Back to Journals » Infection and Drug Resistance » Volume 16
Clinical and Molecular Profile of Carbapenem Resistant Klebsiella pneumoniae Infections in a Tertiary Care Hospital –Mangalore
Authors Pattolath A , Adhikari P , Pai V
Received 16 March 2023
Accepted for publication 15 June 2023
Published 4 July 2023 Volume 2023:16 Pages 4335—4348
DOI https://doi.org/10.2147/IDR.S411056
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Athira Pattolath,1 Prabha Adhikari,1 Vidya Pai2
1Department of Geriatric Medicine, Yenepoya Medical College Hospital, Yenepoya Deemed to be University, Mangalore, Karnataka, India; 2Department of Microbiology, Yenepoya Medical College Hospital, Yenepoya Deemed to be University, Mangalore, Karnataka, India
Correspondence: Prabha Adhikari, Department of Geriatric Medicine, Yenepoya Medical College Hospital, Yenepoya Deemed to be University, University Road, Deralakatte, Mangalore, Karnataka, 575018, India, Tel +91 9880991290, Fax +91 0824-2204664, Email [email protected]
Purpose: Carbapenemase producing Klebsiella pneumoniae infection has increased in recent years, leading to limitations in treatment options. The present study was undertaken to detect the Carbapenemase-producing genes in K. pneumoniae, the risk factors for acquiring them, and their impact on clinical outcomes.
Patients and Methods: This prospective study included 786 clinically significant K. pneumoniae isolates. Antimicrobial susceptibility testing was done by conventional method, carbapenem-resistant isolates were screened by carba NP test, and positive isolates were further evaluated by multiplex PCR method. The patient’s clinical and demographic details, co morbidity, and mortality were collected. Multivariate analysis was performed to check risk factors for acquiring CRKP infection.
Results: The results of our study showed high prevalence of CRKP (68%). The variables subjected to the multivariate analysis found that diabetes, hypertension, cardiovascular disease, COPD, use of immunosuppressants, previous hospitalization history, previous surgery, and parenteral nutrition are found to be significantly associated with carbapenem resistant K. pneumoniae infection. Clinical outcomes revealed that patients in the CRKP group had higher risk of mortality and were discharged against medical advice, and they also had higher rate of septic shock. Most of the isolates carried blaNDM-1 and blaOXA-48 carbapenemase genes. Additionally, the co-existence of blaNDM-1 and blaOXA-48 was found in our isolates.
Conclusion: The prevalence of CRKP was alarmingly high in our hospital with the limited choice of antibiotics. This was associated with high mortality and morbidity with the increase in health care burden. While this information is important to treat critically ill patients with higher antibiotics, strict infection control practices need to be in place to prevent the spread of these infections in the hospital. Clinicians need to be aware of this infection to use appropriate antibiotics to save the lives of critically ill patients with the infection.
Keywords: K. pneumoniae, antimicrobial resistance, carbapenemase, risk factors
Introduction
Klebsiella pneumoniae is a common Enterobacteriaceae in hospitals and the general public that can cause several disorders, including cardiovascular diseases, cystitis, and respiratory diseases.1 When the host’s immune system is weakened or skin tissue is injured, the pathogen can easily enter the host and cause infections through the respiratory tract, blood, urinary system, etc., leading to an extended hospital stay and greater medical costs. Additionally, K. pneumoniae multi-drug resistant (MDR) strains are one of the most significant bacteria causing nosocomial infections (hospital acquired illnesses) and pose a substantial threat to patient life.2
According to the World Health Organization’s assessment of the global status of antibiotic resistance, K. pneumoniae is one of the top three bacteria of global concern because many antibiotics used to treat bacterial diseases are losing their efficacy.3 Furthermore, among the top ten MDR bacteria in intensive care units, K. pneumoniae strains are now the second most prevalent MDR bacteria.4
Carbapenem antibiotics, which include meropenem, ertapenem, and imipenem, are β-lactam antibiotics with a β-lactam ring and a broad spectrum of activity and utility. These antibiotics are used as a last resort to treat infections brought on by extended-spectrum β-lactamases (ESBL) producing organisms and MDR-GNBs.5 However, as carbapenem antibiotics become more widely used, the status of MDR K. pneumoniae worsens, resulting in more significant clinical treatment failure and death.6
Carbapenem resistance can be due to porin mutations, efflux pumps, or carbapenemase synthesis. Although there is an expansion in the number of emerged carbapenemases, five important members that belong to three Ambler classes are the most studied, namely, class A; Klebsiella pneumoniae carbapenemases (blaKPC), Class B; New Delhi metallo β-lactamases (blaNDM), Verona integron-encoded metallo β-lactamases (blaVIM), Active on imipenem metalloβ-lactamases (blaIMP), and class D; Oxacillinase-48-like carbapenemases (blaOXA-48-like).7 According to the Antimicrobial Resistance Reference Gene database maintained by the National Centre for Biotechnology Information (NCBI), these carbapenemases have several variations. The “big five” carbapenemases also vary in their geographic distribution and epidemiological status, which might be either endemic or limited to reported cases.8 These newly-emerging Carbapenem resistant K. pneumoniae (CRKP) classes in K. pneumoniae linked to life-threatening illnesses have been widely reported.9 This pathogen poses a significant risk to human health,10 and it is also a distinct risk factor for nosocomial infection and mortality.11 The emergence of MDR strains has become a critical issue that must be addressed, notably in the case of CRKP. Prevention, inhibition of CRKP infection, and investigation of drug resistance mechanisms have emerged as a contemporary problem in research focus.
