Back to Journals » Journal of Pain Research » Volume 15
Characterizing Fatigue Subtypes in Adolescents with Chronic Musculoskeletal Pain and Pain-Free Controls
Authors Boggero I , Valrie C , Morgan K, Hagiwara N, Kashikar-Zuck S , King C
Received 25 February 2022
Accepted for publication 8 July 2022
Published 26 July 2022 Volume 2022:15 Pages 2041—2049
DOI https://doi.org/10.2147/JPR.S363912
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Giorgio Veneziano
Ian Boggero,1,2 Cecelia Valrie,3,4 Krystal Morgan,5 Nao Hagiwara,3 Susmita Kashikar-Zuck,2,6 Christopher King2,6
1Department of Oral Health Science, Division of Orofacial Pain, University of Kentucky College of Dentistry, Lexington, KY, USA; 2Department of Pediatrics, University of Cincinnati College of Medicine, Cincinnati, OH, USA; 3Department of Psychology, Virginia Commonwealth University, Richmond, VA, USA; 4Institute for Inclusion, Inquiry, and Innovation, Virginia Commonwealth University, Richmond, VA, USA; 5Division of Transplant, University of North Carolina at Chapel Hill, Chapel Hill, NC, USA; 6Division of Behavioral Medicine and Clinical Psychology, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA
Correspondence: Ian Boggero, 740 S Limestone, Lexington, KY, 40536, USA, Tel +859-562-3291, Email [email protected]
Context: General fatigue, sleep-related fatigue, and cognitive fatigue are prevalent and disruptive in adults with chronic musculoskeletal (MSK) pain, but little is known about these fatigue subtypes in pediatric musculoskeletal pain.
Objective: To compare fatigue and its subtypes between adolescents with chronic MSK pain and pain-free controls and to test if fatigue subtypes were associated with concurrent pain and its impact (pain intensity, number of pain sites, pain interference, and functional disability) or experimental pain (intensity and tolerance) in adolescents with chronic MSK pain. Finally, we sought to explore adolescents’ qualitative characterizations of their fatigue.
Methods: Adolescents with chronic MSK pain (12– 17 y.o., n = 26) and pain-free controls (n = 26) completed validated self-report measures of fatigue, pain, and functional disability, underwent an experimental pain tolerance task (cold water immersion of the hand), and provided qualitative descriptions of their fatigue (pain group only).
Results: Adolescents with chronic MSK pain reported significantly greater general, sleep-related, and cognitive fatigue than pain-free controls (all p’s < 0.001). In adolescents with chronic MSK pain, fatigue subtypes were associated with clinical pain and pain impact (r’s = 0.43– 0.84) but not experimental pain measures (p’s > 0.05). Adolescents with chronic MSK pain qualitatively described the negative implications of the different fatigue subtypes, particularly when perceived as long-lasting.
Conclusion: This preliminary study suggests that fatigue subtypes are prevalent and impactful in pediatric patients with chronic MSK pain. When planning multi-disciplinary treatment for pediatric MSK pain, providers should recognize fatigue as another disabling symptom.
Keywords: disability, fatigue, pediatric, musculoskeletal pain, widespread bodily pain
Introduction
Approximately 5% of children and adolescents report experiencing debilitating chronic pain.1 This pain is often musculoskeletal in nature (MSK, eg, juvenile fibromyalgia, amplified widespread musculoskeletal pain, chronic lower back pain, and others) and is associated with worse psychosocial functioning, greater healthcare utilization, missed schooldays, and lower quality of life, among other negative outcomes.1 Fatigue, defined as a persistent overwhelming feeling of tiredness, is prevalent in patients with chronic MSK pain,2–5 including pediatric MSK pain patients.6,7 A meta-analysis of adolescents with juvenile idiopathic arthritis revealed that 60–76% of patients reported fatigue, with 25% reporting severe fatigue.8 Yet, much of what we know about fatigue and pain comes from adults, with limited studies in pediatric chronic pain. The most utilized assessment tool for pediatric fatigue is the Pediatric Quality of Life Multidimensional Fatigue Scale (PEDsQL-MFS) which consists of a total score and individual subtype scores of sleep-related fatigue (eg, feeling tired in the morning), general fatigue (eg, feeling too tired to do things), and cognitive/mental fatigue (eg, difficulty maintaining attention).9–14 In a heterogeneous sample of adolescents with chronic pain,14 cognitive fatigue was more strongly correlated to health related quality of life than were general or sleep-related fatigue, and in adults with chronic pain general fatigue was more strongly correlated to pain-related interference with daily activities than other fatigue subtypes.15,16 These findings suggest there may be specific relationships between fatigue subtypes and pain outcomes, but the PEDsQL-MFS has not yet been utilized to characterize fatigue in adolescents with chronic MSK pain or test how fatigue subtypes are related to different pain variables such as pain intensity, pain interference, disability, number of pain sites, or experimental pain outcomes. Learning about these associations is important because different fatigue subtypes may be indicative of differing underlying processes and may inform the development of targeted interventions for pain.
