Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 15
Characteristics of Atopic Dermatitis Patients Treated with Crisaborole: Real-World Data from a Large Healthcare Provider Database in Israel
Authors Weil C, Adiri R, Chodick G, Gersten M, Cohen Barak E
Received 7 February 2022
Accepted for publication 17 May 2022
Published 30 June 2022 Volume 2022:15 Pages 1205—1211
DOI https://doi.org/10.2147/CCID.S359625
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jeffrey Weinberg
Clara Weil,1,* Roni Adiri,2,* Gabriel Chodick,1,3 Merril Gersten,2 Eran Cohen Barak4,5
1Maccabitech Institute for Research and Innovation, Maccabi Healthcare Services, Tel Aviv, Israel; 2Pfizer Israel, Herzliya Pituah, Israel; 3Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel; 4Dermatology Department, Emek Medical Center, Afula, Israel; 5Bruce and Ruth Rappaport Faculty of Medicine, Technion, Haifa, Israel
*These authors contributed equally to this work
Correspondence: Gabriel Chodick, Maccabitech Institute for Research and Innovation, Maccabi Healthcare, Keufmann 4 St, Tel Aviv, 68125, Israel, Tel +972-514-3755, Email [email protected]
Background: In recent years, new treatments dedicated to atopic dermatitis (AD) have become available in Israel, including crisaborole, a small molecule with unique benzoxaborole chemistry.
Objective: To describe baseline characteristics, history of AD therapies, and use of health-care services of early crisaborole users in real-world settings.
Methods: A retrospective cohort study was performed using the data of a large health provider in Israel. AD patients treated with crisaborole since it became commercially available in Israel in July 2019 through end of Sep 2020, were included. Baseline demographics and clinical characteristics, prior AD-related treatments and healthcare resource utilization were collected.
Results: A total of 441 patients were included (57.8% females, median age = 21.1y; interquartile range = 10.5– 40.8). In 62.1%, a dermatologist prescribed the first dispensed crisaborole. Median time from AD diagnosis to crisaborole treatment was 6.6 years. Up to 12 months prior to crisaborole treatment, low-, mid- and high-potency TCS were used by 30.8%, 31.1% and 55.8% of patients, respectively. Treatments related to moderate-to-severe AD were dispensed to 38.5% of patients in the prior 5 years. Asthma and allergic rhinitis were documented among 22.2% and 37.2%, respectively. In the past year, patients had a median of 9 visits to primary care physicians, 84.6% visited a dermatologist (≥ 5 visits: 12.9%).
Conclusion: While crisaborole is indicated for mild-to-moderate disease, results suggest that a significant proportion of patients had history of advanced AD therapies suggestive of moderate-to-severe AD.
Keywords: atopic dermatitis, topical calcineurin inhibitors, real-world data
Introduction
Atopic dermatitis (AD) is a chronic inflammatory disease, which manifests with erythematous, eczematous lesions accompanied by significant pruritus. Estimates of the prevalence of AD vary across studies and settings, with a reported range of 0.2–36% in pediatric populations (ages <18 years) and 1.2–22.7% among adults.1–5 Considering that approximately 85–94% of patients with AD suffer from mild to moderate disease,5,6 there is need for additional topical treatment options.
In the last decades, two main topical therapies were prescribed to alleviate the symptoms of AD – topical corticosteroids (TCS) and topical calcineurin inhibitors (TCI). Despite their efficacy, local guidelines in Israel recommend to restrict long-term use with TCS due to cutaneous and systemic adverse reactions, and to limit the use of TCI due to application site reactions.7 Crisaborole, a small molecule with unique benzoxaborole chemistry,8,9 is a recently developed topical treatment for AD,10 which selectively inhibits phosphodiesterase 4 enzyme.11 Crisaborole 2% ointment was approved by the FDA in 2016 and subsequently by Israel’s Ministry of Health. It became commercially available in Israel in July 2019 and is indicated for topical treatment of mild to moderate atopic dermatitis in patients 2 years of age and older.
Crisaborole demonstrated efficacy (defined by Investigator’s Static Global Assessment [ISGA] score of 2–3), safety and improvement in quality of life of mild-to-moderate AD patients in its pivotal studies.12 To date, real-world data regarding crisaborole effectiveness and safety, or clinical characteristics of patients treated with crisaborole, are limited. Therefore, this study aimed to describe baseline characteristics, previous treatment lines, and use of health-care services among early crisaborole users in a large health-care provider database in Israel.
Methods
Study Design & Data Source
A retrospective cohort study was performed using data extracted from the Maccabi Health Services (MHS) database. MHS is the second largest of four state-mandated health funds (not-for-profit; payer and provider) in Israel, with a nationally-representative sample of approximately a quarter of the population. The MHS database contains longitudinal data computerized since 1998 on a stable population of >2.6 million members. Data are automatically collected and include comprehensive laboratory data from a single central laboratory, full pharmacy prescription and purchase data, and extensive demographic data on each patient. MHS uses the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) coding systems as well as self-developed coding systems to provide more granular diagnostic information beyond the ICD codes. Medications are coded according to the Israeli coding system with translations to Anatomical Therapeutic Chemical coding system wherever available. Procedures are coded using Current Procedural Terminology (CPT) codes.
Study Population
The cohort of early users of crisaborole included all MHS members (all ages) who initiated crisaborole (at least one dispensed prescription) from July 2019 through 30/9/2020, with at least 12 months’ prior enrolment in MHS. Patients without a diagnosis code for AD (ICD-9691.8) were excluded from the analysis of the main cohort of AD patients treated with crisaborole (ie, patients treated for a non-AD indication or missing AD data).
Study Variables and Definitions
The following baseline data (before/at crisaborole initiation date) were obtained to describe patient characteristics at crisaborole initiation. Sociodemographic characteristics included age, sex, and socioeconomic status (SES) linked to neighborhood of residence. SES was based on a score ranked with 1 (lowest) to 10 derived for commercial purposes by Points Location Intelligence using geographic information systems and data such as expenditures related to retail chains, credit cards and housing. This score is highly correlated with SES measured by the Central Bureau of Statistics.13 SES was categorized into low (1–4), medium (5–6) and high (7–10).
For the first dispensed crisaborole prescription, prescribing physician specialty was described, including dermatology, allergy/immunology, and primary care physician (PCP; defined as pediatricians and family physicians). AD disease duration was estimated as the time between the earliest AD diagnosis code and the start of crisaborole treatment.
Prior AD-related treatment use was described, based on at least 1 dispensed medication or treatment code (baseline periods of interest: prior 5 years; prior 12 months). The specific indication for treatment was not available (for example, low potency TCS may be given for multiple indications). In order to limit the inclusion of other potential indications, medications dispensed prior to the earliest AD diagnosis code were excluded. AD-related medications included topical calcineurin inhibitors (TCI; pimecrolimus, tacrolimus), topical corticosteroids (TCS), systemic immunosuppressants (SI; including methotrexate, azathioprine, cyclosporine, mycophenolate mofetil, and systemic corticosteroids), and biologic treatments (dupilumab). Methotrexate purchases were restricted to 2.5mg tablets to limit inclusion of high-dose treatments for non-AD indications. TCS potency definitions were adapted from the 7 groups used in Israeli clinical guidelines7 and classified as low (VI–VII), mid (IV–V) or high (I–III) potency. Phototherapy was captured using procedural (CPT) codes. AD disease severity was estimated using dispensed treatments up to 5 years prior to crisaborole initiation (sensitivity analysis: 12 months): moderate-to-severe AD was defined by at least 1 dispensed SI or biologic, or phototherapy, with the remaining patients defined as mild AD.
Baseline asthma (ICD-9493.xx) and allergic rhinitis (477.xx) were based on the following definition: ≥1 diagnosis from a relevant specialist, hospital or MHS Medication Approval Committee, or ≥2 diagnoses from a PCP. Asthma and allergic rhinitis were described during two baseline periods of interest: ever (since 1998), and in the prior 5 years (“ever” met the main definition and had ≥1 recent diagnosis code prior to crisaborole initiation).
Data on healthcare resource utilization (HCRU) up to 12 months prior to crisaborole initiation were obtained, including the frequency of visits to PCP and specialists (dermatology, allergy/immunology), and hospitalization (admissions for a duration of at least 1 night, for any cause).
Statistical Methods
The cumulative number of AD patients treated with crisaborole was described over time during the study period. Descriptive statistics are presented as n (%) or median (interquartile range [IQR]). Baseline annual HCRU was summarized as follows: n (%) patients who used ≥1 unit of a given resource per year (ie, “users” of a resource, such as ≥1 visit/year) and, among users of a given resource, the quantity used (eg, number of visits/year) was summarized as median (IQR). Results were stratified by age group of interest at crisaborole initiation: <12, 12–17, and ≥18 years old.
The study protocol was approved by the Maccabi Healthcare Services institutional review board (reference number: 0120–20-MHS) and a waiver of informed consent was granted. The authors confirm that the guidelines outlined in the Declaration of Helsinki were followed.
Results
Among 542 MHS members treated with crisaborole in the study period, 441 eligible AD patients treated with crisaborole were included in the study population (Supplementary Material, Figure S1). Over time, the increase in the AD crisaborole cohort size was relatively constant (Supplementary Material, Figure S2).