CRKP has spread globally, but there are regional variations in the strains.12,13 An observational study in the United States found spatial variance in the CRKP incidence rate, which indicated general emergence and dispersion.14 In China, the frequency of CRKP ranges from 0.9% to 23.6% in different provinces,15 and hence drug resistance status may vary endemically.16 Furthermore, among carbapenemase-producing strains, the incidence of K. pneumoniae carbapenemase (KPC) is lower in Spain than in Greece, and the prevalence of New Delhi metallo β-lactamase (NDM) is notably high in India.17
Despite the large number of research on carbapenem resistant K. pneumoniae infections, the clinical consequences for specific regional areas have not been thoroughly investigated. Therefore, we proposed this study, in which the prevalence of CRKP, risk factors for developing CRKP infection, and clinical profile, which include outcomes of severity and mortality, as well as phenotypical and genotypical characteristics of carbapenemase production were detected.
Materials and Methods
Study Design
Prospective study.
Study Setting
Yenepoya Medical College Hospital, Mangalore, South Karnataka, India
Study Duration
Two years and three months (April 2019-March 2021).
Selection Criteria
Inclusion Criteria
- Patient sample which shows the presence of K. pneumoniae isolates which are clinically significant.
- Age >18 years.
- A single strain of K. pneumoniae per patient.
- Only those isolates of K. pneumoniae obtained as pure growth from clinical samples.
- Inpatients.
Exclusion Criteria
- Polymicrobial infection (Isolation of K. pneumoniae along with other bacteria or fungal organism).
Ethical Statement
The study was conducted according to the guidelines of the World Medical Association Helsinki Declaration for studies on human subjects. It was approved by the Institutional Ethics Committee Board (protocol number YEC-1 2019/038, Dated 11-04-2019) of Yenepoya Deemed to be University. Only participants who gave their informed consent were enrolled in the study.
Isolation & Identification of Bacterial Strain
A total of 786 K. pneumoniae isolates were isolated and identified using the standard manual conventional method from routine clinical samples, such as blood, urine, pus, sputum, endotracheal tube aspirate, and broncho-alveolar lavage (BAL) fluid culture. The samples were inoculated into blood agar, MacConkey agar, and Nutrient agar. Blood and respiratory samples were inoculated on chocolate agar as well. Gram staining was done for the growth on the plates following an overnight incubation at 37 °C. In order to identify K. pneumoniae, biochemical tests, including the catalase test, oxidase test, indole test, citrate utilization test, urea hydrolysis test, motility test, triple sugar iron test, decarboxylase test, methyl red, Voges–Proskauer test, Hugh and Leifson OF test, and nitrate reduction test were carried out.18 The HiMedia Laboratories Pvt. Ltd., Mumbai, India, provided all the media and reagents. The BD Phoenix M50 system (BD Diagnostic Systems, Oxford, UK) was used for additional confirmation.
Antibiotic Susceptibility Testing
According to recommendations from the Clinical Laboratory Institute (CLSI), bacterial susceptibility to antimicrobial drugs was assessed using the traditional Kirby Bauer’s disc diffusion method (in vitro) with Mueller Hinton agar (MHA) plates.19 The K. pneumoniae suspension adjusted to 0.5 McFarland turbidity standards (1x108 CFU/mL) was added to the MHA plates. Amikacin, ampicillin, aztreonam, amoxicillin-clavulanic acid, cefotaxime, ceftazidime, chloramphenicol, ciprofloxacin, gentamicin, imipenem, levofloxacin, meropenem, piperacillin, piperacillin-tazobactam, colistin, and tetracycline were among the antimicrobial discs evaluated. At 37°C, the plates were incubated overnight. The inhibition zones were measured, and the outcomes were compared to the chart of a typical assessment. The ATCC25922 strain of E. coli was chosen as a quality control strain. K. pneumoniae isolates resistant to three or more classes of antibiotics were considered multidrug resistant (MDR).20
Collection of Clinical Information & Risk Factor Analysis
Medical records were reviewed and collected if K. pneumoniae was discovered 48 hours after admission. The following information was documented for the analysis: demographics; chronic illnesses and pathological conditions, such as diabetes mellitus, a solid tumour, cardiovascular disease, respiratory disease, renal disease, hepatic disease, and central nervous system disease; history of hospitalisation within the previous six months; antibiotic therapy administered in the 30 days prior to the positive culture; and recent (1 month) surgical procedure and recent invasive procedures (Parenteral nutrition, central venous, urinary or gastric insertion, and mechanical ventilation).
All patients were monitored for the following outcomes: Mortality, DAMA (Discharged Against Medical Advices), development of sepsis (blood stream infection), length of stay in ICU, evaluation of SOFA score in ICU patients, and duration of mechanical ventilation for the patients.
