Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Changes in Inflammatory Biomarkers in Patients with Schizophrenia: A 3-Year Retrospective Study
Authors Zhu X, Li R, Zhu Y, Zhou J, Huang J, Zhou Y, Tong J, Zhang P, Luo X , Chen S, Li Y , Tian B, Tan SP, Wang Z, Han X, Tian L, Li CSR, Tan YL
Received 15 March 2023
Accepted for publication 19 June 2023
Published 12 July 2023 Volume 2023:19 Pages 1597—1604
DOI https://doi.org/10.2147/NDT.S411028
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Yuping Ning
Xiaoyu Zhu,1 Ran Li,1 Yu Zhu,1 Jia Zhou,1 Junchao Huang,1 Yanfang Zhou,1 Jinghui Tong,1 Ping Zhang,1 Xingguang Luo,2 Song Chen,1 Yanli Li,1 Baopeng Tian,1 Shu-Ping Tan,1 Zhiren Wang,1 Xiaole Han,1 Li Tian,3 Chiang-Shan R Li,2 Yun-Long Tan1
1Psychosomatic Department, Beijing HuiLongGuan Hospital, Beijing, People’s Republic of China; 2Department of Psychiatry, Yale University School of Medicine, New Haven, CT, USA; 3Institute of Biomedicine and Translational Medicine, Department of Physiology, Faculty of Medicine, University of Tartu, Tartu, Estonia
Correspondence: Yun-Long Tan, Psychosomatic Department, Beijing HuiLongGuan Hospital, Beijing, People’s Republic of China, Tel +86-10-83024319, Fax +86-10-62710156, Email [email protected]
Objective: Accumulating evidence suggested that immune system activation might be involved in the pathophysiology of schizophrenia. The neutrophil/lymphocyte ratio (NLR), monocyte/lymphocyte ratio (MLR), platelet/lymphocyte ratio (PLR) and systemic immune-inflammation index (SII) can measure inflammation. This study aimed to investigate the inflammatory state in patients with schizophrenia by using these indicators.
Methods: In this study, the complete blood count data for 187 continuing hospitalized patients with schizophrenia and 187 age- and sex-matched healthy participants was collected annually from 2017 to 2019. Platelet (PLT), lymphocyte (LYM), monocyte (MON) and neutrophil (NEU) counts were aggregated and NLR, MLR, PLR, and SII were calculated. Using a generalized linear mixed model, we assessed the impact of age, sex, diagnosis, and sampling year on the above indicators and evaluated the interaction between the factors.
Results: According to the estimation results of the generalized linear mixed model, the NLR increased by 0.319 (p = 0.004), the MLR increased by 0.037 (p < 0.001), and the SII increased by 57.858 (p = 0.018) in patients with schizophrenia. Data after two years of continuous antipsychotic treatment showed that the NLR and MLR were higher in patients with schizophrenia than those in healthy controls, while the PLT and LYM counts were decreased in patients with schizophrenia. The schizophrenia diagnosis was correlated to the MON and LYM count, NLR, MLR, and SII (p < 0.05).
Conclusion: The differences in these markers were stable and cannot be eliminated by a full course of treatment. This study provides impetus for the inflammatory hypothesis of schizophrenia.
