Back to Journals » Journal of Inflammation Research » Volume 16
Characteristics and Incidence of Colon Complication in Necrotizing pancreatitis: A Propensity Score-Matched Study
Authors Lu J, Zheng Z, Ding Y, Qu Y, Mei W, Fang Z, Qu C, Feng Y, Guo Y , Gao C, Cao F, Li F
Received 19 September 2022
Accepted for publication 24 December 2022
Published 11 January 2023 Volume 2023:16 Pages 127—144
DOI https://doi.org/10.2147/JIR.S388305
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Monika Sharma
Jiongdi Lu,1,2,* Zhi Zheng,3,* Yixuan Ding,1,2 Yuanxu Qu,1,2 Wentong Mei,1,2 Zhen Fang,1,2 Chang Qu,1,2,* Yulu Feng,4 Yulin Guo,1,2 Chongchong Gao,1,2 Feng Cao,1,2 Fei Li1,2
1Clinical Center of Acute Pancreatitis, Capital Medical University, Beijing, People’s Republic of China; 2Department of General Surgery, Xuanwu Hospital, Capital Medical University, Beijing, People’s Republic of China; 3Department of General Surgery, Beijing Friendship Hospital, Capital Medical University, Beijing, People’s Republic of China; 4Chui Yang Liu Hospital Affiliated Tsinghua University, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Fei Li, Clinical Center of Acute Pancreatitis, Department of General Surgery, Department of Surgery, Xuanwu Hospital of Capital Medical University, No. 45, Changchun Street, Xicheng District, Beijing, 100053, People’s Republic of China, Tel +86-10-83198731, Fax +86-10-83198868, Email [email protected] Feng Cao, Clinical Center of Acute Pancreatitis, Department of General Surgery, Xuanwu Hospital of Capital Medical University, No. 45, Changchun Street, Xicheng District, Beijing, 100053, People’s Republic of China, Email [email protected]
Objective: To clarify the incidence of colonic complications in patients with NP and their impact on prognosis.
Methods: The clinical data of NP patients admitted to the Department of General Surgery of Xuanwu Hospital, Capital Medical University from January 2014 to December 2020 were retrospectively analyzed. Patients were grouped according to the presence or absence of colonic complications, and the clinical prognosis of the two groups was analyzed after matching using a 1:1 propensity score, The primary study endpoint was patient mortality during hospitalization. Data are reported as median (range) or percentage of patients (%).
Results: A total of 306 patients with NP were included in this study, and the incidence of colonic complications was 12.4%, including 15 cases of colonic obstruction, 17 cases of colonic fistula, and 9 cases of colonic hemorrhage. Before matching, patients in the colonic group had severe admissions and poor clinical outcomes (P< 0.05). After matching, the baseline data and clinical characteristics at admission were comparable between the two groups of patients. In terms of clinical outcomes, although the mortality was similar in the two groups (P> 0.05), but patients in the colonic group were more likely to have multiorgan failure, length of nutrition support, number of minimally invasive interventions, number of extra-pancreatic infections, length of ICU stay and total length of stay were significantly higher than those of patients in the group without colonic complications (P< 0.05). During long-term follow-up, patients in the colonic group were more likely to develop recurrent pancreatitis.
Conclusion: About 12.4% of NP patients developed colonic complications, and after PSM it was found that colonic complications only led to a longer hospital stay and an increased number of clinical interventions in NP patients and did not increase the mortality.
