Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Characteristics of Poor Prognosis in Patients with Cerebral Venous Sinus Thrombosis: A Multicenter Retrospective Study
Authors Zhang Y, Liu Y , Qin B, Tang S , Liang Z
Received 24 March 2023
Accepted for publication 5 June 2023
Published 13 June 2023 Volume 2023:19 Pages 1417—1426
DOI https://doi.org/10.2147/NDT.S414123
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Yuping Ning
Yunli Zhang,1,2,* Yayuan Liu,1,3,* Bin Qin,1,4 Shiting Tang,1,5 Zhijian Liang1
1Department of Neurology, The First Affiliated Hospital of Guangxi Medical University, Nanning, People’s Republic of China; 2Department of Intensive Care Unit, The People’s Hospital of Guangxi Zhuang Autonomous Region, Nanning, People’s Republic of China; 3Department of Neurology, Minzu Hospital of Guangxi Zhuang Autonomous Region, Nanning, People’s Republic of China; 4Department of Neurology, Liuzhou People’s Hospital, Liuzhou, People’s Republic of China; 5Department of Neurology, Second Affiliated Hospital of Guangxi Medical University, Nanning, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhijian Liang, Department of Neurology, The First Affiliated Hospital of Guangxi Medical University, No.6 Shuangyong Road, Nanning, People’s Republic of China, Tel +86-771-5330705, Fax +86-771-5352627, Email [email protected]
Purpose: The present study aimed to identify the characteristics, predictors, and imaging features of poor recovery in cases of cerebral venous sinus thrombosis (CVST).
Patients and Methods: A total of 290 consecutive adult patients with CVST were enrolled from January 2017 to December 2021 from five hospitals in Nanning, Guangxi. According to the modified Rankin scale (mRS) score at hospital discharge, the patients were classified into good prognosis (GP, mRS ≤ 2) groups and poor prognosis (PP, mRS> 2) groups. Logistic regression was used to identify factors associated with clinical outcomes.
Results: Of the 290 patients, 35 were assigned to the PP group and 255 to the GP group. No significant difference in sex was observed between the two groups. Headache (76.21%) was the most frequent symptom of CVST, and local head and neck infection was the major comorbidity (26.21%). Approximately half of the patients (48.62%) had brain injury lesions < 1 cm, and the most commonly affected sinus was the lateral sinus (81.03%). Less-common headaches (odds ratio [OR]: 2.769, p=0.046), altered mental status (OR: 0.122, p< 0.001), hematologic disorder (OR: 0.191, p=0.045), and injury to multiple lobes (OR: 0.166, p=0.041) were associated with poor clinical outcomes.
Conclusion: Headache was the most common and protective manifestation of CVST, and disturbances in consciousness were an important indication of poor clinical prognosis. Patients with hematologic diseases also tended to have poor outcomes. No significant correlation was found between the number and location of venous sinus thromboses and clinical prognosis; however, intracranial injury involving multiple lobes was often associated with poor prognosis.
Keywords: cerebral venous sinus thrombosis, cerebral infarction, intracranial hemorrhage, hematologic disorder, prognosis
A Letter to the Editor has been published for this article.
Introduction
Cerebral venous sinus thrombosis (CVST) is an uncommon cerebrovascular disease and nonspecific type of stroke, accounting for 0.5–1% of all cases of stroke.1 Clinical symptoms result from increased intracranial pressure caused by impaired venous drainage and CVST-related brain injury. CVST is associated with a wide range of clinical symptoms from isolated headaches (the most common symptom at presentation, reported in 90% of cases) to focal deficits, seizures, and mental status changes.2 The variability and nonspecificity of the clinical course make the diagnosis and prognosis of CVST cases challenging. Moreover, according to recent research,3 the incidence of CVST has increased more than previously estimated with the advent of modern diagnostic techniques, with an overall death and dependency rate of 15%. In addition, the incidence of recurrent CVST is 4 in 100 patient-years in the first year after the first episode.4
Similar to other venous thromboembolism diseases, CVST has a multifactorial etiology, and 85% of all patients exhibit at least one risk factor.4 The risk factors associated with CVST are diverse and complex, and also vary according to regional and racial differences. Studies in European and American populations have described the following predisposing factors for CVST: thrombophilia, local and systemic infection, concomitant solid or hematologic cancer, and pregnancy or puerperium.5–7 Understanding the pathogenesis of CVST is difficult, and further research is warranted to advance methods for its diagnosis and treatment. While risk factors associated with the prognosis of CVST can be identified from among the clinical characteristics of patients, no consensus has been reached regarding predictive factors for CVST. Considering differences among populations of differing ethnicity as well as differences in healthcare practices in different countries and regions, the risk factors for CVST may differ between Western and Asian populations and even among different regions where these populations reside.
