Back to Journals » Vascular Health and Risk Management » Volume 18
Chronic Fatigue Associated with Post-COVID Syndrome versus Transient Fatigue Caused by High-Intensity Exercise: Are They Comparable in Terms of Vascular Effects?
Authors Chudzik M, Cender A, Mordaka R, Zielinski J , Katarzynska J , Marcinek A , Gebicki J
Received 20 April 2022
Accepted for publication 27 August 2022
Published 6 September 2022 Volume 2022:18 Pages 711—719
DOI https://doi.org/10.2147/VHRM.S371468
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Mirna N Chahine
Michal Chudzik,1,2 Anna Cender,1 Robert Mordaka,1 Jacek Zielinski,3 Joanna Katarzynska,4 Andrzej Marcinek,4,5 Jerzy Gebicki4,5
1Medical Center, Saint Family Hospital, Lodz, Poland; 2Department of Internal Medicine and Geronto-Cardiology, Medical Centre for Postgraduate Education, Warsaw, Poland; 3Department of Athletics, Strength and Conditioning, Poznan University of Physical Education, Poznan, Poland; 4Angionica Ltd., Lodz, Poland; 5Institute of Applied Radiation Chemistry, Lodz University of Technology, Lodz, Poland
Correspondence: Jerzy Gebicki, Institute of Applied Radiation Chemistry, Lodz University of Technology, Lodz, 90-924, Poland, Tel +48 42 631 31 71, Email [email protected]; [email protected] Michal Chudzik, Department of Internal Medicine and Geronto-Cardiology, Medical Centre for Postgraduate Education, Warsaw, Poland, Tel +48 691 941 814, Email [email protected]
Purpose: The pathophysiology of chronic fatigue associated with post-COVID syndrome is not well recognized. It is assumed that this condition is partly due to vascular dysfunction developed during an acute phase of infection. There is great demand for a diagnostic tool that is able to clinically assess post-COVID syndrome and monitor the rehabilitation process.
Patients and Methods: The Flow Mediated Skin Fluorescence (FMSF) technique appears uniquely suitable for the analysis of basal microcirculatory oscillations and reactive hyperemia induced by transient ischemia. The FMSF was used to measure vascular circulation in 45 patients with post-COVID syndrome. The results were compared with those for a group of 26 amateur runners before and after high-intensity exercise as well as for a control group of 32 healthy age-matched individuals.
Results: Based on the observed changes in the NOI (Normoxia Oscillatory Index) and RHR (Reactive Hyperemia Response) parameters measured with the FMSF technique, it was found that chronic fatigue associated with post-COVID syndrome is comparable with transient fatigue caused by high-intensity exercise in terms of vascular effects, which are associated with vascular stress in the macrocirculation and microcirculation. Acute and chronic fatigue symptomatology shared similarly altered changes in the NOI and RHR parameters and both can be linked to calcium homeostasis modification.
Conclusion: The NOI and RHR parameters measured with the FMSF technique can be used for non-invasive clinical assessment of post-COVID syndrome as well as for monitoring the rehabilitation process.
