Back to Journals » Infection and Drug Resistance » Volume 15
Changes in Antimicrobial Resistance and Etiology of Blood Culture Isolates: Results of a Decade (2010–2019) of Surveillance in a Northern Region of Colombia
Authors Robledo J, Maldonado N, Robledo C, Ceballos Naranjo L, Hernández Galeano V, Pino JJ
Received 1 June 2022
Accepted for publication 9 September 2022
Published 20 October 2022 Volume 2022:15 Pages 6067—6079
DOI https://doi.org/10.2147/IDR.S375206
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Jaime Robledo,1– 4 Natalia Maldonado,4,5 Carlos Robledo,1,4 Laura Ceballos Naranjo,2 Valentín Hernández Galeano,2 Juan Jose Pino2 On behalf of Germen Antimicrobial Surveillance network
1Laboratorio Médico de Referencia, Medellín, Colombia; 2Escuela de Ciencias de la Salud, Universidad Pontificia Bolivariana, Medellín, Colombia; 3Unidad de Bacteriología y Micobacterias, Corporación para Investigaciones Biológicas (CIB), Medellín, Colombia; 4Grupo GERMEN, Medellín, Colombia; 5UGC Enfermedades Infecciosas y Microbiología, Hospital Universitario Virgen Macarena, Sevilla, Spain
Correspondence: Jaime Robledo, Unidad de Bacteriología y Micobacterias, Corporación para Investigaciones Biológicas, Carrera 72A No. 78B-141, Medellín, Colombia, Tel +57-4-6051808, Email [email protected]
Background: Bloodstream infections (BSI) are important causes of morbidity and mortality worldwide. Antimicrobial surveillance is essential for identifying emerging resistance and generating empirical treatment guides, the purpose of this study is to analyze trends in antimicrobial susceptibility of BSI from 2010 to 2019 in healthcare institutions from Medellin and nearby towns in Colombia.
Methods: A Whonet database was analyzed from the GERMEN antimicrobial surveillance network; frequency and antibiotic susceptibility trends were calculated on more frequent microorganisms using Mann Kendall and Sen’s Slope Estimator Test.
Results: 61,299 isolates were included; the three microorganisms more frequent showed a significant increasing trend through time E. coli (Sen’s Slope estimator = 0.7 p = < 0.01) S. aureus (Sen’s Slope estimator = 0.60 p = < 0.01) and K. pneumonia (Sen’s Slope estimator = 0.30 p = < 0.01). E. coli showed a significant increase trend in cefepime and ceftazidime resistance, while K. pneumoniae showed a significant increase in resistance to cefepime, ciprofloxacin, and gentamicin. P. aeruginosa increases its susceptibility to all analyzed antibiotics and S. aureus to oxacillin. No increasing trend was observed for carbapenem resistance.
Conclusion: An upward trends was observed in more frequent microorganisms and resistance to third and fourth-generation cephalosporins for E. coli and K pneumoniae; in contrast, not increasing trends in antibiotic resistance was observed for P. aeruginosa and S. aureus. The essential role of AMR-surveillance programs is to point out and identify these trends, which should improve antibiotic resistance control.
