Back to Journals » Cancer Management and Research » Volume 9
Chemotherapy-associated paronychia treated with 2% povidone–iodine: a series of cases
Authors Capriotti K , Capriotti J, Pelletier J, Stewart K
Received 10 April 2017
Accepted for publication 18 May 2017
Published 26 June 2017 Volume 2017:9 Pages 225—228
DOI https://doi.org/10.2147/CMAR.S139301
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Antonella D'Anneo
Kara Capriotti,1,2 Joseph Capriotti,1,3 Jesse Pelletier,1,3 Kevin Stewart1,3
1Veloce BioPharma LLC, Fort Lauderdale, FL, 2Bryn Mawr Skin and Cancer Institute, Rosemont, PA, 3Plessen Ophthalmology Consultants, Christiansted, VI, USA
Background: Nail changes are known to occur during the use of chemotherapy for a variety of malignancies, particularly those treated with taxanes and EGFR inhibitors. There are currently no actively recruiting prospective clinical trials investigating potential treatments. There are also no US Food and Drug Administration-approved medical treatments for chemotherapy-associated paronychia and no consensus on the best way to treat these common chemotherapy-induced events.
Methods: A retrospective review of all cases presenting to a single dermatology private practice from June 2016 to January 2017 identified nine patients with chemotherapy-associated paronychia seeking treatment. Each patient was prescribed a topical solution comprised of 2% povidone–iodine in a dimethylsulfoxide vehicle that was prepared by a licensed compounding pharmacy. Patients were seen at 3 week and 6 week follow-up visits.
Results: All 9/9 patients demonstrated complete or partial resolution. The number of nails involved for each patient ranged from 4–12. There were a total of 58 nails affected in the case series, and 44/58 (76%) resolved overall. The treatment was well tolerated.
Conclusion: The topical povidone–iodine/dimethylsufoxide solution described is very effective in alleviating the signs and symptoms of paronychia associated with chemotherapy. This novel combination warrants further investigation in randomized, controlled trials to further elucidate its clinical utility.
Keywords: paronychia, chemotherapy, taxanes, epidermal growth factor receptor inhibitor, povidone–iodine, dimethylsulfoxide
Introduction
Systemic chemotherapy employed for the treatment of a variety of common malignancies can induce painful nails changes in a subset of patients. The most common chemotherapeutic agents associated with these changes are the taxanes (docetaxel, paclitaxel, nab-paclitaxel) and both classes of EGFR inhibitors. Numerous chemotherapy-induced nail pathologies have been reported, ranging from mild and asymptomatic to more severe and potentially debilitating. Minor changes include dyschromia, Beau’s lines, Mees lines, Muehrcke’s lines, onychodystrophy, and subungual hemorrhages.1 Nail changes associated with higher morbidity include periungual erythema, edema, exudate, and suppurative onycholysis, all of which regularly become secondarily infected.2 Additionally, the nail might be affected by periungual or subungual pyogenic granulomas, especially in patients treated with EGFR inhibitors.3 These changes can cause pain and discomfort, leading to impairment of manual activities, deambulation, and even necessitate modification or discontinuation of anticancer treatment.4,5
The National Cancer Institute’s Common Terminology Criteria for Adverse Events (CTCAE) version 4.0 classifies three grades of nail loss. Grade 1 changes are classified as nail fold edema or erythema and disruption of the cuticle. Grade 2 changes are defined as nail unit changes that include nail fold edema or erythema with pain associated with discharge or nail plate separation leading to limitation of instrumental activities of daily living (ADL). Localized intervention is indicated by means of oral intervention (eg, antibiotic, antifungal, antiviral). Grade 3 changes are defined as limiting self-care ADL, necessitating surgical intervention or intravenous antibiotics.6 There is currently no consensus therapy approved by the US Food and Drug Administration for chemotherapy-associated paronychia. There are few clinical trials investigating potential treatments for cutaneous adverse events of chemotherapy and none that specifically evaluate improvement of chemotherapy-associated paronychia as a primary endpoint. Anecdotal data have demonstrated topical application of antibiotics or steroids in mild cases, oral antibiotics or corticosteroids in moderate cases, and severe cases requiring surgical intervention in the form of complete or partial nail avulvsions.7
Methods
An IRB waiver was obtained to perform a retrospective chart review. A retrospective review of all cases presenting to a single private dermatology private practice from June 2016 to January 2017 identified nine patients with chemotherapy-associated paronychia seeking treatment. Patients with recalcitrant chemotherapy-associated paronychia were referred from local oncology offices. Previous treatment modalities prescribed by oncology were discontinued. Each patient was prescribed a topical solution comprised of 2% povidone–iodine (PVP-I) in a dimethylsulfoxide (DMSO) vehicle that was prepared by a licensed compounding pharmacy. The patient was instructed to apply the solution twice daily to the nail folds, nail plate, and subungual space. Patients typically returned to the office at 3 week intervals with number of nails involved being recorded at each visit. Adverse effects were evaluated at each visit. Paronychia was inclusive of periungual edema, erythema, exudate, onycholysis with or without subungual abscess, and periungual or subungual granulation tissue. Bacterial and fungal cultures were performed at baseline visit as well.
