Back to Journals » International Journal of General Medicine » Volume 14
Challenges of Implementing an mHealth Application for Personalized Physical Activity Counselling in Primary Health Care: A Qualitative Study
Authors Wattanapisit A , Amaek W , Wattanapisit S, Tuangratananon T, Wongsiri S, Pengkaew P
Received 23 April 2021
Accepted for publication 9 July 2021
Published 24 July 2021 Volume 2021:14 Pages 3821—3831
DOI https://doi.org/10.2147/IJGM.S317241
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Apichai Wattanapisit,1,2 Waluka Amaek,3 Sanhapan Wattanapisit,4 Titiporn Tuangratananon,5 Sunton Wongsiri,6 Prasert Pengkaew7
1School of Medicine, Walailak University, Nakhon Si Thammarat, Thailand; 2Walailak University Hospital, Nakhon Si Thammarat, Thailand; 3College of Graduate Studies, Walailak University, Nakhon Si Thammarat, Thailand; 4Thasala Hospital, Nakhon Si Thammarat, Thailand; 5International Health Policy Program, Ministry of Public Health, Nonthaburi, Thailand; 6Faculty of Medicine, Prince of Songkla University, Songkhla, Thailand; 7School of Informatics, Walailak University, Nakhon Si Thammarat, Thailand
Correspondence: Apichai Wattanapisit
School of Medicine, Walailak University, 222, Thaiburi, Thasala, Nakhon Si Thammarat, 80161, Thailand
Tel +66 7567 2801
Fax +66 7567 2807
Email [email protected]
Introduction: A mobile health (mHealth) technology has the potential to facilitate personalized physical activity (PA) counselling. We aimed to explore the feasibility and challenges of implementing a newly developed mHealth application (PAC app) for personalized PA counselling.
Material and Methods: A qualitative design employed a descriptive phenomenology approach. Data were collected through focus group discussions (FGDs) with primary health care (PHC) providers and were analyzed using a deductive thematic approach.
Results: A total of 16 participants participated in four FGDs. Four major themes were found: application for personalized PA counselling, barriers to the use of the application by providers, patient involvement, and impact on PHC services.
Discussion: The results showed that the new mHealth application can potentially facilitate PA counselling. However, its use in PHC settings requires an understanding of the context of service delivery; the challenges faced by providers and patients and effects on services must be considered.
Conclusion: Future research should focus on the long-term use of PAC app and its impact on behavioral and health outcomes.
Keywords: counselling, mHealth, personalization, physical activity, primary health care
Introduction
Physical activity (PA) counselling is an intervention to promote PA in clinical settings.1 It is considered as an effective intervention for promoting lifestyle changes in patients in primary health care (PHC).2,3 The recent evidence showed that long-term interventions (12-month follow-up) might be more effective than shorter interventions (6-month follow-up).4 The prevalence of PA counselling in PHC varies.5,6 A study reported a discrepancy between physician-reported (high: 90% reported offering PA counselling) and patient-reported (low: 8.6% reported receiving PA counselling) prevalence.5 This may reflect the different perspectives of health care providers and patients. A major target for PA counselling is patients with chronic illnesses (eg, diabetes mellitus, hypertension, and osteoarthritis).5 However, a lack of specific training in this area, time constraints, and heavy clinical workload are barriers to the provision of PA counselling by PHC providers.7,8
Mobile health (mHealth), which uses mobile devices to support medical and public health practice,9 has played an increasingly important role in community health care and PHC.10,11 Applications on mobile devices are a well-established form of mHealth and have the potential to support several clinical tasks.11 For example, a user can rely on a mobile device application to maintain a healthy lifestyle such as being physically active and eating healthy diet without a face-to-face consultation with a PHC provider. The use of mHealth applications for PA counselling has become more common in the past decade.12 However, the usability and utility of this technology are inconsistent.12 The development of more effective mHealth applications requires an understanding of context and the needs of users.13 The adoption of new mHealth applications is influenced by various factors such as ease of use, utility, trustworthiness, and cost-effectiveness.14–17
We developed an mHealth application for personalized PA counselling based on a literature review and the requirements of users.12,13 However, as the adoption of the application by PHC providers is a major challenge. The present study investigated the feasibility and challenges of the implementation of an mHealth application for personalized PA counselling.
