted for other reasons that were unrelated to PM/DM and its complications were excluded.
Definition
Definition of Infection
Infection was defined as stated previously.5 Bacterial infection was diagnosed based on clinical manifestations, microbiological findings, laboratory data, radiographic imaging, and response to antibiotics. Invasive fungal disease (IFD) was diagnosed according to the 2008 European Organization for the Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group Consensus Group criteria.6 Fungal infection only involving the skin, genitalia, and the oral cavity was considered as a superficial fungal infection.7 Pneumocystis jirovecii pneumonia (PJP) was considered probable on the basis of typical clinical, radiographic manifestations and laboratory results. If etiological evidence from pathological staining or next-generation sequencing was present, PJP was confirmed.8 Colonized bacteria or fungi were considered pathogenic if they were isolated from repeated cultures combined with clinical symptoms that cannot be explained otherwise. Acute viral infection was determined according to (i) clinical features; (ii) typical radiographic manifestations; (iii) elevated titers of virus-specific IgM and subsequent IgG or enhanced replication of virus nucleic acid confirmed by polymerase chain reaction (PCR) assay; and (iv) improvement after anti-virus therapy. Cytomegalovirus (CMV) infection is defined as the presence of CMV replication in tissue, blood, or other bodily fluids regardless of symptomatology.9 Positive CMV replication is considered in the case of positive detection of CMV pp65 antigen, replication of CMV nucleic acid > 500 copies/mL, or positive viral culture. In patients with ILD, pulmonary infection was diagnosed based on clinical symptoms (eg, fever, sputum), infection indicators (eg, elevated white blood cells, procalcitonin), radiographic manifestations (eg, increased infiltrates), bronchoscopic findings, and microbial culture. Since this is a retrospective study, treatment response was also taken into consideration. Severe infection was defined as an infection that results in death, requires intravenous antimicrobial medication or advanced life support.10 Infection with one kind of pathogen in one site was counted as one episode. Accordingly, increasing episodes of infection included multiple infections during the same time and recurrent infections at different time points.
ILD
ILD secondary to PM/DM was determined by chest high-resolution computed tomography (HRCT) as described previously.11 The HRCT images were independently reviewed by two rheumatologists (M. Lao & D. Chen) well-trained in the interpretation of chest CT images and blinded to the patients’ baseline data. ILD caused by other diseases such as infection, chronic obstructive pulmonary disease (COPD), lung injury, and drug exposure were not included.
Causes of Death
The causes of death were categorized as: 1) exacerbation of PM/DM, defined as non-infectious manifestations directly attributed to PM/DM, 2) infections, defined as microbiologically documented or clinically presumed infections, 3) concomitant infection and exacerbation of PM/DM, 4) other causes such as acute serious illness unrelated to PM/DM.
Clinical Data
Demographic and clinical data at admission were collected from the medical records. Disease course was counted from the onset of PM/DM-related symptoms to admission. Neutropenia was defined as an absolute neutrophil count < 2.0×109/L. Lymphopenia was defined as peripheral blood lymphocyte count < 1.0×109/L. Anemia was defined as hemoglobin < 120 g/L in males and hemoglobin < 110 g/L in females at sea level. Hypoalbuminemia was defined as a serum albumin level <3.5 g/dl. Elevated serum creatinine (Scr) was defined as Scr > 115 umol/L. Antinuclear antibodies were detected by indirect immunofluorescence. Other myositis-specific antibodies were detected by Western blot. Test for myositis-specific antibodies (MSA) and myositis-associated autoantibodies (MAA) was performed since 2017.
Therapeutic strategies were determined by 2 physicians (Z. Zhan & H. Li). Accumulated dose of GC in one month prior to admission was summed and converted to equivalent prednisolone (PSL) using the following equation: 1 mg of prednisolone = 0.8 mg of methylprednisolone. The use of immunosuppressants prior to admission was recorded, including cyclophosphamide (CYC), mycophenolate mofetil (MMF), tacrolimus (TAC), methotrexate.