The current study had three aims. The first was to characterize general, sleep-related, and cognitive fatigue in adolescents with chronic MSK pain conditions and compare fatigue characteristics to age-matched pain-free controls. We hypothesized adolescents with chronic MSK pain would report a higher prevalence of fatigue than pain-free controls The second was to test if fatigue subtypes were associated with concurrent and experimental pain variables. We included both self-report and experimental pain variables to capture subjective and objective (eg, evoked responses to a standardized pain stimulus) aspects of pain. For experimental pain we chose a cold pressor task as it has been established as a safe and reliable measure to assess pain processing in children and adolescents.17 We hypothesized that fatigue subtypes would have unique relationships with both self-report and experimental pain variables.15,16 The third was to conduct an exploratory (ie, no a-priori hypotheses) qualitative analysis of adolescents’ narrative descriptions of their fatigue to enrich our understanding of the experience of fatigue beyond the quantitative measures. Although qualitative studies of fatigue in adults with chronic pain find that patients perceive fatigue as unpredictable, uncontrollable, multidimensional, and highly disruptive,17–19 no such studies exist in adolescents with chronic MSK pain.
Methods
Participants
Participants were recruited from a children’s hospital in the US Midwest from September 2019 to July 2020 via flyers posted around the hospital and telephone calls to previous pain research participants. Eligibility criteria for the chronic MSK pain group included having the ability to read/understand English, being aged 12–17 (inclusive), having a physician-confirmed diagnosis of chronic (>3 months) MSK pain (eg, juvenile fibromyalgia, amplified widespread pain, chronic lower back pain), and having a parent/caregiver report that adolescents’ experienced pain and disability over the past two weeks. Participants were excluded if they reported being pregnant, on opioids, or having a lifetime history of cancer, cardiovascular disorder, Raynaud’s disease, lupus, developmental abnormalities, schizophrenia, bipolar disorder, or seizures. The pain-free control group had to be absent of any lifetime history of chronic pain and had to have a parent report no pain or disability in the last two weeks. Control participants were matched by sex and age (± 1 year) to participants in the pain group.
Procedures
Data for this study are a subset of a larger study examining correlates of pediatric MSK pain. Interested participants were screened via a phone conversation with their parent/s to confirm eligibility. If eligible, parents and participants completed an in-person visit where they provided assent/consent. Then, parents were escorted to a waiting area to avoid biasing participants’ responses. Participants completed questionnaires via REDcap with a trained research staff member available to answer questions. Then, participants underwent an experimental task where they submerged their hand in cold water (10°C) to assess pain intensity and tolerance (how long they were able to keep their hand submerged).20 After 20 seconds and immediately after withdrawing their hand, participants provided a verbal numeric rating scale (NRS) of pain intensity (0=“No Pain”, 10=“The worst pain imaginable”). Unbeknownst to the participant, there was a 5-minute limit on the task. Participants were compensated $50 for completing the study. Procedures were approved by the IRB (#2019-0698) and complied with the Declaration of Helsinki.
Materials
Demographics
Participants reported their age, sex, race, and ethnicity.
Fatigue
The PEDsQL-MFS was used to assess fatigue subtypes.9 The PEDsQL-MFS evaluates the extent to which 18 symptoms (α=0.96) have been problematic over the last month (0=“Almost always”, 100=“Never”). Higher scores indicated lower fatigue. Three subscales were computed: General fatigue (6 items, α=0.93), sleep-related fatigue (6 items, α=0.87), and mental/cognitive fatigue (6 items, α=0.95). A structured fatigue interview questionnaire21 (Appendix 1) assessed fatigue prevalence and qualitative descriptors. Participants were presented a definition of fatigue and asked whether they experienced fatigue (Yes/No). If they answered “No”, they were not asked further questions. If they answered “Yes”, they were asked to type what fatigue felt like using an open text box, rate the severity of their fatigue in the past month (1=“No fatigue” to 10=“Extremely fatigued”) and describe the temporal pattern of fatigue (chronic or episodic).