Materials and Methods
Study Design
This study was part of the “Developing a physical activity counselling mobile application in primary care” research and development project. The qualitative portion was conducted between March and April 2021. Descriptive phenomenology was used as the qualitative approach.18 We adopted the Standards for Reporting Qualitative Research (SRQR) and the Consolidated Criteria for Reporting Qualitative Research (COREQ) for the transparent presentation of qualitative methodologies and manuscript writing.19,20
Context and Implementation of an mHealth Application
Application Development
The development of the mHealth application consisted of three phases. We initially reviewed existing electronic health technologies for personalized PA counselling in PHC.12 We then conducted qualitative research to explore the requirements of PHC providers at 3 hospital-based PHC clinics in Nakhon Si Thammarat, Thailand.13 The previous findings reflected a shortage of staff and heavy workload of the setting, which each PHC provider saw 40 patients per day (range 15–100) with a 5-minute contact per patient (range 2–20).13 Finally, our team—which included medical doctors (AW, SWa, TT, and SWo); an industrial designer (WA); and a computer scientist (PP)—developed and validated the mHealth application, “PAC app”. The name of application, PAC app, is an acronym for physical activity counselling application. PAC app is a free application available for android (https://play.google.com/store/apps/details?id=com.pacapp) and iOS (https://apps.apple.com/th/app/pac-app/id1546745127) phones. The application was designed to be either self-guided or provider-assisted. Patients can use the application at home without support from PHC providers or operate it in a waiting room to prepare the individual information for discussing with PHC providers. On the other hand, PHC providers utilize the application as a tool to collect the patient’s profiles and generate personalized PA advice for communicating with the patient. Table 1 summarizes the process, inputs, and outputs of PAC app. Figure 1 illustrates the summary of individualized advice.
 |
Table 1 Summary of the Process, Inputs, and Outputs of PAC App |
 |
Figure 1 Summary pages on PAC app. |
Workshop on PA Counselling
The first author (AW) conducted the two-hour-workshops on PA counselling at the three community hospitals where the previous qualitative research was conducted in February and March 2020.13 The workshop participants were physicians, nurses, and public health officers at the hospitals and their PHC networks. Each workshop had 8–40 participants. The content of the workshops included basic concepts of PA, current PA guidelines, personalized PA counselling processes in PHC, and the use of PAC app to support personalized PA counselling. The author presented the details and functions of PAC app and invited participants to download the application on their mobile phones. The participants could voluntarily download PAC app and inquire about the use of PAC app at the workshop. The author asked the participants to introduce PAC app to their PHC colleagues and use the application at their clinics if possible.
Data Collection
Participants of the study were PHC providers at the three community hospitals and their PHC networks. The authors contacted the workshop participants by phone calls after four to six weeks apart from the workshops on PA counselling. The authors asked the workshop participants if they and their PHC colleagues were able to participate in the qualitative study. Both workshop participants and nonparticipants were invited to take part in the data collection to achieve triangulation and lend credibility to the data.21 The participants provided written consent prior to the focus group discussions (FGDs) and were asked a short set of questions that provided us with data on participants’ characteristics. The study was conducted according to the guidelines of the Declaration of Helsinki and was approved by the Ethics Committee of Walailak University (approval no. WUEC-19-227-01).
Two authors (AW and SWa), who are family physicians trained and experienced in qualitative research, conducted all FGDs in Thai to assess the feasibility and challenges of the mHealth application for personalized PA counselling. Each FGD had four participants and took 30–40 min. The FGDs were conducted at the hospitals and were recorded with a digital audio recorder with the permission of the participants. The semi-structured interview guide generated by the authors based on the objectives of the study and the discussions of the research team was used in the FGDs (Table 2). The participants were asked probing questions to explore the deeper meaning of their answers. A research assistant with experience in qualitative audio transcription was present at each FGD as a note taker. The number of FGDs depended on the saturation of data, which no new data reproduced.22
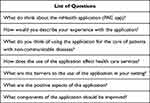 |
Table 2 Semi-Structured Interview Guide |
Data Analysis
All digital audio records were transcribed verbatim (word-for-word) by a research assistant. The transcripts were typed as text files in Microsoft Word (Office 365 University Package; Microsoft, Redmond, WA, USA). Subsequently were imported into the qualitative data analysis software, NVivo (Release 1.3) (QSR International, Victoria, Australia). The participants’ identifiers were coded to preserve confidentiality and anonymity. The data were analyzed with a deductive thematic approach.23,24 Initially, two authors (AW and SWa) read and reread the transcripts to familiarize themselves with the data. The author (AW) generated initial codes and collated the codes into thematic maps, which were cross-checked by another author (SWa). The two authors defined the final themes. Any disagreement in data analysis was resolved through discussion and consensus by the research team. The themes and selected quotes were translated from Thai to English by one author (AW) during manuscript writing. All authors verified and approved the translation.
