Back to Journals » Nature and Science of Sleep » Volume 15
Causal Relations Between Obstructive Sleep Apnea and Stroke: A Mendelian Randomization Study
Authors Li P, Dong Z, Chen W , Yang G
Received 1 December 2022
Accepted for publication 30 March 2023
Published 19 April 2023 Volume 2023:15 Pages 257—266
DOI https://doi.org/10.2147/NSS.S398544
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Ahmed BaHammam
Po Li,1 Zhiyong Dong,2 Wenhui Chen,2 Gang Yang1
1Department of General Surgery, Second People’s Hospital of Zhangye City, Zhangye, 734000, People’s Republic of China; 2Department of Gastrointestinal Surgery, The First Affiliated Hospital of Jinan University, Guangzhou, People’s Republic of China
Correspondence: Gang Yang, Department of General Surgery, Second People’s Hospital of Zhangye City, No. 270 Linsong West Street, Binhe New District, Ganzhou District, Zhangye, Gansu, People’s Republic of China, Tel +86 1899361927, Fax +0936 8215086, Email [email protected] Wenhui Chen, Department of Gastrointestinal Surgery, The First Affiliated Hospital of Jinan University, No. 613 Huangpu Avenue West, Guangzhou, People’s Republic of China, Tel +86 13129349492, Fax +86 20 38688608, Email [email protected]
Background: Previous studies of obstructive sleep apnea (OSA) in relation to stroke have been noted. However, the exact causality remains to be clearly defined. We aimed to adopt a two-sample Mendelian randomization study to investigate the causal effects of OSA on stroke and its subtypes.
Methods: A two-sample Mendelian randomization (MR) analysis was conducted to evaluate the causal effect of OSA on stroke and its subtypes, including, based on publicly genome-wide association studies (GWAS) databases. The inverse variance weighted (IVW) method was used as the main analysis. MR-Egger regression, weighted mode, weighted median, and MR pleiotropy residual sum and outlier (MR-PRESSO) were performed methods and were adopted as supplementary analysis to ensure the robustness of the results.
Results: Genetically predicted OSA was not related to the risk of stroke (odds ratio (OR), 0.99, 95% CI, 0.81– 1.21, p = 0.909), and its subtypes, ischemic stroke (IS) (OR, 1.01, 95% CI, 0.82– 1.23, p = 0.927), large vessel stroke (LVS) (OR, 1.05, 95% CI, 0.73– 1.51, p = 0.795), cardioembolic stroke (CES) (OR, 1.03, 95% CI, 0.74– 1.43, p = 0.855), small vessel stroke (SVS) (OR, 1.13, 95% CI, 0.88– 1.46, p = 0.329), lacunar stroke (LS) (OR, 1.07, 95% CI, 0.74– 1.56, p = 0.721) as well as intracerebral hemorrhage (ICH) (OR, 0.37, 95% CI = 0.09, 1.48, p = 0.160) (Wald ratio method). Other supplementary MR methods also confirmed similar results.
Conclusion: There may be no direct causal relationship between OSA and stroke or its subtypes.
