Back to Journals » International Journal of General Medicine » Volume 15
Characteristics of Depression Clinical Trials Registered on ClinicalTrials.gov
Authors Liang J, He P, Wu H, Xu X , Ji C
Received 28 October 2022
Accepted for publication 19 December 2022
Published 29 December 2022 Volume 2022:15 Pages 8787—8796
DOI https://doi.org/10.2147/IJGM.S394143
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Luca Testarelli
Juan Liang,1 Peijie He,1 Hanting Wu,1 Xiujuan Xu,2 Conghua Ji1,3
1School of Public Health, Zhejiang Chinese Medical University, Hangzhou, 310053, People’s Republic of China; 2Tongde Hospital of Zhejiang Province, Hangzhou, 310012, People’s Republic of China; 3The First Affiliated Hospital of Zhejiang Chinese Medical University, Hangzhou, 310006, People’s Republic of China
Correspondence: Conghua Ji, Email [email protected]
Background: Mental disorders are among the leading causes of the global health-related burden, and depression is one of the most disabling mental disorders. The emergence of the COVID-19 pandemic has created an environment where many determinants of mental health are exacerbated. Many studies have been registered and conducted over the past 16 years, but how to choose the proper design for depression clinical trials remains the main concern. This study aimed to characterize the current status of global depression clinical trials registered on ClinicalTrials.gov.
Methods: We examined all the trials registered on ClinicalTrials.gov from 2007 to 2021.
Results: Overall, 7623 depression clinical trials were identified for analysis. Of those trials, 6402 (83.98%) were intervention trials and 1212 (15.90%) were observational trials. The majority of intervention types were behavioral (35.2%) and drug (28.55%), with very few procedures, dietary supplements, and diagnostic test studies. In addition, 55.53% of trials enrolled < 100 participants. The proportions of trials registered in North America were higher than on other continents. Furthermore, the trials that involved only females (12.6%) were more than only males (0.87%) from 2019 to 2021.
Conclusion: Depression clinical trials registered on ClinicalTrials.gov were dominated by small sample size trials, and there is a lack of trials related to COVID-19. The choice of study design is crucial, and properly designed trials can help improve study efficiency and reduce the likelihood of study failure. Given the increased number of RCT trials, the trial quality is gradually improving over the years. In addition, depression trials concentrating on children and older adults need more scientific attention. Further studies related to COVID-19 are needed, given the great damage that causes to people’s physical and mental health.
Keywords: depression, ClinicalTrials.gov, characteristics of depression clinical trials
Introduction
Depression1 is one of the critical mental disorders, characterized by high morbidity, high disability, high recurrence rate, and high suicide rate. Commonly, the main clinical characteristics of these patients are persistently low mood in which there is a feeling of sadness and loss of interest. Severe psychotic depression is often accompanied by cognitive and neurovegetative symptoms, such as difficulty in concentrating, memory alterations, anorexia, and sleep disturbances.2 For depression patient, symptoms persist over the long term and, when more severe, can impair quality of life and function.3 The proportion of the global population living with depression is estimated to be 322 million people—4.4% of the world’s population according to a new report, released by the World Health Organization.4 The Global Burden of Disease Study(GBD) 2017 revealed that depressive disorders are ranked as the third leading cause of “years lived with disability” worldwide,5 and the most disabling mental disorder was depressive, which ranked among the top 25 leading causes of burden worldwide in 2019.6
Numerous reports mentioned that depressive symptoms and fear have increased during the COVID-19 pandemic.7 A recent poll has shown that a significant number of Americans live in fear of the disease and COVID-19’s consequences.8 Some research indicates that family members who lost family or friends owing to COVID-19 can display acute post-traumatic stress disorder in which emotional numbness and insomnia are prevalent,9 and this condition may trigger the onset of depression. According to the report, long working hours, untimely emergency calls, a quarantined state, and separation from family and friends due to professional commitments put healthcare providers under extreme stress, anxiety, and frustration.10 All these factors greatly increase the risk of depression.
Usually, depression can be assessed using a dimensional approach, through self or clinician-rated questionnaires,11 such as the Hamilton Depression Rating Scale (HAM-D17, 21, 24 items),12 the Montgomery-Åsberg Depression Rating Scale (MADRS10),13 and the Quick Inventory of Depressive Symptomatology (QIDS) Clinician Rating (QIDS-C).14 Clinical trials generate important data on disease recognition and treatment, which can have significant medical, financial, and political implications. Yet, the search on depression may have been limited by the methodological heterogeneity of studies, leading to several published recommendations of ways to optimize clinical trial methodology in this field.15 The International Committee of Medical Journal Editors (ICMJE) advocated that clinical trials should be registered in a public registry before participants were recruited to ensure process transparency and legality.16 The ClinicalTrials.gov database provides the most comprehensive information about ongoing and completed clinical studies worldwide.17 As clinical trials are considered the gold standard for evaluating the safety and efficacy of therapeutics and generating evidence-based knowledge in medicine,18 a growing number of clinical studies have been conducted to examine the scientific evidence of depression. Conducting depression clinical trials is important to improve disease management. However, there is a lack of thorough evaluation of depression clinical trials. Thus, a better understanding of the current features of depression clinical trials is important for improving clinical trial designs and identifying neglected research areas. This understanding will improve the translatability of results into benefits for patients. The current analysis aims to describe the depression trial portfolio using ClinicalTrials.gov data, including trial attributes, enrollment, study design, location, and sponsor. Secondly, we aim to compare the relationship between depression interventions and medical conditions and describe trends in depression trials over time.
Materials and Methods
Data Sources and Search
We searched the database of ClinicalTrials.gov with the keyword “depression” without restriction on languages and study type. The earliest data were generated from 2006, for convenience in grouping and statistical analysis, the search time was limited from January 1, 2007 to December 30, 2021. The registration information of all relevant trials was downloaded. All available results were downloaded as XML files. Subsequently, all data was imported into an Excel form to facilitate further data selection, classification, and management.
Data Extraction
As previously described, trial data were self-reported by trial sponsors or investigators by using a web-based system. Data related to the following variables were independently extracted by two investigators from the downloaded registration information files, after which a third researcher checked the data. The following information was collected from each study: title, date of registration, locations, study type, study design, interventions and control, sponsor and collaborators, phases, sample size, outcomes, and recruiting status. The overall status of registered clinical trials on depression were reviewed and collated.
Study type was categorized as interventional, observational, and unknown. Study design was more refined and includes allocation: N/A, allocation: randomized, allocation: non-randomized, case-control, cohort, ecologic/community, family-based, other, and unknown. Patients’ age was classified as child, adult, and old adult. In terms of the type of intervention, device is a treatment device for depression and procedure is the diagnostic procedure of depression. If the original data is blank, we define it as “unknown”. The original data is incomplete and it is failure to know what “other” includes.
Data Analysis
We analyzed depression data for 2007–2021 and found a dramatic increase in depression clinical trial registrations after 2019, we decided to evaluate registrations for 2019–2021 to examine depression trials methodology.
We reported absolute numbers and percentages for categorical variables and compared them by using χ2 analysis. Analyses were conducted on gender, age, enrollment, design, study type, and locations.
Results
General Characteristics of Registered Trials
From January 1, 2007, to December 30, 2021, a total of 7623 registered clinical trials were retrieved from the Clinicaltrials.gov database. We found an increasing number of trials registered for depression from 2007 to 2021. There were 355 trials in 2007–2009, 557 trials in 2010–2012, 1162 trials in 2013–2015, 1772 trials from 2016–2018, and 3777 trials in 2019–2021. Furthermore, there is a dramatic increase in the number of trials from 2016 to 2021 (Table 1 and Figure 1). The proportion of drug intervention trials decreased over time: from 54.37% in 2007–2010 to 19.94% in 2019–2021. Behavioral intervention trials are increasing in importance because of an increasing proportion of the intervention types from 2007 to 2021: from 15.77% in 2007–2010 to 39.95% in 2019–2021. In addition, there were more behavioral trials (39.95%) than drug trials (19.94%) in 2019–2021. At the same time, the proportion of devices was 11.41%, for example, brain stimulation, which is a potential treatment for non-treatment resistant depression.19 Most depression trials (55.53%) were small sample sizes, enrolling <100 subjects, although some of the trials had an anticipated enrollment of 5000 or more participants (1.50%) in 2007–2021. A substantial proportion of depression studies were interventional (82.5%), and the proportion of observational experiments was only 17.29% in 2019–2021. The majority of depression trials were in North America (52.18%), and the second was in Europe (21.55%) which is more than in Asia and South America (12.97% and 1.84%) from 2007 to 2021. And there was a subtle increase in the proportion of trials in Asia: from 11.27% in 2007–2010 to 14.51% in 2019–2021, and the proportion in North America increased from 45.96% to 50.99%.
 |
Table 1 Characteristics of All Included Studies |
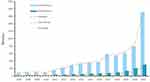 |
Figure 1 The trend of registered depression studies on ClinicalTrials.gov. |
Montgomery-Asberg Depression Rating Scale, Quick Inventory of Depressive Symptoms (QIDS), Hamilton Anxiety Rating Scale (HAM-A) and Clinical Global Impression of Severity (CGI-S) were mainly used as outcome measures in the included depression trials.
Table 2 summarized the trials design characteristics for depression trials in 2019–2021. The total number of depression trials registered was 3777. There was a great increase in the number: from 757 in 2019 to 2014 in 2021. Within 3777 depression trials, the intervention studies were much more than the observational studies, and the number of interventional studies and observational studies were 3116 (82.50%) and 653 (17.29%), respectively. Most depression trials involved adults (93.65%), and 14.75% involved children (14.75%). Furthermore, a great part of depression trials involved all gender (82.26%). It was obvious that more trials involved only females (12.60%) than only males (0.87%) in depression experiments (Figure 1). And the proportion of trials involving only females increased from 11.76% to 13.36%, and trials that involved only males increased from 0.66% to 0.84%. Among all the clinical trials, there were 140 (3.7%) trials related to COVID-19.
 |
Table 2 In-Depth Study Characteristics of Depression Studies in 2019–2021 |
Study Design of Registered Trials
Table 3 compares the study design of interventional studies (3122,82.66%) and observational studies (646,17.1%) in 2019–2021. Interventional trials were classified into four categories: allocation: N/A, allocation: randomized, allocation: non-randomized and unknown, and observational trials which means non-randomized comparative studies were classified into six categories: case-control, cohort, ecologic/community, family-based, other and unknown. The proportion of interventional studies increased from 81.77% to 84. 76% and observational studies decreased from 17.17% to 15.24%. Randomized allocation studies (2430,77.83%) accounted for the largest part of the interventional studies, and there were 337 (52.17%) cohort studies in the observational studies. Comparing four categories of depression interventional trials from 2019 to 2021, N/A allocation studies increased from 12.81% to 14.35%; randomized allocation studies increased from 62.75% to 65.54%; non-randomized allocation studies decreased from 6.08% to 4.87%.