Results
Four FGDs were conducted with 16 participants. Most participants were female (n = 15, 93.8%) and nurses (n = 12, 75.0%). The median age was 38.5 years (range 24–56 years). The median clinical experience was 14.5 years (range 1–34 years). Fifteen (93.8%) attended the workshop on PA counselling. The majority of participants (n = 10, 62.5%) tried to use PAC app for personalized PA counselling in their professional practice (Table 3).
 |
Table 3 Participant Characteristics |
Table 4 presents the summary of codes and themes that emerged from the qualitative data analysis. There were four major themes: (i) application for personalized PA counselling; (ii) barriers to the use of the application by providers; (iii) patient involvement; and (iv) impact on services. Figure 2 summarizes the themes and the relationships between the study findings and the practice of PA counselling.
 |
Table 4 Summary of Codes and Themes |
 |
Figure 2 Summary of themes and conceptual framework. |
Theme 1: Application for Personalized PA Counselling
PAC app was created as a supportive tool to facilitate personalized PA counselling. However, the participants raised some concerns about the application.
Potential Benefits
The application synthesized patient information and offered individualized advice and was thus able to facilitate personalized PA counselling. The application was capable of providing feedback and encouraging patients to change their behaviors.
I think it is good because some patients are concerned about their health and ask about blood tests and how to control for better glucose and lipid results. They also ask what type of exercise is suitable for them. The application is helpful. It makes me more confident when counselling patients. The application helps me to assess information and provides data.
(P2, FGD1, nurse, 2 years of clinical experience)
For example, the patient had not engaged in [regular exercise]. The application showed that the patient was aware of her behavior. The patient said she was aware of it, but the problem was that nothing happened. Then she said “Okay, I will start.” [The application] gave her the confidence to start.
(P9, FGD3, nurse, 19 years of clinical experience)
The best thing about the application is the summary pages. The advice helps to encourage the patient. Some patients intend to exercise, but they do not start. The assessment [by the application] shows the results. Patients feel motivated. It is a positive reinforcement.
(P12, FGD3, nurse, 4 years of clinical experience)
Need for Improvement
There was a need to improve some aspects of the application. A bug-fixing process was critical for improving the validity and reliability of the application. Other elements including language issues (eg, the Thai translation of the word “physical activity” was not as understandable to most patients as “exercise”), printout advice, and more choices of PA were identified as additional areas for further development.
Use of the word “exercise” – what type of exercise? I think it is more understandable [than “physical activity”]. The questions will be clearer.
(P15, FGD4, nurse, 24 years of clinical experience)
Some patients had no symptoms of the disease, but the summary page showed “yes” for symptoms. It was an error that I found.
(P2, FGD1, nurse, 2 years of clinical experience)
I wish to see good data transfer. If a document could be printed [from the application], it could be transferred to the doctor.
(P7, FGD2, Public health officer, 14 years of clinical experience)
I will keep a printout [of the results from the application] in the patient’s folder. If the doctor wants to use it, I will give the patient a prescription [for PA/exercise].
(P5, FGD2, nurse, 34 years of clinical experience)
I want to see more exercise choices for older people—exercises that are light and low-impact.
(P9, FGD3, nurse, 19 years of clinical experience)
Theme 2: Barriers to the Use of the Application by Providers
The use of PAC app for personalized PA counselling created an additional task for providers (ie, managing the new technology). Some participants mentioned that embedding PAC app into the existing electronic medical record system could help to overcome some of the barriers to the use of the application.
Technical Difficulties
Certain processes were required before providers could start to use PAC app. Providers had to download the application onto their mobile phones and create a new account. The application did not collect any personal identifiers and therefore could not identify individual patients after several operations with the same account. Alternatively, providers could create an account for each patient and record the username and password for the patient.
I left the workshop early. I tried to download the application at home but could not find it [on the download platform].