Keywords: bacteremia, drug resistance bacterial, antibacterial agents, antimicrobial surveillance
Introduction
Bloodstream infections (BSI) have a broad spectrum of clinical manifestations; they can vary from self-limited and asymptomatic infections to the development of sepsis.1 BSI and sepsis are among the leading causes of mortality in hospitalized patients, as high as 40% in high-income countries.2 In Europe, there are approximately 1,200,000 BSI episodes with 157,000 annual deaths, and in the United States, there are 575,000–677,000 BSI episodes per year with 79,000–94,000 deaths from this cause.3 Although the information is limited, the situation might be similar in low- and middle-income countries.2
The epidemiology and etiology of BSI are multifactorial and vary according to geographical location, age group, origin of infection, the conditions of health care, the frequency of central line associated blood stream infections, and the clonal spread of more pathogenic strains causing BSI, among others.4–7 In addition, there are important variations in corresponding antimicrobial susceptibility profiles, with an increase in the prevalence of multi-drug-resistant bacteria, especially among Gram-negative bacteria.6,7 Based on a recent report, the most common pathogens isolated from BSIs worldwide are Staphylococcus aureus (20.7%), followed by Escherichia coli (20.5%), Klebsiella pneumoniae (7.7%), Pseudomonas aeruginosa (5.3%), and Enterococcus faecalis (5.2%).6 Some of these bacteria are included in the list of microorganisms prioritized by the World Health Organization (WHO) to guide research and efforts to develop new antibiotics.8
Infections caused by resistant microorganisms are a significant public health problem. In 2019, WHO declared antimicrobial resistance (AMR) as one of the ten main public health problems facing humanity and added two indicators to its 2019–2023 program: BSI caused by E. coli resistant to third-generation cephalosporins and methicillin-resistant Staphylococcus aureus (MRSA) as well as the trend in the national consumption of antibiotics.9
The most recent report from the WHO Global Antimicrobial Resistance and Use Surveillance System (GLASS) shows a frequency of 36% for E. coli resistant to third-generation cephalosporins and 24.9% for methicillin-resistant Staphylococcus aureus causing bloodstream infections. It also shows that the highest resistance proportions were in low- and middle-income countries.10 For example, in Colombia, in hospitalized patients, the National Institute of Health reported up to 35% oxacillin resistance in S. aureus, and for K. pneumoniae and E. coli, resistance to third and fourth-generation cephalosporins was in a range between 24% and 40%.11
Surveillance of etiology and antimicrobial susceptibility patterns of microorganisms associated with BSI is an essential tool for the diagnosis, adequate treatment, and control of these infections.12 AMR surveillance active in local, regional, and national settings plays a crucial role in documenting the spread of resistance, detecting emerging resistant pathogens, and evaluating the effectiveness of control measures.10,11,13 Considering the increasing of antibiotic resistance in our country11,14 and the lack of data showing long-term surveillance, we set up a study with the objective to describe the trends in the etiologies of BSI in different age groups and hospital wards, as well as trends in their antimicrobial susceptibility patterns, by analyzing the data collected by GERMEN, a regional network of antimicrobial resistance surveillance that function in northern Colombia based in Medellín the second most populated city and in surrounding municipalities, during a decade, 2010 to 2019.
Materials and Methods
This is a retrospective, observational, and descriptive study of positive blood culture results and antimicrobial susceptibility of isolated microorganisms between 2010 and 2019. The information was obtained from the GERMEN antimicrobial surveillance network database that uses the WHONET 5.6 platform (www.whonet.org). GERMEN is an antimicrobial resistance surveillance network (www.grupogermen.org) composed of 31 medium- and high-complexity hospitals and eight clinical laboratories located in the city of Medellín and surrounding municipalities that represents 70% of hospital beds in the region.
Study setting and population: Medellin metropolitan area and surrounding municipalities have an approximate population of 4.5 million. The data included in the study were from those patients entered into the Whonet database with a first positive blood culture. Repeated isolates, isolates for screening purposes, and isolates that did not have antimicrobial susceptibility results were excluded. All participating institutions were engaged in quality assurance programs, external quality controls, and proficiency testing coordinated by the National Reference Laboratory at Colombian Instituto Nacional de Salud. In addition, the GERMEN network performed quality control of all data received in WHONET format from participating institutions yearly, following recommendations by CLSI.15
Isolate identification and Antimicrobial Susceptibility methods: All pathogens were identified and tested for antimicrobial susceptibility in each healthcare institution using automated methods, all of them used Vitek 2 (BioMérieux, Inc. Durham, NC 27712, USA) for identification and susceptibility tests. In addition, 9 of them used Maldi tof for identification purposes (either Maldi tof MS - BioMérieux, Inc. Durham, NC 27712, USA or Maldi tof Bruker Daltonics GmbH & Co. KG). Antimicrobial susceptibility testing was interpreted following the Clinical and Laboratory Standard Institute (CLSI) guidelines.16
Species of microorganisms that presented a prevalence of ≥0.5% during the study period were included in the analysis. Species with lower frequencies for descriptive analysis were grouped in the category of “others.” Descriptive analyzes of frequencies and percentages of microorganisms by age group and hospital wards were done using the WHONET 5.6 program. Age groups were classified as follows: neonates (≤28 days), pediatric (≥29 days - ≤14 years), adults (≥15 years - ≤64 years), and older adults (≥65 years). The analysis by ward was performed according to where the patient was at the time of obtaining the blood culture, intensive care unit (ICU), non-ICU hospitalization ward, emergency, and outpatient services.