Keywords: schizophrenia, systemic immune-inflammation index, neutrophil/lymphocyte ratio, monocyte/lymphocyte ratio, platelet/lymphocyte ratio
Introduction
Existing evidence suggests a potential association between schizophrenia, inflammatory responses, and neuro-immunity related genetic factors.1,2 It is theorized that exposure to high levels of interleukin-8 (IL-8) during fetal development may influence brain structure, contributing to the onset of schizophrenia.3–5 Pregnant women’s immune responses can amplify fetal inflammatory factors, thereby elevating the risk of schizophrenia in their offspring.6 Additionally, childhood viral infections or those occurring prior to disorder onset could exacerbate the risk of various mental disorders, including schizophrenia.7–9 A correlation between diverse bacterial and viral infections and the incidence of mental illnesses has been affirmed by numerous studies.8–13 Food antigens or mast cells associated with allergic reactions may trigger symptoms of mental disorders,14–16 and autoimmune diseases have been identified as having a linkage with schizophrenia.17 An elevated level of various autoimmune antibodies has been observed in patients diagnosed with schizophrenia.18
Elevated concentrations of several inflammatory factors have been found in individuals with schizophrenia, pointing towards a potential correlation with immune responses.19,20 Abnormal levels of inflammatory markers have been observed in patients suffering from schizophrenia and bipolar disorder, indicating a substantial link between mental illnesses and inflammatory responses.21,22 Patients with schizophrenia have exhibited abnormal c-reactive protein levels, reduced lymphocyte (LYM) counts, and increased levels of interleukin-1 (IL-1), interleukin-6 (IL-6), interleukin-23 (IL-23), T helper 17 (Th17), tumor necrosis factor-α (TNF-α), neutrophils (NEU), neutrophil/lymphocyte ratios (NLR), and monocyte / lymphocyte ratios (MLR).23,24
Despite the findings from studies indicating the activation of the immune inflammatory response (IRS) and compensatory immune regulatory system (CIRS) in patients with schizophrenia,25 the exact mechanisms remain elusive. One proposition is that chronic mild neuro-inflammation may have a more substantial contribution to mental illness development.26 Chronic inflammation could disrupt neurotransmitter secretion balance, activate adrenergic α1 receptors, and lead to uneven contractions in the vascular wall of the central nervous system. Such occurrences could alter brain blood flow distribution, impair normal brain development and functioning, and subsequently induce mental illness.26 Additionally, immune activation may result in endocannabinoid system abnormalities, giving rise to psychiatric disorders.27 It has been suggested that bacterial translocation, particularly by gram-negative bacteria, could trigger immune activation, leading to alterations in the IL-6/IL-23/Th17 axis and resulting in cognitive deficits and schizophrenia.25,28,29
Due to the robust association between immunity and schizophrenia, numerous inflammatory markers have been utilized in schizophrenia research. Markers, such as NLR, MLR, and platelet/lymphocyte ratio (PLR), are gaining prominence due to their relative ease of collection and confirmed associations with various mental illnesses.13,18,24,30–37 Elevated levels of NLR, MLR, and PLR have been observed in various psychiatric disorders,13,34,36,37 and NLR may serve as a predictor for suicide risk among certain patients with affective disorders.18 Several studies have shown that NLR, PLR, and MLR are significantly higher in patients with schizophrenia.35,38 Furthermore, an investigation analyzing blood data at different schizophrenia stages revealed that NLR, PLR, and MLR were elevated during the disease onset, and PLR and MLR remained high during remission periods.35
Our prior cross-sectional study involving a Chinese cohort demonstrated significant differences in platelet (PLT) and LYM count, NLR, and MLR between individuals with schizophrenia and healthy participants.24 In the current study, we extended our investigation on this cohort with three consecutive annual checkups, to further explore the stability of these markers.
Moreover, we have incorporated the systemic immune-inflammation index (SII) as one of our observation indicators in this study. SII, an inflammation marker that has recently gained significant attention, is extensively employed in cancer, rheumatism, and immunity research.39–42 Recent studies have begun to explore the connection between SII and the coronavirus disease (COVID-19).43,44 However, the relationship between SII and schizophrenia remains largely uninvestigated. This study aims to address this knowledge gap.
Methods
Participants
Data for patients from Beijing Huilongguan Hospital undergoing complete blood count tests were logged into an electronic database. Our initial study24 drew from this database, comprising 395 patients with schizophrenia, diagnosed according to the Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV, and 395 healthy individuals. These groups were matched based on age and sex, with their complete blood count data subjected to analysis. The present study revisited the same 395 patients and healthy participants in the database, focusing on those with complete blood count records for three consecutive years from 2017 to 2019. To ensure comprehensive medical records, only inpatients were included. Given the hospital’s routine of conducting annual physical examinations every October, patient data collected in October of each year were extracted to mitigate potential influence from seasonal fluctuations. After reviewing medical records to exclude participants with conditions impacting inflammatory markers (infectious diseases, acute and chronic inflammations, allergic diseases, autoimmune diseases, malignant tumors) or those taking medications affecting blood markers (antibiotics, antiviral drugs, antiallergic drugs, immunosuppressants, leukocyte promoters), 260 patients and 234 healthy participants were deemed suitable for inclusion in the study. Participants were matched using a precise 1:1 propensity score based on age and sex. The final data analysis included 187 patients and 187 healthy participants.