Keywords: COVID-19, post-COVID syndrome, chronic fatigue, vascular circulation, FMSF technique
Introduction
Severe acute respiratory coronavirus 2 (SARS-CoV-2) is responsible for the COVID-19 pandemic, which has resulted in a global healthcare crisis. The health consequences of COVID-19 infection are broad, and not restricted to the respiratory tract. It is now generally accepted that COVID-19 infection causes serious injuries to blood vessels by damaging the vascular endothelium.1–3 Numerous studies have reported that patients recovering from SARS-CoV-2 infection complain of persistent symptoms, including fatigue, brain fog, diffuse myalgia, and weakness, which may lead to chronic fatigue known as post-COVID or long-COVID.4,5 The cardiopulmonary exercise testing (CPET) studies in post-COVID patients are suggestive of deconditioning with a tendency to hyperventilation.6
The list of post-COVID symptoms is long, but fatigue is the most common, occurring in more than 70% of post-COVID patients. There is a broad overlap in symptomatology of post-COVID syndrome with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and it is assumed that both these pathologies can be linked to calcium homeostasis dysfunction.7–9 It is likely that calcium homeostasis dysfunction may also affect regulation of adrenergic and muscarinic receptors with implications in post-COVID and chronic fatigue syndromes.10 There is limited mechanistic knowledge explaining the pathophysiology of chronic fatigue associated with post-COVID. It can be hypothesized that post-COVID syndrome is primarily connected with permanent vascular dysfunction caused by initial vascular injuries occurring during the acute phase of COVID-19 infection. Therefore, it seems rational to compare the vascular effects of chronic fatigue associated with post-COVID with the vascular effects of transient fatigue caused by high-intensity exercise. High-intensity exercise is known to impose transient stress on the vascular endothelium, as measured by flow-mediated dilatation (FMD).11,12 This effect is particularly pronounced in individuals who are not highly physically fit. It is assumed that high-intensity exercise is accompanied by a corresponding increase in reactive oxygen species (ROS), which has the potential to decrease nitric oxide (NO) bioavailability. This effect is often called the “exercise paradox”. In this sense, exercise can be considered as a stressor inducing anti-stress responses, which can be positive for physical fitness. It is also known that strenuous physical exercise modifies transiently calcium homeostasis and this effect persists until the late recovery phase.13,14
To test our hypothesis that the chronic fatigue associated with post-COVID is associated with permanent vascular dysfunction caused by initial vascular injuries, we decided to compare the vascular effects associated with post-COVID with those generated by high-intensity exercise. For this purpose, we applied the Flow Mediated Skin Fluorescence (FMSF) technique. The FMSF technique can be used for non-invasive assessment of vascular circulation and metabolic regulation.15–21 Recently a new approach to non-invasive assessment of vascular circulation using the FMSF technique has been presented.22 This simple two-parametric approach involving the RHR and log (HS) parameters can be used for characterization of vascular circulation based on distinguishable macro- and microcirculatory responses to hypoxia. A direct comparison of the vascular effects underlying post-COVID fatigue with exercise-induced fatigue using the FMSF technique could enable the identification of diagnostic parameters for clinical assessment of post-COVID syndrome and monitoring the rehabilitation process.
Materials and Methods
Ethics Statement
The study was conducted at the Medical Center, Saint Family Hospital, in Lodz (Poland), the Medical University of Lodz (Poland), and Poznan University of Physical Education (Poland). It conformed to the principles outlined in the Declaration of Helsinki and the study protocol was approved by the Bioethics Committee of Lodz Regional Medical Chamber (approval under STOP-COVID Registry), the Bioethics Committee at the Medical University of Lodz (approval no. RNN/325/17/KE and KE/09/18) and the Ethics Committee of the Poznan University of Medical Sciences (approval no. 1017/16). All the subjects were Polish nationality/Caucasian type and gave written informed consent prior to participation.
Study Population and Clinical Characteristics
The studied population consisted of three groups: post-COVID, control, and amateur runners. The results for the post-COVID group were compared with those for the control group of age-matched healthy individuals without a history of COVID-19 infection. The vascular effects associated with transient fatigue caused by high-intensity exercise were measured in the group of amateur runners before and after exercise.
A summary of the characteristics of each group is presented below:
- Post-COVID group
45 patients (26 female and 19 male), age range 30–50 years, after COVID-19 infection.
The patients all declared having no health related problems prior to infection. The patients expressed subjective feelings of limited tolerance to exercise and above 50% greater fatigue compared to their pre-COVID-19 levels. These symptoms must have continued for at least four weeks following the last symptoms of infection. A list of the multiple symptoms associated with post-COVID syndrome with their frequencies in the group is presented in Table 1.