Using the SPSS statistical package (v.18; SPSS Inc. Chicago, IL), trends in the frequencies of microorganisms and the antimicrobial susceptibility profiles were evaluated using Mann Kendall and Sen’s Slope Estimator Test, considering a p-value ≤0 0.05 as significant. This last analysis was done with microorganisms prioritized by the WHO and those with the highest frequencies, particularly: Escherichia coli, Staphylococcus aureus, Enterococcus faecalis, Enterococcus faecium, Klebsiella pneumoniae, Pseudomonas aeruginosa, Enterobacter cloacae and Serratia marcescens. According with this list of microorganisms the tested antibiotics analyzed were: vancomycin, oxacillin, ceftazidime, cefepime, imipenem, meropenem gentamicin, ciprofloxacin, piperacilline/tazobactam
Results
From 2010 to 2019, a total of 61,299 isolates were analyzed. The year with the highest number of isolates was 2016, with 6921 (11.3%), and the year with the lowest number was 2012, with 5130 representing 8.4% of the total isolates. An increase in the number of isolates was observed associated with an increase in the number of added institutions in later years, comparing the initial and final years of the study.
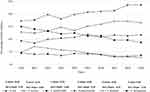
Overall, gram-negative bacteria accounted for 43.96% of isolates. In comparison, gram positives were 40.74%, 2.8% were Candida spp., and 12.4% were other bacterial species with individual frequencies less than 0.5% out of the total isolates. The most frequently isolated microorganisms was E. coli (20.38%), followed by S. aureus (14.84%), S. epidermidis (11.70%), and K. pneumoniae (10.65%). Mann Kendall and Sen’s Slope Estimator Test showed a significant upward trend in the frequency of the most isolated bacteria such as E. coli (Sen’s Slope estimator = 0.7 p = <0.01), S. aureus (Sen’s Slope estimator = 0.60 p = <0.01), K. pneumoniae (Sen’s Slope estimator = 0.30 p = <0.01) and Proteus mirabilis (Sen’s Slope estimator = 0.10 p = <0.01); during the study period while S. epidermidis (Sen’s Slope estimator = - 0.66 p = <0.01), S. hominis (Sen’s Slope estimator = - 0.55 p = <0.01) and P. aeruginosa (Sen’s Slope estimator = - 0.10 p = <0.05) had a significant tendency to decrease in frequency during the same period. The frequencies observed for the other microorganisms during the 10-year period did not show trends with significant variations (Table 1 and Figure 1).
 |
Table 1 Trends in the Frequencies of Microorganisms in BSI from Health Institutions in Medellin Area, 2010–2019 GERMEN Antimicrobial Resistance Surveillance Network |
According to age groups, 4,010 isolates were obtained from the neonatal group, 7,499 from the pediatric population, 23,556 from adults, and 21,911 isolates from older adults. For the neonate’s group, the most frequently isolated microorganisms was S. epidermidis (32.4%), followed by E. coli (8.9%), S. aureus (7.5%), Group B-streptococcus (4.2%), Candida spp. (2,0%) and S. pneumoniae (0.5%). For the pediatric age group, the most frequent microorganism found was S. epidermidis (20.0%), followed by S. aureus (14.7%), S. hominis (10.1%), E. coli (7,0%), and K. pneumoniae (6.0%). For adults, the most frequent microorganisms were E. coli (21.0%), S. aureus (16.9%), and K. pneumoniae (12.3%), while for older adults, the frequencies were E. coli (26.9%), S. aureus (14.0%) and K. pneumoniae (11.9%) (Table 2). E. coli, P. aeruginosa and P. mirabilis were more frequently isolated in older adults than in the rest of the groups. S. aureus was more frequently isolated from adults than pediatric patients, older adults, and neonates. S. hominis and S. pneumoniae were more frequent in the pediatric population, and S. epidermidis, coagulase negative staphylococci, E. faecalis, group B streptococci, and S. marcescens were more frequent in the neonatal group (Table 2).
