Back to Journals » Therapeutics and Clinical Risk Management » Volume 19
Central Oxygen Venous Saturation and Mortality in Patients Undergoing Coronary Artery Bypass Grafting
Authors Rodríguez-Scarpetta MA , Sepúlveda-Tobón AM , Daza-Arana JE , Lozada-Ramos H, Álzate-Sánchez RA
Received 6 February 2023
Accepted for publication 23 April 2023
Published 3 June 2023 Volume 2023:19 Pages 447—454
DOI https://doi.org/10.2147/TCRM.S407454
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Garry Walsh
María A Rodríguez-Scarpetta,1,2 Andrés M Sepúlveda-Tobón,3 Jorge E Daza-Arana,1,2 Heiler Lozada-Ramos,2,4,5 Rodrigo A Álzate-Sánchez3
1Physiotherapy Program, Universidad Santiago de Cali, Santiago de Cali, Colombia; 2Research Group on Health and Movement, Universidad Santiago de Cali, Santiago de Cali, Colombia; 3Master in Epidemiology, Universidad Libre, Santiago de Cali, Colombia; 4Medicine Program, Universidad Santiago de Cali, Palmira, Colombia; 5Doctoral Program in Infectious Diseases, Universidad de Santander, Bucaramanga, Colombia
Correspondence: María A Rodríguez-Scarpetta, Physiotherapy Program, Universidad Santiago de Cali, Calle 5 # 62-00, Santiago de Cali, Colombia, Tel +57 301 4158934, Email [email protected]
Purpose: Central venous oxygen saturation (ScvO2) has been reported as a prognostic marker of in-hospital mortality when it is below 60% in certain situations. Nevertheless, it has not been widely reported in patients undergoing coronary artery bypass graft (CABG). The study determined the association between ScvO2 and in-hospital mortality in patients undergoing CABG in a high-complexity health institution in Santiago de Cali, Colombia.
Patients and Methods: A retrospective cohort study was conducted with patients undergoing isolated CABG. The subject sample included 515 subjects aged 18 years or older. Exposure was defined as ScvO2 < 60% upon admission to the intensive care unit (ICU) following surgery. The major outcome was mortality rates after 30 days. Furthermore, exposure variables were measured at preoperative, intra-operative, and postoperative time points.
Results: A total of 103 exposed and 412 unexposed subjects were included. The final model revealed a higher mortality risk in individuals with ScvO2 < 60% upon ICU admission compared with those with higher saturation levels (relative risk 4.2, 95% confidence interval: 2.4– 7.2; p = 0.001). Values were adjusted using variables such as age (> 75 years), low socioeconomic stratum, chronic kidney failure before surgery, unstable angina before surgery, ischemia time (> 60 min), and intra-operative inotrope use. The primary cause of death was cardiogenic shock (54.7%), followed by sepsis (25.0%) and postoperative bleeding (17.2%).
Conclusion: The study identified an association between ScvO2 < 60% and in-hospital mortality in patients undergoing CABG.