- Control group
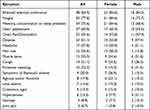 |
Table 1 Frequencies of Symptoms in Individuals with Post-COVID Syndrome Expressed as Numbers and Percentages (n (%)) |
32 healthy individuals (13 female and 19 male), aged 30–50 years, without COVID-19 infection history.
- Amateur runners group
26 highly trained amateur runners (all men), aged 21–40 years, participants of various sports competitions (long-distance running, cross-country, marathons).
All athletes had valid health certificates issued by a physician specializing in sports medicine, which provided eligibility for training and competition. Exclusion criteria were illness symptoms, injuries, and taking of drugs (temporarily or chronically).
The cardiopulmonary exercise test (CPET) was performed on an H/P Cosmos treadmill (H/P Cosmos Sports & Medical GmbH, Germany). The exercise protocol started with a 4-min warm-up at a treadmill speed of 6 km/h. Then, the treadmill speed was increased by 2 km/h every 3 min. The treadmill incline was 1% throughout the whole test. The test terminated if the athlete signaled his subjective exhaustion by raising one hand.
The clinical characteristics of the participants are displayed in Table 2.
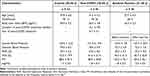 |
Table 2 Characteristics of the Studied Population |
Brief Description of the FMSF Technique and the Measurement Protocol
Measurements were performed using AngioExpert, a device constructed by Angionica Ltd. The AngioExpert device uses the Flow Mediated Skin Fluorescence (FMSF) technique, which measures changes in the intensity of nicotinamide adenine dinucleotide (NADH) fluorescence from the skin on the forearm as a response to blocking and releasing blood flow. The skin is the largest organ of the human body, and is characterized by a specific metabolism. The epidermal layer of skin is not directly vascularized, and oxygen and nutrients are transported from the dermis by diffusion. Therefore, epidermal cell metabolism can be considered a unique and sensitive marker of early dysfunction in vascular circulation and metabolic regulation.
The measurement protocol in the present study was the same as applied previously.20 For analysis of the results obtained in the present study, two new parameters were introduced: Reactive Hyperemia Response (RHR) and Normoxia Oscillatory Index (NOI). These parameters are defined in Figure 1B.
The RHR parameter characterizes endothelial function related predominantly to the production of nitric oxide (NO) in the vasculature due to reactive hyperemia.22 RHR is a unique parameter, based on a combination of both the ischemic and hyperemic parts of the measured FMSF trace, as shown in Figure 1A. The NOI parameter characterizes the microcirculatory oscillations detected at the baseline and represents the contribution of endothelial (<0.021 Hz) and neurogenic (0.021–0.052 Hz) oscillations relative to all oscillations detected at low frequency interval (<0.15 Hz). This parameter is particularly sensitive to high-intensity exercise. Figure 1C and D shows the changes of the fluorescence signal in the normalized baseline before high-intensity exercise, and the corresponding Power Spectral Density in the low frequency interval (<0.15 Hz). Figure 1E and F shows similar changes observed after exercise. An evident decrease in the intensity of endothelial and neurogenic oscillations due to strenuous exercise is the best represented by the NOI parameter as it is not sensitive to individual variability of low frequency microcirculatory oscillations, which are also age-dependent.16 The NOI parameter was normalized after 1–3 hours of rest and returns to the values observed before exercise. This observation is in accordance with other studies.11,12
We observed that both the RHR and NOI parameters should be used jointly for effective diagnostics of post-COVID fatigue and exercise-related fatigue. Based on our experience of using the FMSF technique, the NOI parameter seems more universal as it is age-independent. It is sensitive not only to fatigue caused by intense physical activity, but also to fatigue caused by emotional stress due to peripheral vasoconstriction.