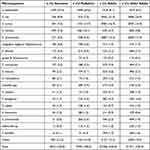 |
Table 2 Distribution of Microorganisms by Age Group in BSI from Health Institutions in Medellín Area, 2010–2019 GERMEN Antimicrobial Resistance Surveillance Network |
The analysis showed 13,491 microorganisms causing BSI isolated from patients in the intensive care unit (ICU), the most frequent bacteria were S. epidermidis (17.0%) followed by K. pneumoniae (12.5%) and S. aureus (11.0%). Meanwhile, 23,990 isolates were obtained from non-ICU hospitalization wards, and 22,390 isolates were obtained from patients in the emergency room. E. coli was the main microorganism in both places, followed by S. aureus and K. pneumoniae. Overall, the most frequent microorganisms isolated from the different services were E. coli (20.4%) and S. aureus (15.4%) (Table 3).
 |
Table 3 Distribution of Microorganisms Obtained from BSI According to Hospital Wards in Medellín Area, 2010–2019 GERMEN Antimicrobial Resistance Surveillance Network |
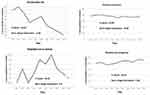
The trend analysis of antimicrobial susceptibility did not show significant changes for gram-positive cocci (Table 4, Figure 2). However, antibiotic susceptibility in gram-negative bacteria showed significant changes over time. Susceptibility to third-generation (ceftazidime) and fourth-generation (cefepime) cephalosporins in E. coli showed a significant downward trend in the studied period, going from 87.8% of isolates susceptible to ceftazidime and 87.7% to cefepime in 2010 to 76% for both antibiotics in 2019 (Sen’s Slope estimator = −1.22 p = <0.01 and Sen’s Slope estimator = −1.26 p = <0.01 respectively).
In K. pneumoniae the percentage of susceptible strains decreased significantly for cefepime going from 75.8% in 2010 to 74% in 2019 (Sen’s Slope estimator = −0.78 p = <0.05), for gentamicin going from 90.3% in 2010 to 83% in 2019 (Sen´s Slope estimator = −0.85 p = <0.05) as well as for ciprofloxacin, going from 88.2% to 81% between 2010 and 2019 (Sen’s Slope estimator = −1,23 p = <0.01). The susceptibility to carbapenems for this microorganism trends decreased, although it was not significant (Sen’s Slope estimator = −0,05 p> 0.05 for imipenem and Sen’s Slope estimator = −0,07 p> 0.05 for meropenem) (Table 4).
A significant increase in susceptible isolates percentage was observed for P. aeruginosa in each antibiotic evaluated throughout the study period. S. marcescens showed a significant increase in the susceptibility to ceftazidime from 72.9% to 84.7% (Sen’s Slope estimator = 2.13 p < 0.05) (Table 4, Figure 2).
Discussion
In the present study, 61,299 isolates from BSI registered in the database of GERMEN antimicrobial surveillance network for ten years (2010–2019) were analyzed. During this period, the most frequently isolated microorganisms were E. coli (20.4%), S. aureus (14.8%), S. epidermidis (11.7%) and K. pneumoniae (10.6%). Among all isolates, E. coli and S. aureus accounted for 35%, a finding like the 40% reported by a global wide SENTRY study.6 Compared with the stratification by regions reported by the same study, the higher frequency found in our study for E. coli (20.4%) over S. aureus (14.8%) is like that found in Europe in the period 2013 to 2016 (27% and 16.4% respectively) and Latin America (18.3% and 16.4% respectively). In a recent study in 16 hospitals in China that spanned a decade, 40% of blood culture isolates were E. coli, K. pneumoniae, and S. aureus.17
Considering the six most frequent species of microorganisms isolated, E. coli, S. aureus, S. epidermidis, K. pneumoniae, S. hominis and P. aeruginosa, the gram-negative bacilli represented 34.8% and gram-positive cocci 31.1%, with a significant tendency to increase in the decade analyzed for E. coli, S. aureus and K. pneumoniae. Two studies conducted in the USA on bloodstream infections in hospitals have also shown significant changes in the pattern of isolated microorganisms over time. The first published in 2004 with data from 1995 to 200218 in which gram-positive cocci were predominant, with 64% (Staphylococcus coagulase negative, S. aureus) and the second published in 2019 with data from 2015 to 201719 that showed almost two decades later the predominance of gram-negatives E. coli and K. pneumoniae, altogether with S. aureus.