Keywords: necrotizing pancreatitis, colon involvement, propensity score match
Introduction
Acute Pancreatitis (AP) is a common digestive system disease, and its incidence is increasing year by year, 20% AP patients will develop pancreatic parenchymal and/or peripancreatic necrosis and progress to necrotizing pancreatitis (NP).1,2 With the expansion of pancreatic necrosis and the development of infectious pancreatic necrosis in NP patients, the colon and colonic mesentery may be affected by several pathways: 1) the invasive compressive effect of pancreatic necrotic tissue; 2) the inflammatory response of the pancreas affecting the colonic blood supply, and 3) direct injury due to the possible removal of pancreatic necrotic tissue.3–5 The incidence of colonic complications in AP patients varies between studies, but the presence of colonic complications will lead to a poorer prognosis.6,7
In recent years, with the accumulation of the number of NP patients in our center, we found that most of the patients diagnosed with colonic complications were complicated with serious complications (such as persistent organ failure, infected pancreatic necrosis, etc.), which are the risk factors affecting the prognosis of patients. Therefore, we retrospectively analyzed the clinical data of previous NP patients to clarify the incidence of colonic complications in NP patients and their impact on prognosis.
Methods
Study Design
In this study, clinical data of patients with AP admitted to the general surgery department of Xuanwu Hospital of Capital Medical University between January 1, 2014, and December 31, 2020, were retrospectively analyzed. This study was reviewed and approved by the Ethical Review Committee of Xuanwu Hospital of the Capital Medical University (No.2020158). This study was designed in accordance with the principles of the Declaration of Helsinki (as revised in 2013). All patient data were anonymously analyzed using an electronic data acquisition system without informed consent. A detailed flowchart of this study is shown in Figure 1.
 |
Figure 1 Flow chart of patient enrollment and follow-up. Abbreviations: AP, acute pancreatitis; NP, necrotizing pancreatitis; CT, computed tomography; MRI, magnetic resonance image. |
Inclusion and Discharge Criteria
Patients with pancreatic and/or peripancreatic necrosis confirmed by imaging examination (enhanced computerized tomography [CT] / magnetic resonance imaging [MRI], etc.) were included in the study.
The exclusion criteria: 1) Mild acute pancreatitis (MAP); 2) NP patients need emergency surgery; 3) Acute exacerbation of chronic pancreatitis or recurrent AP (RAP); 4) Patients with an incomplete case or follow-up data.
Indication of Colon Complication
Confirmation of colonic complications: 1) Colonic fistula: (1) intraoperative exploration reveals a collection of fecal contents; (2) enhanced CT reveals the presence of a sinus tract between the pancreas and the colon; (3) fecal drainage fluid or contents flowing from the drainage tube. (2) Colon obstruction: the patient showed obvious symptoms of intestinal obstruction (abdominal pain, bloating, vomiting, cessation of defecation, etc.), and the site of obstruction was located in the colon on CT. (3) Colon bleeding: (1) bleeding in the drainage tube; (2) bleeding in the colon vessels confirmed by digital subtraction angiography (DSA) or contrast CT.
Observation Outcome
The primary outcome in this study was in-hospital mortality. Other outcomes of this study were persistent organ failure (POF) or new-onset organ failure (NOF), number of patients with confirmed infected pancreatic necrosis (IPN) and extra-pancreatic infection (EPI), type and duration of nutritional support, postoperative complications, length of intensive care unit (ICU) stay and total length of hospital stay. The relevant observables in this study are defined in Table 1.