Previous small-sample studies from the Middle East and Europe suggested that older age, disturbance of consciousness, and hemorrhagic lesions may be associated with poor clinical outcomes, and that thrombosis of the cerebellar vein, internal vein, and superior sagittal sinus may develop into severe CVST.5,8,9 In 2022, a systematic retrospective clinical study of 260 patients in Taiwan found that patients with a poor prognosis had higher levels of D-dimer and longer hospital stays.10 Although significant literature is available regarding the characteristics of CVST around the world, data derived from patients in China are limited. Existing studies in China have been single-center or small-sample studies.11–13 To improve the understanding of the risk factors for CVST and predictors of CVST patient outcomes in the Chinese population, the clinical data of patients with CVST admitted to five hospitals in South China were analyzed retrospectively in the present study. Differences in the clinical characteristics of patients with a favorable prognosis versus those with a poor prognosis were identified to provide clinicians with a reference for preventing the development of CVST and optimizing clinical management decisions.
Materials and Methods
Patients
The records of all patients with CVST diagnosed via computed tomography venography (CTV) or magnetic resonance venography (MRV) at five hospitals (The First Affiliated Hospital of Guangxi Medical University, the People’s Hospital of Guangxi Zhuang Autonomous Region, Minzu Hospital of Guangxi Zhuang Autonomous Region, and the Second, Third Affiliated Hospital of Guangxi Medical University,) between January 2017 and December 2021 were retrospectively analyzed. Patients on long-term anticoagulant therapy and those with a disease history of >1 month, age <18 years, or incomplete data were excluded from the study. The protocol for the records search is outlined in Figure 1.
 |
Figure 1 Flowchart of patient inclusion. |
Data Collection
The medical records of all included patients were collected and further evaluated by two investigators. Data for sex, age, risk factors, onset of symptoms, time from symptoms to diagnosis, and clinical score were collected from the medical records, and data regarding the treatment and monitoring plans were obtained according to the treating physician’s medical advice. In addition, laboratory measurements performed within 24 h before or after diagnosis were included, including routine blood tests, coagulation function results, and electrolyte levels. The Glasgow Coma Scale (GCS) score was recorded for patients with disturbances in consciousness or pupil condition; mechanical ventilation time and vasopressor dosage were recorded for patients with shock; and the first pressure value was recorded for patients who underwent lumbar puncture. The complications and disease management that occurred for patients who died were also recorded.
CTV or MRV revealed the presence of infarct or hemorrhage at the time of initial diagnosis, and the number and location of venous sinus thromboses were recorded. All patients, except those with contraindications, were treated immediately after diagnosis with warfarin or low molecular weight heparin dose was set to maintain the INR at 2.0–3.0. When the symptoms of intracranial hypertension persisted after adequate anticoagulation treatment, CT was performed to confirm the presence of a mass effect and cerebral hernia. Whenever possible, interventional therapy (including thrombolysis and/or thrombectomy) or surgical intervention was performed.
Based on the modified Rankin score (mRS) as a reflection of patients’ recovery, patients were divided into the good prognosis (GP; mRS ≤ 2) and poor prognosis (PP; mRS >2) groups at the time of discharge. Patients in the PP group were followed up by telephone interview at 1 month after discharge. For our investigation of risk factors of CVST patients, we collected data regarding the autoimmune diseases, including systemic lupus erythematosus, nephrotic syndrome, and vasculitis. We also recorded local head and neck infections or injuries mainly referring to sinusitis and meningoencephalitis and history of surgery or trauma to the head and face. Additionally, we collected details regarding hematologic disorders, such as prothrombotic conditions including genetic mutations, if any, in Protein S, Protein C, antithrombin, factor V Leiden, and prothrombin genes, hematologic conditions, including leukemia and lymphoma, anemic conditions including sickle cell disease and trait, iron deficiency and folic acid deficiency, paroxysmal nocturnal hemoglobinuria, primary or secondary polycythemia and primary or secondary thrombocythemia.