When comparing age groups, there were differences with respect to the species isolated, S. epidermidis and coagulase-negative staphylococci were more predominant in neonates and pediatric patients (44.3% and 32.1% respectively). Whereas gram-negative bacilli were more frequent in adults and older adults (32.3% and 38.8% respectively). Other studies showed wide differences in the frequency of microorganism causing BSI between countries and regions, probably related to local epidemiological conditions and healthcare practices in pediatric populations6,20,21 and adults and older adults’ populations.6 Variations in the frequency of microorganisms isolated from blood cultures have been also associated with geographical and economic factors; a study carried out in 23 hospitals around the world showed gram negative bacilli as the most frequently isolated microorganisms from blood in centers close to the equator and with a lesser relationship between gross domestic product and health expenditures.7
In the present study, the microorganisms isolated most frequently from blood cultures in ICUs were in their order, S. epidermidis, K. pneumoniae, S. aureus and E. coli. One of the differences found between ICU and non-ICU wards was the frequency of S. epidermidis, which in the case of ICU were influenced by the higher proportion of isolates found in neonates and pediatric populations. S. epidermidis and coagulase negative staphylococci are not always clinically relevant and are usually considered contaminants; Nevertheless, data from various studies, have demonstrated its etiological role in 10% to 30% of bacteremia.22,23 In a population surveillance study such as ours, it is not possible to determine the clinical significance of S. epidermidis and coagulase negative staphylococci, since one of the criteria for inclusion in the analysis was only one isolate per patient. However, in ICU, non-ICU, and emergency services, the predominant pathogens found were S. aureus, E. coli, and K. pneumoniae, which are usually significant etiologies when isolated from blood cultures.24
During the study period, no significant changes were observed in trends of susceptibility to most of antibiotics active against gram-positive cocci. In addition, some studies have shown a decrease in the proportion of resistant phenotypes in these microorganisms. A SENTRY study analyzed the trend of methicillin-resistant S. aureus (MRSA) for 20 years (1997–2016) in several regions of the world, finding a decreasing trend in its frequency in all regions25. Other studies have documented significant changes with decreased resistance of S. aureus to oxacillin and Enterococcus spp. to vancomycin.26
The most significant trend observed in the decade analyzed was the increase in resistance to several antibiotics in E. coli and K. pneumoniae, two of the most frequent microorganisms isolated in blood cultures. In E. coli increased resistance to ceftazidime and cefepime were observed, while K. pneumoniae exhibited an increase in the resistance to cefepime, gentamicin and ciprofloxacin. The increased resistance in Enterobacteriaceae to third and fourth-generation cephalosporins found in our study coincides with data from other surveillance studies5,6,24,26 and data reported in Latin America.13,27 This increase is probably associated to the presence of CTX-M beta-lactamases which has been reported as endemic worldwide,28 in South America29 and in Colombia.14
Our data did not show a significant increase in resistance to carbapenems in Enterobacteriaceae and P. aeruginosa in the decade analyzed. However, in Latin America, the presence of isolates resistant to carbapenems that carry genes coding for carbapenemases have been reported with increasing frequency30 indicating their potential for dissemination and a further expansion in the region.