MIC Determination by Broth Micro-Dilution Method
According to CLSI recommendations, the broth micro-dilution method was carried out. 0.5 McFarland suspension of the isolates was made and diluted 100-fold with cation-adjusted Mueller–Hinton broth (CAMHB). About 50 μL of the bacterial solution was seeded into a 96-well plate with 50 μL of CAMHB and serial antibiotic concentrations. There were roughly 5×105 CFU/mL of bacteria in the final inoculum. The final concentrations of meropenem were 128 μg/mL, 64 μg/mL, 32 μg/mL, 16 μg/mL, 8 μg/mL, 4 μg/mL, 2 μg/mL, 1 μg/mL, 0.5 μg/mL, 0.25 μg/mL and 0.125 μg/mL. The suspension was cultured at 35°C for 18 to 20 hours.19
Phenotypic Confirmatory Disc Diffusion Test (PCDDT) for ESBL
Phenotypic assays among probable ESBL generating isolates verified ESBL production. The third-generation cephalosporins ceftazidime (30µg) and ceftazidime clavulanic acid (30/10 µg) discs were positioned 25 mm apart on a lawn growth of the microorganism. The zone of inhibition for ceftazidime-clavulanic acid increased by around 5mm when contrasted to ceftazidime, indicating that it produces ESBLs. For ESBL test quality control, K. pneumoniae ATCC 700603 and E. coli ATCC 25922 were used.19
Phonotypical Detection of Carbapenemase Production by Carba NP Test
The test was performed in accordance with Nordmann, Poirel, and Dortet's description of how it should be done: “A change in color of the pH indicator is indicative of carbapenem hydrolysis induced by carbapenemase producing bacteria, which create acid”.8 The steps were carried out according to the manufacturer’s instructions. API suspension media (25 µL; bioMérieux, New Delhi, India) was added to the wells, and 5–6 colonies from the fresh culture plate were collected and placed in the prescribed well. The turbidity of the inoculum was compared to that of the supplied strip. Following that, 10 µL of inoculum was added to two wells, one of which contained imipenem. Imipenem was utilized as the carbapenemase zinc substrate for metallo β-lactamases (MBL)-producing gram-negative bacteria, and the results were considered positive if the color changed from red to yellow, orange, or thick orange in comparison to the control well.19,21 Further tests were performed on organisms that tested positive for carbapenemase.
Molecular Detection of Carbapenemase Genes
Extraction of Bacterial DNA
DNA was extracted using HiPurA® Genomic DNA Purification kits (Hi-Media®, India), which rely primarily on the reversible nucleic acid-binding characteristics of the improved silica gel membrane and the speed and versatility of Miniprep spin columns to produce high-quality DNA. The process consists of three fundamental steps. First, test DNA was allowed to bond to the silica-gel membrane of the HiEluteMiniprep spin column after being extracted from the log-phase bacterial culture by centrifugation and lysed by lysozymes. The second phase involved removing leftover contaminants as a contaminant passed through the membrane, and the third step involved eluting and collecting pure genomic DNA in a tube. DNA from the bacteria was extracted, eluted from the columns in 200 µL elution buffer, and then kept at −20°C in a small Eppendorf tube.
Multiplex PCR Assay
To find particular regions of the gene that encode the carbapenemase enzyme, such as blaVIM, blaNDM-1, blaKPC, blaOXA-48, and blaIMP, the carbapenemase gene (multiplex) probe-based Hi-Media Hi-PCR kit has been used. This kit can precisely identify one or a combination of carbapenemase genes in a single-tube reaction with a wide range of organisms. The company’s recommendations were followed using positive, internal, and negative controls.
The multiplex probe PCR kit is made to find specific areas of the genes that produce different carbapenemase enzymes. This technique is used to amplify the targeted DNA sequence by use of hydrolysis probes that are short oligonucleotides, that have a fluorescent reporter dye attached to the 5’end and a quencher dye to the 3’end. The details of primers and probes22 for blaNDM, blaKPC, blaIMP, blaOXA-48, and blaVIM are shown in Table 1. We used two multiplex assays to identify two combinations of five carbapenemase genes and an internal control; Set 1 and Set 2 contained blaNDM, blaKPC, blaIMP, blaVIM, and blaOXA-48, respectively. In this kit, there are two master mixes. Master mix-1 detects blaNDM-1, blaKPC, blaIMP, and blaVIM in the FAM, HEX, Texas Red, and Cy5 channels, while master mix-2 detects blaOXA-48 in the Texas Red channel. In both final mixes, the Cy5.5 channel contained evidence of internal control.
 |
Table 1 Primers and Probes Used in the Multiplex, Real-Time PCR Test |
A 25µL reaction mixture consisting of 5 µL sample DNA and 20 µL master mix was used for this assay. For each reaction, the master mix contained 12.5 µL Hi-Quanti 2X Realtime PCR master mix (MBT180); 4µL of each CRGI/CRG2Primer-Probe Mix (DS0949/DS0950); 1µL internal control Primer-Probe Mix (DS0498); 1µL Internal control B DNA (DS0385A); 5µLTemplate DNA and 1.5µL Molecular biology-grade water (ML065). The two master mixes (CRG1 and CRG2) were prepared as described in Table 2. Then, 10μL of CRG1 and CRG2 were transferred to the PCR cartridge, and run the PCR. The cycling procedure included 10 minutes of initial denaturation at 95°C, followed by 5 seconds of denaturation at 95°C, 45 cycles of annealing and extension at 60°C for one minute, and a final holding stage in SLAN-96P real-time PCR system. A cycle threshold value of ≤40 was considered positive. In a single-tube reaction, the kit enables the accurate and precise detection of both single and co-present carbapenemase-encoding genes.22,23
 |
Table 2 Composition of Master Mix for Detecting blaNDM, blaKPC, blaVIM, blaIMP, and blaOXA48gene |
Statistical Analyses
Continuous variables were reported as means and standard deviations (SDs) if they were normally distributed or as medians and interquartile ranges (IQRs) when they were not. Categorical variables have been given as frequencies and percentages. Depending on how they were distributed, categorical variables were compared using chi-square or Fisher’s exact tests. Continuous variables were compared using Student’s t-tests or Mann–Whitney U-tests. The significant risk factor for acquiring CRKP was determined by using univariate analysis. For testing the null hypothesis, a P-value of 0.5 was selected as the level of significance. Stepwise multiple logistic regression analyses of the risk factor for CRKP infection were also computed for variables deemed significant on standard statistical analysis to discover independent risk factors. IBM SPSS STATISTICS (version 23.0, New York, USA) was used to analyze all the data.