Statistical Analysis
The data were presented as mean (standard deviation) or count (percentage). Student’s t-test was used for comparisons of continuous variables, and Pearson’s chi-squared test was used for comparisons of categorical variables. Multivariate binary logistic regression was performed for the variables that were significantly associated with patients’ recovery on univariate analysis, and the variables with p<0.05 were considered statistically significant. All statistical analyses were performed using SPSS statistics version 25.0 (IBM, Armonk, NY, USA).
Ethical Approval
This study was conducted in accordance with the Declaration of Helsinki and approved by the First Affiliated Hospital of Guangxi Medical University Ethical Review Committee. The requirement for written informed consent was waived due to the retrospective nature of our study. During the data collection, personally identifying information, such as names, addresses and phone numbers, of the study participants was never recorded. The collected data were kept confidential and used only for the purpose of the study.
Results
Clinical Characteristics of Patients with CVST
A total of 290 patients with CVST, including 140 female and 150 male patients, aged from 18 to 81 years were included. Generally, headache (76.21%) was the most common symptom in the two groups, followed by focal neurologic defects (39.31%); limb weakness/numbness, aphasia, and vision problems) and disturbance of consciousness (13.45%), which was more obvious in the PP group Regarding risk factors, local head and neck infections were the leading comorbidity (26.21%), followed by pregnancy/puerperium (12.07%).
Lesions including ischemic and hemorrhagic were detected in 149 patients (51.37%). Overall, the incidence of ischemic and hemorrhagic lesions was almost identical (21.03% & 30.34%), however, hemorrhagic lesions were more common in the poor prognosis group. The most commonly involved sinus was the lateral sinus (81.03%), followed by the superior sagittal sinus (47.59%) and straight sinus (13.10%). Moreover, multiple sinuses thrombosis involved were in up to 40.69% of patients (Table 1).
 |
Table 1 Demographics of Patients with CVST |
Factors Associated with Poor Prognosis
A total of 35 patients were included in the PP group (mRS >2 at discharge); 10 of these patients died while hospitalized. The incidence rates of the factors hematologic disorder (p=0.007) differed significantly between the GP and PP groups. Moreover, significant differences in the following clinical manifestations were observed between the two groups: headache (p<0.001), focal neurologic defects (p=0.021), and altered mental status (p<0.001). Differences in routinely measured laboratory parameters also were observed between the two groups, with the PP group having a higher APTT (p=0.010), lower hemoglobin (p=0.019), lower potassium (p=0.019), and higher sodium (p=0.002) compared with the GP group. Imaging revealed large sporadic hemorrhagic lesions in the PP group (Table 1).
Logistic regression was performed to identify prognostic factors for poor clinical outcomes among CVST patients. In the binary logistic regression model, hematologic disorders (odds ratio [OR]: 0.191, 95% confidence interval [CI]: 0.039–0.965, p=0.045), headache (OR: 2.769, 95% CI: 1.016–7.546, p=0.046), altered mental status (OR: 0.122, 95% CI: 0.039–0.378, p<0.001), low potassium (OR: 4.424, 95% CI: 1.434–13.646, p=0.010), high sodium (OR: 0.870, 95% CI: 0.779–0.971, p=0.013), and multiple-lobe injury (OR: 0.166, 95% CI: 0.030–0.931, p=0.041) were associated with poor clinical outcomes (Table 2).
 |
Table 2 Multivariate Analysis of the Predictors of Poor Prognosis in Patients with Cerebral Venous Sinus Thrombosis |
Treatments
A total of 256 patients received heparinization therapy, 27 patients received interventional therapy (11 received thrombectomy, 5 received thrombolytics, and 11 received two or more treatments simultaneously [thrombectomy and thrombolytics]) while experiencing neurologic deterioration. Three severe patients in PP of CVST required craniotomy when the patients suffered from massive cerebral hemorrhage or obvious local occupying effects. The recovery of venous circulation was confirmed in eight patients via digital subtraction angiography.