This study has the limitation of reflecting the situation of the etiology and antibiotic susceptibility in BSI isolates from a specific, although the second, more densely populated region in the country. Another limitation of this study was that not reference method for susceptibility was used, although all participant institutions perform quality control procedures for the methodologies used. In addition, all processed data were subject to quality control procedures before analysis. Furthermore, our data differ from data published for the country in K. pneumoniae which shows a significant and increasing resistance trend for carbapenem resistance from 2014 to 2016.31 These differences highlight the importance of regional antibiotic resistance surveillance programs data that uncover situations not observed in consolidated and general data, contributing to understanding regional antibiotic resistance dynamics and supporting more specific measures for its control.
Conclusion
Our study shows a significant upward trend for S. aureus, E. coli, and K. pneumoniae isolated from BSI. Furthermore, the significant increase in resistance to third and fourth-generation cephalosporins in E. coli and K. pneumoniae, suggest the presence and endemicity of extended-spectrum beta-lactamases in our region. This situation is forcing a more frequent use of carbapenems to treat these infections and, therefore, a future lookout for an increase in the frequency of carbapenemase-producing isolates. The essential role of AMR-surveillance programs is to point out and identify these trends, which should contribute together with solid infection control and antimicrobial stewardship programs to improve the control of antibiotic resistance.
Ethics Statement
Ethical approval was given by the “Comite de Etica en Investigación en Salud” (approval reference number: 20012020) from School of Health Sciences, Universidad Pontificia Bolivariana, Medellin, Colombia.
Acknowledgments
To all professionals and institutions that are part of the GERMEN antimicrobial surveillance network and have supplied the data supporting the network: Julian Camilo Galvis, Labmédico; Liliana Franco, Clínica CardioVID; Lina Maria Arteaga Florez, Clínica CES; Maria Isabel Múnera, Clínica Medellín; Yanneth López Vásquez, Clínica EMMSA; Laura Patricia Pérez, Hospital General de Medellín; Milena Zapata, Hospital San Juan de Dios; Lina Maria Ochoa Restrepo, Instituto neurológico de Colombia; Maria Melissa Pacheco, Hospital La María; Jesus Santiago Estrada Mesa, Laboratorio Clínico VID; Isabel Cristina Rios Rendon, Clinica Las Vegas; Alba Mery Gómez Castañeda, Clinica SOMER; Adriana García Muñoz, Hospital Manuel Uribe Angel; Hospital San Rafael de Itagüí; Ana Cristina Estrada Maldonado Clínica del Norte; Ana Cristina Estrada Maldonado, Clinica del Prado; Gloria Elena Durango Zapata Clinica Las Américas; Santiago Atehortua, Hospital Pablo Tobón Uribe; Cesar Alejandro Herrera Ibañez, Clínica IPS Universitaria; Julián Camilo Galvis Ayala, Clinica El Rosario; Magda Costanza Toledo Garzon, Clinica Universitaria Bolivariana; Ana Cristina Estrada Maldonado, Clinica Sagrado Corazón; Servicios de Salud Unlab; Ana Cristina Estrada Maldonado, Prolab; Natalia Llano Rendón, Clinica SOMA; Yaneth López, Laboratorio Medico Echavarría; Dinámica; Maria Isabel Múnera, Laboratorio Clínico Gonzalo Aristizábal; ESIMED; Ana Cristina Estrada Maldonado, Hospital Concejo de Medellín; Leandro Pérez Castro, Clínica San Juan de Dios; Isabel Cristina Rios Rendon, Clínica Vida; Clínica Conquistadores; Hospital Mental de Antioquia and Tatiana Ospina, Clínica Fundadores.
To Nidia Correa for making a critical review, translation an edition of the manuscript. To Julian Galvis for his help with statistical analysis.
Disclosure
JR and CR had given expert talks paid by Biomerieux. Germen surveillance network has received unrestricted grants from Biomerieux, Pfizer, Becton Dickinson, Astra Zeneca and Zambon Laboratories. The authors report no other potential conflicts of interest in relation to this work.