Statistical Analysis
The collected data were analyzed using the dedicated FM analytical software installed on the AngioExpert device. Statistical analyses were performed with OriginPro 2018b software. The Shapiro–Wilk test was used to assess the normality of the distribution. The Levene’s and Brown-Forsythe tests were used to confirm homogeneity of variance in the compared groups. An independent sample t-test or Mann–Whitney U-test was used to compare continuous variables in the control group and post-COVID group. The paired sample t-test and the paired-sample Wilcoxon signed rank test were used to compare the FMSF parameters recorded in the amateur runners group. A two-tailed p < 0.05 was considered statistically significant.
Study Limitation
A limited size of the studied groups does not allow to establish unequivocally an effect of sex on post-COVID syndrome. However, a difference has been observed in the NOI parameter of post-COVID patients (47.8 ± 20.5 for females vs 56.7 ± 22.1 for males) suggesting female sex as a risk factor associated with post-COVID syndrome. No such difference in the NOI parameter has been observed in the control group (72.8 ± 23.8 for females vs 73.6 ± 17.4 for males). The higher risk of females to post-COVID syndrome has already been recognized and may indicate viral-induced sex hormone dysfunction, which can result in early menopause, as observed for other viral diseases.23,24
Also a limited size of the studied groups does not allow to find any remarkable differences in the measured FMSF parameters due to a short-term (4 to 12 weeks after infection) vs a long-term (above 12 weeks after infection) duration of the post-Covid syndrome as documented previously in the studies involving a large cohort of patients.25
A study with more matched groups in terms of size, age and gender is needed.
Results and Discussion
Figure 2A and B presents a comparison of the NOI parameter in the post-COVID group and the control group. It is clear that post-COVID syndrome reverses the distribution of the NOI parameter, indicating that this parameter is very sensitive to the vascular problem monitored.
The effects of high-intensity exercise on the NOI parameter are very similar, as shown in Figure 2C and D. It appears that the fatigue associated with post-COVID syndrome and exercise-related fatigue exert very similar vascular effects, which can be observed as lower intensities representing endothelial and neurogenic microcirculatory oscillations at the baseline. An obvious difference is that the exercise-related effect is fully reversible after 1–3 hours of rest.
The vascular effects of post-COVID- and exercise-related fatigue measured by the RHR parameter are also quite similar, as shown in Figure 3A and B vs C and D.
It should be stressed that both the NOI parameter and the RHR parameter represent distinctive properties of the vascular system. The NOI parameter characterizes microcirculation based on the measurement of microcirculatory oscillations at the baseline. In contrast, the RHR parameter characterizes the vessels based on NO bioavailability, predominantly in large and medium size arteries, due to reactive hyperemia.
The conclusion of our study is that both the macro- and microcirculation are affected by vascular stress related to both post-COVID syndrome and high-intensity exercise. Perhaps, the long list of symptoms associated post-COVID syndrome summarized in Table 1 and reported in many other studies can be linked to endothelial dysfunction present in the blood vessels of both the macro- and microcirculation. It seems likely that the above observation linking pathophysiology of transient fatigue caused by strenuous exercise and chronic post-COVID fatigue can originate from calcium homeostasis modification that leads to endothelial dysfunction.7,8,13,14
In previous communications, we have suggested that the Hypoxia Sensitivity (HS) parameter can be used to predict severity of the acute phase of COVID-19 infection.26,27 However, the present study indicates that this parameter now shown as log(HS) has only minor utility for the diagnostics of post-COVID syndrome, as presented in Table 2. The explanation may be that hypoxemia plays an important role only in the acute phase of infection.
The results of this study show the utility of two key parameters (NOI and RHR) for clinical assessment and monitoring the rehabilitation process of post-COVID patients. They can also be used to identify potential treatments to improve exercise tolerance and fatigue in patients after COVID-19, as is being demonstrated by one of the co-authors.28
Conclusion
The following conclusions can be drawn from this study:
- The FMSF technique appears to be uniquely suitable for the analysis of basal microcirculatory oscillations and reactive hyperemia induced by transient ischemia.
- Chronic fatigue associated with post-COVID syndrome is comparable with transient fatigue caused by high-intensity exercise, in terms of vascular effects.
