Back to Journals » Infection and Drug Resistance » Volume 13
Characterization of an IMP-4-Producing Klebsiella pneumoniae ST1873 Strain Recovered from an Infant with a Bloodstream Infection in China
Authors Xu J, Lin W, Chen Y, He F
Received 26 January 2020
Accepted for publication 23 February 2020
Published 9 March 2020 Volume 2020:13 Pages 773—779
DOI https://doi.org/10.2147/IDR.S247341
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Sahil Khanna
Juan Xu, 1,* Wenping Lin, 2,* Yanmin Chen, 3 Fang He 3
1Institute of Hygiene, Zhejiang Academy of Medical Sciences, Hangzhou Medical College, Hangzhou, Zhejiang 310013, People’s Republic of China; 2Centers for Disease Control and Prevention of Ningbo, Ningbo, Zhejiang 315010, People’s Republic of China; 3Department of Clinical Laboratory, Zhejiang Provincial People’s Hospital, People’s Hospital of Hangzhou Medical College, Hangzhou, Zhejiang 310014, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Fang He Tel/Fax +86-571-8821-5596
Email [email protected]
Purpose: Imipenemase (IMP), an Ambler class B metallo-β-lactamase, is an important carbapenemase that confers resistance to almost all β-lactams. In this study, we characterized the genomic feature of an IMP-4-producing Klebsiella pneumoniae ST1873 strain, a rare sequence type (ST) isolated from an infant with a bloodstream infection in China.
Patients and Methods: K. pneumoniae strain, BKP19, was collected from a bloodstream infection in an infant who was hospitalized at the department of paediatrics. The whole genome sequence of the strain was sequenced using the Illumina NovaSeq 6000 platform and long-read MinION sequencer. Multilocus sequence typing, antimicrobial resistance gene identification, plasmid and phylogenetic relationship analysis of the strain were analysed by various bioinformatics approaches.
Results: K. pneumoniae BKP19 was resistant to multiple antimicrobials, including carbapenems. Eleven antimicrobial resistance genes corresponding to beta-lactam resistance, quinolone resistance, phenicol resistance and fosfomycin resistance could be identified in the genome. The carbapenem resistance gene blaIMP-4 was located in an IS26-associated class 1 integron of an IncN-type plasmid with 39,033 bp (pIMP-4-BKP19). Sequence alignment revealed that pIMP-4-BKP19 is closely related to the common plasmid carrying IMP-4 in K. pneumoniae (pIMP-HZ1-like plasmid) but is smaller, lacking the quinolone resistance gene qnrS1 and multiple tra gene orthologs. Conjugation experiment revealed that pIMP-4-BKP19 is a non-conjugative plasmid. According to in silico MLST analysis, K. pneumoniae strain BKP19 belongs to a sporadic clone ST1873.
Conclusion: In summary, our study reports the first genome sequence of a K. pneumoniae ST1873 strain harbouring the class B β-lactamase blaIMP-4 in an IncN-type plasmid recovered from an infant with a bloodstream infection in China. Considering the global emergence of IMP-4 carbapenemase, more attention must be paid to prevent its future prevalence.
Keywords: Klebsiella pneumoniae, blaIMP-4, IncN plasmid, ST1873, bloodstream infection
Introduction
Klebsiella pneumoniae is an important pathogen of the Enterobacteriaceae family that causes a variety of infectious diseases, including pneumonia, liver abscesses, urinary tract infections and bacteraemia. The emergence of carbapenem-resistant K. pneumoniae (CRKP) leaving few therapeutic options available. Imipenemase (IMP), an Ambler class B metallo-β-lactamase, is an important carbapenemase that confers resistance to almost all β-lactams. One of the most commonly observed IMP variants is IMP-4, which was firstly detected in Acinetobacter spp. in Hong Kong in 2001.1 Since then, IMP-4-type carbapenemases have spread globally.2–5
The blaIMP-4 gene is often integrated in broad-host-range conjugative plasmids and is transferred between different Gram-negative bacilli (eg, Enterobacteriaceae, Acinetobacter spp., Pseudomonas aeruginosa).1,5–8 The horizontal transfer of blaIMP-4 in these plasmids is frequently associated with class 1 integrons.9,10 Plasmid-borne blaIMP-4 has been sporadically reported in different Gram-negative bacilli in China.6,11–13 However, only a few studies have reported the complete sequence of blaIMP-4-harbouring plasmids,6,10,14 which limits our understanding of the transmission mechanism of blaIMP-4 between different Gram-negative bacilli.