Keywords: obstructive sleep apnea, stroke, Mendelian randomization, causal association
Introduction
Obstructive sleep apnea (OSA) has become a common and chronic sleep-related disorder, which is characterized by repeated episodes of partial or complete upper airway collapse during sleep, resulting in intermittent hypoxemia, and sleep fragmentation.1 The prevalence of OSA ranged from 9% to 38% in the overall population, with 13%–33% in men and 6–19% in women.2 Patients with obesity as high as 60% to 94% of patients fulfill the diagnostic criteria for OSA,3 and its prevalence is likely to increase as advancing age and the increasing obesity prevalence. Untreated OSA may result in type 2 diabetes mellitus, high blood pressure, coronary heart disease, stroke, and even sudden death during sleep.4–6
Stroke is also a common neurological disease and is the major cause of global death and adult disability.7 Ischemic stroke is the main type of stroke, accounting for approximately 4/5, while the other 1/5 are hemorrhagic stroke.8 There are many well-known independent risk factors of stroke, including hypertension, diabetes mellitus, obesity, hyperlipidemia, and unhealthy lifestyle (smoking, sedentary lifestyle),9 whereas these traditional risk factors do not explain fully stroke risk. With the increasing global burden of stroke, it is essential to identify the other potential risks for stroke, which can help to better prevent stroke. Multiple meta-analyses from prospective observational studies showed that OSA is an independent risk factor for incident stroke.10–12 However, the results from retrospective studies remain variable. A large-scale study with 10,149 participants at a follow-up of 68 months demonstrated that the occurrence of stroke in OSA patients was not significantly related to the severity of OSA assessed by AHI but with confounding factors (age, sex, and hypertension).13 In addition, OSA also was considered as a risk factor for stroke recurrence,14 while this causal relationship may be explained in part by overlapping risk factors, such as obesity, male, increasing age and prevalent cardiovascular diseases. Furthermore, there may be a bidirectional relationship between OSA and stroke.15 Although numerous evidence from observational studies suggests the association between obesity and risk of stroke, findings from conventional observational studies cannot overcome the problems of reverse causation and confounding factors. Thus, the real causal association between OSA and stroke remains to be clearly defined due to reporting bias, potential confounders or reverse causation from observational studies.
Mendelian randomization (MR) uses genetic variants as instrumental variables (IVs) to explore the potential causal relationship between exposure and outcome.16 The MR design leverages allelic randomization at conception and subsequent irreversible genotype, which is similar to a randomized clinical trial. Accordingly, the design can effectively avoid potential confounders or reverse causation. Currently, none of the previous studies were conducted to investigate whether OSA is causally associated with stroke or its subtypes using the MR design. Therefore, we aimed to adopt a two-sample MR study to evaluate the causal effect of OSA on stroke and its subtypes, including IS, large vessel stroke (LVS), small vessel stroke (SVS), cardioembolic stroke (CES), lacunar stroke (LS) and intracerebral hemorrhage (ICH), based on available genome-wide association study (GWAS) summary databases.
Methods
Study Design
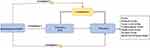
This is a two-sample MR study combined with the recommendations from Strengthening the Reporting of Mendelian Randomization Studies (STROBE-MR) guidelines. The overview and assumptions of the MR study design are shown in Figure 1. We used two-sample MR study designed to evaluate whether OSA was causally associated with stroke and its subtypes. In this design, three assumptions should be included: (1) the instrumental variables that refer to genetic variation have a strong relationship with exposure (OSA); (2) the used IVs are not linked with potential confounders; (3) the genetic variants are related to the outcome only through selected exposure (OSA), not via alternative pathways. This MR study was performed based on published studies and public genome-wide association studies (GWAS) databases. Additional ethics approval or participate informed consent was exempt due to databases from published studies.
Data Sources
Summary-level genetic data for OSA were obtained from the FINNGen consortium in a large-scale GWAS study. These GWAS data included 16,761 OSA cases and 201,194 normal controls of European ancestry (217, 955 subjects in total).17 OSA was defined based on subjective symptoms, clinical examination, and sleep monitors (AHI) ≥5/h or respiratory event index (RED) ≥5/h. These OSA GWAS data included a total of 16,380,465 SNPs.
The GWAS summary data for stroke and its subtypes were obtained from the MEGASTROKE consortium involving a total of 40,585 stroke cases and 406,111 controls of European ancestry,18 which were available in the IEU OpenGWAS database (https://gwas.mrcieu.ac.uk/). Stroke was defined as rapidly developing signs of focal (or global) disturbance of neurological function, lasting ≥24h or leading to death with no obvious cause other than that of vascular origin. These GWAS data included 34,217 cases of ischemic stroke, which was classified as three subtypes according to the Trial of Org 10172 in Acute Stroke Treatment criteria,19 such as LVS (4373 cases), CES (7193 cases) and SVS (5386 cases). Genetic association data on lacunar stroke (LS) were extracted from another recent meta-analysis including 225,419 samples of European ancestry (6030 LS cases and 248,929 controls),20 which were available in the IEU OpenGWAS database (https://gwas.mrcieu.ac.uk/). LS was defined as small subcortical infarcts due to obstruction of deep perforating arteries of the brain. In addition, GWAS data for ICH were obtained from a GWAS meta-analysis with 1545 cases and 1481 controls of European ancestry,21 which were available at online database (https://cd.hugeamp.org/downloads.html). ICH was defined as new and acute (<24 h) neurological deficits with compatible brain imaging.22 Data sources on GWAS databases included are detailed in Table 1.