(P11, FGD3, nurse, 11 years of clinical experience)
Ah, I totally forgot the password. What was it? I created a new account. I did it twice. I have many usernames and passwords [for different applications].
(P5, FGD2, nurse, 34 years of clinical experience)
Integrating the Application into Electronic Medical Records
Using the application on mobile phones was considered difficult because the providers were distracted by a different electronic device. Integrating the application into the electronic medical record system would facilitate its use, as personal information (eg, birth date, body weight, and height) would be filled in automatically. Additionally, it was suggested that PA counselling should be an optional module of the electronic medical record system.
The application should be synced with the HosXP [electronic medical record system]. It would be more convenient if the application were embedded in HosXP.
(P2, FGD1, nurse, 2 years of clinical experience)
If [PAC app] is in HosXP, I could enter the patient’s information and could follow up [with the information]. If it is in here [on a provider’s mobile phone with a provider’s account], I would not know whose information it was.
(P9, FGD3, nurse, 19 years of clinical experience)
Theme 3: Patient Involvement
The application could involve the patient in two different ways. Firstly, the patient could use the application without any support from providers. Thereafter, the patient could see the results generated by the application or discuss them with providers. Secondly, the patient could receive information and counselling from providers based on results provided by the application.
Patients as Non–Tech-Savvy People
Patients—especially older people in rural areas—had difficulties using the technology. In this context, it was impossible to introduce a self-guided mHealth application to most patients.
A patient had a mobile phone, but his child did everything for him. The child tried to download the application [without success]. I tried to assist but was unsuccessful because his phone was an iPhone [mine is an Android phone]. His phone memory was full, so I could not download the application for him.
(P8, FGD2, public health officer, 2 years of clinical experience)
I personally think there are limitations to using the application at the non-communicable disease clinic such as age and use of technology. Hypertensive patients may be better able to use the application than most diabetic patients, who are older and do not use smartphones. If we implement this application at the clinic, we could ask patients’ caregivers to help. It is difficult for older patients to use the application.
(P15, FGD4, nurse, 24 years of clinical experience)
There are limitations in understanding. Some patients cannot access technologies. Age and education level influence the use of the application.
(P14, FGD4, nurse, 8 years of clinical experience)
Personal Device and Account
Most patients with chronic non-communicable diseases were elderly, and only a small proportion used smartphones. It was impractical to ask patients to remember their username and password.
For example, if patients use their mobile phone, they need to remember the password and username. At the next visit, the patient will forget them.
(P5, FGD2, nurse, 34 years of clinical experience)
As mentioned earlier, most patients in my setting are older people. They do not have smartphones. I used my phone [to operate the application].
(P12, FGD3, nurse, 4 years of clinical experience)
Theme 4: Impact on Services
The use of PAC app could potentially improve the practice of personalized PA counselling. However, its processes required time and labor.
Time-Consuming Process
PHC providers saw many patients each day. Balancing workload and human resources was a major challenge. Using PAC app was considered as an additional task that required extra time.
If we expect 100% [use of the application for each patient], it would affect our service. We are now trying to use it [with a small number of patients]. It is still manageable.
(P1, FGD1, nurse, 8 years of clinical experience)
If we are expected to use the application for each patient, a huge number of patients would be a limitation. There are many patients each day. It would be better if we use the application just for some patients.
(P14, FGD4, nurse, 8 years of clinical experience)
Requiring Technical Support
Using PAC app in clinics would be more feasible if technical support were provided. This could be in the form of introductory material to explain the application and its use; alternatively, supportive or trained staff could help both patients and providers to download the application, create a new account, and use the application.
We can introduce patients to the application. We can provide an introductory video on YouTube, which can be accessed [at the clinic] to inform patients that a new application is available and suggesting that they try it. This can reduce our workload. Some patients or caregivers can follow the YouTube video. It would be great if we have the YouTube video. This is just my opinion.
(P16, FGD4, physician, 21 years of clinical experience)
We need at least one person who is trained in using the application. It takes time to complete several activities.
(P5, FGD2, nurse, 34 years of clinical experience)
Discussion
This qualitative study assessed the feasibility and challenges of implementing a new mHealth application for personalized PA counselling. PAC app was developed based on evidence-based sources and the requirements of PHC providers. The application has the potential to facilitate PA counselling. However, a number of issues were mentioned as areas needing improvement; several aspects were related to the implementation of the application in the clinical settings. Providers mentioned the technical difficulties associated with PAC app as a major challenge. Integrating the application into the existing electronic medical record system could improve the utility of the application. Patient involvement was an important component. Personal mobile devices and knowledge were the key concerns regarding the use of the application. Using PAC app for PA counselling affected routine services. An approach to using the application more efficiently and technical support are required.