Characteristics of Patients Who Died
There were 7 patients with rapid deterioration died from cerebral hernia within the first week after admission to one of the included hospitals with an acute onset of a consciousness disorder and unstable vital signs (Table 3, Figure 2).
 |
Table 3 Characteristics of CVST Patients Who Died |
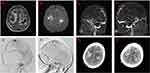 |
Figure 2 Imaging features of a patient with poor recovery. (A–H) A 29-year-old woman who suffered from cerebral hemorrhage in her first trimester. She was hospitalized with coma caused by cerebral venous sinus thrombosis. Computed tomography showed cerebral hemorrhage (A and B), and magnetic resonance venography revealed superior sagittal sinus thrombosis (C and D). The patient’s condition worsened (G and H) after emergency intervention with thrombolytics and thrombectomy (E and F), eventually leading to her death (Table 3, No. 9). |
Discussion
Compared with arterial stroke, CVST is rare. The present retrospective study was conducted on 290 patients with CVST treated in five hospitals, and the results showed that CVST most frequently developed in the lateral sinus and that headache was the most common symptom in these patients. Altered mental status and hematologic disorder were associated with poor prognosis, whereas headache was associated with a good clinical prognosis. Thus, the results of this large-scale retrospective study on CVST patients may provide a reference for clinicians to improve CVST prevention and management.
The baseline characteristics of the patients included in the present study are in line with those reported for other populations in the existing literature.6 However, only 48.27% of the patients in the present study were female, which differs from prior reports that documented a clear predominance of female patients with CVST. In a previous study in China, 53.9% of patients with CVST were female, which is close to the percentage in our study.14 A possible contributing factor is that Chinese women do not use oral contraceptives as frequently as women in Western populations, which might explain the discrepancy in the sex-specific incidence. Moreover, advancements in healthcare for pregnancy may have contributed to the similar incidence rates of CVST between sexes in China.
Headache, the most common symptom, was present in 76.21% of the included patients with CVST. This is consistent with the results published by the International Study on Cerebral Venous and Dural Sinuses Thrombosis.15 Likewise, in other studies conducted in China, headache was the most common symptom.10,12–14 In addition, the present study revealed that headache involvement was associated with a good clinical prognosis, consistent with the findings of a previous study.14 However, the results of present study may provide more robust evidence, as this study analyzed the clinical data of 290 patients from five large tertiary hospital. In patients with CVST, headache is generally caused by impaired venous drainage that results in intracranial hypertension. However, there is also evidence that such patients can experience isolated headaches without any obvious symptoms of increased intracranial pressure.16 The present study also found that altered mental status was a factor for poor prognosis, which is in agreement with a previous retrospective study in Iran that included patients from only a single center.17 Another retrospective study showed that consciousness disturbances were associated with a poor clinical prognosis in a Chinese population.14 The results of the current multicenter study with a large sample size are consistent with this previous study, with altered mental status identified as an additional factor for poor prognosis of Chinese patients with CVST.
Poor prognosis also was associated with older age and the development of cerebral infarctions and hemorrhages in a Turkish population.11 In a study in Iran, early, delayed, and expanded hemorrhage was related to poor outcomes in patients with CVST.17 Different from these prior studies, the present study did not detect any association between hemorrhage and poor prognosis. In addition, Chen et al,10 in their retrospective study, did not observe any association between hemorrhage and poor clinical outcomes. Of note, the current study results revealed that injury to multiple lobes was associated with a poor prognosis for CVST patients. However, intracranial multi-lobe injury was not found to be a factor for poor prognosis in previous studies.5,7,9 Thus, additional cohort studies are needed to confirm this result. Patients with CVST and hematologic disorders may have a poor prognosis, and this information can aid the prediction or identification of severe cases.15 The present study results confirmed that hematologic disorders were associated with poor prognosis in patients with CVST. Although no association was found between poor prognosis and malignancy in a previous study of Chinese patients with CVST, that study did not include patients with hematologic disorders in their patient cohort.14
Blood sodium and potassium levels differed significantly between the GP and PP groups 24 h before and after diagnosis in the present study, however, the values in both groups were basically within the normal range. No other study has evaluated these hematologic parameters with patient data collected before and 24 h after diagnosis. Still, it is not clear whether the sets of hematologic parameters would have continued to differ significantly beyond 24 h after diagnosis with disease progression or after interventional treatment was administered in these patients. In our clinical work, we also observed that patients with severe neurological conditions tend to present with increased sodium and decreased potassium levels, which may be due to the body’s self-regulation, increased osmotic pressure, and excessive diuresis in patients with severe intracranial hypertension.