- The NOI and RHR parameters measured by the FMSF technique can be used for non-invasive clinical assessment of post-COVID syndrome, as well as for monitoring the rehabilitation process.
Funding
This work was supported by the European Union from the resources of the European Regional Development Fund under the Smart Growth Operational Program, Grant No. POIR. 01.01.01-00-0540/15-00.
Disclosure
JK is employed by Angionica Ltd. JG and AM are inventors of the patents protecting the use of FMSF technology EP2713860B1 issued to Angionica Ltd. The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be constructed as a potential conflict of interest.
References
1. Libby P, Lüscher T. COVID-19 is, in the end, an endothelial disease. Eur Heart J. 2020;41(32):3038–3044. doi:10.1093/eurheartj/ehaa623
2. Siddiqi HK, Libby P, Ridker PM. COVID-19 – a vascular disease. Trends Cardiovasc Med. 2021;31(1):1–5. doi:10.1016/j.tcm.2020.10.005
3. Østergaard L. SARS CoV-2 related microvascular damage and symptoms during and after COVID-19: consequences of capillary transit-time changes, tissue hypoxia and inflammation. Physiol Rep. 2021;9(3):e14726. doi:10.14814/phy2.14726
4. Nalbandian A, Sehgal K, Gupta A, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27(4):601–615. doi:10.1038/s41591-021-01283-z
5. Deer RR, Rock MA, Vasilevsky N, et al. Characterizing long COVID: deep phenotype of a complex condition. EBioMedicine. 2021;74:103722. doi:10.1016/j.ebiom.2021.103722
6. Naeije R, Caravita S. Phenotyping long COVID. Eur Respir J. 2021;58(2):2101763. doi:10.1183/13993003.01763-2021
7. Wirth KJ, Scheibenbogen C. Dyspnea in post-COVID syndrome following mild acute COVID-19 infections: potential causes and consequences for a therapeutic approach. Med. 2022;58(3):419. doi:10.3390/medicina58030419
8. Nguyen T, Johnston S, Clarke L, Smith P, Staines D, Marshall-Gradisnik S. Impaired calcium mobilization in natural killer cells from chronic fatigue syndrome/myalgic encephalomyelitis patients is associated with transient receptor potential melastatin 3 ion channels. Clin Exp Immunol. 2017;187(2):284–293. doi:10.1111/cei.12882
9. Perrin R, Riste L, Hann M, Walther A, Mukherjee A, Heald A. Into the looking glass: post-viral syndrome post COVID-19. Med Hypotheses. 2020;144:110055. doi:10.1016/j.mehy.2020.110055
10. Bornstein SR, Voit-Bak K, Donate T, et al. Chronic post-COVID-19 syndrome and chronic fatigue syndrome: is there a role for extracorporeal apheresis? Mol Psychiatry. 2022;27(1):34–37. doi:10.1038/s41380-021-01148-4
11. Dawson EA, Green DJ, Cable NT, Thijssen DHJ. Effects of acute exercise on flow-mediated dilatation in healthy humans. J Appl Physiol. 2013;115(11):1589–1598. doi:10.1152/japplphysiol.00450.2013
12. McClean C, Harris RA, Brown M, Brown JC, Davison GW. Effects of exercise intensity on postexercise endothelial function and oxidative stress. Oxid Med Cell Longev. 2015;2015:723679. doi:10.1155/2015/723679
13. Henderson SA, Graham HK, Mollan RAB, Riddoch C, Sheridan B, Johnston H. Calcium homeostasis and exercise. Int Orthop. 1989;13(1):69–73. doi:10.1007/BF00266727
14. Maïmoun L, Sultan C. Effect of physical activity on calcium homeostasis and calciotropic hormones: a review. Calcif Tissue Int. 2009;85(4):277–286. doi:10.1007/s00223-009-9277-z