Statistical Analysis
Statistical analysis was performed using SPSS 25.0 (SPSS Inc, Chicago, IL, USA). Normally distributed data were presented as mean ± standard deviation (SD), while nonnormal variables were expressed as median (interquartile range, IQR). Categorical variables were presented as frequency and percentage. Comparison between groups was evaluated with chi-square test or Fisher exact test for categorical variables and Student’s t-test for continuous variables with normal distribution. Between-group comparison was evaluated using the Mann–Whitney U-test for continuous variables with nonnormal distribution. Univariate logistic regression was performed on all variables, and clinically significant variables with a P value < 0.1 were adjusted by multivariate logistic regression analyses. The conditioned procedure was applied. A P value < 0.05 was considered statistically significant.
Ethics Approval
Ethics committee of the First Affiliated Hospital of Sun Yat-sen University approved the research (Approval number: 2019422). Informed consents were obtained from the study participants. All the data collection followed the principle of confidentiality. This work was conducted according to the provisions of the Declaration of Helsinki.
Results
Characteristics of Infection
A total of 554 patients, including 401 with DM and 153 with PM were enrolled. The mean age was 49.3±15.3 years and 36.3% were male. The median disease course was 6.0 months. A total of 197 (35.6%) patients developed 404 episodes of infection. Ninety-nine patients (50.3%) developed one episode of infection, 50 patients (25.4%) developed two episodes, and 48 patients (24.4%) developed three episodes or more. Half of the patients (99/197, 50.3%) developed infection within 4 months after disease onset. Severe infection accounted for 77% (311/404) of the episodes. Distribution of infective agents and infective sites are shown in Figure 1A and B.
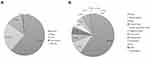 |
Figure 1 Distribution of infective agents and invective sites. (A) Pathogenic agents in all infection. (n=404) (B) Infective sites in all infection. (n=404). Abbreviation: CNS, central nerve system. |
Bacterial infections were predominant, accounting for 61.6% (249/404), followed by fungal infection (93/404, 23.0%), and viral infection (54/404, 13.4%). Seven episodes of tuberculosis infection were diagnosed, of which six were pulmonary tuberculosis and one was skin tuberculosis. Lung is normally involved (242/404, 59.9%), including 1 episode of aspiration pneumonia. Blood stream ranked the second (39/404, 9.7%). Microbial culture was performed in 162 patients. The isolated agents are shown in Supplementary Table S1. A total of 84 strains of bacteria were isolated, mainly from sputum (n=38), blood stream (n=14), and urine (n=12). Gram-negative bacteria accounted for 76.2% (64/84). E.coli (13/64, 20.3%) and P.aeruginosa (11/64, 17.2%) were the leading strains. Gram-positive bacteria accounted for 23.8% (20/84). S.aureus was frequently found (9/20, 45.0%).
Fungal infection accounted for 93 episodes (23.0%). Superficial infection accounted for 41.9% (39/93) of the cases. The majority were candidiasis (38/39, 97.4%). One patient was infected by malasseziosis. Most of the infections occurred in oral cavity (36/39, 92.3%), followed by skin (2/39, 5.1%), and genital tract (1/39, 2.6%). IFD was diagnosed in 54 cases (54/93, 58.1%), including 31 cases of candidiasis (57.4%), 8 cases of aspergillosis (14.8%), 5 cases of PJP (9.3%), 5 cases of cryptococcosis (9.3%), 2 cases of penicilliosis (3.7%), 1 case of trichosporosis (1.9%), 1 case of fusariumsis (1.9%), and 1 case infected by Kodamaea ohmeri (1.9%). Infective sites included lung (23/54, 42.6%), urinary tract (15/54, 27.8%), digestive tract (13/54, 24.1%), eye (2/54, 3.7%), and blood stream (1/54, 1.9%). A total of 68 strains of fungi were isolated, mainly from throat swabs (n=20), urine (n=15), stool (n=13), and sputum (n=9). More than half (53/68, 77.9%) were Candida spp. Eight strains (11.8%) of Aspergillus spp. were identified.
Viral infection was found in 54 (13.4%) episodes. Of note, 27 episodes (50.0%) were CMV infection, among which 24 episodes were asymptomatic, and 3 episodes were cytomegalovirus pneumonia. Five cases (9.3%) were HSV infection, and 7 episodes (13.0%) were herpes zoster. The other eight episodes (14.8%) were nonspecific viral infections.