As a retrospective study, the Human Research Ethics Committee of Beijing Huilongguan Hospital waived the need for consent. However, all patients retained the right to opt-out of medical research participation, as announced on a hospital bulletin board. Personally identifiable information remained unidentifiable throughout the research investigation. This study complied with the Declaration of Helsinki and received approval from the Human Research Ethics Committee of Beijing Huilongguan Hospital [Protocol No. 2017–49].
Blood Count Analysis and Ratio Calculation
The SYSMEX XN-3000 assembly line (Sysmex Corporation, Japan), along with its supporting reagents and quality control products, was utilized to obtain complete blood counts. The operation strictly adhered to the quality control and testing requirements as outlined in the operation manual.
Complete blood count results spanning January 01, 2017, to December 31, 2019, were collected from the hospital’s electronic laboratory system. The yearly complete blood count test data of the patients were incorporated into the analysis. If multiple data records for the same patient within a single year existed, the first complete blood count test data of that year were utilized. NEU, LYM, PLT, and monocyte (MON) counts were extracted, and the neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), monocyte-to-lymphocyte ratio (MLR), and SII (PLT*NEU/LYM) were calculated, each to three decimal places.
Statistical Analyses
IBM SPSS Statistics for Windows Version 22.0 (IBM Corp., Armonk, NY, USA) facilitated all data analyses. Paired-sample nonparametric tests were employed to ascertain differences between groups. A generalized linear mixed model was used to assess the influence of age, sex, diagnosis, and sampling year, along with the interaction among these factors. A significance level was set at 5% (p < 0.05). All data are expressed as mean ± standard deviation (SD).
Results
Participant Characteristics
The 374 participants had an average age of 47.09 ± 9.22 years in 2019, with 62.6% being male. Demographic information and clinical characteristics of the participants are detailed in Table 1.
 |
Table 1 Participant Demographics and Clinical Characteristics |
Analyses of Inflammatory Indicators Spanning 3 Years
Using a generalized linear mixed model, we examined the impact of age, sex, diagnosis, and sampling time on inflammatory markers. The diagnosis of schizophrenia was found to be associated with the MON and LYM counts, the NLR, MLR, and SII (p < 0.05). A noteworthy trend towards correlation was observed between diagnosis and NEU count (p = 0.051). Additionally, age and sex influenced several of the inflammatory markers (refer to Table 2).
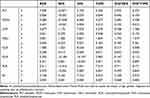 |
Table 2 The Influence of Various Factors on Inflammatory Markers |
Our primary focus was on inflammatory markers, such as MLR, NLR, PLR, and SII. Given that no interaction was found between diagnosis and sex or diagnosis and sampling time for MLR, NLR, PLR, or SII (p > 0.05), these interaction factors were removed. We then applied a generalized linear mixed model to further analyze the impact of each factor on these inflammatory markers.
The diagnosis of schizophrenia was found to correlate with increased NLR, MLR, and SII. A schizophrenia diagnosis increased the NLR by 0.319 (p = 0.004), MLR by 0.037 (p < 0.001), and SII by 57.858 (p = 0.018). Additionally, sex and age exerted a certain influence. The MLR was higher in males (β = 0.033, p = 0.001), while SII (β = −51.882, p = 0.042) and PLR (β = −17.992, p < 0.001) were lower. Moreover, SII showed a decrease with age (β = 2.721, p = 0.043) (see Table 3).
 |
Table 3 The Influence of Various Factors on Inflammatory Markers and Their Coefficients |
Analyses of Inflammatory Indicators in 2019
Considering all patients in this study remained hospitalized from 2017 to 2019, we can surmise that the 2019 patient data likely represent a treated/medicated state. We separately analyzed this data. The PLT and LYM counts were lower in patients with schizophrenia compared to controls (p < 0.05), while no significant difference was observed in MON and NEU counts. The NLR and MLR were higher in patients with schizophrenia compared to controls (p < 0.05), yet no significant difference was observed in PLR and SII between the two groups (refer to Table 4).