Keywords: coronary artery bypass, postoperative complications, mortality, critical care, risk factor
Introduction
Coronary artery bypass graft (CABG) is the most effective revascularization approach for stenotic coronary arteries.1 However, evidence has shown that in-hospital mortality after surgery between 2% and 3% is mainly due to shock.2–4 This physiological condition is characterized by significant tissue hypoperfusion because of decreased oxygen supply (DO2), which results in cell dysfunction and death by different mechanisms and biochemical processes.5,6
Similarly, scales have been designed to predict mortality in the short and long terms in patients with ST-segment elevation myocardial infarction with cardiogenic shock undergoing percutaneous coronary intervention, such as the SINTAX score II and the IMS score;7 lactate and central venous oxygen saturation (ScvO2) measurements could detect patients at high risk of mortality and morbidity after CABG. Tissue hypoperfusion should be monitored in patients undergoing cardiovascular surgery, where ScvO2 is involved as a DO2 indicator. ScvO2 monitoring reflects the balance between DO2 and oxygen consumption. This is a systematic way of monitoring the perfusion and hemodynamics of patients, which are associated with possible postoperative outcomes, for predicting morbidity and mortality.8,9
In a 2011 cohort of 2755 patients undergoing coronary bypass grafting, Holm et al used ScvO2 as a prognostic short- and a long-term marker. They reported that patients with ScvO2 <60% indicated higher mortality rates after 30 d and lower survival rates 5 years after surgery.10 Following this, Svenmarker et al in 2018 characterized a cohort of 6945 patients undergoing cardiovascular surgery. They monitored them for 10 years and revealed that ScvO2 >75% decreases the risk of acute kidney injury (AKI) after surgery and increases short-term survival rates.11 In contrast, Miranda et al in a prospective observational study involving 273 patients undergoing cardiac surgery in 2019 discovered that patients with an intraoperative ScvO2 of 70% had a greater mortality risk.12 Recently, a case–control study was conducted in the city of Cali, Colombia, to identify factors associated with intrahospital mortality following CABG and revealed a significant association between postoperative variables, such as cardiogenic shock, use of vasopressors, tracheal reintubation, surgical site infection, mediastinitis and AKI with dialysis, and ScvO2 <60% upon admission into the intensive care unit (ICU).13
These studies concur that a factor, such as ScvO2, is a good predictor of mortality in individuals undergoing coronary bypass surgery. However, as we conducted in this study, only one of these investigations achieved ScvO2 <60% as a cut-off point.
There are insufficient studies assessing the relationship between ScvO2 and mortality rates in patients undergoing coronary bypass grafting, especially in Latin America, which is the hypothesis of this study. Considering that this surgery is still a better option than percutaneous coronary intervention in patients with multivessel disease, our region should examine this association. Additionally, ScvO2 is a readily available marker, and it can be out quickly at the end of cardiac surgery or upon patient admission to the ICU.
Thus, our study analyzed the in-hospital mortality associated with ScvO2 <60% in patients undergoing CABG to describe the sociodemographic and clinical characteristics and establish a connection to postoperative complications.11
Materials and Methods
Study Design
This retrospective observational cohort study was conducted in a high-complexity health institution in Santiago de Cali, Colombia. Subjects older than 18 who had undergone isolated CABG from January 1, 2006, to December 31, 2015, were included. Subjects with missing medical records, those who were in a coma, and those with prior cardiac surgery were also excluded.
Exposure consisted in subjects admitted to the ICU following coronary bypass grafting with ScvO2 <60% based on blood samples collected from their central venous catheter.
Sample size estimates yielded 103 exposed patients and 412 unexposed patients, with a 1:4 ratio, 95% confidence level (α = 0.05), and 80% statistical power (β = 0.2). This estimation was based on a study by Holm et al,10 who indicated that patients with ScvO2 <60% have higher mortality rates after 30 d compared with those with values greater than 60% (5.4% vs 1.0%; p = 0.0001).
Data were obtained from medical records, clinical laboratory results, diagnostic imaging reports, and perfusion registries. Each individual was identified with an ID code to maintain confidentiality; data were consolidated in a master database that included the variables of the data collection instrument. Concordance assessment and statistical validation of the database were then performed, and data were entered twice, allowing the final data to be organized.
This study was conducted following international recommendations for clinical research included in the Declaration of Helsinki.14 Additionally, resolution 8430 issued by Ministerio de Salud de Colombia (Ministry of Health of Colombia) in 1993 classified this study as risk-free research15 since data were collected from secondary sources, such as medical records. The Research and Ethics Committee approved this project of the study’s institutions.
Data Collection
Sociodemographic and clinical variables were measured at preoperative, intra-operative, and postoperative time points.
The primary outcome variable or event was in-hospital mortality ≤30 days after surgical intervention. Other outcome variables included cardiorespiratory complications, such as pulmonary edema, acute myocardial infarction, acute respiratory distress syndrome, hemothorax, pneumothorax, pleural effusion requiring drainage, tracheal reintubation, tracheostomy, postoperative bleeding, ventilator-associated pneumonia, surgical reintervention, and atelectasis; neurological complications, such as ischemic cerebrovascular accident and delirium; infectious complications such as sepsis, mediastinitis, and surgical site infection; kidney complications, such as kidney failure with or without dialysis; and hematological complications, such as coagulopathy.