 |
Table 1 Details of the GWAS Databases Included in the Mendelian Randomization |
Selection of Instrumental Variables (IVs)
To fulfill three assumptions for MR study design, firstly, OSA-associated single nuclear polymorphisms (SNPs) for genetic instruments were selected based on the genome-wide significance threshold (P < 5 × 10−8). Then, SNPs in high linkage disequilibrium (LD) (R2 > 0.01 and clump window <10,000 kb) were excluded and the SNP with the lowest P value for association with OSA was retained. Furthermore, we also calculated the F statistic to ensure a strong relationship with the exposures, with F ≥ 10 indicating the selected IVs had a strong relationship with OSA. According to the above criteria, five OSA-associated SNPs were extracted from the GWAS datasets. In addition, given the evidence suggesting obesity is an established risk factor for stroke and OSA,1,23 we looked over each SNP in online Phenoscanner (http://www.phenoscanner.medschl.cam.ac.uk/) to identify SNP associated with body mass index (BMI). We found and excluded 1 SNP (rs9937053), which was associated with BMI.
Statistical Analyses
The random-effects inverse-variance weighted (IVW) was performed as a key MR analysis approach to estimate the causal effect of OSA on stroke and its subtypes. The method assumes that all SNPs are valid instruments and evaluate the estimate as the inverse variance weighted mean of the Wald ratio for individual SNPs.24 Furthermore, we further performed three different methods (weighted median, MR-Egger regression, and weighted mode) as sensitivity analyses. The weighted median method provides a consistent causal estimate assuming that more than 50% of the weight comes from valid instrumental variables.25 The MR-Egger regression approach can detect potential directional horizontal pleiotropy and provide a corrective estimate, with the P value <0.05 for the MR-Egger intercept indicating directional pleiotropy.26 The weighted mode method estimates the effect through the mode of the IVW empirical density function.27 Additionally, MR-Pleiotropy Residual Sum and Outlier method (MR-PRESSO) approach was used to identify horizontal pleiotropic outliers and generate new estimates by removing pleiotropic outliers, with a P < 0 0.05 indicating that outlier correction leads to significantly different in estimates.28
Finally, we performed leave-one-out analyses to evaluate the effect of the remaining SNPs on the results after omitting each SNP. Cochrane’s Q value was applied to assess the heterogeneity between SNPs. All statistical analyses were performed by the TwoSampleMR and MRPRESSO packages in R software (version.4.2.0).
Results
Table 2 shows the characteristics of instrumental variables associated with OSA. A total of five OSA-associated SNPs were obtained from GWAS databases, and one SNP (rs9937053) was excluded due to association with BMI. Finally, four SNPs were included as valid IVs to further perform MR analysis. The F statistic of all SNPs was greater than 10, indicating a strong correlation with OSA.
 |
Table 2 Characteristics of Instrumental Variables Associated with Obstructive Sleep Apnea |
The main MR analyses (IVW method) showed that there was no causal relationship observed between OSA and any stroke (OR = 0.99, 95% CI = 0.81–1.21, p = 0.909), IS (OR = 1.01, 95% CI = 0.82–1.23, p = 0.927), LVS (OR = 1.05, 95% CI = 0.73–1.51, p = 0.795), CES (OR = 1.03, 95% CI = 0.74–1.43, p = 0.855), SVS (OR = 1.13, 95% CI = 0.88–1.46, p = 0.329), LS (OR = 1.07, 95% CI = 0.74–1.56, p = 0.721) as well as ICH (OR = 0.37, 95% CI = 0.09, 1.48, p = 0.160) (Wald ratio method). Other supplementary MR methods, including MR-Egger regression, weighted median and weighted mode, also confirmed similar results (Table 3 and Figures 2 and 3).