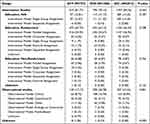 |
Table 3 Design of Depression Studies in 2019–2021 |
Locations of Registered Trials
According to the statistics, from 2007 to 2021, North America (52%) accounts for the largest proportion, followed by Europe (22%) (Figure 2). Table 4 demonstrates the locations of registered depression trials in 2019–2021. The total number of registered trials in the three years was 757, 1006, and 2014 respectively. Comparing the six continents of the world from 2019 to 2021, the number of trials in North America has increased from 383(50.59%) to 1006(52.93%); the number of trials in Europe has increased from 163(21.53%) to 447(22.19%); the trials number of Asia has increased from 118(15.59%) to 267 (13.26%). In 2019–2021, most depression trials were in North America in 1926(50.99%), and the United States accounts for 82.81% of them. In addition, the number in Europe and Asia were 855(22.64%) and 548(14.51%). As is shown in Table 4, 163(21.53%) trials belonged to Europe in 2019, and Europe studies accounted for a proportion (24.35%) of clinical trials launched in 2020 and gradually decreased. Chinese takes the largest (242,44.16%) accounting for part of the Asia depression trials.
 |
Table 4 Locations of Depression Studies |
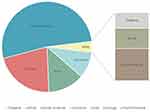 |
Figure 2 Locations of depression studies from 2007 to 2021. |
Discussion
This analysis provides a snapshot of the landscape of depression clinical trials registered on ClinicalTrials.gov, which results provide the basis for the treatment and prevention of diseases within depression, as well as the characteristics of trial design, location, and intervention type.
Depression trials accounted for a growing proportion of of all medical trials (Table 5). There is an urgent need for more effective treatment of depression, not only the disorder is becoming more common, but also it is associated with major health and economic burdens.20 In this study, by comparing essential key characteristics of proper testing and development of depression experiments, several noteworthy observations emerged. We found that depression trials were small in scale, and the majority of studies (55.53%) on ClinicalTrials.gov typically enrolled 100 or fewer patients, and only several studies (1.5%) enrolled 5000 and more patients. Typically, small studies have a high risk of type II error, that is failure to reject the null hypothesis and inappropriately concluding that a treatment or intervention is ineffective when the sample size is too small to determine a significant effect.21,22 These findings raise concerns that the growing depression patient population may still not be receiving the attention, funding, or efforts necessary to identify new therapies.
 |
Table 5 The Percentage of Depression Trials in All Medical Trials |
The statistics in our analysis also showed that interventional studies accounted for the largest portion of clinical trials on depression in the last 3 years, and most interventional trials in depression are on non-responsive depression.23 Although the observational type is also important for generating hypotheses, properly designed RCTs are needed to substantiate effective therapies.22 In contrast, observational studies were decreased because they often summarize and analyze the existing clinical data in clinical work in a retrospective way, and researchers did not randomize patients to control intervention measures.24 Appropriate selection of study design is only one element of a successful study. The choice of study design should take into account cost, access to cases, identification of exposures, epidemiologic measures needed, and the current level of published evidence on the particular exposure-outcome relationship being evaluated.25
We classified medical conditions to examine links between depression interventions and conditions. It shows that depression trials were significantly more likely to focus on behavioral trials than drug trials. Overall, almost 60% of depression trials focus on two therapeutic areas. Some prior reviews have reported that cognitive behavioral therapy as a first-line psychological treatment can effectively improve the symptoms of moderate depression.26 The maximal proportion of behavioral intervention trials was 39.95%, and drug intervention accounted for only 19.94% in the same period. In the past six years, Although the quantity of trials has increased sharply, the proportion of behavioral intervention was increased, but drug intervention was decreased. During the pandemic, most trials temporarily ceased recruitment.27 But online assessments are becoming increasingly popular.28 Thus, it was feasible to recruit and deliver behavioral interventions online.