15. Katarzynska J, Lipinski Z, Cholewinski T, et al. Non-invasive evaluation of microcirculation and metabolic regulation using flow mediated skin fluorescence (FMSF): technical aspects and methodology. Rev Sci Instrum. 2019;90(10):104104. doi:10.1063/1.5092218
16. Gebicki J, Katarzynska J, Cholewinski T, Sieron L, Marcinek A. Flowmotion Monitored by Flow Mediated Skin Fluorescence (FMSF): a tool for characterization of microcirculatory status. Front Physiol. 2020;11:702. doi:10.3389/FPHYS.2020.00702
17. Gebicki J, Marcinek A, Zielinski J. Assessment of microcirculatory status based on stimulation of myogenic oscillations by transient ischemia: from health to disease. Vasc Health Risk Manag. 2021;17:33–36. doi:10.2147/VHRM.S292087
18. Katarzynska J, Borkowska A, Czajkowski P, et al. Flow mediated skin fluorescence technique reveals remarkable effect of age on microcirculation and metabolic regulation in type 1 diabetes. Microvasc Res. 2019;124:19–24. doi:10.1016/j.mvr.2019.02.005
19. Katarzynska J, Borkowska A, Los A, Marcinek A, Cypryk K, Gebicki J. Flow-Mediated Skin Fluorescence (FMSF) technique for studying vascular complications in type 2 diabetes. J Diabetes Sci Technol. 2020;14(3):693–694. doi:10.1177/1932296819895544
20. Los-Stegienta A, Katarzynska J, Borkowska A, Marcinek A, Cypryk K, Gebicki J. Differentiation of diabetic foot ulcers based on stimulation of myogenic oscillations by transient ischemia. Vasc Health Risk Manag. 2021;17:145–152. doi:10.2147/VHRM.S307366
21. Bugaj O, Zieliński J, Kusy K, Kantanista A, Wieliński D, Guzik P. The effect of exercise on the skin content of the reduced form of NAD and its response to transient ischemia and reperfusion in highly trained athletes. Front Physiol. 2019;10:600. doi:10.3389/fphys.2019.00600
22. Katarzynska J, Zielinski J, Marcinek A, Gebicki J. New approach to non-invasive assessment of vascular circulation based on the response to transient ischemia. Vasc Health Risk Manag. 2022;18:113–116. doi:10.2147/VHRM.S358983
23. Stewart S, Newson L, Briggs TA, Grammatopoulos D, Young L, Gill P. Long COVID risk - a signal to address sex hormones and women’s health. Lancet Reg Heal Eur. 2021;11:100242. doi:10.1016/j.lanepe.2021.100242
24. Fernández-de-Las-Peñas C, Martín-Guerrero JD, Pellicer-Valero ÓJ, et al. Female sex is a risk factor associated with long-term post-COVID related-symptoms but not with COVID-19 symptoms: the LONG-COVID-EXP-CM Multicenter Study. J Clin Med. 2022;11(2):413. doi:10.3390/jcm11020413
25. Groff D, Sun A, Ssentongo AE, et al. Short-term and long-term rates of postacute sequelae of SARS-CoV-2 infection: a systematic review. JAMA Netw Open. 2021;4(10):e2128568. doi:10.1001/jamanetworkopen.2021.28568
26. Gebicki J, Katarzynska J, Marcinek A. Can the microcirculatory response to hypoxia be a prognostic factor for Covid-19? Respir Physiol Neurobiol. 2020;280:103478. doi:10.1016/j.resp.2020.103478
27. Gebicki J, Katarzynska J, Marcinek A. Can efficient stimulation of myogenic microcirculatory oscillations by transient ischemia predict low incidence of COVID-19 infection? Respir Physiol Neurobiol. 2021;286:103618. doi:10.1016/j.resp.2021.103618
28. Chudzik M, Burzyńska M, Kapusta J. Use of 1-MNA to improve exercise tolerance and fatigue in patients after COVID-19. Nutrients. 2022;14:3004. doi:10.3390/nu14153004
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