 |
Table 1 Definitions of the Observation Indicators |
Patient Management
According to the current international guidelines,1,2,8 after admission, patients received routine administration of trypsin inhibitors, fluid resuscitation, analgesia, nutritional support, and other treatments, antibiotics only be used in patients with suspected or confirmed infection. Regular laboratory investigations (routine blood tests, blood biochemistry, inflammatory indicators, etc.) and imaging investigations (abdominal ultrasound or CT) were performed to monitor the patient’s disease development. When the patient’s condition improves, continue the current treatment. If the patient’s condition deteriorates, the multidisciplinary (MDT) team (including pancreatic surgeons, anesthesiologists, intensivists, and imaging physicians) will take targeted treatment measures and reassess the patient’s condition.1) For patients suspected or confirmed NOF, organ support therapy (continuous pumping of vasoactive drugs, mechanical ventilation therapy [MVT], continuous renal replacement therapy [CRRT]) was given. 2) For patients with suspected or confirmed infection symptoms, third- and fourth-generation cephalosporins or carbapenem antibiotics were empirically administered, and the antibiotics were adjusted according to the results of drug sensitivity tests.13
The minimally invasive intervention indications for NP patients were as follows: 1) After conservative treatment, the patient’s condition did not improve (such as NOF, increased temperature and inflammatory factor levels, etc.); 2) Confirmed IPN; 3) Patient presents with gastrointestinal or biliary tract obstruction due to compression of pancreatic necrotic tissue, and the specific surgical methods have been discussed in our previous studies.14–16
Intervention strategies for colonic complications: 1) For patients with confirmed colonic fistula, if the patient’s symptoms do not improve after conservative treatment (eg anti-infection, parenteral nutritional support and keeping the drainage tube open, etc.), perform a Phase I terminal ileostomy, clear drainage and close the fistula in Phase II; 2) For patients with confirmed colonic obstruction, place a small intestine decompression tube and if the decompression effect is good, conservative treatment can be continued; if the condition continues to deteriorate, a stage I terminal ileostomy and stage II colon-colon lateral anastomosis will be performed; 3) For patients with confirmed colonic bleeding, the preferred treatment is embolization and hemostatic treatment while clarifying the patient’s bleeding site under DSA.17 Representative images are shown in Figure 2.
Follow-Up
Clinicians follow up with discharged patients through clinical visits, e-mail or telephone visit to assess readmission, mortality, and long-term complications (eg, endocrine pancreatic insufficiency, exocrine pancreatic insufficiency, incisional hernia, pancreatic cyst and chronic pancreatitis, etc.), the follow-up period was 6 months. Moreover, clinicians can use the SF-36, EQ-5D, and Izbicki pain scales to assess patients’ quality of life. The last follow-up date in this study was June 30, 2022.
Statistical Analysis
In this study, we used Excel 2018 (Microsoft, Redmond, CA, USA) to record the patients’ clinical data, SPSS 23.0 (IBM Corp., Armonk, NY, USA) and GraphPad Prism 8.0 (GraphPad Software, La Jolla, CA, United States) for statistical analysis.
Distribution characteristics of the overall population were expressed as categorical variables (percentages). For comparison between groups, normal distribution data were represented as mean ± standard deviation (mean ± SD) and t test was performed., skewed distribution data were represented as median (range) and Mann–Whitney U-test was performed, quantitative data were represented as percentage and subjected to chi-square test. To balance differences between groups and reduce confounding effects, patient baseline data were included in a logistic regression model for 1:1 propensity score matching (PSM) with a caliper value of 0.02. Survival analysis was performed using the Kaplan-Meier method. P value <0.05 were considered significant.
Results
Incidence and Treatment of Colonic Complications
A total of 306 patients diagnosed with necrotizing pancreatitis were included in this study, the incidence of colonic complications in NP patients was 12.4% (n=38), including 17 cases of colonic fistula, 15 cases of colonic obstruction, and 9 cases of colonic bleeding, (2 patients with colonic fistula and colonic bleeding, and 1 patient with colonic obstruction and colonic bleeding.) Figure 3 describes the sites of colonic complications, time to diagnosis, and interventions. The common sites of colonic fistula and colonic obstruction were colonic splenic flexure, transverse colon (Figure 3A), and middle colonic artery was the common arterial sources of colonic bleeding (Figure 3B). Figure 3C shows the time to diagnosis of colonic complications in NP patients, including 62 (33–106) days for colonic fistula, 67 (14–270) days for colonic obstruction, 40 (11–110) days for colonic bleeding, and 62 (11–270) for colonic complication. 52.9% (n=9) of patients with colonic fistula required surgical intervention with an intervention time of 76 (49–226) minutes. 66.7% (n=10) of patients with colonic obstruction required surgical intervention with an intervention time of 117.5 (64–217) minutes, and 88.9% (n=8) of patients with colonic bleeding Patients required interventional embolization intervention with an intervention time of 109.5 (35–193) minutes (Figure 3D and E).
