Back to Journals » Infection and Drug Resistance » Volume 16
Can Platelets/Mean Platelet Volume Accurately Diagnose Periprosthetic Joint Infection? Revealing Their Actual Diagnostic Efficacy
Authors Wang X , Zheng Z, Wang J, Ma H, Wang G, Zhao X
Received 17 August 2023
Accepted for publication 27 October 2023
Published 8 November 2023 Volume 2023:16 Pages 7155—7163
DOI https://doi.org/10.2147/IDR.S420323
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Xinjie Wang,1 Zhongren Zheng,1 Jialiang Wang,1 Hui Ma,2 Guodong Wang,2 Xiaowei Zhao2
1Department of Clinic Medicine, Jining Medical University, Jining, Shandong, 272067, People’s Republic of China; 2Department of Joint and Sports Medicine, Affiliated Hospital of Jining Medical University, Jining, Shandong, 272029, People’s Republic of China
Correspondence: Xiaowei Zhao, Department of Joint and Sports Medicine, Affiliated Hospital of Jining Medical University, Jining, Shandong, 272029, People’s Republic of China, Tel +86 18678766708, Email [email protected]
Background: Currently, there is no single test indicator for diagnosing periprosthetic joint infection (PJI) with an acceptable level of sensitivity. Therefore, ratio indicators have been introduced to improve the accuracy of diagnostic algorithms. Platelet count /mean platelet volume (PMR) is reported to be a potential PJI diagnostic biomarker, but its clinical value for diagnosing PJI is still uncertain. This study aims to provide additional evidence to support the effectiveness of PMR in accurately diagnosing PJI.
Methods: This study recruited 116 patients with PJI and 137 patients with aseptic loosening, divided them into PJI group and AL group. Collect subjects’ preoperative laboratory indicators such as ESR, CRP, PLT, MPV, etc. The area under the curve (AUC) was calculated by plotting the receiver operating characteristic (ROC) curve to determine the diagnostic efficacy of PMR.
Results: ESR, CRP, PLT, and PLT/MPV were significantly increased in the PJI group, while MPV levels were decreased (both P< 0.001). The AUC of the PMR was 0.752, and the optimal cut-off value for diagnosing chronic PJI was determined to be 27.8 based on the Youden index. The sensitivity and specificity for diagnosing PJI were 79.3% and 47.9%, respectively, with a positive predictive value of 68.27%, a negative predictive value of 69.80%, and a diagnostic odds ratio of 4.97. The AUC (0.752) of the ratio biomarker was lower than that of ESR (0.825) and CRP (0.900). After predictive model calculation, the combination of PMR, CRP, and ESR had an AUC value of 0.910, with a sensitivity of 84.5% and a specificity of 84.7%, showing good discriminative ability.
Conclusion: Compared with traditional biomarkers ESR and CRP, the value of the PMR for diagnosing PJI is not significant, but it can be used as an auxiliary indicator for PJI diagnosis in combination with other indicators (P< 0.001).
Keywords: periprosthetic joint infection, biomarkers, C-reactive protein, erythrocyte sedimentation rate, platelet count/mean platelet volume, diagnosis
Introduction
Periprosthetic joint infection (PJI) is a severe complication that can occur after total joint replacement (TJR). It often leads to pain, limited mobility, loosening of the prosthesis, prolonged antibiotic treatment, hospitalization, and the most severe outcomes of amputation or death. Due to the aging population and the increasing demand for TJR, the incidence of PJI is also increasing, causing a huge economic burden and mortality rate.1 Early and accurate diagnosis of PJI is of great significance for its subsequent treatment and prognosis. However, there is currently no independent or simple diagnostic gold standard for diagnosing PJI, so it is very important to find an index that can help clinicians effectively diagnose PJI. Bacterial infection around the prosthesis can lead to an immune response characterized by the recruitment and activation of neutrophils, and the infection can also activate the prothrombin activation pathway by releasing some procoagulant substances (such as tissue factor, thromboxane A2,) Or by affecting the function of vascular endothelial cells to promote the aggregation of platelets and coagulation factors to form thrombus at the site of infection, these mechanisms may lead to the activation of the coagulation system and related inflammatory responses. These changes can be reflected in changes in the body’s blood parameters, so some key indicators for effectively predicting and diagnosing PJI can be obtained in a timely and accurate manner by means of routine blood tests.
Among the inflammation markers, erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are the most commonly used, but their sensitivity and specificity are not perfect. Meanwhile, people have increasingly noticed the role of platelets as an important regulator of innate immunity on various infections, so they began to shift the focus of research to coagulation indicators.2 A large number of studies have shown that coagulation-related indicators may be promising markers for the diagnosis of PJI. Xu3 studied the potential value of platelet count alone in diagnosing PJI and reported good diagnostic value at a cutoff value of 221 × 109/L. In an experiment evaluating the impact of platelet depletion on host antibacterial defense in a mouse model of PJI, platelet count was found to affect bacterial load in the PJI mouse model.4 Tirumala5 analyzed data from 439 joint revision patients and found that platelet count had a sensitivity of 57.5% and specificity of 83.1% in diagnosing PJI, further indicating that platelets may be a potential predictive factor for diagnosing PJI. Djordjevic6 found a correlation between PLT/MPV ratio and bacteremia. In the field of orthopedics, Wang7 found that PLT/MPV ratio may be a useful parameter for early diagnosis of infectious nonunion. In addition, PLT/MPV was significantly correlated with the success rate of PJI treatment and the incidence of postoperative complications. Therefore, PMR may be an important indicator that our clinicians should focus on. Platelet (PLT) and mean platelet volume (MPV) are easily affected by systemic inflammation and infection during the progression of infectious diseases, and are often used as easily obtainable preoperative routine coagulation parameters for revision surgery. