Back to Journals » Patient Preference and Adherence » Volume 17
Characteristics of Inhaler Technique in COPD Patients in a Specialized Center in Armenia, Colombia: A Cross-Sectional Study
Authors Montes Cardona JA, Hincapié Erira DA, Nati-Castillo HA , Sánchez-Vallejo J, Izquierdo-Condoy JS
Received 15 April 2023
Accepted for publication 1 August 2023
Published 16 August 2023 Volume 2023:17 Pages 2025—2038
DOI https://doi.org/10.2147/PPA.S417375
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Jorge A Montes Cardona,1 Diego A Hincapié Erira,1 Humberto Alejandro Nati-Castillo,1 Jaime Sánchez-Vallejo,2 Juan S Izquierdo-Condoy3
1Faculty of Health Sciences, Universidad del Quindío, Armenia, Colombia; 2Pneumology Service, IPS Neumovida, Armenia, Colombia; 3One Health Research Group, Universidad de las Américas, Quito, Ecuador
Correspondence: Juan S Izquierdo-Condoy, OneHealth Global Research Group, Universidad de las Américas, Quito, Ecuador Calle de los Colimes y Avenida De los Granados, Quito, 170137, Tel +593992561230, Email [email protected]
Purpose: The aim of this research was to evaluate the technique of using inhaled drugs in patients with a confirmed history of COPD and describe errors in inhaler technique.
Patients and Methods: Descriptive cross-sectional study was conducted in patients with a history of COPD using inhalation therapy, attending pulmonology consultation between August 2020 and April 2021 in Armenia, Colombia. A non-probabilistic sample of 80 adult participants was calculated, and the inhalation technique was evaluated (depending on the device used) using a scale validated for Colombia. Descriptive analysis of the qualitative variables was performed using frequencies and percentages. The Chi-Square test and Fisher’s exact test (in corresponding cases) were used to look for association relationships between categorical variables.
Results: A total of 80 participants were evaluated, of which 66.3% (n = 53) were male, and 32.5% were older than 80 years. Clinically, 30.0% (n = 24) were classified as Modified Medical Research Council Dyspnea Scale (mMRC) grade 3, and 51.2% (n = 41) had at least one exacerbation per year. The main comorbidity was hypertension (40.3%). Pressurized metered-dose inhalers with spacer were the most used device at 22.7% (n = 39). Incorrect technique (at least one error in the steps of the inhalation technique used) was found in 48.7%. The most frequent error among all the techniques was the failure to perform pre-inspiratory exhalation. No significant differences were observed between the development of the technique and the characteristics of the participants.
Conclusion: Nearly half of the patients who use inhalation devices make errors in the technique. Patient education and training of healthcare personnel represent a fundamental pillar in mitigating the incorrect use of these devices.
Keywords: pulmonary disease, chronic obstructive, administration, inhalation, medication errors
Introduction
Chronic obstructive pulmonary disease (COPD) is characterized by marked airflow limitation due to anatomical alterations in the airways resulting from chronic exposure to risk factors such as tobacco and biomass.1,2 These alterations culminate in the destruction and widening of pulmonary alveoli, as well as hyperplasia of mucin-producing cells at the bronchial level, leading to air entrapment and decreased ventilatory mechanics. These pathologies include pulmonary emphysema, chronic bronchitis, and bronchial asthma.3,4 Approximately 300 million people suffer from COPD in the world in 2020,5 according to data from the World Health Organization (WHO), an estimated 3.23 million people died from this disease in 2019 being the third leading cause of death worldwide, and people living in low- and middle-income countries are the most affected.6 In the Americas, an estimated 13.2 million people are living with COPD, responsible for 235,000 deaths in 2010.7,8 In Colombia, the PREPOCOL study conducted by the Colombian Pulmonological Foundation determined that 9 out of every 100 people over 40 years of age in Colombia suffer from COPD, with a prevalence of 6.2% in Bogotá, 7.9% in Barranquilla, and 13.5% in Medellín among the main cities of the country.9 Quindío was identified as the department (the first-level territorial unit) with the highest prevalence of COPD in the country in 2016.10 The economic impact of the disease on the Colombian health system has been studied in conjunction with tobacco-attributable diseases, and it is estimated that the annual costs incurred by the health system range from 6 to 15% of its total health expenditure.10
As the incidence of COPD patients has been increasing nowadays, the administration of inhaled medications is increasingly frequent, as they represent a fundamental pillar in the treatment of this disease.11 However, it has been identified that up to half of patients use them incorrectly, resulting in poor therapeutic outcomes and an increased risk of hospitalization and future complications.3
The appropriate technique is an important aspect in inhaler therapy, so even before considering therapeutic failure due to the active compound, the possibility of inadequate technique should be considered, taking into account associated patient-dependent factors such as age, low educational level, low socioeconomic status, and comorbidities,12 as well as health care provider-dependent factors such as lack of prior instructions and poor training of the health care professional in the use of inhalers;12 in this context, continuous patient counselling has been shown to have important positive effects on inhaler technique, and the contingent that health care systems can count on for this task includes health care personnel from different areas such as specialist physicians, general practitioners, nurses, respiratory therapists and even pharmacists.13,14 Observational studies have identified a significant relationship between poor inhalation technique and inadequate symptom control.15 The proper technique (steps required) for the use of the inhaler systems evaluated in this research is listed in Table 1, and a graphical guide is presented in Figure 1.
 |
Table 1 List of Steps Necessary to Develop the Correct Inhaler Technique for the Inhaler Systems Studied in This Research |
On average, more than two-thirds of patients make at least one mistake when using their inhalation device.16 In general, the main problems related to the use of the devices are inspiratory flow, duration of inhalation, coordination, dose preparation, pre-inspiratory exhalation, apnea period, and inhalation of the subsequent dose.17 Although several global studies have demonstrated the deficiencies in the technique of inhalation therapy in COPD patients,18,19 so far in Colombia the inhalation technique has not been explored in COPD patients.
The objective of this research was to evaluate the technique of using inhaled drugs in patients with a confirmed history of COPD and describe errors in inhaler technique.
Materials and Methods
Study Design
An observational, cross-sectional study was carried out.
Population and Settings
The Colombian health system focuses health care services on a comprehensive care policy, in which service providers play an important role.20 In this sense, the therapeutic management of many patients with COPD is carried out by medical specialists.
The participants in this study are patients receiving treatment for COPD who attend a specialized pulmonology consultation at the IPS NEUMOVIDA in the city of Armenia, Quindío between August 2020, and April 2021.
Sample
According to data from patients with a history of COPD attending the pulmonology consultation of the IPS NEUMOVIDA in the city of Armenia, it was determined that a total of 99 patients attended a pulmonological medical consultation during the year 2020. From this population, the necessary sample size was calculated using the following equation:21
Where the total population (N = 99), the expected proportion of unknown response took the value of (p = 0.5), confidence level (Z = 95%, or Z = 1.96), and a permissible precision or margin of error of (d = 5%), obtaining a minimum of 79 participants. The sample was collected consecutively through a non-probabilistic sampling, by convenience of the researchers, including as participants the patients who came to receive medical care at the clinic NEUMOVIDA S.A.S. at the described time, who met the selection criteria and who voluntarily agreed to participate in the research.
Inclusion Criteria
Patients diagnosed with COPD (referred by the patient or family member and with corroboration of the diagnosis by verbal confirmation by the internist or treating pulmonologist) are currently on treatment with metered-dose inhalers, dry powder inhalers, or soft mist inhalers, over 18 years of age.
Exclusion Criteria
Patients with cognitive or physical disabilities that prevent the correct performance of the inhalation technique were excluded.
Sample and Data Collection
The patients included in this research were recruited after a specialized medical consultation at NEUMOVIDA S.A.S. In the first contact with the researchers, the participants agreed to participate in this research through personal informed consent. The necessary information was collected by the researchers through a physical questionnaire divided into two segments: demographic variables and variables of the inhalation system.
Initially, demographic data were requested, including variables such as “age”, “sex”, “educational level”, “socio-economic status”,22 “access to health”, and “occupation”. Next, the variables of the inhalation system were evaluated using the scale adapted from the multicenter and prospective study on “education and teaching” of the inhalation procedure in respiratory patients from the “Eden study”, and the scoring system created by the Colombian Pneumology Foundation’s pulmonary rehabilitation program.23 In this section, the variables “COPD spirometric pattern”, and “GOLD Rating” were collected from the participants’ personal cards, while the variables “Exacerbations per year” and “Comorbidities” were collected from the participant’s responses and noted in the questionnaire, and the variable “mMRC grade” was clinically evaluated by the researchers and recorded in the questionnaire.
Finally, the inhaler usage technique was evaluated through a checklist for each inhalation device assessed (part of the questionnaire). This checklist was based on the proposal of the Primary Care Respiratory Group.12 The evaluation was carried out through physical observation by three researchers (DAHE, HAN-C, and JSV) who held the academic title of general practitioners and were supervised by a pulmonology specialist. Using a physical model of each type of inhaler, the researchers observed the patients while they performed the inhaler technique, and the results of each measurement were recorded on the checklist.
Statistical Analysis
Descriptive analysis of the qualitative variables was performed using frequencies and percentages. The Chi-Square test and Fisher’s exact test (in corresponding cases) were used to look for association relationships between categorical variables. In addition, the potential risk of participants for incorrect inhaler technique was assessed by comparing the total number of individuals who performed the correct and incorrect techniques for the 6 inhaler systems evaluated, the results were presented as Odds Ratio (OR) with 95% confidence intervals (95% CI). P-values <0.05 were accepted as statistically significant.
All analysis of the results was carried out in the IBM SPSS Statistics for Windows Version 24.0 (IBM Company, Chicago, IL, USA) software.
Ethical Considerations
This work was presented to the bioethics committee of the University of Quindío, endorsed, and registered in ACTA No. 24 October 02, 2020, research bioethics committee (Resolution 0600 of October 29, 2001). In addition, this research was conducted in accordance with the guidelines of the Declaration of Helsinki.
Results
Demographics
Out of a total of 80 participants, most were male (66.3%) and older than 80 years (32.5%). About 53.8% (n = 43) attended basic education, while 34 participants (42.5%) were from medium-low socioeconomic stratum, and 77.5% (n = 62) belonged to the taxpayer health regime (Table 2).
 |
Table 2 Sociodemographic Characteristics of the Participants |
Regarding the clinical characteristics of the population, it was found that 30.0% (n = 24) of patients experienced exhaustion after walking less than 100 meters on flat terrain, corresponding to grade 3 on the Modified Medical Research Council Dyspnea Scale (mMRC). In addition, 51.2% (n = 41) reported experiencing at least one exacerbation per year. The COPD spirometry pattern was the most prevalent (70.0%), with the mild grade of the GOLD classification being the most common (47.5%). The most frequent comorbidity was arterial hypertension (40.3%) (Table 3).
 |
Table 3 Characteristics of Chronic Obstructive Pulmonary Disease of the Participants |
Features of Inhalation Therapy
When analyzing the inhalation systems used by the population, it was found that 45.0% used more than 2 inhalers to control their pathology, with the metered-dose inhaler (MDI) with spacer being the most used (22.7%), followed by the metered-dose inhaler (MDI) without spacer (17.4%) and the soft mist inhalers (SMIs) (17.4%) (Table 4).
 |
Table 4 Characteristics of Participants’ Inhalation Systems |
Errors in Techniques Between Types of Inhalation Therapies
Among the total number of steps of the 6 inhaler systems evaluated, the inhaler with the highest number of incorrectly performed steps was the multi-dose dry powder inhaler Accuhaler type with 16.2% (n = 22) of total incorrect steps, followed by the metered-dose inhaler without spacer 13.7% (n = 42). The inhalers with the highest total number of correct steps which were the inhaler of correct steps were the soft mist inhaler 95.6% (n = 261) and the multi-dose dry powder inhaler Turbuhaler type 94.4% (n = 136) (Table 5).
 |
Table 5 Evaluation of the Total Number and Specific Number of Steps of the Inhalation Systems Studied in This Research |
When analyzing individually the steps of each inhaler, in the multi-dose dry powder inhaler Accuhaler type step 3 (Exhale) and step 5 (Apnea) were the worst developed by the participants with 64.7% (n = 11) for both steps. Errors in these steps were also the most frequent in the metered-dose inhaler with spacer and in the single-dose dry powder inhaler (Table 5).
In turn, within the overall analysis of the development of the inhaler technique, it was found that the inhaler with the worst performance (at least one step developed incorrectly) was the Accuhaler type multi-dose dry powder inhaler with 64.7% (n = 11) of participants who developed at least 1 step incorrectly, while the soft mist inhaler was the best performed inhaler system with 79.41% (n = 27) of participants who performed all steps correctly (Figure 2).
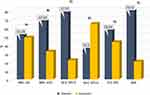 |
Figure 2 Overall analysis of the use of correct and incorrect inhalation technique, according to the different inhalation systems. Figure 2 shows the overall assessment of the inhaler technique, in which the wrong performance of at least 1 step in inhaler technique per participant was considered as an “incorrect” technique. The dry powder multidose inhaler/Accuhaler type D and the metered-dose inhalers with spacer A, had the highest number of participants with the incorrect technique with 64.7% (n=11) and 48.72% (n=19), respectively, followed by the single-dose dry powder inhaler E with 43.34% (n=13) incorrect technique and the metered-dose inhaler without spacer B at 32.36% (n=11). On the other hand, the soft mist inhaler F had the highest number of participants with the correct technique (all steps performed without error) with 79.41% (n=27), followed by the multi-dose dry powder inhaler Turbuhaler type C with 77.77% (n=14) correct technique. Abbreviations: MDI. wS, metered-dose inhalers with spacer; MDI. woS, metered-dose inhalers without spacer; M-d. DPI/T, multi-dose dry powder inhalers/Turbuhaler type; M-d. DPI/T, multi-dose dry powder inhalers/Accuhaler type; S-d. DPI, single-dose dry powder inhalers; SMI, soft mist inhalers. |
Differences and Risk of Incorrect Inhaler Technique
When analyzing differences between the characteristics of the participants, the findings were limited in the group of metered-dose inhaler with spacer, the employed and pensioned participants mostly showed correct technique performance (p = 0.018), as well as the participants with mMRC grades 2 and 3 (p = 0.008). On the other hand, it was evidenced in the users of the Accuhaler type multi-dose dry powder inhaler that those who claimed to suffer fewer exacerbations per year performed the inhalation therapy technique better (p = 0.042) (Supplementary File 1).
On the other hand, the overall assessment of the risk of performing an incorrect inhaler technique (at least one incorrect step) did not expose any characteristic as a potential risk factor for participants (Table 6).
 |
Table 6 Risk Factors for Participants’ Incorrect Inhalation Techniques |
Discussion
To our knowledge, this is the first study to evaluate the technique of different types of inhalers in COPD patients in Colombia. This research found that most participants were over 70 years of age, corresponding to 61.3% of the total sample. In addition, there was a predominance of the male sex (66.3%), which is consistent with the PREPOCOL study that evaluated the prevalence of COPD in Colombia in 2008,15 as well as other research on inhaler technique in various countries.11,24–26 Likewise, despite their age, most participants showed unfavorable socioeconomic conditions, since 53.8% said they had only completed primary education, and 71.4% belonged to a lower middle or low socioeconomic stratum.
The clinical condition of the participants exhibited considerable pulmonary involvement in a significant percentage, characterized by 30.0% and 23.8% corresponding to mMRC grades 3 and 4, respectively; however, only 17.5% of participants were classified as “very severe” according to the GOLD Rating. Additionally, the health status of the participants is affected by different comorbidities, probably related to the advanced age of most participants; in this context, the most frequent comorbidity was arterial hypertension in 40.3%, similar to that reported by Dal Negro, R.W. et al, who found comorbidities in 78.6% of COPD patients, with cardiovascular disorders being the most frequent comorbidity.27
The characteristics of the participants’ inhaler therapy showed a wide use of inhalers, with 80% using 2 inhalers or more for COPD control, which supports the clinical severity of our participants, together with the fact that only a small proportion of participants reported not suffering exacerbations during the last year, a feature that has been attributed to inadequate use of inhalers in other studies.28,29 In this context, the inhalation system most used by the participants was the metered-dose inhaler (MDI) with spacer, followed by the metered-dose inhaler (MDI) without spacer and the fine mist inhaler, a trend different from that found by Duarte de Araújo A. et al, where the most used systems were the single-dose and multi-dose dry powder inhalers.30
The global study of the inhalation technique showed that the system that represented the greatest difficulties for the patients was the multi-dose dry powder inhaler Accuhaler type, with the highest percentage of incorrect steps and the highest number of individuals with incorrect execution (at least one step performed incorrectly).
Within the stratified analysis of each step, even though different inhaler systems were evaluated, we found that, although in different percentages, the predominant incorrect steps were the exhalation prior to the use of the device and the apnea after inhalation, which was evidenced in the users of metered-dose inhalers with and without spacer, multi-dose dry powder inhaler Accuhaler type, and single-dose dry powder inhaler. Findings similar to those presented in investigations in different corners of the world such as Alsufyani A., and Luczak-Wozniak K. et al, who stated post-inspiratory apnea as the main error in users of metered-dose inhalers (MDI) and dry powder inhalers (DPI) among adults with Asthma and COPD in Saudi Arabia and Poland, respectively,31,32 and supported by the systematic review of Cho-Reyes S et al, who found in metered-dose inhaler users deep exhalation prior to inhalation (65.5% [95% CI 52.0, 78.9]) and post-inspiratory apnea (41.9% [95% CI 29.8, 53.9]) as the most frequent errors.33 While Pothirat C. et al exposed that pre-inspiratory exhalation was the most frequent error in metered-dose inhalers without spacer and multi-dose dry powder inhaler Accuhaler type in Thai adults with COPD.24 This being so, we can infer that the main errors among our participants could not be strictly related to inhaler system-dependent characteristics or patient-dependent characteristics such as age but to steps that apparently may depend mostly on external factors such as the explanation received by the physician or health professional in charge of the management.34
On the other hand, although several risk factors have been postulated for the incorrect development of inhaler techniques such as low educational level, low socioeconomic level, and advanced age,12,24,35 the risk analysis of our research did not allow us to recognize any risk factor, probably due to the limited size of the sample studied in this research. However, our findings emphasize the importance of healthcare personnel as a guide for the use of inhalers, manifesting the importance of continuous and personalized education for COPD patients as stated in previous studies.24,32,36 In addition, the importance of including different health professionals in the process of sustained education of COPD patients using inhalers, including nurses, nursing assistants, general practitioners, respiratory therapists, and even pharmacists, probably having a larger human contingent will allow greater scope for the process of patient education and positive long-term effects.
This research had certain limitations, such as a limited sample size. However, the total number of participants was representative of the studied population, which is characterized by patients who are treated in a specialized COPD center in Armenia, Colombia. However, since the sample studied corresponds only to a center specialized in COPD, the findings of this research cannot be representative for the entire population of COPD patients in Colombia. On the other hand, data collection was carried out using a questionnaire, which exposed the results to recall bias. Nevertheless, we consider that performing a physical data collection process among participants with a chronic condition such as COPD, who are quite familiar with the therapy being studied, can help mitigate recall bias in our findings.
Conclusion
The present study involved 80 patients, mostly men over 70 years of age with primary education and health affiliation regime. Forty-five percent used more than 2 inhalers, with the metered-dose inhaler being most frequently used.
The device that demonstrated the best inhalation technique was the soft mist inhaler, in contrast to the multi-dose dry powder inhaler Accuhaler type showed the greatest difficulties in use, having the highest number of errors and incorrect technique.
The steps corresponding to exhalation prior to drug inspiration and post-inspiratory apnea were the most frequent errors despite being present in different inhalation systems.
This research highlights the need to increase efforts in patient education in inhalation technique and training of healthcare personnel to mitigate the proportion of incorrect use of these devices and, consequently, their complications and the deterioration of the patient’s clinical condition. It is proposed to include more health professionals in the management of COPD patients in the Colombian context and in other countries of the region so that patients can receive a continuous and personalized education.
Consent for Publication
Acceptance of voluntary participation was obtained from each of the patients through a physical informed consent form. The informed consent form was completed before beginning the data collection process.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Vijayan VK. Chronic obstructive pulmonary disease. Indian J Med Res. 2013;137(2):251–269.
2. Diette GB, Accinelli RA, Balmes JR, et al. Obstructive lung disease and exposure to burning biomass fuel in the indoor environment. Glob Heart. 2012;7(3):265–270. doi:10.1016/j.gheart.2012.06.016
3. Halpin DMG, Criner GJ, Papi A, et al. Global Initiative for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease. The 2020 GOLD Science Committee Report on COVID-19 and Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2021;203(1):24–36. doi:10.1164/rccm.202009-3533SO
4. Jameson JL, Kasper DL, Longo DL, Fauci AS, Hauser SL. Harrison Principles of Internal Medicine.
5. Ruvuna L, Sood A. Epidemiology of chronic obstructive pulmonary disease. Clin Chest Med. 2020;41(3):315–327. doi:10.1016/j.ccm.2020.05.002
6. World Health Organization. Chronic obstructive pulmonary disease (COPD); 2023. Available from: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd).
7. World Health Organization. The global burden of disease: 2004 update [Internet]. World Health Organization; 2008. Available from: https://apps.who.int/iris/handle/10665/43942.
8. Pan American Health Organization. Chronic obstructive pulmonary disease (COPD) in the Americas. PAHO; 2014 Available from: https://www3.paho.org/hq/dmdocuments/2014/EPOC-Factsheet-2014-Eng-(3).pdf.
9. Ministerio de Salud y Protección Social. Enfermedad pulmonar obstructiva crónica (EPOC). Dirección de Promoción y Prevención. Subdirección de Enfermedades No Transmisibles, Bogotá; 2013. Available from: www.minsalud.gov.co/Documentos%20y%20Publicaciones/epoc.pdf.
10. Ministerio de Salud y Protección Social. Análisis de Situación de Salud (ASIS) Colombia; 2018. Available from: www.minsalud.gov.co/sites/rid/lists/bibliotecadigital/ride/vs/ed/psp/asis-colombia-2018.pdf.
11. Adeloye D, Song P, Zhu Y, Campbell H, Sheikh A, Rudan I. Global, regional, and national prevalence of, and risk factors for, chronic obstructive pulmonary disease (COPD) in 2019: a systematic review and modelling analysis. Lancet Respir Med. 2022;10(5):447–458. doi:10.1016/S2213-2600(21)00511-7
12. Gonzálvez Rey J, Mascarós Balaguer E, García Pardo M Simplemente Inhalar.
13. Basheti IA, Qunaibi EA, Hamadi SA, Reddel HK. Inhaler Technique Training and Health-Care Professionals: effective Long-Term Solution for a Current Problem. Respir Care. 2014;59(11):1716–1725. doi:10.4187/respcare.02671
14. Basheti IA, Salhi YB, Basheti MM, Hamadi SA, Al-Qerem W. Role of the pharmacist in improving inhaler technique and asthma management in rural areas in Jordan. Clin Pharmacol Adv Appl. 2019;11:103–116.
15. Caballero A, Torres-Duque CA, Jaramillo C, et al. Prevalence of COPD in five Colombian cities situated at low, medium, and high altitude (PREPOCOL study). Chest. 2008;133(2):343–349. doi:10.1378/chest.07-1361
16. Lindh A, Theander K, Arne M, et al. Errors in inhaler use related to devices and to inhalation technique among patients with chronic obstructive pulmonary disease in primary health care. Nurs Open. 2019;6(4):1519–1527. doi:10.1002/nop2.357
17. Postma DS, Bush A, van den Berge M. Risk factors and early origins of chronic obstructive pulmonary disease. Lancet Lond Engl. 2015;385(9971):899–909. doi:10.1016/S0140-6736(14)60446-3
18. Waatevik M, Skorge TD, Omenaas E, Bakke PS, Gulsvik A, Johannessen A. Increased prevalence of chronic obstructive pulmonary disease in a general population. Respir Med. 2013;107(7):1037–1045. doi:10.1016/j.rmed.2013.04.008
19. Xie M, Liu X, Cao X, Guo M, Li X. Trends in prevalence and incidence of chronic respiratory diseases from 1990 to 2017. Respir Res. 2020;21(1):49. doi:10.1186/s12931-020-1291-8
20. Ministerio de Saludy Protección Social L. Política De Atención Integral En Salud “Un sistema de salud al servicio de la gente” Grupo de Respiratorio en Atención Primaria - GRAP; 2016. Available from: https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/DE/modelo-pais-2016.pdf.
21. Aguilar-Barojas S. Fórmulas para el cálculo de la muestra en investigaciones de salud. Salud en Tabasco. 2005;11(1–2):333–338.