Klebsiella pneumoniae carbapenemase (KPC) has emerged as the predominant carbapenemase in K. pneumoniae in China, while there are relatively few IMP-4 producing strains.15 Carbapenemase IMP is often distributed among multiple STs in K. pneumoniae, especially some rare STs.
In this study, the IMP-4-producing K. pneumoniae strain BKP19 was collected from a bloodstream infection in an infant who was hospitalized at the department of paediatrics. The isolate was preliminarily identified using the VITEK MS system (bioMérieux, France) and was further confirmed by 16S rRNA gene sequencing. The whole genome of the strain was sequenced. The blaIMP-4-harbouring plasmid and genetic characteristics of the strain were analysed to gain a better understanding of the transmission mechanism of blaIMP-4.
Materials and Methods
Patient and Isolate
A female neonate with a birth weight of 1.13 kg was hospitalized at the department of paediatrics half an hour after preterm delivery at a tertiary hospital in Hangzhou, Zhejiang Province, China. During her hospitalization, the neonate received multiple antimicrobial treatments, including cefotaxime, erythromycin, vancomycin and meropenem. Carbapenem-resistant K. pneumoniae was isolated from a blood sample from the patient one month later after her hospitalization. The isolate was preliminarily identified using the VITEK MS system (bioMérieux, France) and was further confirmed by 16S rRNA gene sequencing.
Antimicrobial Susceptibility Test
Antimicrobial susceptibility testing was conducted using the VITEK 2 system (bioMérieux, France) with Gram-negative antimicrobial susceptibility testing cards (AST-GN16) and the Etest method following the guidelines of the Clinical and Laboratory Standards Institute (CLSI). Antimicrobial susceptibility was determined using the breakpoints approved by the CLSI.16
Whole-Genome Sequencing
The genomic DNA of the isolate was extracted using a QIAamp DNA Mini Kit (Qiagen, USA). The Illumina NovaSeq 6000 platform (Illumina Inc., San Diego, CA, USA) and a long-read MinION sequencer (Nanopore, Oxford, UK) were used for whole-genome sequencing. The de novo hybrid assembly of both short Illumina reads and long MinION reads were performed using Unicycler.17 The whole-genome sequence was automatically annotated by the NCBI Prokaryotic Genome Annotation Pipeline (PGAP) server.
Multilocus Sequence Typing and Antimicrobial Resistance Gene Identification
Multilocus sequence typing (MLST) and the identification of antimicrobial resistance genes and plasmid replicons were performed using the BacWGSTdb server.18
Plasmid Analysis
The graphical circular map of the blaIMP-4-carrying plasmid was converted by the CGView Server.19 The comparisons between the blaIMP-4-carrying plasmid and similar plasmids were conducted by using the BLAST Ring Image Generator (BRIG) in concentric rings.20 The comparison of the blaIMP-4-carrying plasmid with the most closely related plasmid was performed by EasyFig 2.2.3.21
Conjugation Experiment
The transfer capacity of the blaIMP-4-harbouring plasmid was investigated in a conjugation experiment.22 Rifampicin-resistant E. coli EC600 was used as the recipient, and strain BKP19 was used as the donor. The donor and recipient bacteria were cultured in MH broth for 4 hrs. Aliquots of 100 μL of each cultured donor and recipient bacterium were mixed together. A 40 μL aliquot of the mixture was spotted on a sterile filter membrane, which was placed on a Muller-Hinton (MH) agar plate, followed by incubation at 35°C for 18 h. The bacteria were washed from the filter membrane, and blaIMP-4-positive E. coli transconjugants were selected on MH agar plates supplemented with rifampicin (800 mg/L) and imipenem (8 mg/L).
Phylogenetic Analysis
The phylogenetic relationship between BKP19 and other K. pneumoniae strains retrieved from the NCBI GenBank database was analysed using the BacWGSTdb server.18,23 The BacWGSTdb server offers core genome Multilocus Sequence Typing (cgMLST) and single nucleotide polymorphism (SNP) approaches to investigate the phylogenetic relationship of the uploaded genome sequence with sequences deposited in the database. The database currently contains 7480 K. pneumoniae strains.
Nucleotide Sequence Accession Numbers
The results of this whole-genome shotgun project have been deposited at DDBJ/EMBL/GenBank under accession number VWRO00000000. The version described in this paper is the first version.