Results
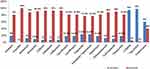
In the current investigation, 786 consecutive nonduplicate K. pneumoniae isolates were obtained from a tertiary care teaching hospital in Mangalore between April 2019 and March 2021. Among all the K. pneumoniae identified (n = 786), 42% (n = 330/786) were in pus, 26% (n = 204/786) in respiratory specimens, 20.3% (n = 160/786) in urine, and 11.7% (n = 92/786) in blood. Figure 1 depicts the distribution of K. pneumoniae isolates from clinical samples in the various treatment units. The most significant contributor to CRKP (29.8%, 160/536) was the medical ICU, whereas most CSKP isolates (31.6%, 79/250) were found in the surgical ward (Figure 2).
 |
Figure 1 Distribution of CRKP isolates in various departments of hospital. |
 |
Figure 2 Distribution of CSKP isolates in various departments of hospital. |
Comparison of Clinical Characteristics, Risk Factor Analysis, and Outcome
Patients with CRKP isolates had a mean age of 62.78± 6.7 years. Thirty-four percent of participants who had an infection with K. pneumoniae were female, while 66% were male. Nearly half of the patients infected with CRKP had an underlying condition such as diabetes, poor glycemic control, or hypertension. The majority of CRKP patients had undergone invasive procedure. Patients in the CRKP group had a greater rate of exposure to antibiotics and prior hospitalization when compared to the CSKP group.
According to univariate analysis, key risk factors included: smoking habit (P = 0.04), having diabetes (P = 0.001), having poor glycemic control (P = 0.001), hypertension (P = 0.001), having a tuberculosis infection (P = 0.001), having chronic kidney disease (CKD) (P = 0.001), having cardiovascular disease (CVD) (P= 0.001), having COPD (P= 0.003), having used immunosuppressive therapy (P = 0.001), and having had surgery in the past (P = 0.001). The univariate analysis also determined that indwelling devices such as urine catheters, nasogastric insertion, parenteral nutrition, and central venous catheter were significantly associated with CRKP infection. Table 3 displays the findings of the univariate analysis of the clinical traits in K. pneumoniae infected participants.
 |
Table 3 Comparison of Clinical Characteristics of CSKP and CRKP Isolates by Univariate Analysis |
Outcome measurements in K. pneumoniae patients found that infection-related mortality was considerably greater in CRKP patients compared to CSKP patients. We found that the SOFA score (P = 0.001) was higher in the CRKP group with regard to the ICU admission status. There were 107 fatalities, of which 97 (90.6%) involved patients with CRKP infections and 10 (9.4%) patients with CSKP infections. Among the 169 participants who were discharged against medical advice (DAMA), 134 (79.2%) of them were from the CRKP group, and 35 (21%) belonged to the CSKP group. A total of 510 participants recovered, with 305 (60%) coming from the CRKP group and 205 (40%) from the CSKP group. Univariate analysis revealed that all of the outcome factors, including recovered (P = 0.001), DAMA (P = 0.003), and mortality (P = 0.001), were significantly associated with severe outcomes in CRKP infection.
When the factors were exposed to multivariate analysis; diabetes (P = 0.001), hypertension (P = 0.001), immunosuppressive therapy (P = 0.001), cardiovascular disease (P = 0.004), prior hospitalization (P= 0.001), prior history of surgery (P= 0.001), COPD (P = 0.001) and parenteral nutrition (P = 0.001) were all significant risk factors affecting the development of CRKP infections. The findings of the multivariate logistic regression study of how risk factors affect participants with K. pneumoniae infection are shown in Table 4.
 |
Table 4 Multivariate Analysis of Factors Influencing the Acquisition of Carbapenem Resistance in K. pneumoniae Isolates |
Antimicrobial Susceptibility of K. pnemumoniae Isolates
There were 786 K. pneumoniae isolates, 536 (68%) of which were carbapenem-resistant strains and 250 (32%) of which were carbapenem-sensitive strains. 77.4% (415/536) of the 536 CRKP isolates were multidrug resistant, meaning they were resistant to more than three classes of antibiotics, compared to 7.2% (18/250) of the CSKP isolates. Figures 3 and 4 depict the phenotypic antimicrobial resistance pattern of isolated carbapenem resistant and carbapenem sensitive K. pneumoniae isolates. Ampicillin (100%) had the most significant level of resistance among the 536 CRKP isolates examined, followed by cefepime (93%), cefotaxime (93%), ceftazidime (93%), amoxicillin-clavulanic acid (90.70%), cotrimoxazole (90%), Aztreonam (88%), and chloramphenicol (88%). Both the CRKP and CSKP isolates showed good sensitivity to colistin and tigecycline. In the CSKP group, all antibiotics studied showed greater susceptibilities except for ampicillin (Figure 4). 87.3% of the CRKP isolates were positive for ESBL.
Determination of Meropenem MIC
The MIC of meropenem showed a varied range. Most of the K. pneumoniae isolates showed a MIC of 8μg/mL (48.5%, 260/536). 27.5% (145/536) of isolates had MIC at 4 μg/mL. Eighteen isolates (3.3%) showed maximum MICs of 128μg/mL. The remaining isolates (20.7%, 113/536) showed 16 to 64 μg/mL MIC levels (Table 5).
 |
Table 5 Determination of Meropenem MIC by Broth Micro-Dilution Method |
In order to determine whether the distribution of MICs varied among carbapenemase types, the MIC profiles for the CRKP isolates were further examined. The data showed that 74.5% (104/140) of blaNDM-1-producing isolates and 84.5% (148/175) of blaOXA-48-producing isolates had a meropenem MIC of 8 µg/mL. In isolates producing harboring genes (blaOXA48-and blaNDM-1), 58% of the isolates (67/115) showed a meropenem MIC of 16 µg/mL. None of the carbapenemase-positive isolates collected had meropenem MICs lower than 4 μg/mL.