Clinical Characteristics of NP Patients
A total of 306 patients diagnosed with necrotizing pancreatitis were included in this study, with a mean age of 49.46 ± 15.38 years, 205 males and 101 females, There were 155 cases of biliary pancreatitis, 98 cases of hyperlipidemic pancreatitis, and 53 cases of the pancreatitis of other etiologies (25 cases of the pancreatitis of unknown etiology, 14 cases of post-ERCP pancreatitis, 13 cases of alcoholic pancreatitis, and 1 case of traumatic pancreatitis).
In terms of baseline data and clinical characteristics at admission, there were no differences between the two groups in terms of gender, age, BMI, and etiology. However, patients in the colon group had more comorbidities and increased ASA score (P<0.05). On admission, compared with patients in the non-colonic group, patients with colonic complications had more extensive pancreatic necrosis (pancreatic necrosis ≥50%, CTSI score ≥ 8, P<0.05), more obvious symptoms of infection (temperature ≥ 38°C on admission, procalcitonin > 0.5ng/mL, etc. P<0.05), and worse nutritional status (hemoglobin level <90 g/L and albumin level <30 g/L, P<0.05). (Table 2). In terms of clinical outcomes, patients in the colon complication group needed long-term nutrition support (P<0.05), more likely to have serious complications (such as IPN, EPI, and POF, P<0.05), increased number of patients requiring minimally invasive intervention and the number of interventions, results in poor prognosis of patients (the incidence of postoperative complications, Length of stay in ICU, total length of stay, and mortality, P<0.05) (Table 3).
 |
Table 2 Characteristics of the Necrotizing Pancreatitis Patients |
 |
Table 3 Comparison of Clinical Outcomes Between Two Groups Before PSM |
Propensity Score Matching Analysis
After PSM, the baseline data and clinical characteristics at admission were similar in both groups (Table 4). In terms of clinical outcomes, the number of patients in both groups with confirmed IPN, requiring combined nutritional support, requiring minimally invasive intervention and mortality were similar (P>0.05), but the number of patients in the colonic group with MOF, duration of enteral nutrition support, length of parenteral nutrition support, number of minimally invasive interventions, number of confirmed EPI, length of ICU stay and total length of stay were significantly higher than those in the non-colonic group (P<0.05) (Table 5).
 |
Table 4 Baseline Data of the Two Groups After PSM |
 |
Table 5 Comparison of Clinical Outcomes Between Two Groups After PSM |
Follow-Up
During the follow-up period, before PSM, a total of 256 patients, 42 patients lost to follow-up, 9 patients died, and 205 patients survived (Figure 4A). After matching, with 52 patients, 3 patients died, 6 patients were lost to follow-up, and 43 patients survived (Figure 4B). The overall survival rates [22 (88.0%) and 21 (77.8%), P>0.05] and follow-up times [(42.16 ± 25.89) days vs (38.33 ± 20.24) days, P>0.05] were not statistically different between the two groups (Figure 4C).
In the colonic group, although patients were more likely to develop recurrent pancreatitis (P<0.05), there were no statistical differences between the two groups in terms of other long-term complications (P>0.05) (Table 6).
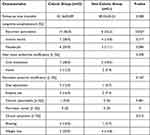 |
Table 6 The Long-Term Complication Between the Two Groups During the Follow-Up Period |
There was no statistical difference in the final scores of the SF-36 health questionnaire, EQ-5D questionnaire, and Lzbicki pain score questionnaire between the two groups (P>0.05) (Table 7).
 |
Table 7 Quality of Life Rating Scale During the Follow-Up Period of Surviving Patients |
Discussion
In this study, we found that after PSM the presence of colonic complications only led to a longer number of minimally invasive interventions, days of nutritional support, and length of hospital stay in NP patients, and did not lead to increased mortality.