Through a contemporary review of clinical trials registered for depression, the current findings show that an increasing number of depression trials are available at ClinicalTrials.gov, especially in the United States. It indicates the high priority given to depression by researchers in the United States, which remains the country with the most depression clinical trials conducted, followed by Canada. On the one hand, the incidence rate of depression is the highest in the United States, which is 16.1%.29,30 On the other hand, the United States, as a developed country, ranks first in the world in terms of investment in scientific research.31
In addition, a notable finding is the 32% and 100% growth rates in the number of trials from 2019 to 2020 and 2020 to 2021. This figure indicates an explosive growth in depression trials worldwide in 2021. Also, COVID-19-related studies in depression trials start to appear and gradually increase in 2020. This could be due to two reasons. First, from the latest published article, the prevalence of depression increased to 4, 802.4/100,000 after the COVID-19 outbreak, which means that 374 million people in the world are suffering from depression. In other words, the pandemic increased the prevalence of depression by about 76 million in 2020. In 2021, there are more than 350 million people with depression worldwide.6,32 That means it is imperative to conduct more research related to depression, such as providing useful tools and recommendations for improving the efficiency, quality, monitoring, and reporting of clinical trials.33
It should be noted that the largest proportion of trials was conducted on adults, followed by the elderly. In addition, we found that some subjects were children. Nationally, representative, epidemiological studies have shown that the lifetime prevalence of depression among adolescents aged 15 to 18 years ranges from 11% to 14%. It is also estimated that approximately half of the first episodes of depression occurred during adolescence.34 These articles suggest that a large proportion of adolescents will suffer from depression during their formative years.35,36 In addition, within the last 3 years, the proportion of trials in females was much higher than in males, as the prevalence of depression and anxiety was higher in women than in men worldwide before COVID-19.6 Women’s psychology is more vulnerable to social and economic changes. Compared with men, women are about twice as likely to suffer from depression.37 During their reproductive years, women are 1.5 to 3 times more likely to suffer from current and lifetime unipolar depression than men.38 Since COVID-19, the differences in depression and anxiety disorders between men and women have been further amplified.39 Therefore, it is necessary to pay more attention to the research on female depression.
While our study is unique, it has some limitations. For trials with fewer than 100 participants, it was difficult to identify how many of these trials were explicitly registered as pilots or feasibility trials. Information was not available on whether the female-only trials were conducted among patients with postpartum depression or postmenopausal women. ClinicalTrials.gov does not include all trials conducted worldwide. In addition, trials may not be included in our analysis if essential elements or keywords were not included at the time of registration. Misclassification may lead to some inappropriate conclusions. However, our study process attempted to minimize these potential biases. Trial design, implementation, and results must be transparent, and then the results must be rapidly disseminated to clinical practice.
Conclusions
In summary, our research suggests that temporary depression trials are not only small in sample size but also the number of trials. With the increase in the number of depressed patients in recent years, more comprehensive trials are urgently needed. First of all, the choice of study design is crucial, properly designed trials can help improve study efficiency and reduce the likelihood of study failure. Given the increased number of RCT trials, the trial quality is gradually improving over the years. Secondly, depression trials concentrating on children and older adults need more scientific attention. Further studies related to COVID-19 are needed, given the great damage that causes to people’s physical and mental health.
Data Sharing Statement
This study is based on a public database and is not suitable for the approval of the ethics committee.
Acknowledgments
Authors’ contributions: C.H.J., and J.L. were responsible for the concept and design of the study; X.J.X., P.J.H., and H.T.W. were responsible for data acquisition; H.T.W., X.J.X., and J.L. were responsible for statistical analysis; C.H.J. and J.L. were responsible for the interpretation of results, and C.H.J. and J.L. analyzed the data and drafted the manuscript. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Health Commission of Zhejiang Province (No. 2019KY348 and 2021KY606), the People’s Republic of China.
Disclosure
The authors declare no financial or other conflicts of interest.
References
1. McCarron RM, Shapiro B, Rawles J, et al. Depression. Ann Intern Med. 2021;174(5):Itc65–itc80. doi:10.7326/AITC202105180
2. American Psychiatric Association. Practice guideline for the treatment of patients with major depressive disorder (revision). Am J Psychiatry. 2000;157(4 Suppl):1–45.
3. Park SC, Sakong J, Koo BH, et al. Clinical significance of the number of depressive symptoms in major depressive disorder: results from the CRESCEND study. J Korean Med Sci. 2016;31(4):617–622. doi:10.3346/jkms.2016.31.4.617
4. Friedrich MJ. Depression Is the Leading Cause of Disability Around the World. JAMA. 2017;317(15):1517.
5. Roberts NL, Mountjoy-Venning WC, Anjomshoa M, Banoub JA, Yasin YJ. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–1858. doi:10.1016/S0140-6736(18)32279-7
6. Santomauro DF, Mantilla Herrera AM, Shadid J. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–1712. doi:10.1016/S0140-6736(21)02143-7
7. Sanwald S, Widenhorn-Müller K, Gahr M, et al. Primary emotions as predictors for fear of COVID-19 in former inpatients with Major Depressive Disorder and healthy control participants. BMC Psychiatry. 2022;22(1):94. doi:10.1186/s12888-021-03677-2
8. Li R. Fear of COVID-19: what causes fear and how individuals cope with it. Health Commun. 2021;2021:1–10.
9. Stamu-O’Brien C, Carniciu S, Halvorsen E, et al. Psychological aspects of COVID-19. J Cosmet Dermatol. 2020;19(9):2169–2173. doi:10.1111/jocd.13601
10. Khanagar SB, Ramya HK, Vishwanathaiah S, et al. Depression, Anxiety, and Psychological Distress among healthcare providers during the outbreak of the life-threatening coronavirus disease (COVID-19). J Contemp Dent Pract. 2020;21(5):471–472. doi:10.5005/jp-journals-10024-2836
11. Ferreira MF, Castanheira L, Sebastião AM, et al. Depression assessment in clinical trials and pre-clinical tests: a critical review. Curr Top Med Chem. 2018;18(19):1677–1703. doi:10.2174/1568026618666181115095920
12. Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23(1):56–62. doi:10.1136/jnnp.23.1.56
13. Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134(4):382–389. doi:10.1192/bjp.134.4.382
14. Rush AJ, Trivedi MH, Ibrahim HM, et al. The 16-item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54(5):573–583. doi:10.1016/S0006-3223(02)01866-8
15. Turner EH, Matthews AM, Linardatos E, et al. Selective publication of antidepressant trials and its influence on apparent efficacy. N Engl J Med. 2008;358(3):252–260. doi:10.1056/NEJMsa065779
16. DeAngelis C, Drazen JM, Frizelle FA, et al. [Registration of clinical trials: a statement from the International Committee of Medical Journal Editors]. Ned Tijdschr Geneeskd. 2004;148(38):1870–1871. Dutch.
17. Zwierzyna M, Davies M, Hingorani AD, et al. Clinical trial design and dissemination: comprehensive analysis of clinicaltrials.gov and PubMed data since 2005. BMJ. 2018;361:k2130. doi:10.1136/bmj.k2130
18. Akobeng AK. Understanding randomised controlled trials. Arch Dis Child. 2005;90(8):840–844. doi:10.1136/adc.2004.058222
19. Mutz J, Edgcumbe DR, Brunoni AR, et al. Efficacy and acceptability of non-invasive brain stimulation for the treatment of adult unipolar and bipolar depression: a systematic review and meta-analysis of randomised sham-controlled trials. Neurosci Biobehav Rev. 2018;92:291–303. doi:10.1016/j.neubiorev.2018.05.015
20. Rasendran C, Imran Y, Talcott KE. Incremental economic burden of depression in ophthalmic patients. Am J Ophthalmol. 2021;229:184–193. doi:10.1016/j.ajo.2021.03.062
21. Chen J, Huang J, Li JV, et al. The characteristics of TCM clinical trials: a systematic review of ClinicalTrials.gov. Evid Based Complement Alternat Med. 2017;2017:9461415. doi:10.1155/2017/9461415
22. Inrig JK, Califf RM, Tasneem A, et al. The landscape of clinical trials in nephrology: a systematic review of Clinicaltrials.gov. Am J Kidney Dis. 2014;63(5):771–780. doi:10.1053/j.ajkd.2013.10.043
23. Sforzini L, Worrell C, Kose M, et al. A Delphi-method-based consensus guideline for definition of treatment-resistant depression for clinical trials. Mol Psychiatry. 2022;27(3):1286–1299. doi:10.1038/s41380-021-01381-x
24. Turner DP, Houle TT. Observational Study Designs. Headache. 2019;59(7):981–987. doi:10.1111/head.13572
25. Thiese MS. Observational and interventional study design types; an overview. Biochem Med. 2014;24(2):199–210. doi:10.11613/BM.2014.022
26. Liu Z, Qiao D, Xu Y, et al. The efficacy of computerized cognitive behavioral therapy for depressive and anxiety symptoms in patients with COVID-19: randomized controlled trial. J Med Internet Res. 2021;23(5):e26883. doi:10.2196/26883
27. Neumann S, Henderson E. A snapshot of the response from UK-based clinical trials of investigational medicinal products to COVID-19. Cureus. 2020;12(9):e10613. doi:10.7759/cureus.10613
28. Khan MA, Vivek V, Khojah M, et al. Learners’ perspective towards E-Exams during COVID-19 outbreak: evidence from Higher Educational Institutions of India and Saudi Arabia. Int J Environ Res Public Health. 2021;18(12):6534. doi:10.3390/ijerph18126534
29. Mojtabai R, Amin-Esmaeili M, Spivak S, et al. Remission and treatment augmentation of depression in the United States. J Clin Psychiatry. 2021;82(6). doi:10.4088/JCP.21m13988
30. Liu X, Mukai Y, Furtek CI, et al. Epidemiology of treatment-resistant depression in the United States. J Clin Psychiatry. 2021;83(1). doi:10.4088/JCP.21m13964
31. Im EO, Sakashita R, Oh EG, et al. COVID-19 and nursing research across five countries/regions: commonalities and recommendations. Res Nurs Health. 2021;44(5):758–766. doi:10.1002/nur.22171
32. Li DJ, Hsu ST, Chou FH, et al. Predictors for depression, sleep disturbance, and subjective pain among inpatients with depressive disorders during the COVID-19 pandemic: a cross-sectional study. Int J Environ Res Public Health. 2021;18:12.
33. Grignolo A. The Clinical Trials Transformation Initiative (CTTI). Ann Ist Super Sanita. 2011;47(1):14–18. doi:10.4415/ANN_11_01_04
34. Mendelson T, Tandon SD. Prevention of Depression in Childhood and Adolescence. Child Adolesc Psychiatr Clin N Am. 2016;25(2):201–218. doi:10.1016/j.chc.2015.11.005
35. Rice F, Riglin L, Lomax T, et al. Adolescent and adult differences in major depression symptom profiles. J Affect Disord. 2019;243:175–181. doi:10.1016/j.jad.2018.09.015
36. Hauenstein EJ. Depression in adolescence. J Obstet Gynecol Neonatal Nurs. 2003;32(2):239–248. doi:10.1177/0884217503252133
37. Stepanikova I, Acharya S, Abdalla S, et al. Gender discrimination and depressive symptoms among child-bearing women: ELSPAC-CZ cohort study. EClinicalMedicine. 2020;20:100297. doi:10.1016/j.eclinm.2020.100297
38. Copeland WE, Worthman C, Shanahan L, et al. Early pubertal timing and testosterone associated with higher levels of adolescent depression in girls. J Am Acad Child Adolesc Psychiatry. 2019;58(12):1197–1206. doi:10.1016/j.jaac.2019.02.007
39. Pérez-Cano HJ, Moreno-Murguía MB, Morales-López O, et al. Anxiety, depression, and stress in response to the coronavirus disease-19 pandemic. Cir Cir. 2020;88(5):562–568. doi:10.24875/CIRU.20000561
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