Pain
Participants were asked to list their pain diagnosis. At the start of the lab session, participants verbally reported their current bodily pain intensity using a numeric rating scale (NRS, 0=“Not at all”, 10=“Worst pain imaginable”). Participants also reported average pain intensity over the past two weeks using the same NRS.22 Pain interference was assessed using the 8-item PROMIS pediatric pain interference scale (1=“Never” to 5=“Almost always”).23 A total score was computed by summing all items (α=0.86). The number of pain sites was assessed using a body map of 18 body sites on which participants indicated whether they had experienced pain over the past three months. A total score was computed by summing marked sites (0–18).24 Cold pain intensity was computed by averaging the two NRS ratings obtained during the hand submersion task. Cold pain tolerance was operationalized as the time (in seconds) that participants kept their hand submerged.
Disability
Functional disability was assessed using the Functional Disability Inventory.25 Responses to all 15 items (0=“No trouble”, 5=“Impossible”) were summed into a total score (α=92), with higher numbers indicating greater disability.
Data Analysis
Power was based on correlations between fatigue subtypes and pain interference in adults with chronic pain (r=0.37 for the smallest of these correlations).15 A sample of 55 would provide >80% power to detect similar correlations. We conservatively sought to recruit n=30 in both the pain and control groups. Due to the COVID-19 shutdown in March 2020, we obtained n=26 in each group, providing >80% power to detect r≥.38.
The data did not contain outliers (± 3 SD from the mean) and all variables were approximately normally distributed (± 1.5 kurtosis). For Aim 1, we computed descriptive statistics. Effect sizes were computed using Hedges’ g.26 For Aim 2, correlations were computed using only data from the chronic MSK pain group. Linear regressions were then used, with all three fatigue subtypes entered as simultaneous predictors for each pain variable. Age and sex were analyzed as covariates in all models but were not significant and were thus removed to preserve power. Analyses were run on SPSS Version 27 (IBM Corp., Armonk, NY).
For exploratory Aim 3, qualitative responses from the structured fatigue interview were examined. A co-author (NH) and a research assistant unitized thought units from all 24 written responses (n=2 in the chronic MSK group did not report fatigue). From these thought units, themes were identified, refined, and organized into higher-level categories by consulting with a co-author (CV) whose expertise is in pain and fatigue research. Data were then coded independently using a codebook created for the study by two research assistants who met with NH to resolve discrepancies. Codes were quantified by the number of adolescents who mentioned a given theme. Because approximately half of the participants in the chronic MSK pain group reported fatigue as chronic (n=13) vs episodic (n=11), we analyzed the qualitative data separately for these groups.
Results
Clinical Description
Approximately 31% of parents of participants in the chronic MSK pain group rated their child’s pain over the last two weeks as mild, 46% as moderate, and 23% as severe. The most common pain diagnoses were Ehlers Danlos Syndrome, juvenile fibromyalgia, and widespread musculoskeletal pain (Table 1). The average duration of pain was 40.90 months (SD=39.78 months, range=4–144 months).
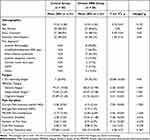 |
Table 1 Demographic Information and Descriptive Statistics for Fatigue and Pain Variables |
Aim 1: Prevalence/Intensity of Fatigue Between Participants with MSK Pain and Controls
Those in the chronic MSK pain group reported significantly greater fatigue and fatigue subtypes than age- and sex-matched pain-free controls (Table 1). Effect sizes ranged between Hedges g=1.25–1.47, with the largest difference being in general fatigue. Based on the structured fatigue interview, 92.3% (n=24) of the chronic MSK pain group reported fatigue versus 26.9% (n=7) in the control group (X2=23.08, p<0.001). Those who reported fatigue rated it as low- to moderate intensity in the pain-free control group (n=7, M=4.43, SD=1.34) and moderate- to high-intensity in the chronic MSK pain group (n=24, M=6.67, SD=1.58). Only one participant in the control group reported chronic fatigue, compared to 13 in the MSK pain group.