Data Analysis
A descriptive analysis of the variables of the general population and the exposed and unexposed subjects was followed. First, this description was performed for categorical data by distributing relative and absolute frequency values. Next, a numerical analysis of central tendency and dispersion measures was conducted for quantitative data, followed by the corresponding categorization. Finally, statistical differences were determined using the chi-square test for proportions and Student’s t-test for numerical data, with their respective 95% confidence intervals (95% CI).
General and group-based survival rates were determined; based on the data obtained, a Kaplan–Meier curve was created, and the Log rank test was estimated. Additionally, a prediction model was built based on Poisson’s multiple regression analysis to determine the association between ScvO2 and in-hospital mortality, adjusting for possible confounding variables. Finally, the strength of association was measured based on the raw and adjusted relative risk (RR), with a 0.05 significance level and 95% confidence level.
Confusion, effect modification, or interaction tests were conducted using the adjusted regression model variables. The model was validated with Pearson’s chi-square goodness-of-fit test and the likelihood ratio test. STATA 16.0 statistical software was used to analyze the data.
Results
The retrospective cohort included 515 patients, of which 103 had ScvO2 <60%; the mean age was 68.3 (SD ± 11), and 72.8% (n = 75) patients were male. The following were the main and statistically significant preoperative clinical characteristics of exposed subjects: history of sepsis, chronic kidney failure (CKF), creatinine level <2.3 mg/dL, peripheral vascular disease, prior use of intra-aortic balloon pump (IABP), angina, left coronary trunk injury, and hemoglobin level <12 g/dL (Supplementary Table 1). Subsequently, it was discovered that some transurgical factors, such as ischemic time over 60 min, cardiogenic shock occurrence, and need for vasopressor agents, were mainly observed in exposed subjects (Supplementary Table 2).
It was noticed that exposed individuals required higher levels of red blood cell transfusion, hemodynamic support with vasopressors, and inotrope and IABP use in the postoperative stage. Additionally, they were prone to present heart arrhythmia such as atrial fibrillation (Supplementary Table 3). ScvO2 <60% was associated with a higher risk of invasive mechanical ventilation for more than 2 days, postoperative bleeding, surgical reintervention, sepsis, mediastinitis, AKI with dialysis, and coagulopathy (Table 1).
 |
Table 1 Postsurgical Complications and In-Hospital Mortality in Patients with Central Venous Oxygen Saturation (ScvO2) <60% |
In-hospital mortality was observed in 39.8% of exposed subjects as opposed to 5.72% of unexposed subjects. The average number of days following surgery in which subjects with ScvO2 <60% died was 6.8 d (SD ± 9.5). The most common cause was cardiogenic shock (54.7%), followed by sepsis (25.0%) and bleeding (17.2%) (Supplementary Table 4).
Several predictive models were created using Poisson multiple regression analysis and the theoretical framework, as well as statistical criteria for identifying variables with statistical significance and theoretical importance that allowed the most parsimonious model to be constructed. Ultimately, the final model indicated a higher mortality risk in subjects undergoing CABG and reporting ScvO2 <60% upon ICU admission, as opposed to those with higher saturation levels (RR 4.2, 95% CI: 2.4–7.2; p = 0.001), adjusted by variables, such as age >75, low socioeconomic stratum (SES), CKF before surgery, angina before surgery, ischemia time more than 60 min, and intra-operative inotrope use.
As a result, six variables were obtained from the final regression model: age >75, low SES, CKF before surgery, angina before surgery, ischemia time more than 60 min, and intra-operative inotrope use. Based on this analysis, it is possible to conclude that these variables are responsible for 26% of the event onset (Table 2). The estimated survival function and its corresponding Kaplan–Meier curve revealed a significant difference between the survival rates of the higher mortality groups, consisting of subjects with ScvO2 <60% (log rank test, chi-square test = 4.26; p = 0.0390). Moreover, 48 hr after ICU admission, the number of deaths in the exposed group was three-fold higher than that in the unexposed group (30 vs 9), with 26.8% and 60.9% survival rates, respectively (Figure 1). The goodness-of-fit test for model validation showed that the observed data have a Poisson distribution (Pearson’s chi-square: 366.15, p > 0.05).