 |
Table 4 Comparison of PLT, MON, LYM, NEU, PLR, NLR, MLR, and SII Between Patients with Schizophrenia and Healthy Controls in 2019 |
Discussion
This study reveals a decrease in PLT and LYM counts, along with an increase in the NLR and MLR among patients diagnosed with schizophrenia, reinforcing the conclusions of our previous research.24
A significant correlation was observed between schizophrenia and the NLR, MLR, and SII. Our analysis of data spanning three years indicated that the abnormal inflammatory state observed in patients diagnosed with schizophrenia was not transitory or incidental, but rather persistent and enduring. The constancy of NLR, MLR, and SII changes over time suggests that they could serve as stable markers for the disease. Importantly, these anomalies were directly linked to the disease, with no influence from age and gender interactions.
While we could not gather information on patients’ psychopathology and medications for this study, all participants had been hospitalized from 2017 to 2019. This suggests that they underwent consistent treatment for a minimum of two years, equivalent to a full course of schizophrenia treatment. Data from 2019 revealed that the MLR and NLR in patients with schizophrenia remained significantly higher than those in healthy individuals. This indicates that the abnormal inflammatory state does not diminish even after a full course of treatment. While some researchers argue that antipsychotic medications affect inflammatory indicators, such as c-reactive protein, erythrocyte sedimentation rate, IL-6, IL-1β, and TNF-α,45–47 others contend that specific antipsychotics, such as clozapine, do not significantly impact the ratios of the inflammatory markers we investigated.35
Our findings lend further support to the hypothesis that there is a connection between inflammation and schizophrenia. While we did not observe an increase in NEU counts in patients, as some prior studies have reported, we did note a decrease in LYM counts and elevations in NLR and MLR. This aligns with the results of previous research,23,38 indicating the existence of an inflammatory response in patients with schizophrenia. Although the inflammatory state in schizophrenia patients is clear, the causal link between schizophrenia and inflammation remains speculative, pending further research.
There have been few studies that examine the relationship between sex, age, and the PLR, MLR, NLR, and SII. Two substantial studies among healthy Chinese individuals attempted to explore the effect of age and sex on these inflammatory markers, but yielded inconsistent results.48,49 Our study showed that males have higher MLR, but lower SII and PLR. Estrogen, which exhibits anti-inflammatory properties and may alleviate psychiatric symptoms,50,51 could account for these differences in inflammatory markers. However, body-produced estrogen levels fluctuate, and considering the impact of female menopause adds further complexity. Our findings suggest that age impacts SII, but comprehensive research on age and sex would necessitate a larger sample size. Consequently, our study can only provide reference points for future related research, given our limited number of participants.
This research has several strengths. Our team is the first to use these inflammatory markers to study schizophrenia in a Chinese population, thereby addressing a racial data gap in the field. The application of SII analysis, in particular, is a pioneering approach in the context of schizophrenia research. Additionally, we amassed data from hundreds of individuals over a retrospective three-year period, a scale rarely seen in similar studies. By carefully matching patient and control groups on a one-to-one basis according to age and sex, we minimized confounding factors. Moreover, the use of a generalized linear mixed model made our analysis of influencing factors more comprehensive.
However, this study is not without its limitations. As an observational and retrospective study, we did not carry out medical interventions or establish groups and comparisons based on these interventions, which restricts our ability to make causal inferences. Although we inferred the treatment status of the patients based on data continuity, gathering more precise information on treatment and disease status at the time of sampling would have enhanced our research. We observed that inflammatory markers did not change significantly over the three-year study period, possibly because the time span was too brief. Future studies with a longer tracking period might provide a more rigorous evaluation of these markers.
This study’s focus on the relationship between schizophrenia and several inflammatory factors could also be viewed as a limitation. The etiology of schizophrenia is multifaceted, with links to adipokine dysregulation, metabolic syndrome, and stress, among other factors.52–54 Additionally, adipokine dysregulation, stress, smoking, weight, and lifestyle can affect immune response.55,56 Interactions between these elements complicate the pathogenesis of schizophrenia, yet our study was unable to delve deeper into these aspects. Future research that considers these intricate factors and their interrelationships may enhance our understanding of schizophrenia’s pathogenesis.