The median age at crisaborole initiation was 21.1 (IQR = 10.5–40.8) years, with adults (≥18 years) accounting for 54.9% of the cohort. Table 1 includes baseline socio-demographic characteristics and comorbidities by age group and Figure 1 depicts the age and sex distribution of treated patients. While women accounted for 57.8% of crisaborole users overall, differences in the sex distribution were larger in the age group 20–39 years. The majority (68.2%) of crisaborole users resided in areas with high socioeconomic status. Asthma and allergic rhinitis were documented among 22.2% and 37.2%, respectively.
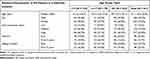 |
Table 1 Baseline Socio-Demographic Characteristics and Comorbidities of AD Patients at Crisaborole Initiation (N = 441) |
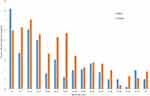 |
Figure 1 Age and sex-specific proportion of AD patients treated with crisaborole in MHS through September 2020 (N = 441). |
Dermatologists prescribed the majority of patients’ initial crisaborole purchases overall (62.1%), particularly among adults (70.7%). Among children (<12 years) and adolescents (12–17 years), initial prescriptions by a dermatologist accounted for 48.8% and 57.1%, respectively (Figure 2).
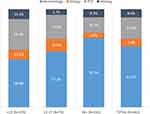 |
Figure 2 Specialty of the physician who prescribed the first dispensed crisaborole prescription among AD patients, by age group (N = 441). |
At the time of crisaborole initiation, patients had a median AD duration of 6.6 (IQR = 1.5–15.2) years overall, 2.7 (IQR = 0.9–5.2) among children aged <12 years and 10.8 (IQR = 2.0–18.7) years among adults (Table 2). Up to 12 months prior to crisaborole treatment, low-, mid- and high-potency TCS were used by 30.8%, 31.1% and 55.8% of patients, respectively. A total of 31.1% of patients had 2 or more dispensed high-potency TCS in the past year (Supplementary Material, Table S1, which includes additional results regarding the quantity of TCS dispensed by potency and age). Overall, 38.5% of patients (and 47.1% of adults) had a history of treatments related to moderate-to-severe AD (SI, biologic or phototherapy) up to 5 years prior to crisaborole treatment (Table 2). These patients with treatment patterns suggestive of moderate-to-severe AD were more likely to have a history of asthma and allergic rhinitis (Supplementary Material, Table S2).
 |
Table 2 Baseline Disease Characteristics and Prior Treatments of AD Patients at Crisaborole Initiation (N = 441) |
In the prior 12 months, 84.6% of patients had ≥1 dermatologist visit, and 46.0% of patients had ≥10 PCP visits. The percentage of patients who saw a dermatologist 2–4 and ≥5 times during the year was 41.5% and 12.9%, respectively (Table 3). A total of 5.2% of patients were hospitalized for any cause in the 12 months prior to crisaborole treatment.
 |
Table 3 Baseline HCRU of AD Patients at Crisaborole Initiation (N = 441) |
Discussion
Using electronic health-care data from a large health-care provider, this study provides real-world data characterizing early users of crisaborole in Israel. Overall, crisaborole users had a median AD duration of 6.6 years and children and adolescents accounted for almost half of new users. Women comprised the majority of crisaborole users aged 12 years and older. In age groups 20–39, relatively higher utilization by women may be indicative of increased awareness and concern related to the use of TCS in women of reproductive age. Pediatric and adult crisaborole users were characterized by a relatively high socioeconomic status. This is consistent with previous research from MHS and globally indicating that AD prevalence increases with SES, while AD disease severity is associated with lower SES, with awareness, access to care, and hygiene/environmental factors potentially driving this association.5,14 The distribution of SES in the present cohort also reflects the fact that access to crisaborole during the study period was constrained by cost as it was not included in Israel’s National Basket of Health Services at the time of the study.
While crisaborole is indicated for mild to moderate AD (defined by ISGA score of 2–3), we observed a relatively high proportion of patients in our study (38.5%) with treatment patterns in the prior 5 years that were suggestive of moderate-to-severe AD. In addition, in the year prior to crisaborole initiation, almost a third of patients used 2 or more high-potency TCS and more than half of the patients were seen by a dermatologist at least twice. Taken together, these results suggest that a substantial proportion of this cohort had active disease and treatment use suggestive of moderate-to-severe AD, whereas the registered treatment indication was for mild-to-moderate AD. Perhaps, as a new treatment modality, crisaborole was considered by physicians only after failure of the familiar TCS/TCI treatments. It is also possible that the relatively high costs of crisaborole discouraged its use for milder disease, such that crisaborole was more likely to be considered as a rescue treatment for patients with active or moderate-to-severe disease.