Resistance Mechanism of Carbapenem
Of the CRKP examined, the carbaNP test was positive in 81.7% (n = 438/536) of the cases. Four hundred and thirty (80.22%) of the 536 isolates of the CRKPs had carbapenemase genes, according to real-time PCR. The mean Ct value of the blaNDM-1 results was 17, and the range was from 13 to 25. The mean Ct value of the blaoxa-48 results was 15.2, ranging from 11 to 21. Table 6 lists the findings of Multiplex PCR for the carbapenemase genes. The distribution of the genes was as follows: blaNDM-1 alone accounted for 32% (175/536), while blaOXA-48 alone accounted for 26.11% (140/536). Among the carbapenemases, the coexistence of blaNDM-1 and blaOXA-48 like was found in 21% (115/536) of the carbapenemases. blaKPC, blaVIM and blaIMP were noticeably absent. The findings of the real-time PCR amplification for the carbapenemase genes are shown in Figure 5.
 |
Table 6 Multiplex Quantitative Real-Time PCR Assay for the CRKP Isolates Carrying Carbapenemase Genes |
In our investigation, the most common genes in sputum isolates were blaOXA-48 (47.4%), followed by blaNDM-1 (36.4%), and blaOXA-48 with blaNDM-1 (16%). Fifty percent of the genes in the pus sample were blaNDM-1. The coexistence of blaOXA-48 and blaNDM-1 was predominant (48%) in urine samples. The most often found gene in the blood sample was blaNDM-1 (71%). Table 7 lists the distribution of carbapenemase genes amongst isolates of K. pneumoniae from various clinical origins.
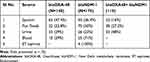 |
Table 7 Distribution of Carbapenemases Genes Among Isolates of K. pneumoniae from Various Sources |
Discussion
Antimicrobial resistance (AMR) is on the rise, notably among gram-negative bacteria such as Klebsiella spp. Numerous studies have revealed an increase in the incidence of antibiotic resistance among Klebsiella species. It is problematic since it causes several different acute infections. This widespread resistance could be attributed to the injudicious use of higher antibiotics without sufficient sensitivity guidelines. Furthermore, India’s increased population density may have contributed to isolating more multidrug resistant K pneumoniae species.24 Carbapenems are currently the drug of choice for treating severe hospital acquired infections. Recent research has revealed extremely high levels of carbapenem resistance in India and the Indian subcontinent, necessitating the adoption of alternative therapies.25 It would be interesting to identify the microorganisms that produce carbapenemase accurately, and this would require phenotypic and genotypic research to identify every gene responsible for making carbapenemase.
This research was conducted in a tertiary care facility in Karnataka, India. During the study period, 786 consecutive, non-repeat, distinct K. pneumoniae isolates were recovered from various clinical samples collected in our laboratory, with pus showing the highest recovery, followed by respiratory specimens, urine, and blood. Previous research from India has revealed that urine samples isolate the most K. pneumoniae, followed by sputum or exudative specimens.26,27 Furthermore, the majority of CRKP samples isolated in this investigation were from ICU patients (29.8%, 160/536), followed by the Surgery ward (26%, 139/536) and SICU (12%, 64/536) patients. Similarly, several investigations28,29 found that CRKP isolates were substantially linked with ICU admitted patients. In the current study, the prevalence of CRKP was 68%, whereas it was 77% in a study carried out in a tertiary care hospital in Haryana, India.30 Pawar et al discovered a prevalence of CRKP of roughly 31.77%,31 while Kumari et al discovered it to be 16.8% in a study in Bihar.25
Several risk factors for CRKP have been reported in previously released reviews, which include severe serious illnesses, the use of broad-spectrum antibiotics, the use of carbapenem antibiotics, a lengthy hospital stay, malignancies, hematopoietic stem cell transplantation, tracheotomies, mechanical ventilation, and indwelling catheters.32,33 In our study, the results of the univariate analysis demonstrated that smoking, diabetes, hypertension, COPD, tuberculosis infections, chronic kidney disease, cardiovascular disease, indwelling catheters, prior exposure to broad-spectrum antibiotics, prior hospitalizations, prior history of surgery and use of immunosuppressant’s were all possible causes for CRKP infections. These findings are consistent with those of earlier research conducted in other regions of the world.34,35
Regarding ICU admission status and treatment procedures performed, we found that the SOFA score (>12 points) was higher in the CRKP group. The findings indicate that the severity of the disease is the primary cause of mortality, which is explained by the extremely high baseline median SOFA Score. In-hospital mortality was greater in CRKP patients in univariate analysis (OR, 5.303; 95% CI, 2.714–10.36; P = 0.001); however, in multivariate analysis, it was not statistically significant.
According to multivariate regression analysis, diabetes, hypertension, COPD, cardiovascular disease, immunosuppressive treatment, past hospitalization, prior surgical history, and parenteral nutrition were found to be significantly associated with CRKP infection. According to this, having a severe coexisting co-morbid condition such as diabetes, hypertension, CKD, and cardiovascular disorders was a significant risk factor for CRKP infections. Therefore, patients with more comorbidities, greater severity, and worse immunity were more likely to develop multi-drug resistance from sensitive K. pneumoniae. To accurately assess the true impact of antibiotic resistance, it is crucial to account for potential confounding factors such as underlying co-morbidities.
According to our study, chronic obstructive pulmonary disease (COPD) is a risk factor for CRKP infection, which is in agreement with earlier findings.36,37 Patients with MDR-K. pneumoniae exhibited a greater prevalence of chronic pulmonary illness, which could explain why K. pneumoniae was the primary pathogen in patients with gram-negative bacillus pneumonia acquired in the hospital or the community.