Conclusion
Our findings highlight a distinctive inflammatory profile in patients with schizophrenia compared to healthy individuals. The alterations in these inflammatory markers appear stable and remain unaffected by systemic treatments. We propose that this persistent, treatment-resistant inflammatory state provides a critical lens for comprehending the complex nature of schizophrenia. Further exploration in this area may pave the way for new strategies in managing this multifaceted disorder.
Acknowledgments
Support was received from the National Natural Science Foundation of China (82171507) and Beijing Municipal Natural Science Foundation (7212054).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
None to declare.
References
1. Matheson SL, Shepherd AM, Carr VJ. How much do we know about schizophrenia and how well do we know it? Evidence from the Schizophrenia Library. Psychol Med. 2014;44(16):3387–3405. doi:10.1017/S0033291714000166
2. Birnbaum R, Weinberger DR. A genetics perspective on the role of the (Neuro) immune system in schizophrenia. Schizophr Res. 2019;217:105–113. doi:10.1016/j.schres.2019.02.005
3. Brown AS, Begg MD, Gravenstein S, et al. Serologic evidence of prenatal influenza in the etiology of schizophrenia. Arch Gen Psychiatry. 2004;61(8):774–780. doi:10.1001/archpsyc.61.8.774
4. Brown AS. Prenatal infection as a risk factor for schizophrenia. Schizophr Bull. 2006;32(2):200–202. doi:10.1093/schbul/sbj052
5. Ellman LM, Deicken RF, Vinogradov S, et al. Structural brain alterations in schizophrenia following fetal exposure to the inflammatory cytokine interleukin-8. Schizophr Res. 2010;121(1–3):46–54. doi:10.1016/j.schres.2010.05.014
6. Ashdown H, Dumont Y, Ng M, Poole S, Boksa P, Luheshi GN. The role of cytokines in mediating effects of prenatal infection on the fetus: implications for schizophrenia. Mol Psychiatry. 2006;11(1):47–55. doi:10.1038/sj.mp.4001748
7. Gattaz WF, Abrahão AL, Foccacia R. Childhood meningitis, brain maturation and the risk of psychosis. Eur Arch Psychiatry Clin Neurosci. 2004;254(1):23–26. doi:10.1007/s00406-004-0431-3
8. Koponen H, Rantakallio P, Veijola J, Jones P, Jokelainen J, Isohanni M. Childhood central nervous system infections and risk for schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2004;254(1):9–13. doi:10.1007/s00406-004-0485-2
9. Leweke FM, Gerth CW, Koethe D, et al. Antibodies to infectious agents in individuals with recent onset schizophrenia. Eur Arch Psychiatry Clin Neurosci. 2004;254(1):4–8. doi:10.1007/s00406-004-0481-6
10. Severance EG, Gressitt KL, Stallings CR, et al. Candida albicans exposures, sex specificity and cognitive deficits in schizophrenia and bipolar disorder. NPJ Schizophr. 2016;2:16018. doi:10.1038/npjschz.2016.18
11. Kalayci F, Ozdemir A, Saribas S, et al. The relationship of Chlamydophila pneumoniae with schizophrenia: the role of brain-derived neurotrophic factor (BDNF) and neurotrophin-3 (NT-3) in this relationship. Rev Argent Microbiol. 2017;49(1):39–49. doi:10.1016/j.ram.2016.09.009
12. Xiaoyu Z, Xiaole H, Ran L, Baohua Z, Kezhi L. Research progress on C - reactive protein and schizophrenia. Sichuan Mental Health. 2019;032(002):190–192.
13. Zulfic Z, Weickert CS, Weickert TW, Liu D, Myles N, Galletly C. Neutrophil-lymphocyte ratio - a simple, accessible measure of inflammation, morbidity and prognosis in psychiatric disorders. Australas Psychiatry. 2020;2020:1039856220908172.
