Back to Journals » Journal of Inflammation Research » Volume 14
Chemokine Receptor 2 (CXCR2) Gene Polymorphisms and Their Association with the Risk of Developing Peri-Implantitis in Chinese Han Population
Authors Qi Y, Li C, Du Y, Lin J, Li N, Yu Y
Received 28 January 2021
Accepted for publication 11 March 2021
Published 23 April 2021 Volume 2021:14 Pages 1625—1631
DOI https://doi.org/10.2147/JIR.S304261
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Ning Quan
Yuesun Qi,1,2,* Cheng Li,1,3,* Yimin Du,2 Jichao Lin,1 Nan Li,2 Youcheng Yu1
1Department of Stomatology, Zhongshan Hospital, Fudan University, Shanghai, 200032, People’s Republic of China; 2Department of Stomatology, Jinshan Hospital, Fudan University, Shanghai, 200540, People’s Republic of China; 3Department of Stomatology, Jing’an District Institute of Dental Diseases, Shanghai, 200040, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Youcheng Yu
Department of Stomatology, Zhongshan Hospital, Fudan University, No. 180 Fenglin Road, Xuhui District, Shanghai, 200032, People’s Republic of China
Tel/Fax +86 21 64041990
Email [email protected]
Purpose: This study aimed to investigate the role of chemokine receptor 2 (CXCR2) gene polymorphisms in peri-implantitis susceptibility in a Chinese Han population.
Patients and Methods: A total of 260 individuals were included in this study, including 127 peri-implantitis patients and 133 healthy implants. CXCR2 gene rs2230054 and rs1126580 polymorphisms in different groups were analyzed by the Chi-square test. The odds ratios (ORs) and 95% confidence intervals (95% CIs) were employed to evaluate the association between CXCR2 polymorphism and peri-implantitis susceptibility.
Results: The CT genotype of rs2230054 and the AG genotype and G allele of rs1126580 significantly increased in peri-implantitis patients compared with healthy implants (P < 0.05). The CT genotype of rs2230054 (OR = 1.825, 95% CI = 1.028– 3.239) and the AG genotype of rs1126580 (OR = 2.223, 95% CI 1.272– 3.885) carriers had a high risk to infect with peri-implantitis. Additionally, these CXCR2 gene polymorphisms have been revealed to be associated with the periodontal status of peri-implantitis patients.
Conclusion: The CXCR2 gene rs2230054 and rs1126580 polymorphisms were associated with the peri-implantitis susceptibility in the Chinese Han population. The CT genotype of rs2230054 and the AG genotype and G allele of rs1126580 serve as risk factors for the occurrence of peri-implantitis.
Keywords: chemokine receptor 2, CXCR2, polymorphism, peri-implantitis, Han population
Introduction
Dental implants are common options for patients who need the treatment of partial or total edentulism.1 Peri-implantitis is an irreversible chronic inflammatory, which is one of the major causes of the failure in implant dentistry and is prevalent in patients that received dental implant.1,2 The diagnosis of peri-implantitis depends on the bone loss and bleeding on probing with or without concomitant and the presence of purulent drainage.3 There are a variety of risk factors that may attribute to peri-implantitis, including systemic conditions, environmental factors, history of periodontitis, and implant materials.4,5 Additionally, the genetic trait has also been considered as an etiology of peri-implantitis, as the genetic variations could affect the function of genes.6 The significant association between cytokine gene polymorphism, such as CD14, TNFα, and IL-6, and peri-implantitis risk in the Serbian population have been indicated in the previous study.7 The identification of a marker that correlated with the development of peri-implantitis is of great importance in the clinic to improve the management of peri-implantitis.
Interleukin-8 (IL-8) is a proinflammatory cytokine.8 By binding to Chemokine Receptor 2 (CXCR2), IL-8 could initiate chemotaxis, induce angiogenesis, stimulate cell proliferation, mediate hypernociception, and increase the concentration of calcium in various functional cells.9 Single-nucleotide polymorphisms (SNPs) in gene sequences could alter the transcription of gene or the function of encoded protein, which may account for the pathogenesis of human disease.10 CXCR2 is located on 2q35, of which the gene polymorphisms have been revealed to be associated with the susceptibility of various diseases, such as stroke in patients with essential hypertension, prostate cancer, and systemic sclerosis.11–13 CXCR2 gene has been demonstrated to be expressed in oral epithelial cells.14 Kavrikova et al have reported that CXCR2 gene variants are correlated with the subgingival Gran-negative bacteria in chronic periodontitis patients, which is the major cause of periodontitis.15 Therefore, CXCR2 was speculated to be involved in the pathogenesis of peri-implantitis.