Additionally, more patients in the CRKP group were found with septic shock and parenteral nutrition.
According to our research, the CRKP group had more patients who were receiving immunosuppressive medication than the CSKP group. Thus, individuals who are prone to infectious infections may have the option of using immunity enhancing treatments such intravenous immunoglobulin or thymosin application.
The prevalence of MDR K. pneumoniae clinical isolates has been continuously increasing over the world.38 The current study found that K. pneumoniae is resistant to most commonly used antibiotics. In our study, K. pneumoniae showed notable antibiotic resistance, the same as in the Wang et al findings.16 The CRKP strains in this investigation were extremely resistant to most antibiotics, which may be related to the duration and type of drug exposure, as well as the prevalence of antibiotic-resistance genes.36 Surprisingly, the rate of antibiotic resistance in K. pneumoniae to the tested antibiotics observed in this investigation was higher than that found in the surveillance study conducted in India.37 Similar to other studies; it was discovered that K. pneumoniae isolates in our study were entirely resistant to ampicillin.16,38 Furthermore, tigecycline and colistin have good in vitro activity against our CRKP isolates, nevertheless, resistance concerns occur during therapy, posing a substantial risk to public health,38 and colistin resistance is primarily connected with genetic mutations in lipid A modification.39
Four hundred and thirty-eight of the 536 isolates (81.7%) displayed phenotypic positive by Carba NP test, which was similar to what Vamsi et al observed.22 According to the results of the genotypic detection for the carbapenemases, 32% of the isolates were found to carry the blaNDM-1 gene, and 26.11% of the isolates carried the bla OXA-48 gene. In our collection, we found the genes for blaNDM-1 and blaOXA-48, although other carbapenemase producing genes, such as blaKPC, blaIMP and bla VIM were not discovered in any of the K. pneumoniae isolates examined. This is consistent with the findings of Jaggi et al, who discovered that the NDM gene, alone or in combination with OXA-48, was present in 35.9% of CRKP isolates, while VIM and KPC were absent in all of their isolates.40 18.3% (98/536) of the carbapenem-resistant isolates examined in our study tested negative for all the examined genes. This can be explained by the fact that these strains exert their resistance through different mechanisms, such as those involving the presence or lack of porins or efflux pumps or a gene not examined in this work.
According to our investigation, blaNDM-1 and blaOXA-48 coexisted at a rate of 21% within the same isolate, which was equivalent to the 20.0% coexistence rate reported by Garg et al.39 Because carbapenem-resistant genes can co-exist with beta-lactamases and other resistant genes on plasmids, treating infections caused by carbapenem-resistant strains becomes more difficult.41 Additionally, coexistence with carbapenem results in the retention of genes that make organisms resistant to other antimicrobials, which poses a threat to the economy, patient recovery, and antibiotic chemotherapy globally.42
Study Limitation
Because the study was conducted in a single tertiary care center, our findings may not be generalizable to other settings, and only resistance to carbapenems via carbapenemase production was investigated. It has yet to be determined how other co-existing mechanisms, such as porin loss or efflux pumps, contribute to carbapenem resistance. The clonality of the isolates and the gene sequence were not examined in the study, which would have improved the evaluation of the spread of a carbapenemase or some clones to comprehend CRKP isolates in the clinical environment. Despite these drawbacks, the study has delivered information on the occurrence of common carbapenemase genes and the relevance of the issue.
Conclusion
In conclusion, this study demonstrated that the detection rate of CRKP in our hospital was greater than that of CSKP. The drug resistance condition must be highly valued because the CRKP in our investigation exhibits a multi-drug resistant phenotype and is resistant to several common antibiotics. The development of many resistance genes is linked to CRKP resistance. The primary carbapenemase genes recovered from clinical CRKP in our hospital were blaNDM-1 and blaOXA-48. The risk factors for contracting the CRKP infection were examined in our study. As a result, understanding the risks of acquisition and attempting to avoid them, if feasible, would aid in mitigating the spread of these organisms and reducing the burden of related infections on the health system and human lives. We identified eight independent factors associated with CRKP, including diabetes, hypertension, COPD, cardiovascular disease, a history of hospitalization, a prior history of surgery, parenteral nutrition, and recent exposure to immunosuppressant’s within 3 months of acquisition.
Strict and effective nosocomial infection management and control strategies should be developed, epidemiological investigations should be conducted on time, and antibiotic resistance monitoring should be strengthened. It is critical to prevent the spread and incidence of CRKP in hospitals.
Abbreviations
MDR, Multi-drug resistant; CRKP, Carbapenem resistant Klebsiella pneumoniae; CSKP, Carbapenem sensitive Klebsiella pneumoniae; ATCC, American Type Culture Collection; CLSI, Clinical Laboratory Standard Institute; MIC, minimum inhibitory concentration; NDM, New Delhi metallo β-lactamases; KPC, Klebsiella pneumoniae carbapenemases; IMP, Active on imipenem metalloβ-lactamases; VIM, Verona integron-encoded metallo β-lactamases; OXA-48, Oxacillinase-48-like carbapenemases.
Acknowledgments
The authors thank the Department of Geriatrics, Department of Microbiology, Yenepoya research center (YRC), and the Head of the Institution for providing the financial assistance, materials, and infrastructure to conduct the study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lin D, Chen J, Yang Y, Cheng J, Sun C. Epidemiological study of carbapenem-resistant Klebsiella pneumoniae. Open Med. 2018;13(1):460–466. doi:10.1515/med-2018-0070
2. Ferreira CM, Ferreira WA, Silva LM, Barbosa TC, Souza VC, Naveca FG. Molecular epidemiology of KPC-2 producing Klebsiella pneumoniae. SOJ Microbiol Infect Dis. 2018;5:1–3.