14. Hájek T, Pasková B, Janovská D, et al. Higher prevalence of antibodies to Borrelia burgdorferi in psychiatric patients than in healthy subjects. Am J Psychiatry. 2002;159(2):297–301. doi:10.1176/appi.ajp.159.2.297
15. Severance EG, Gressitt KL, Alaedini A, et al. IgG dynamics of dietary antigens point to cerebrospinal fluid barrier or flow dysfunction in first-episode schizophrenia. Brain Behav Immun. 2015;44:148–158. doi:10.1016/j.bbi.2014.09.009
16. Georgin-Lavialle S, Gaillard R, Moura D, Hermine O. Mastocytosis in adulthood and neuropsychiatric disorders. Transl Res. 2016;174:77–85.e1. doi:10.1016/j.trsl.2016.03.013
17. Benros ME, Nielsen PR, Nordentoft M, Eaton WW, Dalton SO, Mortensen PB. Autoimmune diseases and severe infections as risk factors for schizophrenia: a 30-year population-based register study. Am J Psychiatry. 2011;168(12):1303–1310. doi:10.1176/appi.ajp.2011.11030516
18. Ivkovi M, Pantovi-Stefanovi M, Dunji-Kosti B, et al. Neutrophil-to-lymphocyte ratio predicting suicide risk in euthymic patients with bipolar disorder: moderatory effect of family history. Compr Psychiatry. 2016;66:87–95. doi:10.1016/j.comppsych.2016.01.005
19. Kelly DL, Li X, Kilday C, et al. Increased circulating regulatory T cells in medicated people with schizophrenia. Psychiatry Res. 2018;269:517–523. doi:10.1016/j.psychres.2018.09.006
20. Delaney S, Fallon B, Alaedini A, et al. Inflammatory biomarkers in psychosis and clinical high risk populations. Schizophr Res. 2019;206:440–443. doi:10.1016/j.schres.2018.10.017
21. Hartwig FP, Borges MC, Horta BL, Bowden J, Davey Smith G. Inflammatory biomarkers and risk of schizophrenia: a 2-sample Mendelian randomization study. JAMA Psychiatry. 2017;74(12):1226–1233. doi:10.1001/jamapsychiatry.2017.3191
22. Tanaka T, Matsuda T, Hayes LN, et al. Infection and inflammation in schizophrenia and bipolar disorder. Neurosci Res. 2017;115:59–63. doi:10.1016/j.neures.2016.11.002
23. Özdin S, Sarisoy G, Böke Ö. A comparison of the neutrophil-lymphocyte, platelet-lymphocyte and monocyte-lymphocyte ratios in schizophrenia and bipolar disorder patients - a retrospective file review. Nord J Psychiatry. 2017;71(7):509–512. doi:10.1080/08039488.2017.1340517
24. Zhu X, Zhou J, Zhu Y, et al. Neutrophil/lymphocyte, platelet/lymphocyte and monocyte/lymphocyte ratios in schizophrenia. Australas Psychiatry. 2021;2021:10398562211022753.
25. Maes M, Plaimas K, Suratanee A, Noto C, Kanchanatawan B. First episode psychosis and schizophrenia are systemic neuro-immune disorders triggered by a biotic stimulus in individuals with reduced immune regulation and neuroprotection. Cells. 2021;10(11):2929. doi:10.3390/cells10112929
26. Bechter K. Schizophrenie--eine milde Enzephalitis? [Schizophrenia--a mild encephalitis?]. Fortschr Neurol Psychiatr. 2013;81(5):250–259. German. doi:10.1055/s-0033-1335253
27. Morris G, Sominsky L, Walder KR, et al. Inflammation and nitro-oxidative stress as drivers of endocannabinoid system aberrations in mood disorders and schizophrenia. Mol Neurobiol. 2022;59(6):3485–3503. doi:10.1007/s12035-022-02800-y
28. Al-Musawi AF, Al-Hakeim HK, Al-Khfaji ZA, et al. In Schizophrenia, the Effects of the IL-6/IL-23/Th17 Axis on Health-Related quality of life and disabilities are partly mediated by generalized cognitive decline and the symptomatome. Int J Environ Res Public Health. 2022;19(22):15281. doi:10.3390/ijerph192215281
29. Al-Hakeim HK, Al-Musawi AF, Al-Mulla A, Al-Dujaili AH, Debnath M, Maes M. The interleukin-6/interleukin-23/T helper 17-axis as a driver of neuro-immune toxicity in the major neurocognitive psychosis or deficit schizophrenia: a precision nomothetic psychiatry analysis. PLoS One. 2022;17(10):e0275839. doi:10.1371/journal.pone.0275839
30. Zahorec R. Ratio of neutrophil to lymphocyte counts--rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy. 2001;102(1):5–14.