Results
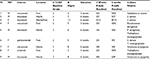
All 9/9 patients demonstrated complete or partial resolution within 6 weeks of therapy. Seven patients were classified as CTCAE grade 2 and two patients as grade 3 at treatment initiation, and each of the patients demonstrated improvement and CTCAE downgrading during treatment. Four patients had finger-only involvement, four patients had toe-only and one patient had mixed involvement of both fingers and toes. The number of nails involved for each patient ranged from 4–12. There were a total of 58 nails affected in the series of all cases, and 44/58 (76%) completely resolved. Complete resolution of paronychia occurred in 3/9 (33%) patients, and partial resolution occurred in 6/9 (66%) of patients. Of the nine patients, 4/9 (44%) received taxanes and 5/9 (56%) received EGFR inhibitors. For the patients receiving taxanes who developed paronychia, all four patients had a partial response. All 4/4 patients demonstrating partial response at the 6 week follow-up had at least one nail with residual onycholysis, which was counted as a treatment failure. The other nail morbidities including erythema, edema, exudate, and subungual suppuration demonstrated downgrading. Of the patients receiving EGFR inhibitors, three patients had complete response (all at the 3 week visit) and two patients had partial responses. Patients receiving taxanes and EGFR inhibitors with a partial response (6/6) did not return after the 6 week visit as pain had greatly subsided and they resumed ADL. Mild irritation at application site was noted in 2/9 (22%) of patients but did not affect application schedule. All 9/9 patients subjectively reported resolution of nail unit pain within 2–7 days, and none required chemotherapy dose modification or discontinuation by oncology while using topical therapy. None of the patients reported stinging or burning at application site. All 9/9 (100%) of patients had positive fungal and/or positive bacterial cultures at baseline (Table 1).
Discussion
The pathophysiology of chemotherapy-associated paronychia is thought to originate with chemotherapy’s direct impact on nail apparatus changes, which includes the nail plate and the surrounding soft tissue structures. Nail plate changes from chemotherapy are believed to result from many factors, including defective nail plate production resulting from acute damage to the nail matrix, disruption of the nail plate secondary to chemotherapy’s toxic effects on cellular maturation, and direct toxicity to structures of and surrounding the nail apparatus.8 These structural disruptions, in combination with the inherent immunosuppression of the patient, allow for the nail apparatus to become secondarily infected. Numerous case reports and case series document secondary bacterial, fungal, and yeast infections of both the nail plate and periungual soft tissue structures.2,9–15
PVP-I is well recognized as a broad-spectrum, resistance-free biocidal agent that has a long track record of safety and tolerability given its long-term use as a presurgical antiseptic. Although immensely versatile in its ability to kill all known microorganisms including bacteria, viruses, yeasts, molds, fungi, and protozoa, PVP-I has been primarily only used in dermatology as a presurgical skin preparation. The mechanism of action likely involves impaired electron transport, inhibition of cellular respiration, destabilization of membranes, inhibition of protein synthesis, and denaturation of nucleic acids. PVP-I is a polymeric complex of long-chain polyvinylpyrrolidone units with associated iodine, trioiodide, and iodate species in a complicated equilibrium. Paradoxically, dilution of PVP-I increases its antimicrobial potency by releasing more free molecular iodine, the most active biocidal form of iodine present in PVP-I.16
Aside from its antimicrobial properties, PVP-I also has the ability to suppress the inflammatory component of paronychia. Anti-inflammatory properties of a liposomal hydrogel with PVP-I for wound healing were studied in vitro and found to be rapidly effective in its ability to scavenge superoxide anions, inhibit neutrophil production of reactive oxygen species, and stabilize mast cells.17 In this way, PVP-I can behave as both an oxidizing agent and a reducing agent, mainly by iodine’s free radical scavenging and reduction of superoxide.18 All of our patients noted that the pain associated with the paronychia substantially decreased within the first 48 hours after application, which could be explained by a generalized ant-inflammatory effect of PVP-I.