The PAC app was developed based on current PA guidelines, exercise preparticipation health screening, and Exercise is Medicine® health care providers’ action guide, which personalize PA counselling.25–27 In designing the application, we also considered the technological utility, user requirements, and characteristics of PHC services to encourage the adoption and improve the usability of the application by PHC providers.8,12,13 In one study, mHealth solutions for supporting the management of chronic conditions in the elderly based on data from 42 published articles included a user-centered design and interdisciplinary team approach.28 The design of PAC app was in accordance with these two core solutions. However, the results of our study raise a number of issues related to the adoption and implementation of a new mHealth application for PA counselling, suggesting that using an mHealth technology as a tool to support personalized medicine requires more than a well-designed application. Although the application has the potential to perform the intended task, further improvement is needed based on user feedback. Other external factors such as characteristics of PHC services and users’ attitude and experience that could facilitate or prohibit the implementation of an mHealth application in a specific setting should be considered.
Ten out of 16 participants tried PAC app for PA counselling, demonstrating the possibility of implementing this technology for clinical purposes. One study reported that the adoption of mHealth among PHC physicians varied according to the mHealth application’s functions.29 Common reasons for using mHealth applications were medical references (77.0%), medical calculation (78.3%), and to a lesser extent, for tracking health information (22.1%), patient education (14.3%), and interacting with electronic health records (30.9%).29 The results of the aforementioned study revealed a lack of interaction between PHC providers and patients; that is, providers tended to use mHealth applications as sources of medical knowledge rather than as a tool to interact with their patients. Challenges of implementing the PA counselling application included technical difficulties and integration into optional platforms (electronic medical record system). Educating users on the application could promote its implementation in PHC services.30 Although PAC app was designed for both patients and PHC providers, only providers were considered as the end users in this initial phase to test the application. The findings showed that there was a need to train PHC providers to use the application and deal with some minor technical issues. The development of a PA counselling functionality embedded in the electronic medical record system involves several steps including new coding and graphic design. Moreover, an mHealth application integrated into the electronic medical record system must ensure privacy, access, safety, ethics, and quality.31,32 This should be the next step in the development of PAC app.
The usability and utility of mHealth for PA counselling varies across studies.12 The intent to use mHealth technologies was critical for its acceptance by patients.33–36 Both intrinsic (eg, sex, age, education level, self-efficacy, usage experience, and health perception) and extrinsic (eg, social influence and facilitating conditions) factors were associated with the intent to use mHealth technologies.33–36 The findings of our study were based on the perspectives of PHC providers on patients’ use and acceptance, which does not reflect all aspects of personal factors. According to our results, it is unlikely that patients will use the application for PA counselling without support from caregivers and PHC providers. In terms of care delivery, the use of an mHealth application for PA counselling depends on the service workflow; a time-consuming process was considered a disadvantage of mHealth technology.37 Providing training and technical support and establishing a collaborative team of PHC providers may improve the use of mHealth technology in PHC services.37,38
Some strengths of this study should be highlighted. The study was conducted at similar sites as a previous study exploring the views of PHC providers on the development of an mHealth application.13 Some providers participated in both studies to express their requirements and provide feedback on the use of the application. Prior to this qualitative study, the authors conducted workshops on PA counselling to introduce relevant concepts as well as details of the application, which highlighted the importance of personalized PA counselling for patients with chronic diseases.
There were some limitations to this study. Firstly, it included a small number of participants and there was an imbalance in the distribution of professions and gender (eg, there was only one male participant, who was also the sole physician). This was also a limitation of our previous study because of the limited number of staff at the clinics.13 We invited more providers from the hospitals’ PHC networks who attended the workshops to participate in the present study. However, only 16 participants (15 from three hospitals and one from the PHC network) accepted the invitation. Generalizability was another limitation of the qualitative study design, as the study was conducted at three community hospitals in Southern Thailand. The findings of the study may shed light on the wider understanding of the implementation of an mHealth application for personalized PA counselling, however, the findings would not be fully generalized to other contexts.