 |
Table 3 MR Analyses Effect Estimates for Associations Between Obstructive Sleep Apnea and Stroke |
The Cochran Q-test and MR Egger intercept test showed no evidence of heterogeneity or directional pleiotropy was found (all P > 0.05). Besides, MR-PRESSO also showed no outliers were observed (all global p > 0.05), indicating no horizontal pleiotropy. We also performed leave-one-out analyses and failed to find that the IVW estimate was substantially influenced after excluding one single SNP (Figure 4).
Discussion
Currently, there is still controversy about whether OSA has a causal effect on stroke and its subtypes. To clarify this relationship, in this study, we first applied two-sample MR analysis to investigate the potential causal relationship between OSA and stroke or its subtypes. Our findings suggest that there was no evidence supporting causal associations between OSA and stroke or its subtypes (IS, LVS, CES, LS and ICH). The sensitivity analyses also further confirmed the robust results.
In recent decades, a growing number of evidence have reported that OSA was associated with the development of stroke. A meta-analysis from 89 observational studies including 7096 stroke patients demonstrated that the prevalence of OSA with AHI ≥5/h and ≥30/h was 71% and 30%, respectively, in stroke patients, which was in line with the results across acute, subacute, and chronic periods.29 Another meta-analysis with 3 million patients from 58 studies showed OSA prevalence was up to 58.8% in patients with cerebrovascular disease.30 Specifically, OSA increases a 2-fold risk of incident stroke with a follow-up period of 3–10 years.31 A meta-analysis from 10 prospective studies showed similar results.10 However, these findings from the observational studies have an obvious limitation in that they cannot overcome the influence of underlying confounding factors, including gender, age, obesity, hypertension and diabetes. Our MR analysis found no evidence for causal effect between OSA and the risk of stroke or its subtypes. In this study, we used the strict criteria of SNP selection and excluded an SNP associated with BMI (rs9937053) via online Phenoscanner. Besides, MR-Egger and MR-PREESO method also proved that there was no pleiotropy. Hence, the findings were robust. Of note, we were unlikely to completely deny the possibility that OSA might have an effect on stroke through other pathways from certain comorbidities, such as coronary artery disease, hypertension, pulmonary hypertension, type 2 diabetes, and metabolic syndrome.6
Though no significant causal effect of OSA on stroke was observed, OSA still might influence the development of stroke. Some underlying pathophysiologic mechanisms between OSA and stroke have been recognized, in acute and chronic hemodynamic, biochemical, and cellular abnormality levels.15 OSA-related reactive oxygen species (ROS) formation, the release of inflammatory mediators and increased expression of adhesion molecules result in hypercoagulability and endothelial dysfunction, which play key roles in the development of atherosclerosis and stroke.32 OSA can give rise to cardioembolic stroke by increasing the risk of atrial fibrillation.15 OSA can directly influence cerebral hemodynamics, brain damage and autonomic dysfunction, resulting in acute stroke.6,33,34 Considering these possible mechanisms, further research on the large sample size of GWAS to prove a causal association between OSA and stroke should be conducted.
The strength of our study is that it was the first time to evaluate the causal effects of OSA on stroke and all subtypes using two-sample MR analysis based on large-scale GWAS summary statistics. Our study offers new insights into the causality between OSA and stroke. However, the current study has several limitations. To begin with, our study was limited by the analysis population from single European ancestry, which may affect our findings’ generalizability to other ancestries. Secondly, the limited number of valid instrumental variables may influence estimation of causal association. However, the selected IVs had a strong correlation with OSA (F statistic >10), and no heterogeneity or pleiotropy was observed during MR analysis, which indicated that our results were robust. Thirdly, due to lack of classification of OSA severity in current data, we were unable to fully assess the potential differences between different OSA severity classifications and stroke risk. Finally, we cannot entirely rule out all potential pleiotropy which may lead to biased results, although no significant pleiotropy was found by MR-Egger regression. In light of these limitations, further studies with larger MR studies should be undertaken to better confirm the current results.