Several methodological limitations should be noted. AD severity scoring was not available as it is not routinely used in clinical practice or consistently reported. Our definition of moderate-to-severe AD based on recent use of SI, biologics and/or phototherapy may be subject to misclassification and did not distinguish between moderate and severe disease. In addition, as data on treatment indications were not available, some prior treatments (eg, topical or systemic corticosteroids) may have been prescribed for indications other than AD. Nonetheless, though systemic corticosteroids are not generally recommended for AD,15 they are still frequently prescribed to treat moderate-to-severe AD. Breakdown of treatment patterns within the SI/biologic group was not available for this analysis. Finally, follow-up data on treatment effectiveness and safety data were beyond the scope of this analysis. These results underscore the importance of real-world studies to better understand the baseline characteristics of patients and inform future studies of treatment effectiveness.
Conclusions
This study provides real-world data on the characteristics of the first cohort of AD patients treated with crisaborole since its approval in Israel. While crisaborole is indicated for mild-to-moderate disease, results suggest that a significant proportion of these patients had moderate-to-severe disease. This may inform further real-world analyses of crisaborole effectiveness.
Acknowledgment
This research was sponsored by Pfizer. We would like to acknowledge Dr. Matanya Tirosh for helpful discussions during the preparation of this manuscript.
Disclosure
Dr Roni Adiri reports being an employee of Pfizer, outside the submitted work; Professor Gabriel Chodick reports grants from Merck, during the conduct of the study; Dr Merril Gersten reports owning Pfizer stock and is employed by Pfizer. The authors report no other conflicts of interest in this work.
References
1. Bylund S, Kobyletzki L, Svalstedt M, et al. Prevalence and incidence of atopic dermatitis: a systematic review. Acta Derm Venereol. 2020;100(12):adv00160. doi:10.2340/00015555-3510
2. Mathiesen SM, Thomsen SF. The prevalence of atopic dermatitis in adults: systematic review on population studies. Dermatol Online J. 2019;25(8). doi:10.5070/D3258045124
3. Nutten S. Atopic dermatitis: global epidemiology and risk factors. Ann Nutr Metab. 2015;66(Suppl 1):8–16. doi:10.1159/000370220
4. Wang J, Ramette A, Jurca M, et al. Association between breastfeeding and eczema during childhood and adolescence: a cohort study. PLoS One. 2017;12(9):e0185066. doi:10.1371/journal.pone.0185066
5. Weil C, Sugerman PB, Chodick G, et al. Epidemiology and economic burden of atopic dermatitis: real-world retrospective data from a large nationwide Israeli Healthcare Provider Database. Adv Ther. 2022;39:1–13.
6. Silverberg JI, Simpson EL. Associations of childhood eczema severity: a US population-based study. Dermatitis. 2014;25(3):107–114. doi:10.1097/DER.0000000000000034
7. Israeli Dermatology Association. Guidelines for the Treatment of Atopic Dermatitis. Israeli Medical Association; 2020.
8. Jarnagin K, Chanda S, Coronado D, et al. Crisaborole topical ointment, 2%: a nonsteroidal, topical, anti-inflammatory phosphodiesterase 4 inhibitor in clinical development for the treatment of atopic dermatitis. J Drugs Dermatol. 2016;15(4):390–396.
9. Kelly KA, Feldman SR. A wealth of new topicals for atopic dermatitis. J Dermatol Treat. 2021;32(6):575. doi:10.1080/09546634.2021.1956770
10. Guttman-Yassky E, Hanifin JM, Boguniewicz M, et al. The role of phosphodiesterase 4 in the pathophysiology of atopic dermatitis and the perspective for its inhibition. Exp Dermatol. 2019;28(1):3–10. doi:10.1111/exd.13808
11. Paller AS, Tom WL, Lebwohl MG, et al. Efficacy and safety of crisaborole ointment, a novel, nonsteroidal phosphodiesterase 4 (PDE4) inhibitor for the topical treatment of atopic dermatitis (AD) in children and adults. J Am Acad Dermatol. 2016;75(3):494–503.e6. doi:10.1016/j.jaad.2016.05.046
12. Simpson EL, Paller AS, Boguniewicz M, et al. Crisaborole ointment improves quality of life of patients with mild to moderate atopic dermatitis and their families. Dermatol Ther (Heidelb). 2018;8(4):605–619. doi:10.1007/s13555-018-0263-0
13. Israel Central Bureau of Statistics. Characterization and Classification of Geographic Units by the Socio-Economic Level of the Population 2008. Publication No. 1530. Jerusalem, Israel: Israel Central Bureau of Statistics; 2013.
14. Chung J, Simpson EL. The socioeconomics of atopic dermatitis. Ann Allergy Asthma Immunol. 2019;122(4):360–366. doi:10.1016/j.anai.2018.12.017
15. Drucker AM, Eyerich K, de Bruin-Weller MS, et al. Use of systemic corticosteroids for atopic dermatitis: International Eczema Council consensus statement. Br J Dermatol. 2018;178(3):768–775. doi:10.1111/bjd.15928
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