Aim 2: Relations of Fatigue Subtypes with Pain Variables
Fatigue subtypes were moderately intercorrelated (r’s=0.42-0.72; Table 2). General fatigue was correlated with all clinical pain variables, whereas correlations between cognitive/sleep-related fatigue and pain variables were dependent on the specific association examined. None of the subtypes were associated with experimental pain outcomes.
 |
Table 2 Descriptive Statistics and Bivariate Correlations Among Fatigue Subtypes and Pain Variables in the Chronic MSK Pain Group Only (n = 26) |
Linear regression analyses indicated that greater general fatigue (controlling for cognitive and sleep-related fatigue) was associated with worse disability and higher pain interference (Table 3). Sleep-related fatigue was also associated with higher disability, controlling for other subtypes. When all three subtypes were entered together, they explained 60% of the variance in pain interference and 76% of the variance in functional disability.
 |
Table 3 Associations of Fatigue Subtypes with Pain Variables, Controlling for Other Fatigue Subtypes in Chronic MSK Pain Group Only (n=26) |
Exploratory Aim 3: Qualitative Descriptions of Fatigue
Table 4 summarizes the frequency of themes mentioned by the participants with MSK pain. Three higher-order themes were identified: description, manifestation, and impact of fatigue. When describing fatigue, most adolescents with MSK pain described fatigue as feeling “tired” or “worn down.” Those who reported chronic fatigue (n=13) tended to highlight the pervasive nature of their symptoms (eg, “I feel like I’m exhausted and took 20 exams at once 24/7” and “[I]t’s like a heavy blanket that is always on you”). There were three sub-themes within the manifestation theme: general, cognitive, and sleep-wake. Five adolescents mentioned general manifestations of fatigue (eg, “I just can’t function or keep it together”). Additionally, five mentioned cognitive manifestations (eg, “[I] have trouble thinking.”). Finally, half of the adolescents identified sleep-wake manifestations (eg, “[I] always feel like I need a nap”). More adolescents in the chronic (vs episodic) group reported manifestations of fatigue across all three sub-themes. Adolescents in the chronic fatigue group stated fatigue interfered with their performance in school-related or daily activities whereas those in the episodic group mentioned more not finishing or wanting to do more activities.
 |
Table 4 Joint Display of Episodic and Chronic Fatigue Themes Endorsed by Participants with Chronic MSK Pain |
Discussion
Fatigue remains poorly characterized in pediatric chronic MSK pain. We found that over 90% of participants with chronic MSK pain reported fatigue, and they rated it as moderate/severe in intensity. These results corroborate what has been found in other pediatric MSK pain populations8,27 and suggest that fatigue is at least – if not more – prevalent and intense in adolescents with chronic pain than in adults with chronic pain. Our study extends these findings by highlighting that fatigue in pediatric chronic MSK pain appears to be multidimensional, and that fatigue subtypes (particularly general fatigue) were robustly related to specific clinical pain variables and to daily function – a finding that is strongly consistent with the adult chronic pain literature.15,16 All three fatigue subtypes were more strongly correlated to variables of poor pain-related functioning (ie, pain interference, disability) than to variables relating to the experience of pain (intensity, number of pain sites), suggesting that fatigue may affect how people function with pain more than how they experience it.
Moreover, fatigue in this population appears to have a temporal component, with over half of participants reporting it as chronic. Results from the qualitative components of the study suggest participants described fatigue symptoms as general, sleep-related, or cognitive. This consistency is particularly striking because these descriptions were completed before participants completed the PEDsQL-MFS to avoid biasing their responses. Our qualitative data also suggest that participants who report chronic versus episodic fatigue differ in their experiences of fatigue symptoms. No existing quantitative fatigue measures consider this distinction, and future work should determine how to best assess temporal components of fatigue in chronic pain.
Interestingly, none of the subtypes were associated with experimental pain outcomes, indicating that experimental pain may be driven by factors other than fatigue. Fatigue may influence people’s ability to function with pain (hence, associations between fatigue and health-related quality of life, pain interference, and disability [eg, 14–16]) and not people’s actual experience of pain intensity.28 It is also possible that other experimental pain paradigms may be more sensitive to fatigue effects than the cold pressor task. For example, fatigue might impact how the central nervous system modulates nociceptive information and may be better assessed via temporal summation or conditioned pain modulation paradigms. These possibilities should be formally tested.
The current study has limitations. The small sample was heterogeneous and may not generalize to more specific (eg, juvenile fibromyalgia only) or broader (ie, all chronic pain) populations. We were underpowered to assess if the relationships among fatigue subtypes and pain outcomes were condition specific. The study did not control for medication use or pain duration. Because patients were recruited from a hospital setting and required a physician-confirmed pain diagnosis, adolescents who did not seek medical care were not represented. Results need to be replicated with a larger and more representative sample.