Conclusion
In conclusion, there may be no direct causal relationship between OSA and stroke or its subtypes.
Data Sharing Statement
All data are publicly available GWAS summary data.
Acknowledgments
The authors thank all investigators for sharing the genome-wide association studies (GWASs) summary statistics.
Disclosure
The authors have no commercial associations that might be a conflict of interest in relation to this article.
References
1. Gottlieb DJ, Punjabi NM. Diagnosis and management of obstructive sleep Apnea: a review. JAMA. 2020;323(14):1389–1400. doi:10.1001/jama.2020.3514
2. Senaratna CV, Perret JL, Lodge CJ, et al. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017;34:70–81.
3. Loo GH, Rajan R, Mohd Tamil A, Ritza Kosai N. Prevalence of obstructive sleep apnea in an Asian bariatric population: an underdiagnosed dilemma. Surg Obes Relat Dis. 2020;16(6):778–783. doi:10.1016/j.soard.2020.02.003
4. Javaheri S, Barbe F, Campos-Rodriguez F, et al. Sleep apnea: types, mechanisms, and clinical cardiovascular consequences. J Am Coll Cardiol. 2017;69(7):841–858. doi:10.1016/j.jacc.2016.11.069
5. Kapur VK, Auckley DH, Chowdhuri S, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep Apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2017;13(3):479–504. doi:10.5664/jcsm.6506
6. Yeghiazarians Y, Jneid H, Tietjens JR, et al. Obstructive sleep apnea and cardiovascular disease: a scientific statement from the American heart association. Circulation. 2021;144(3):e56–e67. doi:10.1161/CIR.0000000000000988
7. Wang H, Naghavi M, Allen C, et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the global burden of disease study 2015. Lancet. 2016;388(10053):1459–1544.
8. Campbell BCV, Khatri P. Stroke. Lancet. 2020;396(10244):129–142. doi:10.1016/S0140-6736(20)31179-X
9. Feigin VL, Roth GA, Naghavi M, et al. Global burden of stroke and risk factors in 188 countries, during 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet Neurol. 2016;15(9):913–924. doi:10.1016/S1474-4422(16)30073-4
10. Li M, Hou WS, Zhang XW, Tang ZY. Obstructive sleep apnea and risk of stroke: a meta-analysis of prospective studies. Int J Cardiol. 2014;172(2):466–469. doi:10.1016/j.ijcard.2013.12.230
11. Loke YK, Brown JW, Kwok CS, Niruban A, Myint PK. Association of obstructive sleep apnea with risk of serious cardiovascular events: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2012;5(5):720–728. doi:10.1161/CIRCOUTCOMES.111.964783
12. Dong JY, Zhang YH, Qin LQ. Obstructive sleep apnea and cardiovascular risk: meta-analysis of prospective cohort studies. Atherosclerosis. 2013;229(2):489–495. doi:10.1016/j.atherosclerosis.2013.04.026
13. Kendzerska T, Gershon AS, Hawker G, Leung RS, Tomlinson G. Obstructive sleep apnea and risk of cardiovascular events and all-cause mortality: a decade-long historical cohort study. PLoS Med. 2014;11(2):e1001599. doi:10.1371/journal.pmed.1001599
14. Brown DL, Shafie-Khorassani F, Kim S, et al. Sleep-Disordered Breathing Is Associated With Recurrent Ischemic Stroke. Stroke. 2019;50(3):571–576. doi:10.1161/STROKEAHA.118.023807
15. Javaheri S, Peker Y, Yaggi HK, Bassetti CLA. Obstructive sleep apnea and stroke: the mechanisms, the randomized trials, and the road ahead. Sleep Med Rev. 2022;61:101568.