The technique of interventional therapy with CVST is not mature in some areas of our country. A previous study with a small sample size showed that endovascular treatment may through venous recanalization improve neurological outcomes in most patients with CVST,18–20 while reducing the dose of thrombolytic drugs to decrease the risk of cerebral hemorrhage. This study did not find that interventional therapy had significant benefits in terms of prognosis compared with that observed for patients who did not receive interventional therapy. However, due to the small number of cases and different intervention levels in the five centers, the statistical results cannot fully represent the correlation between this technique and patient prognosis.
The present study has some limitations. First, as this was a retrospective study, selection bias was unavoidable. Second, genetic tests for inherited thrombophilia were not performed owing to the nonavailability of the test in the included institutions. Finally, due to the retrospective nature of this study, a uniform evaluation of long-term outcomes was not possible. Thus, further research with long-term follow-up in a large cohort is needed.
Conclusion
The current retrospective study, which included 290 patients from five hospitals, revealed that CVST most commonly developed in the lateral sinus and transverse-sigmoid sinus and that headache was the most common symptom in Chinese patients. Moreover, altered mental status, intracranial injury involving multiple lobes, and hematologic disorders were associated with poor prognosis. These findings may provide a reference for clinicians to improve strategies for the prevention and treatment of CVST.
Abbreviations
CVST, cerebral venous sinus thrombosis; mRS, modified Rankin scale; GP, good prognosis; PP, poor prognosis; CTV, computed tomography venography; MRV, magnetic resonance venography; GCS, Glasgow Coma Scale; APTT, activated partial thromboplastin time; ARF, acute renal failure; SLE, systemic lupus erythematosus; DIC, disseminated intravascular coagulation; HIE, hypoxic ischemic encephalopathy; CHD, congenital heart disease; CT, computed tomography; SAH, subarachnoid hemorrhage.
Data Sharing Statement
The datasets used and /or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
Ethical approval of this study was granted by the Guangxi Medical University Review Board. The requirement for written informed consent from patients was waived due to the retrospective nature of our study. During the data collection, personally identifying information, such as names, addresses and phone numbers, of the study participants was never recorded. The collected data were kept confidential and used only for the purpose of the study.
Acknowledgments
We thank all the patients and staff of the Department of Neurology of the enrolled hospitals and our colleagues for their valuable support of this study.
Author Contributions
All authors made a significant contribution to the work reported, whether in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work.