Comparison Between Patients with or Without Infection
Patients with infection were older (52.5±14.6 vs 47.5±15.5, P<0.001), more likely to have ILD (51.8% vs 38.1%, P=0.002), lymphopenia (56.3% vs 35.9%, P<0.001), anemia (42.1% vs 24.6%, P<0.001), hypoalbuminemia (59.9% vs 43.1%, P<0.001), and received higher dose of PSL (300mg vs 150mg, P=0.01) than those without (Table 1).
 |
Table 1 Comparison Between Patients with or without Infection |
Infection in Patients with Specific Myositis Antibodies
MSA/MAA were detected in 301 patients. Interestingly, the positive rate of anti-EJ (6.9% vs 1.0%, P=0.01) and anti-JO1 (19.8% vs 9.5%, P=0.01) antibodies was higher in patients with infection. (Supplementary Table S2) Considering anti-MDA5-positive amyopathic dermatomyositis and anti-JO1 positive antisynthetase syndrome are two common subtypes in PM/DM, we further analyzed the infection patterns in these patients.
Patients with anti-MDA5 positive were more likely to develop infection, including increasing episodes (11.7% vs 4.3%, P=0.02) and severe infection (35.1% vs 16.4%, P<0.001). The in-hospital mortality in patients with anti-MDA5 positive was remarkably higher than those with anti-MDA5 negative (11.7% vs 3.4%, P=0.01). (Table 2) Major causes of death included infection (5/11, 45.5%) and the exacerbation of PM/DM combined with infection (4/11, 36.4%).
 |
Table 2 Comparison Between Patients with Different MSA/MAA |
ILD was more common in patients with anti-JO1 positive (64.1% vs 45.4%, P=0.03). Patients with anti-JO1 positive were prone to develop severe infection (46.2% vs 28.2%, P=0.02). All-cause mortalities in the two groups were comparable (Table 2).
Comparison Between Patients with DM and PM
Features of infection were compared in 148 DM patients with 309 episodes of infection and 49 PM patients with 95 episodes of infection. Neither the infective agents nor infective sites differed between groups (Supplementary Table S3).
In-Hospital Mortality
Thirty-six patients died during hospitalization and 35 of them were in the infection group. The I-HMR was 6.5% (36/554), and it was much higher in the infection group than that in the control group (17.8% vs 0.3%, P<0.001). The causes of death included infection (20/36, 55.6%), exacerbation of PM/DM combined with severe infection (9/36, 25.0%), and exacerbation of PM/DM (4/36, 11.1%). A total of 102 episodes of infection occurred in 35 deceased patients in the infection group, including 81 episodes (79.4%) of severe infection. In deceased patients, bacterial infection was the most frequent (50/102, 49.0%), followed by fungal infection (32/102, 31.4%), and viral infection (18/102, 17.6%). The most common infective sites were lung (60/102, 58.8%) and blood stream (19/102, 18.6%). Isolated agents and infection sites from 27 patients with etiological evidence are shown in Table 3. Of note, 11 (40.7%) of them developed multiple infections.
 |
Table 3 The Isolated Agents in Infective Sites in Deceased Patients |
Comparison between patients alive and dead was performed. Non-survivors were older (60.2±11.8 vs 48.6±15.1 years, P<0.001) and complicated with COPD (5.6% vs 0.6%, P=0.04) or ILD (72.2% vs 40.9%, P<0.001). Lymphopenia (66.7% vs 41.5%, P=0.003), elevated Scr (13.9% vs 1.9%, P=0.002), and hypoalbuminemia (80.6% vs 46.9%, P<0.001) were more frequent in non-survivors. It’s worth noting that the occurrence of infection (72.2% vs 28.6%, P<0.001), including episodes and severe infection (97.2% vs 27.4%, P<0.001) increased remarkably in non-survivors (Table 4).
 |
Table 4 Comparison Between Patients Alive and Dead |
Associated Factors for Infection and in-Hospital Mortality
Variables with clinical significance for infection and a P value < 0.1 in univariate logistic regression analysis were shown in Supplementary Table S4. As a result, older age [adjusted odds ratio (OR): 1.02, 95% confidential interval (CI): 1.00–1.03, P=0.02], ILD (adjusted OR: 1.57, 95% CI: 1.09–2.28, P=0.02), lymphopenia (adjusted OR: 1.91, 95% CI: 1.31–2.77, P=0.001), and anemia (adjusted OR: 1.78, 95% CI: 1.20–2.64, P=0.004) were associated factors for infection in PM/DM (Figure 2A).