16. Lawlor DA, Harbord RM, Sterne JA, Timpson N, Davey Smith G. Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med. 2008;27(8):1133–1163. doi:10.1002/sim.3034
17. Strausz S, Ruotsalainen S, Ollila HM, et al. Genetic analysis of obstructive sleep apnoea discovers a strong association with cardiometabolic health. Eur Respir J. 2021;57(5):2003091. doi:10.1183/13993003.03091-2020
18. Malik R, Chauhan G, Traylor M, et al. Multiancestry genome-wide association study of 520,000 subjects identifies 32 loci associated with stroke and stroke subtypes. Nat Genet. 2018;50(4):524–537. doi:10.1038/s41588-018-0058-3
19. Adams HP
20. Traylor M, Persyn E, Tomppo L, et al. Genetic basis of lacunar stroke: a pooled analysis of individual patient data and genome-wide association studies. Lancet Neurol. 2021;20(5):351–361. doi:10.1016/S1474-4422(21)00031-4
21. Woo D, Falcone GJ, Devan WJ, et al. Meta-analysis of genome-wide association studies identifies 1q22 as a susceptibility locus for intracerebral hemorrhage. Am J Hum Genet. 2014;94(4):511–521. doi:10.1016/j.ajhg.2014.02.012
22. Cordonnier C, Demchuk A, Ziai W, Anderson CS. Intracerebral haemorrhage: current approaches to acute management. Lancet. 2018;392(10154):1257–1268. doi:10.1016/S0140-6736(18)31878-6
23. Lu Y, Hajifathalian K, Ezzati M, et al. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1·8 million participants. Lancet. 2014;383(9921):970–983.
24. Burgess S, Butterworth A, Thompson SG. Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol. 2013;37(7):658–665. doi:10.1002/gepi.21758
25. Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol. 2016;40(4):304–314. doi:10.1002/gepi.21965
26. Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol. 2015;44(2):512–525. doi:10.1093/ije/dyv080
27. Hartwig FP, Davey Smith G, Bowden J. Robust inference in summary data Mendelian randomization via the zero modal pleiotropy assumption. Int J Epidemiol. 2017;46(6):1985–1998. doi:10.1093/ije/dyx102
28. Verbanck M, Chen CY, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet. 2018;50(5):693–698. doi:10.1038/s41588-018-0099-7
29. Seiler A, Camilo M, Korostovtseva L, et al. Prevalence of sleep-disordered breathing after stroke and TIA: a meta-analysis. Neurology. 2019;92(7):e648–e54. doi:10.1212/WNL.0000000000006904
30. Wu Z, Chen F, Yu F, Wang Y, Guo Z. A meta-analysis of obstructive sleep apnea in patients with cerebrovascular disease. Sleep Breath. 2018;22(3):729–742. doi:10.1007/s11325-017-1604-4
31. Bassetti CLA, Randerath W, Vignatelli L, et al. EAN/ERS/ESO/ESRS statement on the impact of sleep disorders on risk and outcome of stroke. Eur Respir J. 2020;55(4):1901104. doi:10.1183/13993003.01104-2019
32. Lavie L, Dyugovskaya L, Lavie P. Sleep-apnea-related intermittent hypoxia and atherogenesis: adhesion molecules and monocytes/endothelial cells interactions. Atherosclerosis. 2005;183(1):183–184. doi:10.1016/j.atherosclerosis.2005.06.024
33. Pizza F, Biallas M, Kallweit U, Wolf M, Bassetti CL. Cerebral hemodynamic changes in stroke during sleep-disordered breathing. Stroke. 2012;43(7):1951–1953. doi:10.1161/STROKEAHA.112.656298
34. Urbano F, Roux F, Schindler J, Mohsenin V. Impaired cerebral autoregulation in obstructive sleep apnea. J Appl Physiol. 2008;105(6):1852–1857. doi:10.1152/japplphysiol.90900.2008
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.