31. Balta S, Demirkol S, Unlu M, Arslan Z, Celik T. Neutrophil to lymphocyte ratio may be predict of mortality in all conditions. Br J Cancer. 2013;109(12):3125–3126. doi:10.1038/bjc.2013.598
32. Kalelioglu T, Akkus M, Karamustafalioglu N, et al. Neutrophil-lymphocyte and platelet-lymphocyte ratios as inflammation markers for bipolar disorder. Psychiatry Res. 2015;228(3):925–927. doi:10.1016/j.psychres.2015.05.110
33. Mazza MG, Lucchi S, Tringali A, Rossetti A, Botti ER, Clerici M. Neutrophil/lymphocyte ratio and platelet/lymphocyte ratio in mood disorders: a meta-analysis. Prog Neuropsychopharmacol Biol Psychiatry. 2018;84(Pt A):229–236. doi:10.1016/j.pnpbp.2018.03.012
34. Olcina Rodríguez JF, Díaz Fernández J, Orta Mira N, López-Briz E, Gómez-Pajares F. Neutrophil/lymphocyte ratio: can a non-specific marker of inflammation helps to confirm the inflammatory hypothesis of the serious mental diseases? A case-control study. Med Hypotheses. 2019;130:109279. doi:10.1016/j.mehy.2019.109279
35. Özdin S, Böke Ö. Neutrophil/lymphocyte, platelet/lymphocyte and monocyte/lymphocyte ratios in different stages of schizophrenia. Psychiatry Res. 2019;271:131–135. doi:10.1016/j.psychres.2018.11.043
36. Özyurt G, Binici NC. The neutrophil-lymphocyte ratio and platelet-lymphocyte ratio in adolescent obsessive-compulsive disorder: does comorbid anxiety disorder affect inflammatory response. Psychiatry Res. 2019;272:311–315. doi:10.1016/j.psychres.2018.12.131
37. Marazziti D, Torrigiani S, Carbone MG, et al. Neutrophil/lymphocyte, platelet/lymphocyte and monocyte/lymphocyte ratios in mood disorders. Curr Med Chem. 2021;29(36):5758–5781.
38. Mazza MG, Lucchi S, Rossetti A, Clerici M. Neutrophil-lymphocyte ratio, monocyte-lymphocyte ratio and platelet-lymphocyte ratio in non-affective psychosis: a meta-analysis and systematic review. World J Biol Psychiatry. 2019;20:1–13. doi:10.1080/15622975.2019.1561058
39. Zhang Y, Lin S, Yang X, Wang R, Luo L. Prognostic value of pretreatment systemic immune-inflammation index in patients with gastrointestinal cancers. J Cell Physiol. 2019;234(5):5555–5563. doi:10.1002/jcp.27373
40. Yorulmaz A, Hayran Y, Akpinar U, Yalcin B. Systemic Immune-Inflammation Index (SII) predicts increased severity in psoriasis and psoriatic arthritis. Curr Health Sci J. 2020;46(4):352–357. doi:10.12865/CHSJ.46.04.05
41. Mei Y, Yang J, Yuan Y, et al. Systemic inflammation index values are associated with worsened disease severity and poor response to autoimmune encephalitis treatment. Front Neurol. 2021;12:709553. doi:10.3389/fneur.2021.709553
42. Wang Q, Zhu SR, Huang XP, Liu XQ, Liu JB, Tian G. Prognostic value of systemic immune-inflammation index in patients with urinary system cancers: a meta-analysis. Eur Rev Med Pharmacol Sci. 2021;25(3):1302–1310. doi:10.26355/eurrev_202102_24834
43. Fois AG, Paliogiannis P, Scano V, et al. The systemic inflammation index on admission predicts in-hospital mortality in COVID-19 patients. Molecules. 2020;25(23):5725. doi:10.3390/molecules25235725
44. Mazza MG, Palladini M, De Lorenzo R, et al. Persistent psychopathology and neurocognitive impairment in COVID-19 survivors: effect of inflammatory biomarkers at three-month follow-up. Brain Behav Immun. 2021;94:138–147. doi:10.1016/j.bbi.2021.02.021