The incidence of colonic complications among NP patients was 12.4%, similar to the results of Hu, Lin, and Thomas et al (15.12%, 19%, and 11%),3,18,19 but higher than the incidence reported by Minnen, Jiang, and Kochhar et al (7.27%, 7.76%, and 4.15%),20–22 considered to be related to the type of patients included between studies (eg, AP, NP, SAP, etc.). Regarding the time to diagnosis of colonic complications, the time to diagnosis of colonic complications in the study of Heeter et al was 89 (13–394) days,23 Thomas et al noted that early in the course of NP patients, colonic ischemia [29 (0–200)] days, colonic perforation [47.5 (2–135)] days and fulminant C. difficile colitis [19 (1–63)] days, while colonic fistulas [144.5 (18–466)] and inflammatory colonic strictures (obstruction) [87 (7–289)] days were mostly seen later in the course of the disease.3 In contrast, the time to diagnosis of colonic complications in this study was 62 (11–270) days, which occurred mostly in the late course of NP patients, the difference in the time to diagnosis of colonic complications may be related to the severity of the patient’s disease and the clinician’s diagnosis and treatment.
In our center, we found that the most common sites of colonic complications in patients with NP were the colonic splenic flexure and the transverse colon, respectively, which were considered to be related to the fact that the area of pancreatic necrosis often extends to the tail of the pancreatic body and the lack of blood supply to the colonic splenic flexure in patients with NP.24–26 The causes of different colonic complications may be as follows: 1) direct erosion of colonic trophoblastic vessels by pancreatic fluid-rich necrotic tissue, causing erosion and destruction of colonic arterial blood vessel walls, leading to pseudoaneurysm formation and colonic bleeding;17 2) spread of peripancreatic necrotic tissue to the colon and colonic mesentery causing colonic adhesions, or compression by inflammatory masses of the pancreas or colonic fibrosis leading to narrowing of the intestinal lumen, and fixed position of the colonic splenic flexure, poor mobility, prone to colonic obstruction;3,4 3) direct erosion of the colonic intestinal wall by pancreatic digestive enzymes, inflammatory factors in the area of pancreatic necrosis stimulate vasospasm and reduce capillary perfusion, leading to thrombosis causing intestinal necrosis and colonic fistula;18 4) direct injury from surgical operations or compression by drainage tubes during the removal of necrotic tissue, causing tortuous edematous colonic vascular hemorrhage or intestinal fistula formation.21,27 In this study, we found that although colonic complications in NP patients are insidious, most of them are often accompanied by the worsening of patients’ clinical symptoms (eg, sepsis, hemorrhagic shock, blood in stool, etc.). Therefore, clinicians should pay high attention to NP patients with sudden exacerbations.