The CXCR2 gene + 785C/T (rs2230054) and the CXCR2 + 1440G/A (rs1126580) are two common SNPs of CXCR2. In this study, the genotypes were analyzed in these two SNPs in peri-implantitis patients and healthy controls in the Chinese Han population, to calculate the association of these SNPs with the susceptibility of peri-implantitis.
Patients and Methods
Subjects
A total of 127 patients diagnosed with peri-implantitis and 133 individuals with healthy implant were recruited in this study from 2017–2019. The basic clinical characteristics of the study subjects are summarized in Table 1. The periodontal evaluation was performed through a series of corresponding parameters, including gingival index, plaque index, calculus index, peri-implant pocket depth, and clinical attachment level, which have been listed in Table 2. All patients included in this study are Chinese Han population and attended to regular implant maintenance therapy at 6, 12, and 24 months after the loading of implants. The peri-implantitis patients were included according to the previous definition of peri-implantitis and peri-implant health16,17 and details are as follows: the presence of one or more implants with the loading period of more than 12 months; the presence of bleeding probing and the probing pocket depths > 4mm; the presence of crestal bone loss in at least one area around an implant; exposure of at least two edges of the implant. The exclusion criteria for enrolling patients were a history of systemic disease or occlusal trauma and the use of prophylactic antibiotics or anti-inflammatory drugs. The healthy individuals had no history or clinical signs of peri-implantitis; had a probing pocket depth < 3mm; had no radiographic signs of peri-implant bone resorption. This study was approved by the ethics committee of Zhongshan hospital (2016–145), Fudan university and was in accordance with the Declaration of Helsinki. All participants provided written informed consent before the sample collections.
 |
Table 1 Basic Clinical Characteristics of the Study Population |
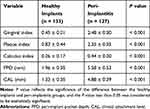 |
Table 2 Periodontal Status of the Studied Population |
Sample Collection
Buccal epithelial cell samples were collected from each participant. Briefly, patients first gargled with 3% glucose solution, and scrape oral mucosa with a sterile wood spatula. The tip of the spatula was immediately shaken into the mouthwash solution and centrifugated at 2000 g for min to obtain buccal epithelial cells. The genomic DNA was extracted from collected buccal epithelial cell samples with the QIAamp DNA Mini Kit (QIAGEN, Germany) according to the manufacturer’s protocol. The genomic DNA was stored at −80°C.
Genotyping
The genotypes of SNPs in the CXCR2 gene were examined using the polymerase chain reaction method (PCR). PCR was performed in a volume of 25 μL, including 100 ng DNA, 0.5 μM primers, 4 U of Taq DNA polymerase, 2mM buffer, and 0.5 mM deoxyribonucleoside triphosphate mix. The reaction condition was as follows: denaturation for 5 min at 95°C followed by 35 cycles of 95°C for 1 min, annealing at 58°C for 1 min, 72°C for 1 min, and a final extension at 72°C for 7 min. The primer sequences of + 785C/T (rs2230054) and + 1440G/A (rs1126580) were summarized in Table 3.
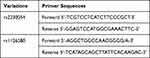 |
Table 3 Primer Sequences of CXCR2 Gene rs2230054 and rs1126580 Polymorphisms |
The purification of PCR products was conducted with ExoSAP-IT (USB Corp) and sequenced with an Applied Biosystems 3730×l automated sequencer (Applied Biosystems, Foster City, CA, USA), and all sequences were analyzed by Vector NTI software.
Statistical Analysis
Statistical analyses were performed with the PASW Statistical 18.0 statistical software. The genotype and allele frequencies for rs2230054 and the rs1126580 were calculated by direct counting. Hardy–Weinberg equilibrium (HWE) of each polymorphism was tested to assess the representativeness of the study population. The distributions of the genotypes and allele of rs2230054 and rs1126580 in different groups were compared by the Chi-square test. The association between CXCR2 polymorphism and peri-implantitis susceptibility was evaluated by the odds ratios (ORs) and 95% confidence intervals (95% CIs). P < 0.05 was considered to be statistically significant.
Results
Characteristics of the Study Subjects
The basic clinical characteristics of the study population are summarized in Table 1. 127 peri-implantitis patients were composed of 70 males and 57 females with the average age of 44.07 ± 6.05, which showed no significant difference with that of healthy implants (P > 0.05). Meanwhile, alcohol consumption, platform type, position, peri-implantitis, brushing daily, dental floss daily, mouth washing daily, and smoking habit between peri-implantitis and healthy implants were not significantly different (P > 0.05). However, the history of periodontitis of peri-implantitis patients was dramatically frequent than in healthy implants (P = 0.034). The concentration of chemokines, including IL-8 (P < 0.001) and MIP1-α (P < 0.001), was significantly higher in peri-implantitis patients than that of healthy implant.