References
1. Martinez RM, Wolk DM, Hayden RT, Wolk DM, Carroll KC, Tang Y-W. Bloodstream Infections. Microbiol Spectr. 2016;4(4). doi:10.1128/MICROBIOLSPEC.DMIH2-0031-2016
2. Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the Global Burden of Disease Study. Lancet. 2020;395(10219):200–211. doi:10.1016/S0140-6736(19)32989-7
3. Goto M, Al-Hasan MN. Overall burden of bloodstream infection and nosocomial bloodstream infection in North America and Europe. Clin Microbiol Infect. 2013;19(6):501–509. doi:10.1111/1469-0691.12195
4. Mcalearney AS, Hefner JL. Getting to zero: goal commitment to reduce blood stream infections. Med Care Res Rev. 2015:1–20. DOI:10.1177/1077558715616028
5. Kraker De MEA, Jarlier V, Monen JCM, Heuer OE, Sande Van De N, Grundmann H. The changing epidemiology of bacteraemias in Europe: trends from the European antimicrobial resistance surveillance system. Clin Microbiol Infect. 2012;19(9):860–868. doi:10.1111/1469-0691.12028
6. Diekema DJ, Hsueh PR, Mendes RE, et al. The microbiology of bloodstream infection: 20-year trends from the SENTRY antimicrobial surveillance program. Antimicrob Agents Chemother. 2019;63(7). doi:10.1128/AAC.00355-19
7. Fisman D, Patrozou E, Carmeli Y, et al. Geographical variability in the likelihood of bloodstream infections due to gram-negative bacteria: correlation with proximity to the equator and health care expenditure. PLoS One. 2014;9(12):1–18. doi:10.1371/journal.pone.0114548
8. World Health Organization (WHO). WHO global priority list of antibiotic-resistant bacteria to guide research, discovery, and development of new antibiotics; 2017. Available from: https://apps.who.int/iris/handle/10665/311820.
9. World Health Organization. Thirteenth general programme of work, 2019–2023. Geneva; 2019. Available from: https://apps.who.int/%0Airis/bitstream/handle/10665/324775/WHO-PRP-18.1-eng.pdf,%0A.
10. Agnew E, Dolecek C, Hasan R, et al. Global Antimicrobial Resistance and Use Surveillance System (GLASS) Report; 2021. Available from: http://www.who.int/glass/resources/publications/early-implementation-report-2020/en/.
11. Instituto Nacional de Salud. Vigilancia Por Laboratorio En Infecciones Asociadas a La Atención En Salud (IAAS) Colombia, Años 2012 [Laboratory surveillance of healthcare associated infections Colombia years 2012 to 2020]; 2021. Spanish. Available from: https://www.ins.gov.co/buscador-eventos/Informacin.delaboratorio/vigilancia-por-laboratorio-de-resistencia-antimicrobiana-en-iaas-en-colombia-año-2016-A-2020.pdf.
12. Johnson A. Surveillance of antibiotic resistance. Philos Trans R Soc B Biol Sci. 2015;370(1670):1670. doi:10.1098/rstb.2014.0080
13. ReLAVRA/OPS. Red Latinoamericana y del Caribe de Vigilancia de la Resistencia a los Antimicrobianos [Latinoamerican and caribbean network for AMR surveillance] - ReLAVRA+. OPS/OMS 2012; 2021. Available from: https://www3.paho.org/hq/index.php?option=com_content&view=article&id=13682:.
14. Rada AM, Hernández-Gómez C, Restrepo E, Villegas MV. Distribución y caracterización molecular de betalactamasas en bacterias Gram negativas en Colombia, 2001–2016. [Distribution and molecular characterization of beta-lactamases in gram negative bacteria in Colombia, 2001-2016] Biomédica. 2019;39:199–220. doi:10.7705/BIOMEDICA.V39I3.4351
15. Clinical and Laboratory Standards Institute. CLSI: Analysis and Presentation of Cumulative Antimicrobial Susceptibility Test Data.
16. Wayne PA. Performance Standards for Antimicrobial Susceptibility Testing. M-100.
17. Jin L, Zhao C, Li H, Wang R, Wang Q, Wang H. Clinical profile, prognostic factors, and outcome prediction in hospitalized patients with bloodstream infection: results from a 10-year prospective multicenter study. Front Med. 2021;8. doi:10.3389/fmed.2021.629671.
18. Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB. Cases from a prospective nationwide surveillance study. BSI US Hosp • CID; 2004: 179. Available from: https://academic.oup.com/cid/article/39/3/309/351413.
19. Sader HS, Castanheira M, Streit JM, Flamm RK. Frequency of occurrence and antimicrobial susceptibility of bacteria isolated from patients hospitalized with bloodstream infections in United States medical centers (2015–2017). Diagn Microbiol Infect Dis. 2019;95(3):114850. doi:10.1016/j.diagmicrobio.2019.06.002
20. Morkel G, Bekker A, Marais BJ, Kirsten G, van Wyk J, Dramowski A. Bloodstream infections and antimicrobial resistance patterns in a South African neonatal intensive care unit. Paediatr Int Child Health. 2014;34(2):108–114. doi:10.1179/2046905513Y.0000000082
21. Spaulding AB, Watson D, Dreyfus J, et al. Epidemiology of bloodstream infections in hospitalized children in the United States, 2009–2016. Clin Infect Dis. 2019;69(6):995–1002. doi:10.1093/cid/ciy1030
22. Beekmann SE, Diekema DJ, Doern GV. Determining the clinical significance of coagulase-negative staphylococci isolated from blood cultures. Infect Control Hosp Epidemiol. 2005;26(6):559–566. doi:10.1086/502584
23. Finkelstein R, Fusman R, Oren I, Kassis I, Hashman N. Clinical and epidemiologic significance of coagulase-negative staphylococci bacteremia in a tertiary care university Israeli hospital. Am J Infect Control. 2002;30(1):21–25. doi:10.1067/mic.2002.118406
24. Pien BC, Sundaram P, Raoof N, et al. The clinical and prognostic importance of positive blood cultures in adults. Am J Med. 2010;123(9):819–828. doi:10.1016/j.amjmed.2010.03.021
25. Diekema DJ, Pfaller MA, Shortridge D, Zervos M, Jones RN. Twenty-year trends in antimicrobial susceptibilities among Staphylococcus aureus from the SENTRY Antimicrobial Surveillance Program. Open Forum Infect Dis. 2019;6(Suppl 1):S47–S53. doi:10.1093/ofid/ofy270
26. Pfaller MA, Carvalhaes CG, Smith CJ, Diekema DJ, Castanheira M. Bacterial and fungal pathogens isolated from patients with bloodstream infection: frequency of occurrence and antimicrobial susceptibility patterns from the SENTRY Antimicrobial Surveillance Program (2012–2017). Diagn Microbiol Infect Dis. 2020;97(2):115016. doi:10.1016/j.diagmicrobio.2020.115016
27. Salles MJC, Zurita J, Mejía C, et al. Resistant Gram-negative infections in the outpatient setting in Latin America. Epidemiol Infect. 2013;141(12):2459–2472. doi:10.1017/S095026881300191X
28. Cantón R, Coque TM. The CTX-M β-lactamase pandemic. Curr Opin Microbiol. 2006;9(5):466–475. doi:10.1016/j.mib.2006.08.011
29. Radice M, Power P, Di Conza J, et al. Early dissemination of CTX-M-derived enzymes in South America [3] (multiple letters). Antimicrob Agents Chemother. 2002;46(2):602–604. doi:10.1128/AAC.46.2.602-604.2002
30. García-Betancur JC, Appel TM, Esparza G, et al. Update on the epidemiology of carbapenemases in Latin America and the Caribbean. Expert Rev Anti Infect Ther. 2021;19(2):197–213. doi:10.1080/14787210.2020.1813023
31. Panamerican Health Organization. Magnitud y tendencias de la resistencia a los antimicrobianos en Latinoamérica. ReLAVRA 2014, 2015, 2016. Informe resumido [Magnitude and Trends of Antimicrobial Resistance in Latin America. ReLAVRA 2014, 2015, 2016. Summary Report]; 2020. Spanish. Available from: https://www.Paho.org/es/documentos/magnitud-tendencias-resistencia-antimicrobianos-latinoamerica-relavra-2014-2015-2016. Accessed October 8, 2022.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.