The study also has considerable strengths. A matched design was used to control for demographic factors that have been linked to fatigue. The use of quantitative, qualitative, and experimental pain data in this preliminary investigation lays the foundation for more comprehensive studies to examine fatigue in pediatric chronic MSK pain. Eventually, a better understanding of fatigue and its subtypes may lead to more effective multi-disciplinary pain management.
Key Message
General, cognitive, and sleep-related fatigue were positively associated with bodily pain intensity, pain interference, functional disability, and the number of pain sites. Adolescents with MSK pain described their fatigue as problematic. Providers, teachers, and family members should recognize fatigue as another disabling symptom when working with adolescents with chronic MSK pain.
Acknowledgments
The authors would like to acknowledge Hannah Pickerill for her instrumental role in collecting the data and running the study visits. The authors would also like to thank all the participants and their families for dedicating their time to completing the research project.
Funding
This study was funded by an internal grant (Arnold Strauss Award) awarded to the first author at Cincinnati Children’s Hospital Medical Center. The CCTST at the University of Cincinnati is funded by the National Institutes of Health (NIH) Clinical and Translational Science Award (CTSA) program, grant 2UL1TR001425-05A1. The first author was also supported as a University of Kentucky DREAMS Scholar by the NIH National Center for Advancing Translational Sciences (UL1TR001998).The content is solely the authors’ responsibility and does not necessarily represent the official views of the NIH.
Disclosure
The authors declare no conflicts of interest.
References
1. Huguet A, Miró J. The severity of chronic pediatric pain: an epidemiological study. J Pain. 2008;9(3):226–236. doi:10.1016/j.jpain.2007.10.015
2. Creavin ST, Dunn K, Mallen CD, Nijrolder I, van der Windt DA. Co-occurrence and associations of pain and fatigue in a community sample of Dutch adults. Europe J Pain. 2010;14(3):327–334. doi:10.1016/j.ejpain.2009.05.010
3. Eccles JA, Davies KA. The challenges of chronic pain and fatigue. Clin Med. 2021;21(1):19–27. doi:10.7861/clinmed.2020-1009
4. Clauw DJ, Chrousos GP. Chronic pain and fatigue syndromes: overlapping clinical and neuroendocrine features and potential pathogenic mechanisms. Neuroimmunomod. 1997;4(3):134–153. doi:10.1159/000097332
5. Boggero IA, Kniffin TC, de Leeuw R, Carlson CR. Fatigue mediates the relationship between pain interference and distress in patients with persistent orofacial pain. J Oral Facial Pain Head. 2014;28(1):38–45. doi:10.11607/jop.1204
6. Sturgeon JA, Darnall BD, Kao MC, Mackey SC. Physical and psychological correlates of fatigue and physical function: a Collaborative Health Outcomes Information Registry (CHOIR) study. J Pain. 2015;16(3):291–298. doi:10.1016/j.jpain.2014.12.004
7. Boggero IA, Rojas-Ramirez MV, de Leeuw R, Carlson CR. Satisfaction with life in orofacial pain disorders: associations and theoretical implications. J Oral Facial Pain Head. 2016;30(2):99–106. doi:10.11607/ofph.1526
8. Armbrust W, Siers NE, Lelieveld OT, et al. Fatigue in patients with juvenile idiopathic arthritis: a systematic review of the literature. Sem Arthritis Rheum. 2016;45(5):587–595. doi:10.1016/j.semarthrit.2015.10.008
9. Varni JW, Burwinkle TM, Szer IS. The PedsQL Multidimensional Fatigue Scale in pediatric rheumatology: reliability and validity. J Rheum. 2004;31(12):2494–2500.