 |
Table 2 Relative Mortality Risk in Subjects with ScvO2 <60%, 95% CI, Based on Poisson Regression |
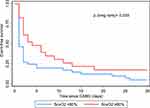 |
Figure 1 Kaplan–Meier’s survival function according to ScvO2. |
Discussion
Once the final model was built, the results show a positive association between ScvO2 and mortality, as well as with the preoperative variables age >75, low SES, CKF, and angina; and intra-operative variables ischemia time more than 60 min and inotrope use. In this context, it is worth noting that research on mortality associated with ScvO2 mostly focused on septic shock and was precariously conducted for patients undergoing cardiovascular surgery and isolated CABG. Although the IABP did not remain in the final model, it has been determined that in individuals managed in the ICU with acute coronary syndrome who require support with IABP, factors such as chronic renal failure and elevated lactate and glycemia levels can predict higher mortality.16
ScvO2 and Mortality
In 2010, Pope et al conducted a case–control study. They measured ScvO2 in 619 patients with sepsis and found a mean baseline ScvO2 of 73% and a baseline mortality rate due to hypoxia of 25% of the sample. Subjects who still presented with this condition after 6 hr indicated a 40% mortality rate.17 Similar findings were observed in this study, where 39.8% mortality was reported for exposed subjects. Nevertheless, our population consisted of patients undergoing isolated CABG.
Miranda et al reported a prospective observational study in 2020 that evaluated intra-operative ScvO2 values in 273 patients undergoing heart surgery, finding that ScvO2 70% is an independent risk factor for in-hospital mortality (OR = 2.94, 95% CI: 1.10–7.89, p = 0.032).12 Alternatively, a retrospective cohort study with subjects undergoing isolated CABG reported a higher number of patients with ScvO2 <60% dying during the next 30 days, with a statistically significant association (RR 6.8, 95% CI: 3.0–15.6, p = 0.0001).10 Likewise, Lozada et al recently conducted a case–control study and showed the factors associated with intrahospital mortality following CABG; among other variables, a significant connection to SvO2 <60% upon ICU admission was reported.13 In this sense, it is important to understand that ScvO2 is determined by changes in oxygen supply and consumption, which is associated with the physiopathological features of shock states. As a result, its levels should be monitored in high-risk patients following surgery to reverse the triggering causes of tissue hypoxia and prevent morbimortality.18
Other Related Risk Factors
Age
This is certainly a factor with the closest association with mortality in CABG patients, also showing the closest connection to coronary disease onset and mortality.19 Gabe et al conducted a prospective study on senile patients undergoing coronary surgery (>80 years), who indicated a higher risk of hospital mortality (OR 1.26, 95% CI: 1.06–1.49; p = 0.009).20
SES
Some results of this study include an association between low SES and mortality in subjects with ScvO2 <60%, which corroborated with what was reported by Hanna et al, who evidenced a negative impact of SES as measured by the area deprivation index in short-term mortality in patients undergoing CABG.21 Moreover, Nielsen et al studied the relationship between social factors and mortality risk after CABG and described a strong connection with the low-income population.22 Alternatively, a recent study evaluated the family income and educational level of 5243 subjects undergoing isolated CABG. No significant differences in mortality after 30 days were observed for those who reported lower income levels; however, a connection to mortality after 5 years and postoperative complications, such as mediastinitis and bleeding, was found.23 These results indicate the influence of social determinants of health on the clinical outcomes of patients undergoing coronary bypass grafting.
