Back to Journals » International Journal of General Medicine » Volume 15
Chest Radiograph Severity Scores, Comorbidity Prevalence, and Outcomes of Patients with Coronavirus Disease Treated at the King Abdullah University Hospital in Jordan: A Retrospective Study
Authors Gharaibeh M, Elheis M , Khasawneh R , Al-Omari M, Jibril M, Dilki K, El-Obeid E, Altalhi M, Abualigah L
Received 2 February 2022
Accepted for publication 12 May 2022
Published 20 May 2022 Volume 2022:15 Pages 5103—5110
DOI https://doi.org/10.2147/IJGM.S360851
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Maha Gharaibeh,1 Mwaffaq Elheis,1 Ruba Khasawneh,1 Mamoon Al-Omari,1 Mohammad Jibril,1 Khalid Dilki,1 Eyhab El-Obeid,1 Maryam Altalhi,2 Laith Abualigah3
1Department of Diagnostic and Interventional Radiology, Faculty of Medicine, Jordan University of Science and Technology, Irbid, 2210, Jordan; 2Department of Management Information System, College of Business Administration, Taif University, Taif, 21944, Saudi Arabia; 3Faculty of Computer Sciences and Informatics, Amman Arab University, Amman, 11953, Jordan
Correspondence: Maha Gharaibeh; Laith Abualigah, Tel +96 2799716333, Email [email protected]; [email protected]
Introduction: Hospitalized patients with coronavirus disease (COVID-19) often undergo chest x-ray (CXR). Utilizing CXR findings could reduce the cost of COVID-19 treatment and the resultant pressure on the Jordanian healthcare system.
Methods: We evaluated the association between the CXR severity score, based on the Radiographic Assessment of Lung Edema (RALE) scoring system, and outcomes of patients with COVID-19. The main objective of this work is to assess the role of the RALE scoring system in predicting in-hospital mortality and clinical outcomes of patients with COVID-19. Adults with a positive severe acute respiratory syndrome COVID-19 two reverse-transcription polymerase chain reaction test results and a baseline CXR image, obtained in November 2020, were included. The RALE severity scores were calculated by expert radiologists and categorized as normal, mild, moderate, and severe. Chi-square tests and multivariable logistic regression were used to assess the association between the severity category and admission location and clinical characteristics.
Results: Based on the multivariable regression analysis, it has been found that male sex, hypertension, and the RALE severity score were significantly associated with in-hospital mortality. The baseline RALE severity score was associated with the need for critical care (P< 0.001), in-hospital mortality (P< 0.001), and the admission location (P=0.002).
Discussion: The utilization of RALE severity scores helps to predict clinical outcomes and promote prudent use of resources during the COVID-19 pandemic.
Keywords: COVID-19, chest radiograph, RALE score, prognosis, statistical analysis
Introduction
Since the outbreak of COVID-19 in December 2019, the world has been under strain.1,2 As of March 1, 2022, the virus has infected over 433 million individuals, accounting for 5.9 million deaths worldwide.20
Concurrently, the virus has infected over 1,638,228 people in Jordan, with most cases being reported in Amman. As COVID-19 continues to spread, the number of deaths related to it has reached 13,959 (as of March 11, 2022) and is expected to continue to rise.3 Many studies have examined the outcomes of COVID-19 among non-communicable disease (NCD) patients.4–6 The COVID-19 infection has a high direct death ratio, and it has put pressure on healthcare systems in Jordan and elsewhere, forcing many hospitals to suspend or delay services for NCD patients.4 The limited availability of personal protective equipment and hospital beds has also increased the pressure on the Jordanian healthcare system.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is highly infectious and causes what is commonly called COVID-19, which is a respiratory infection that leads to severe pneumonia and even acute respiratory distress syndrome (ARDS).7,8 At present, the gold standard for diagnosing COVID-19 infection is the reverse transcription-polymerase chain reaction (RT-PCR) test; however, as the demand exceeds testing capacity, the Chest Radiographs (CXRs) are used as an alternative test for suspected cases.1,9,10
According to a study on the utility of CXR in assisting the diagnostic process of COVID-19,21 it has been determined that the presence of confluent and/or patchy, consolidation, or bandlike ground-glass opacity in the mid to lower and peripheral of the lung zone distribution of CXR indicates the infection of COVID-19, and it was recommended to use these indicators in conjunction with the clinical diagnosis to make an accurate judgment.