3. Amann S, Neef K, Kohl S. Antimicrobial resistance (AMR). Eur J Hosp Pharm. 2019;26(3):175–177. doi:10.1136/ejhpharm-2018-001820
4. Rello J, Kalwaje Eshwara V, Lagunes L, et al. A global priority list of the TOp TEn resistant Microorganisms (TOTEM) study at intensive care: a prioritization exercise based on multi-criteria decision analysis. Eur J Clin Microbiol Infect Dis. 2019;38(2):319–323. PMID: 30426331. doi:10.1007/s10096-018-3428-y
5. Eatemadi A, Al Risi E, Kasliwal AK, Al Zaabi A, Moradzadegan H, Aslani Z. A proposed evidence-based local guideline for definition of multidrug-resistant (MDR), extensively drug-resistant (XDR) and pan drug-resistant (PDR) bacteria by the Microbiology Laboratory. Int J Curr Sci Res Rev. 2021;4(3):146–153. doi:10.47191/ijcsrr/V4-i3-01
6. Kobayashi SD, Porter AR, Freedman B, et al. Antibody-mediated killing of carbapenem-resistant ST258 Klebsiella pneumoniae by human neutrophils. mBio. 2018;9(2):e00297–18. doi:10.1128/mBio.00297-18
7. Ragheb SM, Tawfick MM, El-Kholy AA, Abdulall AK. Phenotypic and genotypic features of Klebsiella pneumoniae harboring carbapenemases in Egypt: OXA-48-like carbapenemases as an investigated model. Antibiotics. 2020;9(12):852. doi:10.3390/antibiotics9120852
8. Hammoudi Halat D, Ayoub Moubareck C. The current burden of carbapenemases: review of significant properties and dissemination among gram-negative bacteria. Antibiotics. 2020;9(4):186. doi:10.3390/antibiotics9040186
9. Eichenberger EM, Thaden JT. Epidemiology and mechanisms of resistance of extensively drug resistant gram-negative bacteria. Antibiotics. 2019;8(2):37. doi:10.3390/antibiotics8020037
10. Hu Y, Liu C, Shen Z, et al. Prevalence, risk factors and molecular epidemiology of carbapenem-resistant Klebsiella pneumoniae in patients from Zhejiang, China, 2008–2018. Emerg Microbes Infect. 2020;9(1):1771–1779. doi:10.1080/22221751.2020.1799721
11. Dai G, Xu Y, Kong H, Xie W, Wang H. Risk factors for carbapenem-resistant Klebsiella pneumoniae infection and associated clinical outcomes. Am J Transl Res. 2021;13(6):7276–7281. PMID: 34306493; PMCID: PMC8290679.
12. Tacconelli E, Carrara E, Savoldi A, et al.; WHO Pathogens Priority List Working Group. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis. 2018;18(3):318–327. PMID: 29276051. doi:10.1016/S1473-3099(17)30753-3
13. Cassini A, Högberg LD, Plachouras D, et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: a population-level modelling analysis. Lancet Infect Dis. 2019;19(1):56–66. doi:10.1016/S1473-3099(18)30605-4
14. Han JH, Goldstein EJC, Wise J, Bilker WB, Tolomeo P, Lautenbach E. Epidemiology of carbapenem-resistant Klebsiella pneumoniae in a network of long-term acute care hospitals. Clin Infect Dis. 2017;64(7):839–844. PMID: 28013258; PMCID: PMC5399931. doi:10.1093/cid/ciw856
15. Zhou M, Wang Y, Liu C, et al. Comparison of five commonly used automated susceptibility testing methods for accuracy in the China Antimicrobial Resistance Surveillance System (CARSS) hospitals. Infect Drug Resist. 2018;11:1347–1358. doi:10.2147/IDR.S166790
16. Wang N, Zhan M, Liu J, et al. Prevalence of carbapenem-resistant Klebsiella pneumoniae infection in a Northern Province in China: clinical characteristics, drug resistance, and geographic distribution. Infect Drug Resist. 2022;15:569–579. doi:10.2147/IDR.S347343
17. Lee CR, Lee JH, Park KS, Kim YB, Jeong BC, Lee SH. Global dissemination of carbapenemase-producing Klebsiella pneumoniae: epidemiology, genetic context, treatment options, and detection methods. Front Microbiol. 2016;7. doi:10.3389/fmicb.2016.00895
18. Connie R, Donald C. Textbook of Diagnostic Microbiology.
19. Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing: 29th Informational Supplement (M100-S26). Wayne, PA: CLSI; 2019.