Conclusion
The findings of this study provide insight into the feasibility and challenges of implementing an mHealth application for personalized PA counselling. PAC app should be modified and updated to improve the essential functions and reduce the bugs in the program. The application should be a user-friendly tool for patients and providers that requires minimal technological understanding or experience. Additionally, the use of the application should be dependent on the workflow of PHC services. Future research should focus on the long-term use of PAC app and its effect on behavioral and health outcomes. In addition, a qualitative research on patients’ perspectives toward the use of the application will be valuable to improve the future version of PAC app.
Acknowledgments
The authors thank the hospital directors and primary health care staff for their support and participation; and Aekthawat Watthanachon for assistance with research administration.
Funding
This research was funded by The Medical Association of Thailand. The APC was partially funded by Walailak University under the new strategic research (P2P) project.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wattanapisit A, Wattanapisit S, Wongsiri S. Overview of physical activity counseling in primary care. Korean J Fam Med. 2020. doi:10.4082/kjfm.19.0113
2. Elley CR, Kerse N, Arroll B, et al. Effectiveness of counselling patients on physical activity in general practice: cluster randomised controlled trial. BMJ. 2003;326:793. doi:10.1136/bmj.326.7393.793
3. Orrow G, Kinmonth A-L, Sanderson S, et al. Effectiveness of physical activity promotion based in primary care: systematic review and meta-analysis of randomised controlled trials. BMJ. 2012;344(1):e1389. doi:10.1136/bmj.e1389
4. van der Wardt V, Di Lorito C, Viniol A. Promoting physical activity in primary care: a systematic review and meta-analysis. Br J Gen Pract. 2021;71(706):e399–e405. doi:10.3399/BJGP.2020.0817
5. Füzéki E, Weber T, Groneberg DA, et al. Physical activity counseling in primary care in Germany—an integrative review. Int J Environ Res Public Health. 2020;17:5625. doi:10.3390/ijerph17155625
6. Gabrys L, Jordan S, Schlaud M. Prevalence and temporal trends of physical activity counselling in primary health care in Germany from 1997–1999 to 2008–2011. Int J Behav Nutr Phys Act. 2015;12(1):136. doi:10.1186/s12966-015-0299-9
7. Hébert ET, Caughy MO, Shuval K. Primary care providers‘ perceptions of physical activity counselling in a clinical setting: a systematic review. Br J Sports Med. 2012;46(9):625–631. doi:10.1136/bjsports-2011-090734
8. Wattanapisit A, Thanamee S, Wongsiri S. Physical activity counselling among GPs: a qualitative study from Thailand. BMC Fam Pract. 2019;20(1):72. doi:10.1186/s12875-019-0968-x
9. World Health Organization. mHealth: New Horizons for Health Through Mobile Technologies: Second Global Survey on eHealth. Geneva, Switzerland: World Health Organization; 2011.
10. Early J, Gonzalez C, Gordon-Dseagu V, et al. Use of mobile health (mHealth) technologies and interventions among community health workers globally: a scoping review. Health Promot Pract. 2019;20(6):805–817. doi:10.1177/1524839919855391
11. Wattanapisit A, Teo CH, Wattanapisit S, et al. Can mobile health apps replace GPs? A scoping review of comparisons between mobile apps and GP tasks. BMC Med Inform Decis Mak. 2020;20(1):5. doi:10.1186/s12911-019-1016-4
12. Wattanapisit A, Tuangratananon T, Wattanapisit S. Usability and utility of eHealth for physical activity counselling in primary health care: a scoping review. BMC Fam Pract. 2020;21(1):229. doi:10.1186/s12875-020-01304-9
13. Wattanapisit A, Wattanapisit S, Tuangratananon T, et al. Primary health care providers’ perspectives on developing an eHealth tool for physical activity counselling: a qualitative study. J Multidiscip Healthc. 2021;14:321–333. doi:10.2147/JMDH.S298390
14. Akdur G, Aydin MN, Akdur G. Adoption of mobile health apps in dietetic practice: case study of diyetkolik. JMIR Mhealth Uhealth. 2020;8(10):e16911. doi:10.2196/16911
15. Alam MZ, Hoque MR, Hu W, Barua Z. Factors influencing the adoption of mHealth services in a developing country: a patient-centric study. Int J Inf Manage. 2020;50:128–143. doi:10.1016/j.ijinfomgt.2019.04.016
16. Hoque R, Sorwar G. Understanding factors influencing the adoption of mHealth by the elderly: an extension of the UTAUT model. Int J Med Inform. 2017;101:75–84. doi:10.1016/j.ijmedinf.2017.02.002
17. Jacob C, Sanchez-Vazquez A, Ivory C. Understanding clinicians’ adoption of mobile health tools: a qualitative review of the most used frameworks. JMIR Mhealth Uhealth. 2020;8:e18072. doi:10.2196/18072
18. Matua GA, Van Der Wal DM. Differentiating between descriptive and interpretive phenomenological research approaches. Nurse Res. 2015;22(6):22–27. doi:10.7748/nr.22.6.22.e1344
19. O’Brien BC, Harris IB, Beckman TJ, et al. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–1251. doi:10.1097/ACM.0000000000000388
20. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. doi:10.1093/intqhc/mzm042