Ethical Approval
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of Zhejiang Provincial People’s Hospital. Written informed consent from the patient was exempted by the Ethics Committee of Zhejiang Provincial People’s Hospital because the present study only focused on bacteria. The clinical isolate K. pneumoniae BKP19 was part of the routine hospital laboratory procedure.
Results and Discussion
The MICs of the antibiotics tested are presented in Table 1. K. pneumoniae BKP19 was resistant to multiple antimicrobials, including cefazolin, ceftriaxone, cefepime, cefoxitin, imipenem, meropenem, ciprofloxacin and levofloxacin. This strain was susceptible to aminoglycosides, aztreonam, tigecycline and colistin.
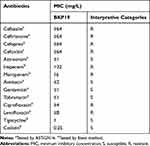 |
Table 1 MICs of the Antibiotics Tested in K. pneumoniae BKP19 |
The genome of K. pneumoniae strain BKP19 consists of five contigs that comprise 5,600,093 bp. Among them, contig 1 (2,265,448 bp), contig 2 (1,983,649 bp) and contig 3 (1,049,807 bp) belong to the chromosome, and the others belong to two plasmids (contig 4: 262,156 bp and contig pIMP-4-BKP19: 39,033 bp). The PGAP server predicted a total of 5,262 protein-coding sequences, 88 tRNA genes and 25 rRNA operons. Three plasmid replicons were identified: IncFIB(K) and IncHI1B on plasmid 4 and IncN on plasmid pIMP-4-BKP19.
The antimicrobial resistance genes present in the genome of the isolate are presented in Table 2. We identified the aminoglycoside resistance genes aph(6)-Id and strA; the beta-lactam resistance genes blaSHV-2, blaSHV-11 and blaIMP-4; the quinolone resistance genes oqxA and oqxB; the phenicol resistance gene catA1; the sulphonamide resistance gene sul2; the trimethoprim resistance gene dfrA5 and the fosfomycin resistance gene fosA. blaSHV-2, oqxA, oqxB and fosA were located in the chromosome. aph(6)-Id, strA, blaSHV-11, catA1, dfrA5 and sul2 were located in plasmid 4. The carbapenem-resistant gene blaIMP-4 was located in plasmid pIMP-4-BKP19.
 |
Table 2 Antimicrobial Resistance Genes in K. pneumoniae BKP19 |
pIMP-4-BKP19 is an IncN-type plasmid that comprises 39,033 bp. The circular map of pIMP-4-BKP19 is presented in Figure 1. It contains conserved IncN-type backbone regions that contain a replication gene and its accessory structure for plasmid replication. The tra genes (traB, traK and traM) for conjugal transfer, the stbABC operon for plasmid maintenance, the ardA, ardK and ardR genes with an antirestriction function and the mucAB operon for UV protection were identified in the plasmid backbone. The blaIMP-4 gene was located in an IS26-associated class 1 integron, preceded by IS26-intI1 in the upstream region and followed by another IS26 sequence in the downstream region. The similarity of pIMP-4-BKP19 to other blaIMP-4-carrying plasmids was analysed with the Basic Local Alignment Search Tool (BLASTN). Several similar blaIMP-4-carrying plasmids were found in the NCBI GenBank database (Figure 2). The most common type of plasmid carrying IMP-4 in K. pneumoniae that has been reported to date is a pIMP-HZ1-like IncN-type plasmid with a size of approximately 50 kb (eg, K. pneumoniae strain Kp1 plasmid pIMP-HZ1, accession no KU886034, 51,599 bp; K. pneumoniae strain 24,854 plasmid p24854-IMP, accession no. MH909341, 51,393bp),14 these plasmids also carry the quinolone resistance gene qnrS1. The structural characteristics of pIMP-4-BKP19 compared to pIMP-HZ1 and p24854-IMP are presented in Figure 3. The structure of the pIMP-4-BKP19 plasmid is very similar to these two plasmids, with >99% query coverage and >99% nucleotide identity, but pIMP-4-BKP19 is smaller than the other plasmids (only 39,033 bp). There are three major genetic differences between the backbones of pIMP-4-BKP19 and the pIMP-HZ1-like plasmids. First, a segment downstream of blaIMP-4 is shortened and reversed, with an IS26 mobile element occurring on each side of the segment. The reduced sequence mainly includes genes encoding the tra gene orthologs (traC, traE, traF and traG). Second, the quinolone resistance gene qnrS1 is absent. There are insertion elements on both sides of the qnrS1 gene in the pIMP-HZ1-like plasmid. It is likely that the qnrS1 gene was introduced into the IncN plasmid through these insertion elements. Third, some nucleotide sequences downstream of ISKpn19 are absent. Conjugation experiment revealed that pIMP-4-BKP19 is a non-conjugative plasmid.