It is important to properly classify patients with COVID-19 infection, depending on the severity of their condition, to achieve adequate resource allocation.11 Peripheral oxygen saturation (SpO2) levels reflect the extent of pulmonary function impairment and are among the parameters investigated at the time of hospital admission. In addition, among patients with NCDs, SpO2 values may help determine whether a patient with COVID-19 infection requires treatment in an intensive care unit (ICU).11–13 Therefore, using CXR images alongside other emergency department parameters may improve the accuracy of diagnosis and the suitability of treatment modalities. Although the CXR is classified as a non-sensitive method for the early detection of the disease, it is considered the most useful tool to monitor the progression of abnormalities in the lung of infected patients.22
The severity of CXR helps to predict COVID-19 outcomes, especially with the presence of CXR reporting systems, such as Brixia, and Radiographic Assessment of Lung Edema (RALE),23 which helped to predict the negative outcomes of the disease, reliably. In addition, using the CXR severity score may help in decision-making regarding the most suitable admission department.14,15
However, Computed Tomography (CT) imaging may be a more accurate and sensitive diagnostic method than CXR images; nevertheless, the disinfection procedures and radiation exposure involved have resulted in the American College of Radiology recommendation that portable CXR machines be included as a first-line triage tool.9,16,17
According to the statistics of the ministry of health in Jordan (as of March 11, 2022),3 the occupancy rate of isolation beds, ICU beds, and Ventilators were 8%, 17%, and 8%, accordingly. In Jordan, CXR is routinely performed, before and after COVID-19, for patients presenting with respiratory clinical symptoms at the emergency department.
Therefore, CXR imaging results combined with RT-PCR results can decrease the pressure on the healthcare system in Jordan. In addition, the admission location of the patients can be predicted and the decision-making at the emergency department can be improved. Although the healthcare system of Jordan faces limited bed availability in the ICUs, the use of CXR findings can be the new standard to make more beds available for severe cases. This study aimed to examine the relationship between CXR severity scores and clinical outcomes of COVID-19 patients.
The rest of this work is distributed as follows: Materials and Methods presents the material and methods used in this work. Results introduces the results of the experiments and results. Besides, Discussion discusses the study from different aspects. Finally, Conclusion concludes the work and results of the study.
Materials and Methods
This single-center, retrospective cohort study was conducted at King Abdullah University Hospital in Irbid, Jordan. It was conducted in accordance with the principles embodied in the Declaration of Helsinki and was approved by the institutional review board of the King Abdullah University Hospital, where the ethics committee waived the informed consent requirement because of the retrospective design of the study.
The used data included all hospitalized patients with RT-PCR-confirmed COVID-19 infection. CXR images of eligible patients were acquired during the month of November 2020, as shown in Figure 1.
 |
Figure 1 Flow diagram of the retrospectively reviewed chest x-ray (CXR) images. |
Patients were included in the present study if they were aged ≥18 years, had an RT-PCR-confirmed diagnosis of COVID-19, and underwent CXR imaging at the time of hospital admission, where they presented with symptoms consistent with the COVID-19 infection (fever, cough, dyspnea, respiratory impairment, diarrhea, and asthenia).
The PCR-RT findings were used as reference findings, where the exclusion criteria were patients aged <18 years, symptomatic patients with a negative PCR test, the low-quality images due to insufficient inhale breathing during scanning, and no CXR image is available at the emergency department.
Data on the patients’ demographic and clinical characteristics were retrieved from the electronic system of the King Abdullah University Hospital, including vital signs, blood test findings, and SpO2 values on admission, and health history, including smoking status, NCD diagnoses, and other comorbidities. All admission CXR images included in this study were performed within 48 hours after admission at the emergency department of the King Abdullah University Hospital with the posterior-anterior projection and saved in a picture archiving and communication system.
The Radiographic Assessment of Lung Edema (RALE) score was developed by Warren et al18 to assess the severity of lung edema and ARDS; it is a widely accepted and useful tool for lung disease assessment. In this study, three expert radiologists with 4–30 years of experience reviewed the images and estimated severity scores using a modified RALE scoring criteria and consensus.
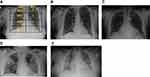
The CXR scores were categorized as normal, mild, moderate, or severe. These scores were obtained by dividing each lung into four segments (a total of eight segments per radiograph). A score of one point was assigned to each segment with any sign of infection, such as consolidation or ground-glass opacities. The total scores represented the sum of individual scores, where the level of severity was identified according to total points assigned to each radiograph as follows: normal 0, mild (1–2), moderate (3–6), and severe (7–8) as shown in Figure 2.