CKG
This has been linked to short- and long-term mortality, considering its direct association with cardiovascular diseases. In their study, Alramadan et al found that the adjusted mortality risk after 30 days in CABG patients increased as their mild kidney disease worsened (OR 1.6; 95% CI: 1.4–1.8, p = 0.001).24 These findings are consistent with what was published by Günday et al, who described how subjects with mild CKF before surgery have a significantly lower mean coronary flow reserve after CABG surgery as opposed to normal kidney function before surgery (2.09 ± 0.08 vs 2.37 ± 0.06, p < 0.05), which may be explained by the microvascular bed deterioration observed in this population.25 However, Wang et al concluded that mild CKF before surgery resulted in a long-term decrease in survival in CABG patients with no extracorporeal circulation and did not show strong evidence of fatal hospital outcomes.26
In this study, angina before surgery was a 2-fold risk factor for in-hospital mortality, which conformed to the cohort study by STS, whose results included a similar relationship between both variables (RR 1.12, 95% CI: 1.07–1.17, p < 0.05) adjusted for age.27
Ischemia Time (Aortic Cross-Clamp Time)
Our study revealed a two-fold greater mortality risk in subjects with ischemia time more than 60 min as opposed to those with lower ischemia time (RR 1.9, 95% CI: 1.04−3.44, p = 0.032), similar to that described by Ruggieri et al in their multicenter prospective study conducted with patients undergoing CABG.1 In this research, the graft or ischemia time was more than 60 min in 38.3% and more than 75 min in 20.9%, showing that the adjusted mortality risk after 30 days was higher for PC >75 min (p = 0.002, OR 3.479; 95% CI: 1.609–7.520); likewise, a higher connection to early mortality was observed. Similarly, patients with left ventricular ejection fraction (LVEF) <40% showed a higher correlation with mortality,28 as reported by Doenst et al, who reported that patients with low LVEF had higher mortality rates than patients with standard values.29
Perioperative myocardial damage is considered a fundamental determinant in individuals undergoing cardiac surgery. Prolonged aortic cross-clamp time (XCT) is associated with myocardial enzyme release in response to ischemia, leading to several adverse events. This prolonged XCT is usually associated with prolonged cardiopulmonary bypass (CPB), which worsens the prognosis. Additionally, a prolonged XCT could lead to the need to use inotropes longer, increased in-hospital/30 days mortality, need for IABP support, prolonged stay in intensive care, presence of arrhythmias such as atrial fibrillation, and use of extracorporeal membrane oxygenation.26
Inotrope Use
The study’s final model showed that intra-operative inotrope use is linked to in-hospital mortality in CABG patients, which is congruent with the findings of Yamazki et al, who looked at vasoactive-inotropic scores (VIS), which define how much circulatory support is needed. They developed a multivariate logistic regression analysis to determine the association between VIS and unfavorable clinical outcomes, evidencing a correlation between high VIS at the end of surgery and higher morbidity and mortality rates (adjusted odds ratio [OR] 4.87, 95% CI: 1.51–4.07, p = 0.007).30
Several studies suggest that inotropic drugs worsen ischemia, which is why they should be used cautiously.
Finally, we can state that the ScvO2 is a simple and easy-to-use instrument assessed upon ICU admission and allows us to detect the mortality risk of persons undergoing CABG and associated complications, making it a useful prognostic factor in predicting survival in this group of patients. Subsequently, early therapeutic actions could be carried out to impact the outcomes favorably.
Study Limitations and Strengths
A strength of this study is that the researchers collected and processed the database, reducing the likelihood of information bias, and the current international classifications were followed, as well as those suggested by other publications on CABG patients. Finally, this study is one of the few to evaluate the association between ScvO2 and mortality in subjects undergoing isolated CABG. One of this study’s limitations is the measurement of the lactate variable, which is useful as well as venous oxygen saturation for the detection of patients with a high risk of mortality, which was not used in this study. Based on the results derived in this study, further multicenter research should be conducted in Colombia and Latin America to boost the study goals with a sample size big enough to involve more variables and further evaluate ScvO2 as a predictor of clinical outcomes in subjects undergoing CABG.
Conclusion
Summarily, it could be said that patients undergoing CABG indicate a positive correlation between ScvO2 <60% and in-hospital mortality, which was adjusted for age <75, SES, KCF, and angina as preoperative variables; and ischemia time <60 min, and inotrope use as intra-operative variables. The primary mortality causes are cardiogenic shock, sepsis, and postsurgical bleeding.