DMSO is an effective pharmaceutical vehicle known to enhance percutaneous penetration of small molecules when used in sufficiently high concentrations. It is a polar, aprotic solvent that has the ability to carry an enormous library of molecules through the stratum corneum and into the dermis. We have surprisingly found that DMSO can also deliver PVP-I through keratinized epithelial surfaces, despite the large size of the PVP-I complexes. PVP-I in combination with DMSO has the ability to penetrate the nail structure, quickly reduce inflammation and pain, and eradicate both fungal and bacterial organisms present in pretreatment cultures.
Nail changes occur with 34.9% and 17.2% of patients receiving taxanes and EGFR inhibitors, respectively.20,21 It has been reported that taxanes are associated most commonly with erythema, edema, exudate, suppuration, and onycholysis. Peripheral nerve fibers may play a role in the development of chemotherapy-induced onycholysis as the inflammatory process is maintained by postganglionic sympathetic terminals and nociceptive c-fiber afferents.22,23 Elevated protoporphyrin levels have also been suggested as causative, but a definitive mechanism has not been elucidated.24–26 EGFR inhibitors have the tendency to cause erythema, edema, exudate, and granulation tissue (both periungual and subungual) consistent with pyogenic granulomas. Increased VEGF has been postulated to be causative.27 This case review demonstrates considerable success with this novel, dilute PVP-I treatment. Our anecdotal results in this small number of severe cases are encouraging. Prospective evaluation in vehicle-controlled, double-blinded clinical trials may be warranted to further evaluate this promising new therapy.
Ethical statement
Sterling IRB was used. The waiver granted was an exemption from IRB Review Determination pursuant to the terms of the U.S. Department of Health and Human Service’s Policy for Protection of Human Research Subjects under 45 C.F.R. 46.101(b). Patient consent to review their medical records was not required by the IRB. Patient confidentiality was maintained according to established HIPPA guidelines.
Disclosure
Authors listed are equity holders in Veloce BioPharma, LLC. Drs. Capriotti are cofounders and paid consultants for Veloce BioPharma, LLC. The authors report no other conflicts of interest in this work.
References
Susser WS, Whitaker-Worth DL, Grant-Keis JM. Mucocutaneous reactions to chemotherapy. J Am Acad Dermatol. 1999;40(3):367–398. | ||
Minisini AM, Tosti A, Sobrero AF, et al. Taxane-induced nail changes: incidence, clinical presentation and outcome. Ann Oncol. 2002;14:333–337. | ||
Robert C, Sibaud V, Mateus C, et al. Nail toxicities induced by systemic chemotherapy treatments. Lancet Oncol. 2015;16(4):e181–e190. | ||
Piracccine BM, Alessandrini A. Drug-related nail disease. Clin Dermatol. 2013;5:618–626. | ||
Rosen AC, Case EC, Dusza SW, et al. Impact of dermatologic adverse events on quality of life in 283 cancer patients: a questionnaire study in a dermatology referral clinic. Am J Clin Dermatol. 2013;14:327–333. | ||
National Cancer Institute Cancer Therapy Evaluation Program [homepage on the Internet]. Common Terminology Criteria for Adverse Events and Common Toxicity Criteria [v4.0]; 2010. Available from: http://www.oncology.tv/SymptomManagement/NationalCancerInstituteUpdatesCTCAEtov403.aspx. Accessed April 8, 2017. | ||