Factors with clinical and statistical significance for in-hospital mortality by univariate logistic regression were shown in Supplementary Table S5. Considering the 95% CI in some variables such as patients with infection and patients with severe infection were too wide, we excluded them from multivariate logistic regression analysis. Accordingly, older age (adjusted OR: 1.05, 95% CI: 1.02–1.09, P=0.004), ILD (adjusted OR: 2.76, 95% CI: 1.11–6.84, P=0.03), increasing episodes of infection (adjusted OR: 1.91, 95% CI: 1.53–2.38, P<0.001), and elevated Scr (adjusted OR: 6.83, 95% CI: 1.77–26.40, P=0.01) were associated factors for in-hospital mortality (Figure 2B).
Discussion
We are the first to report the infectious pattern in patients with PM/DM from southern China. In this retrospective study, we showed the high incidence of infection in PM/DM, especially during early disease. Severe infections are common. Gram-negative bacteria are the leading pathogens. Lung is frequently involved. Infection in patients with different MSA/MAA exhibits unique features. Infection is the leading cause for in-hospital mortality. Older age, ILD, elevated Scr and number of episodes of infection are an important associated factor for mortality.
Infection is one of the major concerns in CTD. However, most of the studies focus on infection in patients with systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), or ANCA-associated vasculitis (AAV). Indeed, 35.6% of the patients with PM/DM experienced infection in our study, and 77% were severe infections. The prevalence is comparable with previous reports (28–37%).12,13 Half of the patients developed at least two episodes of infection during the observation period. Infection is likely to occur within four months from the onset of PM/DM-related symptoms, ie, the early stage of the disease. One of the reasons could be that in this period, the disease is usually active and aggressive treatment is required, resulting in severe immunosuppression. Our findings emphasize the likelihood of infection in patients with PM/DM, especially during the first four months after disease onset. Severe infections are not infrequent.
In consistent with previous reports,11,14 bacterial pneumonia is the most common pattern. Fungal infection and viral infections accounted for one-third. In agreement with previous findings, gram-negative bacteria are the leading pathogenic agents. However, the distribution of specific pathogens varies. In our study, E.coli and P.aeruginosa were frequent, while Klebsiella and Acinetobacter were the primary pathogenic agents in other studies.12,13 Among gram-positive bacteria, S. aureus came first. Accordingly, empiric antibiotics covering gram-negative bacterial, including E.coli and P.aeruginosa are considered as the first choice to treat bacterial infection in PM/DM.
MSA/MAA profile is differently expressed in patients with or without infection. Patients with anti-MDA5 positive or anti-synthetase antibodies are two subgroups with unique clinical features. In a recent study performed in northern China, PM/DM patients with infection were more likely to be anti-MDA5 positive and less likely to be anti-JO-1 positive.13 Positive rate of anti-MDA5 in the infection group in our study was higher than that in the control group, although no statistical significance was reached. Lack of data in MSA/MAA profile in 253 patients may lead to statistical discrepancies. Alternatively, we noticed the number of infection episodes, especially severe infection increased in patients who were anti-MDA5 positive. Infection appeared to be a major cause of death in this group. Some studies found the higher expression of anti-JO1 antibody in non-infective patients.13 A multicenter retrospective study including 828 patients from Europe and America revealed the presence of anti-synthetase antibodies does not influence the survival of idiopathic inflammatory myositis (IIM).15 Another Chinese retrospective study enrolling 124 patients found none of the four anti-synthetase antibodies (ie, anti-EJ, anti-PL7, anti-PL12, anti-JO1) is a predictor for poor prognosis in the long term.16 Neither of these studies compared the infection rate between patients with or without anti-synthetase antibodies. In the current study, severe infection seemed to increase in patients with anti-JO1 positive. In consistence with previous reports, the mortality was not associated with the presence of anti-JO1 antibody. Our study reveals the relatively benign outcome in patients with anti-JO1 antibodies.