For the periodontal status of participants, peri-implantitis patients possessed much higher scores of the gingival index, plaque index, calculus index than that of healthy implants (P < 0.001, Table 2). Moreover, the peri-implant pocket depth and the clinical attachment level of peri-implantitis patients were also significantly larger than that of healthy implants (P < 0.001, Table 2).
Association of CXCR2 Polymorphisms with the Risk of Peri-Implantitis
Both the distribution of the genotype and allele of CXCR2 gene rs2230054 and rs1126580 polymorphisms in healthy implants did not deviate from HWE, indicating the good representativeness of the study subjects (PHWE > 0.05, Table 4).
 |
Table 4 Genotype and Allele Frequencies of CXCR2 Gene rs2230054 and rs1126580 Polymorphisms Between Healthy Implants and Peri-Implantitis Groups |
For rs2230054 polymorphism, the frequency of CT genotype significantly increased in peri-implantitis patients compared with healthy implants (64.6% vs 51.9%, P = 0.039). Individuals with CT genotype showed a high risk of peri-implantitis (OR = 1.825, 95% CI = 1.028–3.239). Similarly, in rs1126580 polymorphism, the AG genotype frequency dramatically increased in peri-implantitis (P = 0.005) and AG genotype indicated a high risk of peri-implantitis (OR = 2.223, 95% CI = 1.272–3.885). Moreover, the G allele of rs1126580 significantly increased in peri-implantitis compared with healthy implants, which was correlated with the susceptibility of peri-implantitis (OR = 1.441, 95% CI = 1.015–2.046).
Association of CXCR2 Polymorphisms with the Periodontal Status of Peri-Implantitis Patients
The association between CXCR2 polymorphisms and the periodontal index of healthy implant and peri-implantitis patients was evaluated. As shown in Table 5, rs2230054 and rs1126580 genotype significantly affected the gingival index of peri-implantitis (P < 0.05), while the rs2230054 CT carriers and the rs1126580 AG carriers had a higher gingival index than other genotype carriers. Additionally, the rs1126580 AG genotype of CXCR2 also exerted markable effects on the plaque index, calculus index, peri-implant pocket depth, and clinical attachment level of peri-implantitis patients (P < 0.05).
 |
Table 5 Association Analysis of CXCR2 Gene Polymorphisms with Periodontal Status |
Discussion
Peri-implantitis is a primary cause of the failure in implant dentistry.18 Multiple factors have been suggested to influence the occurrence of peri-implantitis, such as occlusal factors, general condition, smoking as well as oral health habit.19 Among various risk factors, the role of genetic traits in the pathogenesis and development of peri-implantitis has drawn special attention. For example, Zhou and Zhao demonstrated people carrying the CC genotype of osteoprotegerin gene rs2073618 polymorphism are more likely to infect peri-implantitis than other genotype carriers.20 The polymorphic variant rs1342913 BRINP3 showed a significant association with the peri-implantitis.21 CXCR2 has been reported to express in a wide range of leukocytes and to mediate a variety of biological activities, including inflammatory reaction, tumor growth, and metastasis. For instance, CXCR2 was suggested to regulate cell proliferation, invasion, and angiogenesis of pancreatic cancer and suppress tumor progression via disrupting interactions between tumor cells and fibroblasts.22–25
Recently, CXCR2 polymorphism has been associated with various diseases. The CXCR2 rs1126579 polymorphism was associated with the risk of ischemic stroke, whereas the CC genotype was protective against stroke.12 In the present study, the potential relevance of rs2230054 and rs1126580 polymorphisms in CXCR2 with the risk of peri-implantitis was investigated in a Chinese Han population. The significant difference was found in the rs2230054 and the rs1126580 genotypes between peri-implantitis and healthy implants. The frequency of CT genotype in rs2230054 and the AG genotype and G allele in rs1126580 significantly increased in peri-implantitis patients indicating that these genotypes and alleles might serve as risk factors for the onset of peri-implantitis whereas the role of CXCR2 polymorphisms was distinct in different populations. Kavrikova et al analyzed the association of CXCR2 gene variants with periodontal bacteria in patients with chronic periodontitis in the Czech population and found that the C allele of rs2230054 and the T allele of rs1126579 in men were closely associated with Aggregatibacter actinomycetemcomitans, the main etiological agent of periodontitis.15 In the Brazilian population, among three SNPs of the CXCR2 gene, including rs2230054, rs1126579, and rs1126580, only rs1126580 showed significant association with periodontitis of patients.26
Further, the history of periodontitis is also an important risk factor for peri-implantitis. Previous studies have reported that patients with a history of periodontitis might be at high risk for peri-implantitis.27 Here, the history of periodontitis was demonstrated to be significantly different between healthy implants and peri-implantitis and the periodontal status of the studied population was also obviously unequal, which is consistent with previous studies. Additionally, rs1126580 polymorphism was found to be associated with the periodontal status of peri-implantitis patients, including the gingival index, plaque index, calculus index, peri-implant pocket depth, and clinical attachment level. While rs2230054 polymorphism was associated with the gingival index of peri-implantitis patients. These periodontal clinical parameters were always applied to assess the health of peri-implant tissues in the clinic. Therefore, these results suggested that the rs2230054 and rs1126580 polymorphisms of the CXCR2 gene were risk factors of peri-implantitis and were speculated to predicate peri-implantitis susceptibility.