22. Gallego Acevedo JM, López Camacho D, Sepúlveda CE, editors. Los límites de la estratificación: en busca de alternativas. Bogotá: Editorial Universidad del Rosario; 2014. 1–21. Available from: http://books.scielo.org/id/yn4vh.
23. Giner J, Macian V, Hernandez C. Estudio multicéntrico y prospectivo de “educación y enseñanza” del procedimiento de inhalación en pacientes respiratorios (estudio Eden). Arch Bronconeumol. 2002;38:300–305. doi:10.1016/S0300-2896(02)75222-8
24. Pothirat C, Chaiwong W, Phetsuk N, Pisalthanapuna S, Chetsadaphan N, Choomuang W. Evaluating inhaler use technique in COPD patients. Int J Chron Obstruct Pulmon Dis. 2015;10(1):1291–1298. doi:10.2147/COPD.S85681
25. Al-Worafi YM. Evaluation of inhaler technique among patients with asthma and COPD in Yemen. J Taibah Univ Med Sci. 2018;13(5):488–490. doi:10.1016/j.jtumed.2018.06.002
26. Sulku J, Högman M, Ställberg B, et al. Incorrect inhaler technique is common in patients with COPD – data from the TIE study. Eur Respir J. 2016;48(suppl 60):67.
27. Dal Negro RW, Bonadiman L, Turco P. Prevalence of different comorbidities in COPD patients by gender and GOLD stage. Multidiscip Respir Med. 2015;10(1):24. doi:10.1186/s40248-015-0023-2
28. Melani AS, Bonavia M, Cilenti V, et al. Inhaler mishandling remains common in real life and is associated with reduced disease control. Respir Med. 2011;105(6):930–938. doi:10.1016/j.rmed.2011.01.005
29. Lavorini F, Magnan A, Christophe Dubus J, et al. Effect of incorrect use of dry powder inhalers on management of patients with asthma and COPD. Respir Med. 2008;102(4):593–604. doi:10.1016/j.rmed.2007.11.003
30. Duarte-de-Araújo A, Teixeira P, Hespanhol V, Correia-de-Sousa J. COPD: misuse of inhaler devices in clinical practice. Int J Chron Obstruct Pulmon Dis. 2019;14:1209–1217. doi:10.2147/COPD.S178040
31. Luczak-Wozniak K, Dabrowska M, Domagala I, et al. Mishandling of pMDI and DPI inhalers in asthma and COPD - Repetitive and non-repetitive errors. Pulm Pharmacol Ther. 2018;51:65–72. doi:10.1016/j.pupt.2018.06.002
32. Alsufyani AM. An evaluation of metered-dose inhaler administration technique among patients of asthma and chronic obstructive pulmonary disease in Saudi Arabia. Egypt J Chest Dis Tuberc. 2021;70(1):54. doi:10.4103/ejcdt.ejcdt_54_20
33. Cho-Reyes S, Celli BR, Dembek C, Yeh K, Navaie M. Inhalation Technique Errors with Metered-Dose Inhalers Among Patients with Obstructive Lung Diseases: a Systematic Review and Meta-Analysis of U.S. Studies. Chronic Obstr Pulm Dis Miami Fla. 2019;6(3):267–280.
34. Sanaullah T, Khan S, Masoom A, Mandokhail ZK, Sadiqa A, Malik MI. Inhaler Use Technique in Chronic Obstructive Pulmonary Disease Patients: errors, Practices and Barriers. Cureus. 2020;12(9):e10569. doi:10.7759/cureus.10569
35. Oliveira de PD, Menezes AMB, Bertoldi AD, Wehrmeister FC, Macedo SEC. Assessment of inhaler techniques employed by patients with respiratory diseases in southern Brazil: a population-based study. J Bras Pneumol. 2014;40:513–520. doi:10.1590/S1806-37132014000500007
36. Kim JS, Hashweh N, Li H, Choudhary S, Santosh S, Charbek E. Effectiveness of one-on-one coaching in improving pressurized metered dose inhaler (pMDI) technique among COPD patients: a prospective clinical study. BMC Pulm Med. 2021;21(1):266. doi:10.1186/s12890-021-01627-y
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.