Many variables such as older age, ILD were suggested as risk factors for infection in IIM.8,9,17 Of note, lymphopenia is recognized continuously as a main contributor to infection, despite the variance in study design. In agreement, lymphopenia remains to be an associated factor for infection in our study. The average count of lymphocytes was 0.9×109/l. It suggests that the count of lymphocytes even decreased slightly, is an important associated factor for infection, and requires close surveillance.
The all-cause mortality of IIM ranges from 4% to 35%.1,18,19 In our study, it was 6.5%, close to a recent survey from northern China (6.4%),20 and higher than that in patients with other CTDs such as SLE from the same center (2.1%).5 The median disease course was 3.6 months, indicating that death is likely to occur during the early stage of disease. The in-hospital mortality in the infection group was 17.8%, apparently higher than that in non-infection group (0.3%). Nearly half of the deceased patients developed multiple infections. Rational use of antibiotics and prevention against superinfection should be a major concern in clinical practice. Despite of different combinations of variables, infection continues to be a strong predictor for mortality in IIM.21,22 Cumulative mortality at one year after the diagnosis of IIM was reported to be 9%.23 However, the survival rate dropped to 68.3% at one year after the first episode of major infection.12 A Chinese cohort study showed similar results that survival declined to 78.1% at one year after the first occurrence of infection, compared with 96.3% in those without.13 We also established the association between increased mortality and number of episodes of infection, which suggests that multiple infections at the same time or recurrent infections are associated with poor prognosis.
Strengths and Limitations
Infection in PM/DM is less frequently reported compared with that in SLE or RA, and only a few studies were conducted enrolling a large number of patients. However, infection is an absolutely crucial problem in treating PM/DM. Infections occurring in different populations or different regions possess their own characteristics. In this study, we reported the infectious pattern in a large number of Chinese patients, providing details regarding to infection episodes, pathogens, severity, and causes for in-hospital mortality. We believe our findings will provide important information for the prevention of infection in PM/DM. This study has some drawbacks, however. Data were generated from a tertiary hospital which receives patients who are difficult to treat. Only inpatients records were available in our electronic database. Therefore, outpatients were not included. The selection bias may influence the estimates. Besides, MSA/MAA was routinely checked only after the year 2017, and unavailable data in some patients hindered further analysis of the role of MSA/MAA in infection.
Conclusions
Infection is a severe complication of PM/DM and a major contributor to in-hospital mortality. Bacteria are the leading pathogens, especially gram-negative bacteria such as E. coli and P.aeruginosa. Lung is frequently involved. Accordingly, increased vigilance combined with prophylaxis against pyogenic infections, including regular physical examination of the lungs, are necessary for the timely diagnosis of infection in patients with PM/DM, especially in those with advanced age, anti-MDA5 positive, ILD or lymphopenia.
Funding
This project was supported by grants from the Natural Science Foundation of Guangdong Province (2022A1515010911), and Guangzhou science and Technology Program Project (202201011824).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sara M, Gabriela S, Laura T, et al. A population-based study of infection-related hospital mortality in patients with dermatomyositis/polymyositis. Arthritis Care Res. 2015;67:673–680. doi:10.1002/acr.22501
2. Wu C, Wang Q, He L, Yang E, Zeng X. Hospitalization mortality and associated risk factors in patients with polymyositis and dermatomyositis: a retrospective case-control study. PLoS One. 2018;13:e0192491. doi:10.1371/journal.pone.0192491
3. Lundberg IE, Tjärnlund A, Bottai M, et al. 2017 European League Against Rheumatism/American College of Rheumatology classification criteria for adult and juvenile idiopathic inflammatory myopathies and their major subgroups. Ann Rheum Dis. 2017;76:1955–1964. doi:10.1136/annrheumdis-2017-211468
4. Simone B, Maryam D, Antonella N, et al. Performance of the new EULAR/ACR classification criteria for idiopathic inflammatory myopathies (IIM) in a large monocentric IIM cohort. Semin Arthritis Rheum. 2020;50:492–497. doi:10.1016/j.semarthrit.2019.12.001
5. Dongying C, Jingyi X, Haihong C, et al. Infection in Southern Chinese Patients with Systemic Lupus Erythematosus: spectrum, Drug Resistance, Outcomes, and Risk Factors. J Rheumatol. 2016;43:1650–1656. doi:10.3899/jrheum.151523
6. Ben P, Thomas W, Peter D, et al. European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group; National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group (2008) Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses. Clin Infect Dis. 2008;46:1813–1821. doi:10.1086/588660
7. Scientific working group. The diagnosis and treatment of Candidiasis: the expert consensus. Clin J Infect Chemother. 2011;11:11–95.