Acknowledgments
To the research and education department of Clínica de Occidente, which allowed for the performance of the study. This research has been funded by Dirección General de Investigaciones of Universidad Santiago de Cali under call No. 02-2023.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sonny A, Joseph L. Improving CABG mortality further: striving toward perfection. J Am Coll Cardiol. 2021;78(2):123–125. doi:10.1016/j.jacc.2021.05.009
2. Keogh B, Robin K. The society of cardiothoracic surgeons of Great Britain and Ireland. Fifth national adult cardiac surgical database report; 2003.
3. Rodríguez-Hernández A, García-Torres M, Reta EB, Baranda-Tovar FM. Analysis of mortality and hospital stay in cardiac surgery in Mexico 2015: data from the national cardiology institute. Arch Cardiol Mex. 2018;88(5):397–402. doi:10.1016/j.acmx.2017.11.004
4. Acuña I, Hennessey JM, Albornoz JP, González LJ. Complicaciones quirúrgicas de la circulación extracorpórea. Rev Repert Med y Cirugía. 2015;24(4):261–266. doi:10.31260/RepertMedCir.v24.n4.2015.599
5. De Sousa AG, Fichino MZS, Da Silva GS, Bastos FCC, Piotto RF. Epidemiologia da cirurgia de revascularização miocárdica do hospital beneficência Portuguesa de São paulo. Braz J Cardiovasc Surg. 2015;30(1):33–39.
6. Svenmarker S, Häggmark S, Östman M, Holmgren A, Näslund U. Central venous oxygen saturation during cardiopulmonary bypass predicts 3-year survival. Interact Cardiovasc Thorac Surg. 2013;16(1):21–26. doi:10.1093/icvts/ivs363
7. Mert İH, Faysal S, Ahmet ÇY, Murat S, Tufan Ç. Prognostic value of intermountain risk score for short- and long-term mortality in patients with cardiogenic shock. Coron Artery Dis. 2023;34(2):154–159. PMID: 36720024. doi:10.1097/MCA.0000000000001219
8. Peters SG, Afessa B, Decker PA, Schroeder DR, Offord KP, Scott JP. Increased risk associated with pulmonary artery catheterization in the medical intensive care unit. J Crit Care. 2003;18(3):166–171. doi:10.1016/j.jcrc.2003.08.006
9. Gillies M, Bellomo R, Doolan L, Buxton B. Bench-to-bedside review: inotropic drug therapy after adult cardiac surgery -- a systematic literature review. Crit Care. 2005;9(3):266–279. doi:10.1186/cc3024
10. Holm J, Håkanson E, Vánky F, Svedjeholm R. Mixed venous oxygen saturation predicts short- and long-term outcome after coronary artery bypass grafting surgery: a retrospective cohort analysis. Br J Anaesth. 2011;107(3):344–350. doi:10.1093/bja/aer166
11. Svenmarker S, Hannuksela M, Haney M. A retrospective analysis of the mixed venous oxygen saturation as the target for systemic blood flow control during cardiopulmonary bypass. Perfus. 2018;33(6):453–462. doi:10.1177/0267659118766437
12. Miranda C, de A, Meletti JFA, Lima LHN, Marchi E. Perioperative central venous oxygen saturation and its correlation with mortality during cardiac surgery: an observational prospective study. Br J Anaesth. 2020;70(5):484–490.
13. Lozada-Ramos H, Daza-Arana JE, Zárate Gonzalez M, Medina Gallo LF, Lanas F. Risk factors for in-hospital mortality after coronary artery bypass grafting in Colombia. J Cardiovasc Surg. 2022;63(1):78–84. doi:10.23736/S0021-9509.21.11829-4
14. Asociación Médica Mundial [World Medical Association]. Declaración de Helsinki. Principios éticos para las investigaciones médicas en seres humanos [Helsinki Declaration. Ethical principles for medical research in humans]; 1964. Available from: http://bvs.sld.cu/revistas/recursos.
15. Ministerio de Salud [Ministry of Health]. Resolución 8430 de 1993 [Resolution 8430 of 1993]. República de Colombia; 1993. Available from: https://www.invima.gov.co/images/pd.