The limitation of this study was the studied population was not large enough to achieve nominal significance. As this is a hospital-based case-control and cross-sectional study, the recruited population may not be representative of the general population. More representative studies are required to confirm the role of CXCR2 gene polymorphisms in peri-implantitis in various populations.
Taken together, our results revealed that the rs2230054 and rs1126580 polymorphisms of the CXCR2 gene were closely correlated with peri-implantitis susceptibility in the Chinese Han population. The CT genotype in rs230054, the AG genotype and G allele in rs1126580 were potential risk factors for the occurrence of peri-implantitis.
Abbreviations
CXCR2, Chemokine Receptor 2; ORs, odds ratios; CIs, confidence intervals; IL-8, Interleukin-8; SNPs, Single-nucleotide polymorphisms; PCR, polymerase chain reaction method; HWE, Hardy–Weinberg equilibrium.
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lindhe J, Meyle J; Group DoEWoP. Peri-implant diseases: consensus report of the Sixth European Workshop on Periodontology. J Clin Periodontol. 2008;35(8 Suppl):282–285. doi:10.1111/j.1600-051X.2008.01283.x
2. Konstantinidis IK, Kotsakis GA, Gerdes S, Walter MH. Cross-sectional study on the prevalence and risk indicators of peri-implant diseases. Eur J Oral Implantol. 2015;8(1):75–88.
3. Lang NP, Berglundh T; Working Group 4 of Seventh European Workshop on P. Periimplant diseases: where are we now?–Consensus of the Seventh European Workshop on Periodontology. J Clin Periodontol. 2011;38(Suppl 11):178–181. doi:10.1111/j.1600-051X.2010.01674.x
4. Heitz-Mayfield LJ. Peri-implant diseases: diagnosis and risk indicators. J Clin Periodontol. 2008;35(8Suppl):292–304. doi:10.1111/j.1600-051X.2008.01275.x
5. Schminke B, Vom Orde F, Gruber R, Schliephake H, Burgers R, Miosge N. The pathology of bone tissue during peri-implantitis. J Dent Res. 2015;94(2):354–361. doi:10.1177/0022034514559128
6. Chen X, Zhao Y. Genetic involvement in dental implant failure: association with polymorphisms of genes modulating inflammatory responses and bone metabolism. J Oral Implantol. 2019;45(4):318–326. doi:10.1563/aaid-joi-D-18-00212
7. Petkovic-Curcin A, Zeljic K, Cikota-Aleksic B, Dakovic D, Tatic Z, Magic Z. Association of cytokine gene polymorphism with peri-implantitis risk. Int J Oral Maxillofac Implants. 2017;32(5):e241–e8. doi:10.11607/jomi.5814
8. Sprenger H, Lloyd AR, Lautens LL, Bonner TI, Kelvin DJ. Structure, genomic organization, and expression of the human interleukin-8 receptor B gene. J Biol Chem. 1994;269(15):11065–11072. doi:10.1016/S0021-9258(19)78092-2
9. Morris SW, Nelson N, Valentine MB, et al. Assignment of the genes encoding human interleukin-8 receptor types 1 and 2 and an interleukin-8 receptor pseudogene to chromosome 2q35. Genomics. 1992;14(3):685–691. doi:10.1016/S0888-7543(05)80169-7
10. Xie H, Zeng D, Chen X, et al. Prediction on the risk population of idiosyncratic adverse reactions based on molecular docking with mutant proteins. Oncotarget. 2017;8(56):95568–95576. doi:10.18632/oncotarget.21509
11. Salim PH, Jobim M, Bredemeier M, et al. Combined effects of CXCL8 and CXCR2 gene polymorphisms on susceptibility to systemic sclerosis. Cytokine. 2012;60(2):473–477. doi:10.1016/j.cyto.2012.05.026