10. Varni JW, Burwinkle TM, Katz ER, Meeske K, Dickinson P. The PedsQL in pediatric cancer: reliability and validity of the pediatric quality of life inventory generic core scales, multidimensional fatigue scale, and cancer module. Cancer. 2002;94(7):2090–2106. doi:10.1002/cncr.10428
11. Varni JW, Limbers CA, Bryant WP, Wilson DP. The PedsQL Multidimensional Fatigue Scale In pediatric obesity: feasibility, reliability and validity. Int J Ped Obesity. 2010;5(1):34–42. doi:10.3109/17477160903111706
12. Varni JW, Limbers CA, Bryant WP, Wilson DP. The PedsQL Multidimensional Fatigue Scale in type 1 diabetes: feasibility, reliability, and validity. Ped Diabetes. 2009;10(5):321–328. doi:10.1111/j.1399-5448.2008.00482.x
13. Panepinto JA, Torres S, Bendo CB, et al. PedsQL Multidimensional Fatigue Scale in sickle cell disease: feasibility, reliability, and validity. Ped Blood Cancer. 2014;61(1):171–177. doi:10.1111/j.1399-5448.2008.00482.x
14. Gold JI, Mahrer NE, Yee J, Palermo TM. Pain, fatigue and health-related quality of life in children and adolescents with chronic pain. Clin J Pain. 2009;25(5):407–412. doi:10.1097/AJP.0b013e318192bfb1
15. Boggero IA, Rojas-Ramirez MV, Carlson CR. All fatigue is not created equal: the association of fatigue and its subtypes on pain interference in orofacial pain. Clin J Pain. 2017;33(3):231–237. doi:10.1097/AJP.0000000000000391
16. Boggero IA, Rojas-Ramirez MV, King CD. Cross-sectional associations of fatigue subtypes with pain interference in younger, middle-aged, and older adults with chronic orofacial pain. Pain Med. 2020;21(9):1961–1970. doi:10.1093/pm/pnaa092
17. Birnie KA, Petter M, Boerner KE, Noel M, Chambers CT. Contemporary use of the cold pressor task in pediatric pain research: a systematic review of methods. J Pain. 2012;13(9):817–826. doi:10.1016/j.jpain.2012.06.005
18. Velasco-Furlong L, Gutiérrez-Hermoso L, Mateos-Pintado B, et al. The 4 U’s rule of fibromyalgia: a proposed model for fatigue in a sample of women with fibromyalgia: a qualitative study. Int J Environ Res Public Health. 2020;17(17):6224. doi:10.3390/ijerph17176224
19. Grape HE, Solbrække KN, Kirkevold M, Mengshoel AM. Tiredness and fatigue during processes of illness and recovery: a qualitative study of women recovered from fibromyalgia syndrome. Physiother Theory Pract. 2017;33(1):31–40. doi:10.1080/09593985.2016.1247933
20. Jaime-Lara RB, Koons BC, Matura LA, Hodgson NA, Riegel B. A qualitative metasynthesis of the experience of fatigue across five chronic conditions. J Pain Symptom Manage. 2020;59(6):1320–1343. doi:10.1016/j.jpainsymman.2019.12.358
21. Trout K. Multidimensional Conceptualization and Assessment of Fatigue in Pediatric Sickle Cell Disease: Impact of Fatigue on Quality of Life. Unpublished Doctoral Dissertation. East Carolina University; 2018.
22. Salamon KS, Davies WH, Fuentes MR, Weisman SJ, Hainsworth KR. The pain frequency-severity-duration scale as a measure of pain: preliminary validation in a pediatric chronic pain sample. Pain Res Treat. 2014;1–6. doi:10.1155/2014/653592
23. Amtmann D, Cook KF, Jensen MP, et al. Development of a PROMIS item bank to measure pain interference. Pain. 2010;150(1):173–182. doi:10.1016/j.pain.2010.04.025
24. Ting TV, Barnett K, Lynch-Jordan A, et al. 2010 American College of Rheumatology adult fibromyalgia criteria for use in an adolescent female population with juvenile fibromyalgia. J Pediatrics. 2016;169:181–187. doi:10.1016/j.jpeds.2015.10.011
25. Walker LS, Greene JW. The functional disability inventory: measuring a neglected dimension of child health status. J Ped Psycholo. 1991;16(1):39–58. doi:10.1093/jpepsy/16.1.39
26. Rosenthal R, Cooper H, Hedges L. Parametric measures of effect size. Handb Res Synth. 1994;621(2):231–244.
27. Yoon IA, Sturgeon JA, Feinstein AB, Bhandari RP. The role of fatigue in functional outcomes for youth with chronic pain. Euro J Pain. 2019;23(8):1548–1562. doi:10.1002/ejp.1431
28. Boggero IA, Segerstrom SC. Self‐regulatory ability, fatigue, and the experience of pain: mechanistic insights from pain‐free undergraduates. Psychophys. 2019;56(9):e13388. doi:10.1111/psyp.13388
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