20. Magiorakos AP, Srinivasan A, Carey RB, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–281. PMID: 21793988. doi:10.1111/j.1469-0691.2011.03570.x
21. Ravikant Kumari P, Kumar M, Roy P, Jeya M, Jeya M. Detection of carbapenem-resistant Enterobacteriaceae by real-time PCR and assessment of hospitalization related risk factors associated with their fecal carriage: a case-control study. J Pure Appl Microbiol. 2022;16(2):1111–1121. doi:10.22207/JPAM.16.2.37
22. Yoshioka N, Hagiya H, Deguchi M, et al. Multiplex real-time PCR assay for six major carbapenemase genes. Pathogens. 2021;10(3):276. doi:10.3390/pathogens10030276
23. Vamsi SK, Moorthy RS, Hemiliamma MN, Chandra Reddy RB, Chanderakant DJ, Sirikonda S. Phenotypic and genotypic detection of carbapenemase production among gram negative bacteria isolated from hospital acquired infections. Saudi Med J. 2022;43(3):236–243. doi:10.15537/smj.2022.43.3.20210809
24. Taneja N, Sharma M. Antimicrobial resistance in the environment: the Indian scenario. Indian J Med Res. 2019;149(2):119. doi:10.4103/ijmr.IJMR_331_18
25. Kumari N, Kumar M, Katiyar A, et al. Genome-wide identification of carbapenem-resistant Gram-negative bacterial (CR-GNB) isolates retrieved from hospitalized patients in Bihar, India. Sci Rep. 2022;12(1):8477. PMID: 35590022; PMCID: PMC9120164. doi:10.1038/s41598-022-12471-3
26. Remya P, Shanthi M, Sekar U. Occurrence and characterization of hyperviscous K1 and K2 serotype in Klebsiella pneumoniae. J Lab Physicians. 2018;10(03):283–288. doi:10.4103/JLP.JLP_48_18
27. Indrajith S, Mukhopadhyay AK, Chowdhury G, et al. Molecular insights of Carbapenem resistance Klebsiella pneumoniae isolates with focus on multidrug resistance from clinical samples. J Infect Public Health. 2021;14(1):131–138. doi:10.1016/j.jiph.2020.09.018
28. Al-Zahrani IA, Alasiri BA. The emergence of carbapenem-resistant Klebsiella pneumoniae isolates producing OXA-48 and NDM in the Southern (Asir) province, Saudi Arabia. Saudi Med J. 2018;39(1):23–30. doi:10.15537/smj.2018.1.21094
29. Alhazmi W, Al-Jabri A, Al-Zahrani I. The molecular characterization of nosocomial carbapenem-resistant Klebsiella pneumoniae Co-Harboring blaNDM and blaOXA-48 in Jeddah. Microbiol Res. 2022;13(4):753–764. doi:10.3390/microbiolres13040054
30. Gupta P, Bollam N, Mehta Y, Sengupta S, Gandra S. Risk factors associated with carbapenem-resistant Klebsiella pneumoniae bloodstream infections in a tertiary-care hospital in India. Infect Control Hosp Epidemiol. 2021;42(11):1418–1420. doi:10.1017/ice.2020.1280
31. Pawar S, Mohite S, Shinde R, Patil S, Karande G. Carbapenem resistant Enterobacteriaceae: prevalence and bacteriological profile in tertiary teaching hospital from rural western India. Indian J Microbiol Res. 2018;5(3):342–347.
32. Katchanov J, Asar L, Klupp EM, et al. Carbapenem-resistant Gram-negative pathogens in a German university medical center: prevalence, clinical implications and the role of novel β-lactam/β lactamase inhibitor combinations. PLoS One. 2018;13(4):e0195757. doi:10.1371/journal.pone.0195757
33. Zhao D, Zuo Y, Wang Z, Li J. Characterize carbapenem-resistant Klebsiella pneumoniae isolates for nosocomial pneumonia and their Gram-negative bacteria neighbors in the respiratory tract. Mol Biol Rep. 2019;46(1):609–616. doi:10.1007/s11033-018-4515-y
34. Zhang S, Yang Z, Sun L, et al. Clinical observation and prognostic analysis of patients with Klebsiella pneumoniae bloodstream infection. Front Cell Infect Microbiol. 2020;10:577244. PMID: 33240822; PMCID: PMC7680902. doi:10.3389/fcimb.2020.577244
35. Moghnieh R, Abdallah D, Jadayel M, et al. Epidemiology, risk factors, and prediction score of carbapenem resistance among inpatients colonized or infected with 3rd generation cephalosporin resistant Enterobacterales. Sci Rep. 2021;11(1):14757. PMID: 34285312; PMCID: PMC8292374. doi:10.1038/s41598-021-94295-1
36. Xu T, Feng W, Sun F, Qian Y. Clinical and resistance characterization of carbapenem-resistant Klebsiella pneumoniae isolated from intensive care units in China. Ann Transl Med. 2022;10(20):1109. doi:10.21037/atm-22-4323
37. Walia K, Madhumathi J, Veeraraghavan B, et al. Establishing antimicrobial resistance surveillance & Research network in India: journey so far. Indian J Med Res. 2019;149(2):164. doi:10.4103/ijmr.IJMR_226_18
38. Sharma A, Thakur A, Thakur N, et al. Changing trend in the antibiotic resistance pattern of Klebsiella pneumonia isolated from endotracheal aspirate samples of ICU patients of a tertiary care hospital in North India. Cureus. 2023;15(3). doi:10.7759/cureus.36317
39. Garg A, Garg J, Upadhyay GC, Agarwal A, Bhattacharjee A. Evaluation of the Rapidec Carba NP test kit for detection of carbapenemase-producing gram-negative bacteria. Antimicrob Agents Chemother. 2015;59(12):7870–7872. doi:10.1128/AAC.01783-15
40. Jaggi N, Chatterjee N, Singh V, et al. Carbapenem resistance in Escherichia coli and Klebsiella pneumoniae among Indian and international patients in North India. Acta Microbiol Immunol Hung. 2019;66(3):367–376. doi:10.1556/030.66.2019.02
41. Nordmann P, Poirel L. Epidemiology and diagnostics of carbapenem resistance in gram-negative bacteria. Clin Infect Dis. 2019;69(Supplement_7):S521–S528. doi:10.1093/cid/ciz824
42. Karampatakis T, Tsergouli K, Politi L, et al. Molecular epidemiology of endemic carbapenem-resistant gram-negative bacteria in an intensive care unit. Microb Drug Resist. 2019;25(5):712–716. PMID: 30589601. doi:10.1089/mdr.2018.0266
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.