At admission, the degree of pancreatic necrosis and the level of inflammatory factors were significantly higher in patients in the colonic group than in those in the non-colonic group, and as the extent of pancreatic necrosis expanded and the degree of necrosis increased in patients, inflammatory factors entered the blood and caused severe systemic inflammatory response syndrome (SIRS) and decreased immune function, making it more likely to develop IPN and POF,28 leading to an increased incidence of colonic complications and mortality in patients.3,18 The impact of colonic complications on the digestive function of NP patients requires therapeutic measures such as suppression of pancreatic fluid secretion, nutritional support, minimally invasive interventions, and the prolongation of the patient’s hospital stay. In addition, the number of patients in the colonic group who develop extra-pancreatic infections and MOF remains higher than those in the non-colonic group, and severe systemic or local inflammatory reactions and hemodynamic disturbances due to organ failure disrupt the colonic blood supply, leading to the development of colonic complications, which in turn affect the prognosis of patients.21
Previous studies have suggested that colography facilitates the early detection of asymptomatic fistula patients. For patients with obvious colon fistula, approximately 47% of patients recover after treatment with percutaneous catheter drainage (PCD) and continuous negative pressure irrigation (CNPI), avoiding further surgical treatment.19
For clinicians, surgical interventions are still the preferred method for treating colonic complications, and different interventions can be used to remove pancreatic necrotic tissue by multiple and timely drainages depending on whether the patient is wrapped in necrotic tissue, which helps to reduce the inflammatory response and injury around the colon and reduce or avoid the occurrence of medically induced intestinal injury.23,29,30
After long-term follow-up, although the quality of life scores of the two groups were similar, the incidence of RAP in the colonic group was much higher than that in the non-colonic group and Petrov et al study (56% vs 22.2% vs 21.0%).31 Due to the wide range of pancreatic necrosis, multiple interventions were needed to control infection in the colonic group, moreover, there are a large number of co-morbidities in the colonic group, which may induce the deterioration of self-co-morbidities under the inflammatory stimulation of residual necrotic tissue, and eventually lead to the the emergence of RAP.32 The similar incidence of other long-term complications between the two groups may be related to the small number of patients in the colon group, which needs to be verified by further large-sample studies in the future.
The main limitations of our study are as follows:1) Our center is a large acute pancreatitis treatment center, and most of the patients have a history of outpatient treatment and are in serious condition, which potentially increases the incidence of colonic complications; 2) This is a retrospective study, and some of the patients are outpatient referrals, and the clinical indicators included are influenced by the level of detail of clinical information at the time of patient referral, which may have some statistical bias; 3) The number of patients in both groups after PSM is small (n=38), and there may be some selection bias.
Conclusion
In this study, the incidence of colonic complications in NP patients was 12.4%. After PSM, colonic complications only led to a longer hospital stay and an increased number of clinical interventions and did not increase the mortality. During long-term follow-up, patients in the colonic group were more likely to have RAP.
Abbreviations
AP, Acute pancreatitis; NP, Necrotizing pancreatitis; CT, Computed tomography; MRI, Magnetic Resonance Image; MAP, Mild acute pancreatitis; RAP, Recurrent Acute pancreatitis; CP, Chronic pancreatitis; DSA, Digital subtraction angiography; POF, Persistent organ failure; NOF, New-onset organ failure; IPN, Infected pancreatic necrosis; EPI, Extra-pancreatic infection; ICU, Intensive care unit; PEI, Pancreatic exocrine dysfunction; MDT, Multidisciplinary team; MVT, Mechanical ventilation therapy; CRRT, Continuous renal replacement therapy; PSM, Propensity score matching; BMI, Body mass index; ERCP, Endoscopic retrograde cholangiography; CTSI, Computed tomography severity index; PCT, Procalcitonin; MOF, Multiple organ failure; SIRS, Systemic inflammatory response syndrome; EN, Enteral nutrition; PN, Parenteral nutrition.
Ethics Approval and Consent to Participate
The clinical data of patients in this study were collected from the database of Xuanwu Hospital, Capital Medical University, and have been reviewed and approved by the Review Committee of Xuanwu Hospital, Capital Medical University (No. 2020-158). Because this was a retrospective study that only analyzed existing clinical and follow-up data, the need to obtain informed patient consent was waived.
Acknowledgments
We would like to thank Professor Chun-jing Bian and Professor Ang Li for their guidance in this manuscript.