Paraccini BM, Iorizzo M, Starace M, et al. Drug-induced nail diseases. Dermatol Clin. 2006;24:387–391. | ||
Gupta A, Parakh A, Dubey AP. Chemotherapy induced nail changes. Indian J Dermatol. 2008;53(4):204–205. | ||
Hussain S, Anderson DN, Salvatti ME, et al. Onycholysis as a complication of systemic chemotherapy: report of five cases associated with prolonged weekly paclitaxel therapy and review of the literature. Cancer. 2000;88(10):2367–2371. | ||
Chen G, Chen Y, Hsu M, et al. Onychomadesis and onycholysis associated with capecitabine. Br J Dermatol. 2001;145(3):521–522. | ||
Segaert S, Van Cutsem E. Clinical signs, pathophysiology and management of skin toxicity during therapy with epidermal growth factor receptor inhibitors. Ann Oncol. 2005;16(9):1425–1433. | ||
Spazzapan S, Crivellari D, Lombardi D, et al. Nail toxicity related to weekly taxanes: an important issue requiring a change in common toxicity criteria grading? J Clin Oncol. 2002;20(21):4404–4405. | ||
Mortimer J, Jung J, Yuan Y, et al. Skin/nail infections with the addition of pertuzumab to trastuzumab-based chemotherapy. Breast Cancer Res Treat. 2014; 148(3):563–570. | ||
Wantzin GL, Thomsen K. Acute paronychia after high-dose methotrexate therapy. Arch Dermatol. 1983;119(7):623–624. | ||
Hijjawi JB, Dennison DG. Acute felon as a complication of systemic paclitaxel therapy: case report and review of the literature. Hand. 2007;2(3):101–103. | ||
Capriotti K, Capriotti JA. Topical iodophor preparations: chemistry, microbiology, and clinical utility. Dermatol Online J. 2012; 18(11):1. | ||
Beukelman CJ, van den Berg AJ, Hoekstra MJ, et al. Anti-inflammatory properties of a liposomal hydrogel with povidone-iodine (Repithel®) for wound healing in vitro. Burns. 2008;34:845–855. | ||
Schwarz HA, Bielski BHJ. Reactions of HO2 and O2– with iodine and bromine and the I2- and I atom reduction potentials. J Phys Chem. 1986;90:1445–1448. | ||
Capriotti K, Capriotti JA. Dimethyl sulfoxide: history, chemistry, and clinical utility in dermatology. J Clin Aesthet Dermatol. 2012;5(9):24–26. | ||
Capriotti K, Capriotti JA, Lessin S, et al. The risk of nail changes with taxane chemotherapy: a systemic review of the literature and meta-analysis. Br J Dermatol. 2015;173(3):842–845. | ||
Garden BC, Wu S, Lacouture ME. The risk of nail changes with Epidermal Growth Factor Receptor Inhibitors. J Am Acad Dermatol. 2012;67(3):400–408. | ||
Wasner G, Hilpert F, Schattschneider J, Binder A, Pfisterer J, Baron R. Docetaxel-induced nail changes – a neurogenic mechanism: a case report. J Neurooncol. 2002;58(2):167–174. | ||
Wasner G, Hilpert F, Baron R, Pfisterer J. Clinical picture: nail changes secondary to docetaxel. Lancet. 2001;357(9260):910. | ||
Ghetti E, Piraccini BM, Tosti A. Onycholysis and subungual haemorrhages secondary to systemic chemotherapy (paclitaxel). J Europ Acad Dermtol Venereol. 2003;17(4):459–460. | ||
Pham AQ, Berz D, Karwan P, Colvin GA. Cremophor-induced lupus erythematosus-like reaction with taxol administration: a case report and review of the literature. Case Rep Oncol. 2011;4(3):526–530. | ||
Tokunaga M, Iga N, Endo Y, et al. Elevated protoporphyrin in patients with skin cancer receiving taxane chemotherapy. Eur J Dermatol. 2013;23(6):826–829. | ||
Bragado R, Bello E, Requena L, et al. Increased expression of vascular endothelial growth factor in pyogenic granulomas. Acta Derm Venereol. 1999;79:422–425. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.