16. Hayıroğlu Mİ, Çanga Y, Yıldırımtürk Ö, et al. Clinical characteristics and outcomes of acute coronary syndrome patients with intra-aortic balloon pump inserted in intensive cardiac care unit of a tertiary clinic. Turk Kardiyol Dern Ars. 2018;46(1):10–17. PMID: 29339686. doi:10.5543/tkda.2017.11126
17. Pope JV, Jones AE, Gaieski DF, Arnold RC, Trzeciak S, Shapiro NI. Multicenter study of central venous oxygen saturation (ScvO(2)) as a predictor of mortality in patients with sepsis. Ann Emerg Med. 2010;55(1):40–46. doi:10.1016/j.annemergmed.2009.08.014
18. Revisión ADE, Carrillo-Esper R, José Núñez-Bacarreza J, Raúl Carrillo-Córdova J. medigraphic.com Anestesiología Anestesiología Saturación venosa central. Concept Act Art Medigraph. 2007;30(3):165–171.
19. Madhavan MV, Gersh BJ, Alexander KP, Granger CB, Stone GW. Coronary artery disease in patients ≥80 years of age. J Am Coll Cardiol. 2018;71(18):2015–2040. doi:10.1016/j.jacc.2017.12.068
20. Gabe ED, Favaloro RR, Favaloro MR. Cirugía coronaria en pacientes ancianos. Resultados hospitalarios y a largo plazo. Rev Esp Cardiol. 2001;54(6):709–714. doi:10.1016/S0300-8932(01)76386-5
21. Hannan EL, Wu Y, Cozzens K, et al. The association of socio-economic factors with outcomes for coronary artery bypass surgery. Ann Thorac Surg. 2022;114(4):1318–1325. doi:10.1016/j.athoracsur.2021.10.006
22. Nielsen S, Giang KW, Wallinder A, et al. Social factors, sex, and mortality risk after coronary artery bypass grafting: a population-based cohort study. J Am Heart Assoc. 2019;8(6):e011490. doi:10.1161/JAHA.118.011490
23. Coyan GN, Okoye A, Shah A, et al. Effect of neighborhood socioeconomic factors on readmissions and mortality after coronary artery bypass grafting. Ann Thorac Surg. 2021;111(2):561–567. doi:10.1016/j.athoracsur.2020.05.102
24. Alramadan MJ, Karim MN, Hossain MN, et al. Renal disease is associated with poor outcomes following isolated coronary artery bypass grafting. Glob Heart. 2019;14(4):347–353. doi:10.1016/j.gheart.2019.08.002
25. Günday M, Ciftci Ö, Calişkan M, et al. Does mild renal failure affect coronary flow reserve after coronary artery bypass graft surgery? Heart Surg Forum. 2014;17(1):18. doi:10.1532/HSF98.2013272
26. Wang W, Wang Y, Xu R, et al. Outcomes following coronary artery bypass graft surgery in patients with mild preoperative renal insufficiency. Braz J Cardiovasc Surg. 2018;33(2):155–161. PMID: 29898145; PMCID: PMC5985842. doi:10.21470/1678-9741-2017-0148
27. Shahian DM, O’Brien SM, Filardo G, et al. The society of thoracic surgeons 2008 cardiac surgery risk models: part 1--coronary artery bypass grafting surgery. Ann Thorac Surg. 2009;88(1 Suppl):1.
28. Ruggieri VG, Bounader K, Verhoye JP, et al. Prognostic impact of prolonged cross-clamp time in coronary artery bypass grafting. Heart Lung Circ. 2018;27(12):1476–1482. doi:10.1016/j.hlc.2017.09.006
29. Doenst T, Borger MA, Weisel RD, Yau TM, Maganti M, Rao V. Relation between aortic cross-clamp time and mortality — not as straightforward as expected. Eur J Cardio Thoracic Surg. 2008;33(4):660–665. doi:10.1016/j.ejcts.2008.01.001
30. Yamazaki Y, Oba K, Matsui Y, Morimoto Y. Vasoactive-inotropic score as a predictor of morbidity and mortality in adults after cardiac surgery with cardiopulmonary bypass. J Anesth. 2018;32(2):167–173. doi:10.1007/s00540-018-2447-2
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