 |
Figure 1 Backbone structure of the blaIMP-4-encoding plasmid pIMP-4-BKP19. |
According to the in silico MLST analysis, K. pneumoniae strain BKP19 belongs to sequence type (ST) 1873, which is a very rare ST. IMP often appears in some rare STs (eg, ST476, ST2270, ST37, ST107, ST133, ST323, ST686, ST1114) in K. pneumoniae.6,10,12,24 We analysed the genome data in the NCBI GenBank database (accessed on 10 December 2019) and found that no ST1873 K. pneumoniae sequences are currently available in the database. We then further analysed the similar isolates with the threshold of 2000 (based on the cgMLST strategy) in BacWGSTdb. Fifteen phylogenetically related K. pneumoniae strains could be found in the database (Table S1). The strain closest to BKP19 was K. pneumoniae PN089E1 (ST2958) isolated from Cameroon in 2016 with 1610 different alleles.
Here, we report the first genome sequence of a K. pneumoniae ST1873 strain harbouring the class B β-lactamase blaIMP-4 recovered from an infant with a bloodstream infection in China. Comprehensive analysis of the blaIMP-4-carrying plasmid revealed that it was an IncN-type plasmid that has variant region within the integron mediated by IS26. Plasmids belonging to the IncN type commonly exhibit a broad host range and high transmission efficiency.6 It seems that the IS26-associated class 1 integron contributes to the dissemination of IMP-4 in different plasmids and that the IS26 mobile element plays an important role in the recombination of plasmid backbones. Our data may help to understand the genomic features of this bacterial pathogen. The genome sequence of K. pneumoniae BKP19 can be used as a reference sequence for comparative genomic analysis to obtain a better understanding on the transmission mechanism of blaIMP-4.
Conclusion
Our study reports the first genome sequence of a K. pneumoniae ST1873 strain harbouring the class B β-lactamase blaIMP-4 in a IncN-type plasmid recovered from an infant with a bloodstream infection in China. Considering the global emergence of IMP-4 carbapenemase, more attention must be paid to prevent its future prevalence.
Acknowledgments
This study was supported by grants from the National Natural Science Foundation of China (81702042), Natural Science Foundation of Zhejiang Province (LQ19H200003) and the Zhejiang Provincial Medical and Health Science and Technology plan (2018KY344 and 2019KY311).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Chu YW, Afzal-shah M, Houang ET, et al. IMP-4, a novel metallo-beta-lactamase from nosocomial Acinetobacter spp. collected in Hong Kong between 1994 and 1998. Antimicrob Agents Chemother. 2001;45(3):710–714. doi:10.1128/AAC.45.3.710-714.2001
2. Lee JH, Bae IK, Lee CH, Jeong S. Molecular characteristics of first IMP-4-producing enterobacter cloacae sequence type 74 and 194 in Korea. Front Microbiol. 2017;8:2343. doi:10.3389/fmicb.2017.02343
3. Lee JH, Lee CH, Bae IK. Emergence of IMP-4-producing enterobacter aerogenes clinical isolate. Clin Lab. 2018;64(7):1323–1326. doi:10.7754/Clin.Lab.2018.180211
4. Ghaith DM, Zafer MM, Ismail DK, et al. First reported nosocomial outbreak of Serratia marcescens harboring bla IMP-4 and bla VIM-2 in a neonatal intensive care unit in Cairo, Egypt. Infect Drug Resist. 2018;11:2211–2217. doi:10.2147/IDR.S174869
5. Espedido BA, Partridge SR, Iredell JR. bla(IMP-4) in different genetic contexts in Enterobacteriaceae isolates from Australia. Antimicrob Agents Chemother. 2008;52(8):2984–2987. doi:10.1128/AAC.01634-07
6. Feng W, Zhou D, Wang Q, et al. Dissemination of IMP-4-encoding pIMP-HZ1-related plasmids among Klebsiella pneumoniae and Pseudomonas aeruginosa in a Chinese teaching hospital. Sci Rep. 2016;6:33419. doi:10.1038/srep33419
7. Dolejska M, Papagiannitsis CC. Characterization of the complete nucleotide sequences of IMP-4-encoding plasmids, belonging to diverse inc families, recovered from enterobacteriaceae isolates of wildlife origin. Antimicrob Agents Chemother. 2018;62(5).