The intra-rater and inter-rater reliability were examined by a team of two radiologists using the coefficient of intraclass correlation for the modified RALE. A Chi-square test is a statistical hypothesis test that is used to investigate the relationship between variables. It is a number that shows the difference between the observed counts and the expected counts in case there were no relationships in the population. In this study, the Chi-square test was used to measure the correlation between CXR severity score, NCD, discharge status, and admission location, where the value of P≤0.05 was considered as an indicator to the statistically significant. All analyses were completed using SPSS (IBM Corp. Released 2015. IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY: IBM Corp).
Results
Of the 153 eligible patients, five were excluded due to their lack of CXR images because the attending physicians did not request for them upon the patients’ presentation to the emergency department. The included patients had RT-PCR-confirmed COVID-19 infection. A total of 148 patients (84 women) with a mean age of 65.07 (median: 66.50) years were included in this study.
At the time of admission, the median blood pressure value was 127/73 mmHg, median SPO2 was 80%, and median respiratory rate was 22 breaths per minute. Data on NCD prevalence, blood test findings, and comorbidities are presented in Table 1.
 |
Table 1 Demographic and Clinical Characteristics of Patients Included in the Present Study |
Approximately half of the patients (81 [54.7%]) had diabetes mellitus (DM); 96 (64.8%), 19 (12.8%), and 72 (48.6%) patients had, in the respective order, hypertension (HTN), dyslipidemia, and other comorbidities such as cardiovascular disease (heart failure, ischemic heart disease), respiratory disease (asthma, pulmonary edema, chronic obstructive pulmonary disease, pulmonary embolism), cancer (colon and breast), kidney disease (end stage renal disease and renal failure), cerebrovascular disease (stroke), Parkinson’s disease, dementia, and Alzheimer’s disease. All these factors may aggravate the severity of COVID-19 infection. In addition, 50 (33.8%) patients were admitted to the ICU; however, the overall mortality rate was 50.7%, whereas the mortality rate in the ICU was 98%. No significant differences between men and women were found in DM or dyslipidemia prevalence as per results in Table 2.
 |
Table 2 Sex-Based Comparison of the Patients with COVID-19 (N=148) |
However, there were significant mean differences in HTN scores (χ2=5.12, P=0.01). In addition, there was a significant correlation between sex and the need for critical care (χ2=29.3, P<0.001); most men were admitted to the ICU, whereas most women were admitted to the general floor. The number of men admitted to the ICU was higher than that of women, suggesting a greater need for observation and interventions such as mechanical ventilators, O2 supply, and general nursing care in the former group than in the latter group.
Patients with DM had more severe CXR scores than did patients without DM; however, no significant correlation was observed (χ2=6.44, P=0.09). Meanwhile, HTN was correlated with CXR severity (χ2=7.65, P=0.05). Patients with high CXR scores were admitted to the ICU more frequently than did those with low scores. Moreover, CXR severity scores were used to predict admission location; most patients with high RALE scores were admitted to the ICU or intermediate units, 75 (59.5%) patients with moderate and severe CXR scores were admitted to the ICU or intermediate units, and there was a significant correlation between CXR severity scores and admission location (χ2=21.01, P=0.002), as shown in Table 3.
 |
Table 3 Chest X-Ray Severity Groups |
Inter-rater and intra-rater reliability results were good for the modified RALE score, with intraclass correlation coefficients of 0.86 (95% CI: 0.80, 0.92), and 0.84 (95% CI: 0.75, 0.92), respectively. As per the results in Table 3, there was a significant correlation between CXR severity score and mortality rate (P<0.001); in fact, 73 (97.3%) patients that died due to COVID-19 infection had moderate and severe CXR scores.
The experimental results can be considered as evidence on the association of CXR severity with outcome in COVID-19. Also, it has a significant positive impact on the management of Covid by predicting the clinical outcomes of COVID-19 in Jordan, Specifically. Besides the novelty of the findings, since this is the first study on severity scores, comorbidity prevalence, and outcomes of patients with COVID-19 disease.
Discussion
One of the most important goals during the COVID-19 pandemic is to perform the most effective and cost-effective medical procedures, especially in resource-limited countries, such as Jordan. Reducing the time of the patient’s presence in the emergency department and increasing the quality of the decision on patient admission location. Most of the studies on COVID-19 have focused on the role of CT.11,19 However, to the best of our knowledge, the present study is the first to examine the correlation between CXR and NCD, admission location, and discharge status in Jordan.
The findings of this study have shown a significant correlation between CXR and the admission location, which can be solid evidence for the use of CXR combined with RT-PCR results to decide the admission location during the COVID-19 pandemic. Moreover, the CXR procedure is more accessible, cost-effective, timesaving, and more controlled regarding the infection control measures than the CT procedure.