21. Patton MQ. Enhancing the quality and credibility of qualitative analysis. Health Serv Res. 1999;34:1189–1208.
22. Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant. 2018;52(4):1893–1907. doi:10.1007/s11135-017-0574-8
23. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi:10.1191/1478088706qp063oa
24. Gale NK, Heath G, Cameron E, et al. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13(1):117. doi:10.1186/1471-2288-13-117
25. American College of Sports Medicine. Exercise is medicine: healthcare providers’ action guide. Available from: https://www.exerciseismedicine.org/support_page.php/provider-action-guide/.
26. Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–1462. doi:10.1136/bjsports-2020-102955
27. Riebe D, Franklin BA, Thompson PD, et al. Updating ACSM’s recommendations for exercise preparticipation health screening. Med Sci Sports Exerc. 2015;47(11):2473–2479. doi:10.1249/MSS.0000000000000664
28. Matthew-Maich N, Harris L, Ploeg J, et al. Designing, implementing, and evaluating mobile health technologies for managing chronic conditions in older adults: a scoping review. JMIR Mhealth Uhealth. 2016;4(2):e29. doi:10.2196/mhealth.5127
29. Lim HM, Dunn AG, Muhammad Firdaus Ooi S, et al. mHealth adoption among primary care physicians in Malaysia and its associated factors: a cross-sectional study. Fam Pract. 2020. doi:10.1093/fampra/cmaa103
30. Bally ELS, Cesuroglu T. Toward integration of mHealth in primary care in the Netherlands: a qualitative analysis of stakeholder perspectives. Front Public Health. 2020;7:407. doi:10.3389/fpubh.2019.00407
31. Boers SN, Jongsma KR, Lucivero F, et al. SERIES: eHealth in primary care. Part 2: exploring the ethical implications of its application in primary care practice. Eur J Gen Pract. 2020;26(1):26–32. doi:10.1080/13814788.2019.1678958
32. Shaw T, McGregor D, Brunner M, et al. What is eHealth (6)? Development of a conceptual model for eHealth: qualitative study with key informants. J Med Internet Res. 2017;19(10):e324. doi:10.2196/jmir.8106
33. Apolinário-Hagen J, Menzel M, Hennemann S, et al. Acceptance of mobile health apps for disease management among people with multiple sclerosis: web-based survey study. JMIR Form Res. 2018;2(2):e11977. doi:10.2196/11977
34. Dou K, Yu P, Deng N, et al. Patients’ acceptance of smartphone health technology for chronic disease management: a theoretical model and empirical test. JMIR Mhealth Uhealth. 2017;5:e177. doi:10.2196/mhealth.7886
35. Petersen F, Jacobs M, Pather S. Barriers for user acceptance of mobile health applications for diabetic patients: applying the UTAUT model.
36. Salgado T, Tavares J, Oliveira T. Drivers of mobile health acceptance and use from the patient perspective: survey study and quantitative model development. JMIR Mhealth Uhealth. 2020;8:e17588. doi:10.2196/17588
37. Odendaal WA, Anstey Watkins J, Leon N, et al. Health workers’ perceptions and experiences of using mHealth technologies to deliver primary healthcare services: a qualitative evidence synthesis. Cochrane Database Syst Rev. 2020;3:Cd011942.
38. Shaw RJ, Bonnet JP, Modarai F, et al. Mobile health technology for personalized primary care medicine. Am J Med. 2015;128(6):555–557. doi:10.1016/j.amjmed.2015.01.005
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