8. Cooley L, Dendle C, Wolf J, et al. Consensus guidelines for diagnosis, prophylaxis and management of Pneumocystis jirovecii pneumonia in patients with haematological and solid malignancies. Intern Med J. 2014;44:1350–1363. doi:10.1111/imj.12599
9. Razonable R, Humar A. Cytomegalovirus in solid organ transplant recipients-guidelines of the American Society of Transplantation Infectious Diseases community of practice. Clin Transplant. 2019;33:e13512. doi:10.1111/ctr.13512
10. Andrew R, Sujith S, Kimme H, James G. Serious infection across biologic-treated patients with rheumatoid arthritis: results from the British Society for Rheumatology Biologics Register for Rheumatoid Arthritis. Ann Rheum Di s. 2018;77:905–910.
11. Nishino M, Itoh H, Hatabu H. A practical approach to high-resolution CT of diffuse lung disease. Eur J Radiol. 2014;83:6–19. doi:10.1016/j.ejrad.2012.12.028
12. Isabelle M, Jean-François M, Eric H, et al. Infectious complications in polymyositis and dermatomyositis: a series of 279 patients. Semin Arthritis Rheum. 2011;41:48–60. doi:10.1016/j.semarthrit.2010.08.003
13. Chen IJ, Tsai WP, Wu YJ, et al. Infections in polymyositis and dermatomyositis: analysis of 192 cases. Rheumatology. 2010;49:2429–2437. doi:10.1093/rheumatology/keq279
14. Yong G, Xiao S, Lin H, Guo W, Xin L. Infection is not rare in patients with idiopathic inflammatory myopathies. Clin Exp Rheumatol. 2022;40:254–259. doi:10.55563/clinexprheumatol/yps7ai
15. Lorenzo C, Ernesto TA, Federica M, et al. Influence of Antisynthetase Antibodies Specificities on Antisynthetase Syndrome Clinical Spectrum Time Course. J Clin Med. 2013;8:2013.
16. Shi J, Li S, Yang H, et al. Clinical Profiles and Prognosis of Patients with Distinct Antisynthetase Autoantibodies. J Rheumatol. 2017;44:1051–1057. doi:10.3899/jrheum.161480
17. Marie I, Hachulla E, Chérin P, et al. Opportunistic Infections in Polymyositis and Dermatomyositis. Arthritis Rheum. 2005;53:155–165. doi:10.1002/art.21083
18. Marie I, Hachulla E, Hatron PY, et al. Polymyositis and dermatomyositis: short term and longterm outcome, and predictive factors of prognosis. J Rheumatol. 2001;28:2230–2237.
19. Marie I, Hachulla E, Chérin P, et al. Interstitial lung disease in polymyositis and dermatomyositis. Arthritis Rheum. 2002;47:614–622. doi:10.1002/art.10794
20. Wu C, Wang Q, He L, Yang E, Zeng X. Hospitalization mortality and associated risk factors in patients with polymyositis and dermatomyositis: a retrospective case-control study. PLoS One. 2018;13:e0192491.
21. Yang X, Hao Y, Zhang X, et al. Mortality of Chinese patients with polymyositis and dermatomyositis. Clin Rheumatol. 2020;39:1569–1579. doi:10.1007/s10067-019-04910-w
22. Marie I. Morbidity and mortality in adult polymyositis and dermatomyositisX. Curr Rheumatol Rep. 2012;1:275–285. doi:10.1007/s11926-012-0249-3
23. Dobloug GC, Svensson J, Lundberg IE, Holmqvist M. Mortality in idiopathic inflammatory myopathy: results from a Swedish nationwide population-based cohort study. Ann Rheum Dis. 2018;77:40–47. doi:10.1136/annrheumdis-2017-211402
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