Furthermore, the findings of this study support previous findings of a study conducted in Italy,11 which used a semiquantitative severity score and showed perfect interobserver agreement and significant correlations with clinical parameters.
Moreover, the findings support another study that has examined the effect of severity scoring systems in the prediction of patient outcomes.24 The study used the Brixia score, where the results recommended using the Brixia score for mortality prediction.
Due to the development of Artificial Intelligence (AI) techniques, the scoring of CXR became one of the interesting topics, where the studies perform a comparison between the AI models and severity scores in terms of the level of accuracy for the prediction of patient outcomes.25,26 From this standpoint, the studies recommend the utilization of AI in combination with early warning scores to optimize the performance of the prediction techniques.
In the present study, we examined the correlation between CXR severity, NCD prevalence, admission location, sex, and discharge status. This study showed a positive relationship between NCD prevalence in patients with COVID-19 infection and CXR severity; patients with HTN had CXR scores of higher severity than did patients without HTN; there was no significant correlation between DM, dyslipidemia, and CXR scores.
In addition, all patients with severe scores were admitted to the ICU or intermediate unit; these findings suggest that CXR severity scores may help determine the need for critical care, thereby enabling a prudent use of healthcare resources.16,17 Most patients with severe CXR scores died due to COVID-19-related complications while being treated in the ICU or intermediate unit; meanwhile, some patients died while being treated on the general floor. These findings highlight the strain that the Jordanian healthcare system has come under during this pandemic, with the number of beds, personal protective equipment supplies, and availability of medical staff all being limited.
In this study, we evaluated CXR severity scores and their association with COVID-19 prognosis. To our knowledge, only one other study has examined severity scores, comorbidity prevalence, and outcomes of patients with COVID-19 disease treated in Jordan. This study had some limitations. First, this study was retrospective, single-centered, and included small sample size, all of which may limit the generalization of the findings as only Jordanian patients were included. Future studies should include larger samples or a wider range of patients to validate the present findings and further elucidate the role of CXR severity scores in triaging COVID-19 infected patients in the emergency department and predicting in-hospital outcomes of these patients.
Conclusion
Overall, the aims of this study were achieved. The present findings suggest that using CXR severity scores may help predict patient trajectory, supporting the prudent use of resources under the strain associated with the COVID-19 pandemic. These findings may be relevant to under-resourced countries such as Jordan. Further research is required to validate these findings and elucidate the underlying mechanisms. We highly recommend the use of CXR combined with RT-PCR results to decide the admission location, which can lead to improved quality of care and more effective use of healthcare resources.
Data Sharing Statement
The data presented in this study are available on request from the corresponding author (Maha Gharaibeh).
Ethics Approval
This study was approved by the institutional review board of Jordan University of Science and Technology, and King Abdullah University Hospital (approval number: 35/138/2021) and patients’ data are confidential. King Abdullah University Hospital belongs to the Jordan University of Science and Technology. It was conducted in accordance with the principles embodied in the Declaration of Helsinki. Informed consent is not required for all individuals in this study. The ethics committee waived the informed consent requirement because of the retrospective design of the study.
Acknowledgments
The authors would like to thank the front-line healthcare providers in Jordan and essential workers during this pandemic.
Funding
This study was financially supported via a funding grant by Deanship of Scientific Research, Taif University Researchers Supporting Project number (TURSP-2020/300), Taif University, Taif, Saudi Arabia.
Disclosure
The authors declare no conflict of interest.
References
1. Singhal T. A review of coronavirus disease-2019 (COVID-19). Indian J Pediatr. 2020;87(4):281–286. doi:10.1007/s12098-020-03263-6
2. Clark A, Jit M, Warren-Gash C, et al. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob Health. 2020;8(8):e1003–e1017. doi:10.1016/S2214-109X(20)30264-3