8. Abraham S, O’dea M, Trott DJ, et al. Isolation and plasmid characterization of carbapenemase (IMP-4) producing salmonella enterica typhimurium from cats. Sci Rep. 2016;6:35527. doi:10.1038/srep35527
9. Roy Chowdhury P, Ingold A, Vanegas N, et al. Dissemination of multiple drug resistance genes by class 1 integrons in Klebsiella pneumoniae isolates from four countries: a comparative study. Antimicrob Agents Chemother. 2011;55(7):3140–3149. doi:10.1128/AAC.01529-10
10. Zhou K, Yu W, Shen P, et al. A novel Tn1696-like composite transposon (Tn6404) harboring bla IMP-4 in a Klebsiella pneumoniae isolate carrying a rare ESBL gene bla SFO-1. Sci Rep. 2017;7(1):17321. doi:10.1038/s41598-017-17641-2
11. Wang J, Yuan M, Chen H, et al. First report of klebsiella oxytoca strain simultaneously producing NDM-1, IMP-4, and KPC-2 carbapenemases. Antimicrob Agents Chemother. 2017;61(9). doi:10.1128/AAC.00877-17.
12. Ho PL, Lo WU, Chan J, et al. pIMP-PH114 carrying bla IMP-4 in a Klebsiella pneumoniae strain is closely related to other multidrug-resistant IncA/C2 plasmids. Curr Microbiol. 2014;68(2):227–232. doi:10.1007/s00284-013-0471-x
13. Li J, Hu Z, Hu Q. Isolation of the first IMP-4 metallo-beta-lactamase producing Klebsiella pneumoniae in Tianjin, China. Braz J Microbiol. 2012;43(3):917–922. doi:10.1590/S1517-83822012000300010
14. Lo WU, Cheung YY, Lai E, Lung D, Que TL, Ho PL. Complete sequence of an IncN plasmid, pIMP-HZ1, carrying blaIMP-4 in a Klebsiella pneumoniae strain associated with medical travel to China. Antimicrob Agents Chemother. 2013;57(3):1561–1562. doi:10.1128/AAC.02298-12
15. Zhang R, Liu L, Zhou H, et al. Nationwide surveillance of clinical carbapenem-resistant enterobacteriaceae (CRE) strains in China. EBioMedicine. 2017;19:98–106. doi:10.1016/j.ebiom.2017.04.032
16. Clinical and Laboratory Standards Institute (CLSI) M100. Performance Standards for Antimicrobial Susceptibility Testing, 29th Ed; 2019.
17. Ruan Z, Wu J, Chen H, Draz MS, Xu J, He F. Hybrid genome assembly and annotation of a pandrug-resistant klebsiella pneumoniae strain using nanopore and illumina sequencing. Infect Drug Resist. 2020;13:199–206. doi:10.2147/IDR.S240404
18. Ruan Z, Feng Y. BacWGSTdb, a database for genotyping and source tracking bacterial pathogens. Nucleic Acids Res. 2016;44(D1):D682–D687. doi:10.1093/nar/gkv1004
19. Grant JR, Stothard P. The CGView server: a comparative genomics tool for circular genomes. Nucleic Acids Res. 2008;36(WebServer issue):W181–W184. doi:10.1093/nar/gkn179
20. Alikhan NF, Petty NK, Ben Zakour NL, Beatson SA. BLAST ring image generator (BRIG): simple prokaryote genome comparisons. BMC Genomics. 2011;12:402. doi:10.1186/1471-2164-12-402
21. Sullivan MJ, Petty NK, Beatson SA. Easyfig: a genome comparison visualizer. Bioinformatics. 2011;27(7):1009–1010. doi:10.1093/bioinformatics/btr039
22. Du X, He F, Shi Q, et al. The rapid emergence of tigecycline resistance in blaKPC-2 harboring klebsiella pneumoniae, as mediated in vivo by mutation in tetA during tigecycline treatment. Front Microbiol. 2018;9:648. doi:10.3389/fmicb.2018.00648
23. Ruan Z, Yu Y, Feng Y. The global dissemination of bacterial infections necessitates the study of reverse genomic epidemiology. Brief Bioinform. 2019. doi:10.1093/bib/bbz010
24. Wang Y, Cao W, Zhu X, et al. Characterization of a novel Klebsiella pneumoniae sequence type 476 carrying both bla KPC-2 and bla IMP-4. Eur J Clin Microbiol Infect Dis. 2012;31(8):1867–1872. doi:10.1007/s10096-011-1512-7
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