Funding
The research was supported by: 1. Beijing Municipal Science & Technology Commission (grant number: Z171100001017077); 2. Beijing Municipal Science and Technology Commission Clinical Diagnosis and Treatment Technology Research and Demonstration Application Project (grant number: Z191100006619038); 3. Capital Medical Development and Research Special Project (grant number: 2020-1-2012); 4. Construction Project of Clinical Advanced subjects of Capital Medical University (grant number: 1192070312); 5. Capital Medical Development and Research Special Project (grant number: Z201100005520090); 6. Beijing Medical Authority Cultivation Program (grant number: PX2022035).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Trikudanathan G, Wolbrink DRJ, van Santvoort HC, Mallery S, Freeman M, Besselink MG. Current concepts in severe acute and necrotizing pancreatitis: an evidence-based approach. Gastroenterology. 2019;156(7):1994–2007.e3. doi:10.1053/j.gastro.2019.01.269
2. Mederos MA, Reber HA, Girgis MD. Acute pancreatitis: a review. JAMA. 2021;325(4):382–390. doi:10.1001/jama.2020.20317
3. Maatman TK, Nicolas ME, Roch AM, et al. Colon involvement in necrotizing pancreatitis: incidence, risk factors, and outcomes. Ann Surg. 2022;275(3):568–575. doi:10.1097/SLA.0000000000004149
4. Aldridge MC, Francis ND, Glazer G, Dudley HA. Colonic complications of severe acute pancreatitis. Br J Surg. 1989;76(4):362–367. doi:10.1002/bjs.1800760416
5. Mann NS. Colonic involvement in pancreatitis. Am J Gastroenterol. 1980;73(4):357–362.
6. Mohamed SR, Siriwardena AK. Understanding the colonic complications of pancreatitis. Pancreatology. 2008;8(2):153–158. doi:10.1159/000123607
7. Aldridge MC, Francis ND, Glazer G, Dudley HA. Colonic complications of severe acute pancreatitis. Br J Surg. 1989;76(4):362–367.
8. Banks PA, Bollen TL, Dervenis C, et al.; Acute Pancreatitis Classification Working Group. Classification of acute pancreatitis--2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62(1):102–111. doi:10.1136/gutjnl-2012-302779.
9. Balthazar EJ, Ranson JH, Naidich DP, Megibow AJ, Caccavale R, Cooper MM. Acute pancreatitis: prognostic value of CT. Radiology. 1985;156(3):767–772. doi:10.1148/radiology.156.3.4023241
10. Pando E, Alberti P, Hidalgo J, et al. The role of extra-pancreatic infections in the prediction of severity and local complications in acute pancreatitis. Pancreatology. 2018;18(5):486–493. doi:10.1016/j.pan.2018.05.481
11. Brown LA, Hore TA, Phillips AR, Windsor JA, Petrov MS. A systematic review of the extra-pancreatic infectious complications in acute pancreatitis. Pancreatology. 2014;14(6):436–443. doi:10.1016/j.pan.2014.09.010
12. Beyer G, Habtezion A, Werner J, Lerch MM, Mayerle J. Chronic pancreatitis. Lancet. 2020;396(10249):499–512. doi:10.1016/S0140-6736(20)31318-0
13. Lu JD, Cao F, Ding YX, Wu YD, Guo YL, Li F. Timing, distribution, and microbiology of infectious complications after necrotizing pancreatitis. World J Gastroenterol. 2019;25(34):5162–5173. doi:10.3748/wjg.v25.i34.5162
14. Li A, Cao F, Li J, et al. Step-up mini-invasive surgery for infected pancreatic necrosis: results from prospective cohort study. Pancreatology. 2016;16(4):508–514. doi:10.1016/j.pan.2016.03.014
15. Cao F, Li A, Wang X, Gao C, Li J, Li F. Laparoscopic transgastric necrosectomy in treatment of walled-off pancreatic necrosis with sinistral portal hypertension. BMC Surg. 2021;21(1):362. doi:10.1186/s12893-021-01361-6