3. Jordanian Ministry of Health. Coronavirus disease; 2020. Available from: https://corona.moh.gov.jo/en.
4. Gutierrez JP, Bertozzi SM. Non-communicable diseases and inequalities increase risk of death among COVID-19 patients in Mexico. PLoS One. 2020;15:e0240394. doi:10.1371/journal.pone.0240394
5. Basto-Abreu A, Barrientos-Gutiérrez T, Rojas-Martínez R, et al. Prevalence of diabetes and poor glycemic control in Mexico: results from Ensanut 2016 [Article in Spanish]. Salud Publica Mex. 2020;62:50–59. doi:10.21149/10752
6. Hernández-ávila M, Gutiérrez JP, Reynoso-Noverón N. Diabetes mellitus in Mexico. Salud Publica Mex. 2013;55(Suppl 2):S129–S136. doi:10.21149/spm.v55s2.5108
7. Gibson PG, Qin L, Puah SH. COVID −19 acute respiratory distress syndrome (ARDS): clinical features and differences from typical pre- COVID −19 ARDS. Med J Aust. 2020;213:54–56. doi:10.5694/mja2.50674
8. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180(7):934–943. doi:10.1001/jamainternmed.2020.0994
9. Al-Smadi AS, Bhatnagar A, Ali R, Lewis N, Johnson S. Correlation of chest radiography findings with the severity and progression of COVID-19 pneumonia. Clin Imaging. 2021;71:17–23. doi:10.1016/j.clinimag.2020.11.004
10. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi:10.1001/jama.2020.1585
11. Monaco CG, Zaottini F, Schiaffino S, et al. Chest x-ray severity score in COVID-19 patients on emergency department admission: a two-centre study. Eur Radiol Exp. 2020;4(1):68. doi:10.1186/s41747-020-00195-w
12. Velavan TP, Meyer CG. Mild versus severe COVID-19: laboratory markers. Int J Infect Dis. 2020;95:304–307. doi:10.1016/j.ijid.2020.04.061
13. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China. N Engl J Med. 2020;382(8):727–733. doi:10.1056/NEJMoa2001017
14. Murphy K, Smits H, Knoops AJG, et al. COVID-19 on chest radiographs: a multireader evaluation of an artificial intelligence system. Radiology. 2020;296(3):E166–E172. doi:10.1148/radiol.2020201874
15. Kim HW, Capaccione KM, Li G, et al. The role of initial chest X-ray in triaging patients with suspected COVID-19 during the pandemic. Emerg Radiol. 2020;27(6):617–621. doi:10.1007/s10140-020-01808-y
16. Kaleemi R, Hilal K, Arshad A, et al. The association of chest radiographic findings and severity scoring with clinical outcomes in patients with COVID-19 presenting to the emergency department of a tertiary care hospital in Pakistan. PLoS One. 2021;16(1):e0244886. doi:10.1371/journal.pone.0244886
17. Yasin R, Gouda W. Chest X-ray findings monitoring COVID-19 disease course and severity. Egypt J Radiol Nucl Med. 2020;51(1):193. doi:10.1186/s43055-020-00296-x
18. Warren MA, Zhao Z, Koyama T, et al. Severity scoring of lung oedema on the chest radiograph is associated with clinical outcomes in ARDS. Thorax. 2018;73(9):840–846. doi:10.1136/thoraxjnl-2017-211280
19. Mossa-Basha M, Meltzer CC, Kim DC, Tuite MJ, Kolli KP, Tan BS. Radiology department preparedness for COVID-19: radiology scientific expert review panel. Radiology. 2020;296(2):E106–E112. doi:10.1148/radiol.2020200988
20. World Health Organization. COVID-19 Weekly Epidemiological Update.
21. Smith DL, Grenier JP, Batte C, et al. A characteristic chest radiographic pattern in the setting of the COVID-19 pandemic. Radiology. 2020;2(5):e200280. doi:10.1148/ryct.2020200280
22. Cleverley J, Piper J, Jones MM. The role of chest radiography in confirming covid-19 pneumonia. BMJ. 2020;370. doi:10.1136/bmj.m2426
23. Au-Yong I, Higashi Y, Giannotti E, et al. Chest radiograph scoring alone or combined with other risk scores for predicting outcomes in COVID-19. Radiology. 2022;302(2):460–469. doi:10.1148/radiol.2021210986
24. Maroldi R, Rondi P, Agazzi GM, et al. Which role for chest x-ray score in predicting the outcome in COVID-19 pneumonia?. Eur Radiol. 2021;31(6):4016–4022. doi:10.1007/s00330-020-07504-2
25. Ebrahimian S, Homayounieh F, Rockenbach MA, et al. Artificial intelligence matches subjective severity assessment of pneumonia for prediction of patient outcome and need for mechanical ventilation: a cohort study. Sci Rep. 2021;11(1):1–10. doi:10.1038/s41598-020-79470-0
26. Mushtaq J, Pennella R, Lavalle S, et al. Initial chest radiographs and artificial intelligence (AI) predict clinical outcomes in COVID-19 patients: analysis of 697 Italian patients. Eur Radiol. 2021;31(3):1770–1779. doi:10.1007/s00330-020-07269-8
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.