Funding
This research was sponsored by the National Natural Science Foundation of China (82260243) and National Key R&D Program of China (No. 2018YFC1311305).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ferro JM, Canhão P. Cerebral venous sinus thrombosis: update on diagnosis and management. Curr Cardiol Rep. 2014;16(9):523. doi:10.1007/s11886-014-0523-2
2. Bourrienne MC, Gay J, Mazighi M, Ajzenberg N. State of the art in cerebral venous sinus thrombosis animal models. J Thromb Haemost. 2022;20(10):2187–2196. doi:10.1111/jth.15816
3. Kristoffersen ES, Harper CE, Vetvik KG, Zarnovicky S, Hansen JM, Faiz KW. Incidence and mortality of cerebral venous thrombosis in a Norwegian population. Stroke. 2020;51(10):3023–3029. doi:10.1161/STROKEAHA.120.030800
4. Capecchi M, Abbattista M, Martinelli I. Cerebral venous sinus thrombosis. J Thromb Haemost. 2018;16(10):1918–1931. doi:10.1111/jth.14210
5. Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F. Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke. 2004;35(3):664–670. doi:10.1161/01.STR.0000117571.76197.26
6. Ruiz-Sandoval JL, Chiquete E, Bañuelos-Becerra LJ, et al. Cerebral venous thrombosis in a Mexican multicenter registry of acute cerebrovascular disease: the RENAMEVASC study. J Stroke Cerebrovasc Dis. 2012;21(5):395–400. doi:10.1016/j.jstrokecerebrovasdis.2011.01.001
7. Dentali F, Poli D, Scoditti U, et al. Long-term outcomes of patients with cerebral vein thrombosis: a multicenter study. J Thromb Haemost. 2012;10(7):1297–1302. doi:10.1111/j.1538-7836.2012.04774.x
8. Duman T, Uluduz D, Midi I, et al. A multicenter study of 1144 patients with cerebral venous thrombosis: the VENOST study. J Stroke Cerebrovasc Dis. 2017;26(8):1848–1857. doi:10.1016/j.jstrokecerebrovasdis.2017.04.020
9. Foschi M, Pavolucci L, Rondelli F, et al. Clinicoradiological profile and functional outcome of acute cerebral venous thrombosis: a hospital-based cohort study. Cureus. 2021;13(9):e17898. doi:10.7759/cureus.17898
10. Chen YC, Chang CW, Wu HC, Chen CM, Chang CH, Chang KH. Clinical characteristics and prognostic factors of non-infectious cerebral venous sinus thrombosis. J Clin Med. 2022;11(20):25.
11. Deng J, Li C, Kuang W, et al. Clinical characteristics of cerebral venous sinus thrombosis in childhood-onset systemic lupus erythematosus patients: a single-centre study from China. Clin Exp Rheumatol. 2021;39(6):1440–1445. doi:10.55563/clinexprheumatol/kn8hco
12. Wang JW, Li JP, Song YL, et al. Clinical characteristics of cerebral venous sinus thrombosis. Neurosciences. 2015;20(3):292–295. doi:10.17712/nsj.2015.3.20140625
13. Wang XH, Zhang LM, Chai YM, Wang J, Yu LF, Zhou SZ. Clinical characteristics and outcomes of pediatric cerebral venous sinus thrombosis: an analysis of 30 cases in China. Front Pediatr. 2019;7:364. doi:10.3389/fped.2019.00364
14. Pan L, Ding J, Ya J, et al. Risk factors and predictors of outcomes in 243 Chinese patients with cerebral venous sinus thrombosis: a retrospective analysis. Clin Neurol Neurosurg. 2019;183:105384. doi:10.1016/j.clineuro.2019.105384
15. Saposnik G, Barinagarrementeria F, Brown RD, et al. Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(4):1158–1192. doi:10.1161/STR.0b013e31820a8364
16. Mehta A, Danesh J, Kuruvilla D. Cerebral venous thrombosis headache. Curr Pain Headache Rep. 2019;23(7):47. doi:10.1007/s11916-019-0786-9
17. Shakibajahromi B, Haghighi AB, Salehi A, et al. Clinical and radiological characteristics and predictors of outcome of cerebral venous sinus thrombosis, a hospital-based study. Acta Neurol Belg. 2020;120(4):845–852. doi:10.1007/s13760-018-1009-6
18. Zhen Y, Zhang N, He L, Shen L, Yan K. Mechanical thrombectomy combined with recombinant tissue plasminogen activator thrombolysis in the venous sinus for the treatment of severe cerebral venous sinus thrombosis. Exp Ther Med. 2015;9(3):1080–1084. doi:10.3892/etm.2015.2198
19. Guo XB, Liu S, Guan S. The clinical analysis and treatment strategy of endovascular treatment for cerebral venous sinus thrombosis combined with intracerebral hemorrhage. Sci Rep. 2020;10(1):22300. doi:10.1038/s41598-020-78570-1
20. Wang C, Sun J, Shao J, Zhang X, Chen X. Clinical observation and value analysis of endovascular interventional therapy for intracranial venous sinus thrombosis. Biomed Res Int. 2022;2022:4931210. doi:10.1155/2022/4931210
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