16. Cao F, Duan N, Gao C, Li A, Li F. One-step verse step-up laparoscopic-assisted necrosectomy for infected pancreatic necrosis. Dig Surg. 2020;37(3):211–219. doi:10.1159/000501076
17. Zhang C, Li A, Luo T, et al. Strategy and management of severe hemorrhage complicating pancreatitis and post-pancreatectomy. Diagn Interv Radiol. 2019;25(1):81–89. doi:10.5152/dir.2018.18283
18. Hua Z, Su Y, Huang X, et al. Analysis of risk factors related to gastrointestinal fistula in patients with severe acute pancreatitis: a retrospective study of 344 cases in a single Chinese center. BMC Gastroenterol. 2017;17(1):29. doi:10.1186/s12876-017-0587-8
19. Gao L, Zhang JZ, Gao K, et al. Management of colonic fistulas in patients with infected pancreatic necrosis being treated with a step-up approach. HPB (Oxford). 2020;22(12):1738–1744. doi:10.1016/j.hpb.2020.03.021
20. Van Minnen LP, Besselink MG, Bosscha K, Van Leeuwen MS, Schipper ME, Gooszen HG. Colonic involvement in acute pancreatitis. A retrospective study of 16 patients. Dig Surg. 2004;21(1):33–38. doi:10.1159/000075824
21. Jiang W, Tong Z, Yang D, et al. Gastrointestinal Fistulas in Acute Pancreatitis With Infected Pancreatic or Peripancreatic Necrosis: a 4-Year Single-Center Experience. Medicine. 2016;95(14):e3318. doi:10.1097/MD.0000000000003318
22. Kochhar R, Jain K, Gupta V, et al. Fistulization in the GI tract in acute pancreatitis. Gastrointest Endosc. 2012;75(2):436–440. doi:10.1016/j.gie.2011.09.032
23. Heeter ZR, Hauptmann E, Crane R, et al. Pancreaticocolonic fistulas secondary to severe acute pancreatitis treated by percutaneous drainage: successful nonsurgical outcomes in a single-center case series. J Vasc Interv Radiol. 2013;24(1):122–129. doi:10.1016/j.jvir.2012.09.020
24. Adams DB, Davis BR, Anderson MC. Colonic complications of pancreatitis. Am Surg. 1994;60(1):44–49.
25. Russell JC, Welch JP, Clark DG. Colonic complications of acute pancreatitis and pancreatic abscess. Am J Surg. 1983;146(5):558–564. doi:10.1016/0002-9610(83)90288-X
26. Gumaste VV, Gupta R, Wasserman D, Dave PB, Vieux U. Colonic involvement in acute pancreatitis. Am J Gastroenterol. 1995;90(4):640–641.
27. Flati G, Andrén-Sandberg A, La Pinta M, Porowska B, Carboni M. Potentially fatal bleeding in acute pancreatitis: pathophysiology, prevention, and treatment. Pancreas. 2003;26(1):8–14. doi:10.1097/00006676-200301000-00002
28. Tan C, Yang L, Shi F, et al. Early systemic inflammatory response syndrome duration predicts infected pancreatic necrosis. J Gastrointest Surg. 2020;24(3):590–597. doi:10.1007/s11605-019-04149-5
29. Jagielski M, Smoczyński M, Adrych K. Endoscopic treatment of walled-off pancreatic necrosis complicated with pancreaticocolonic fistula. Surg Endosc. 2018;32(3):1572–1580. doi:10.1007/s00464-018-6032-4
30. Mohamed SR, Siriwardena AK. Understanding the colonic complications of pancreatitis. Pancreatology. 2008;8(2):153–158.
31. Petrov Maxim S, Dhiraj Y. Global epidemiology and holistic prevention of pancreatitis. Nat Rev Gastroenterol Hepatol. 2019;16:175–184. doi:10.1038/s41575-018-0087-5
32. Murata A, Ohtani M, Muramatsu K, et al. Influence of comorbidity on outcomes of older patients with acute pancreatitis based on a national administrative database. Hepatobiliary Pancreat Dis Int. 2015;14(4):422–428. doi:10.1016/S1499-3872(15)60398-8
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