45. Meyer JM, McEvoy JP, Davis VG, et al. Inflammatory markers in schizophrenia: comparing antipsychotic effects in Phase 1 of the clinical antipsychotic trials of intervention effectiveness study. Biol Psychiatry. 2009;66(11):1013–1022. doi:10.1016/j.biopsych.2009.06.005
46. Al-Amin MM, Nasir Uddin MM, Mahmud Reza H. Effects of antipsychotics on the inflammatory response system of patients with schizophrenia in peripheral blood mononuclear cell cultures. Clin Psychopharmacol Neurosci. 2013;11(3):144–151. doi:10.9758/cpn.2013.11.3.144
47. Balõtšev R, Haring L, Koido K, et al. Antipsychotic treatment is associated with inflammatory and metabolic biomarkers alterations among first-episode psychosis patients: a 7-month follow-up study. Early Interv Psychiatry. 2019;13(1):101–109. doi:10.1111/eip.12457
48. Meng X, Chang Q, Liu Y, et al. Determinant roles of gender and age on SII, PLR, NLR, LMR and MLR and their reference intervals defining in Henan, China: a posteriori and big-data-based. J Clin Lab Anal. 2018;32(2):e22228. doi:10.1002/jcla.22228
49. Luo H, He L, Zhang G, et al. Normal reference intervals of neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, lymphocyte-to-monocyte ratio, and systemic immune inflammation index in healthy adults: a large multi-center study from western China. Clin Lab. 2019;65(3). doi:10.7754/Clin.Lab.2018.180715
50. Sommer IE, van Westrhenen R, Begemann MJ, de Witte LD, Leucht S, Kahn RS. Efficacy of anti-inflammatory agents to improve symptoms in patients with schizophrenia: an update. Schizophr Bull. 2014;40(1):181–191. doi:10.1093/schbul/sbt139
51. Çakici N, van Beveren N, Judge-Hundal G, Koola MM, Sommer I. An update on the efficacy of anti-inflammatory agents for patients with schizophrenia: a meta-analysis. Psychol Med. 2019;49(14):2307–2319. doi:10.1017/S0033291719001995
52. Sahpolat M, Ari M, Kokacya MH. Plasma apelin, visfatin and resistin levels in patients with first episode psychosis and chronic schizophrenia. Clin Psychopharmacol Neurosci. 2020;18(1):109–115. doi:10.9758/cpn.2020.18.1.109
53. Sahpolat M, Ari M. Higher prevalence of metabolic syndrome and related factors in patients with first-episode psychosis and schizophrenia: a cross-sectional study in Turkey. Nord J Psychiatry. 2021;75(1):73–78. doi:10.1080/08039488.2020.1815080
54. Zhu X, Zhu Y, Huang J, et al. Abnormal cortisol profile during psychosocial stress among patients with schizophrenia in a Chinese population. Sci Rep. 2022;12(1):18591. doi:10.1038/s41598-022-20808-1
55. Sahpolat M, Ayar D, Ari M, Karaman MA. Elevated monocyte to high-density lipoprotein ratios as an inflammation markers for schizophrenia patients. Clin Psychopharmacol Neurosci. 2021;19(1):112–116. doi:10.9758/cpn.2021.19.1.112
56. Ramos-Lopez O, Milagro FI, Riezu-Boj JI, Martinez JA. Epigenetic signatures underlying inflammation: an interplay of nutrition, physical activity, metabolic diseases, and environmental factors for personalized nutrition. Inflamm Res. 2021;70(1):29–49. doi:10.1007/s00011-020-01425-y
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