12. Timasheva YR, Nasibullin TR, Mustafina OE. The CXCR2 gene polymorphism is associated with stroke in patients with essential hypertension. Cerebrovasc Dis Extra. 2015;5(3):124–131. doi:10.1159/000441529
13. Franz JM, Portela P, Salim PH, et al. CXCR2 +1208 CT genotype may predict earlier clinical stage at diagnosis in patients with prostate cancer. Cytokine. 2017;97:193–200. doi:10.1016/j.cyto.2017.06.001
14. Khurram SA, Bingle L, McCabe BM, Farthing PM, Whawell SA. The chemokine receptors CXCR1 and CXCR2 regulate oral cancer cell behaviour. J Oral Pathol Med. 2014;43(9):667–674. doi:10.1111/jop.12191
15. Kavrikova D, Borilova Linhartova P, Lucanova S, Poskerova H, Fassmann A, Izakovicova Holla L. Chemokine receptor 2 (CXCR2) gene variants and their association with periodontal bacteria in patients with chronic periodontitis. Mediators Inflamm. 2019;2019:2061868. doi:10.1155/2019/2061868
16. Berglundh T, Armitage G, Araujo MG, et al. Peri-implant diseases and conditions: consensus report of workgroup 4 of the 2017 World Workshop on the classification of periodontal and peri-implant diseases and conditions. J Clin Periodontol. 2018;45 Suppl 20:S286–S91. doi:10.1111/jcpe.12957
17. Monje A, Vera M, Munoz-Sanz A, Wang HL, Nart J. Suppuration as diagnostic criterium of peri-implantitis. J Periodontol. 2021;92(2):216–224. doi:10.1002/JPER.20-0159
18. Simonis P, Dufour T, Tenenbaum H. Long-term implant survival and success: a 10–16-year follow-up of non-submerged dental implants. Clin Oral Implants Res. 2010;21(7):772–777. doi:10.1111/j.1600-0501.2010.01912.x
19. Stacchi C, Berton F, Perinetti G, et al. Risk factors for peri-implantitis: effect of history of periodontal disease and smoking habits. A systematic review and meta-analysis. J Oral Maxillofac Res. 2016;7(3):e3.
20. Zhou J, Zhao Y. Osteoprotegerin gene (OPG) Polymorphisms Associated with Peri-implantitis Susceptibility in a Chinese Han Population. Med Sci Monit. 2016;22:4271–4276. doi:10.12659/MSM.897592
21. Casado PL, Aguiar DP, Costa LC, et al. Different contribution of BRINP3 gene in chronic periodontitis and peri-implantitis: a cross-sectional study. BMC Oral Health. 2015;15(1):33. doi:10.1186/s12903-015-0018-6
22. Matsuo Y, Ochi N, Sawai H, et al. CXCL8/IL-8 and CXCL12/SDF-1alpha co-operatively promote invasiveness and angiogenesis in pancreatic cancer. Int J Cancer. 2009;124(4):853–861. doi:10.1002/ijc.24040
23. Wang S, Wu Y, Hou Y, et al. CXCR2 macromolecular complex in pancreatic cancer: a potential therapeutic target in tumor growth. Transl Oncol. 2013;6(2):216–225. doi:10.1593/tlo.13133
24. Ijichi H, Chytil A, Gorska AE, et al. Inhibiting Cxcr2 disrupts tumor-stromal interactions and improves survival in a mouse model of pancreatic ductal adenocarcinoma. J Clin Invest. 2011;121(10):4106–4117. doi:10.1172/JCI42754
25. Steele CW, Karim SA, Leach JDG, et al. CXCR2 inhibition profoundly suppresses metastases and augments immunotherapy in pancreatic ductal adenocarcinoma. Cancer Cell. 2016;29(6):832–845. doi:10.1016/j.ccell.2016.04.014
26. Viana AC, Kim YJ, Curtis KM, et al. Association of haplotypes in the CXCR2 gene with periodontitis in a Brazilian population. DNA Cell Biol. 2010;29(4):191–200. doi:10.1089/dna.2009.0919
27. Ferreira SD, Martins CC, Amaral SA, et al. Periodontitis as a risk factor for peri-implantitis: systematic review and meta-analysis of observational studies. J Dent. 2018;79:1–10. doi:10.1016/j.jdent.2018.09.010
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
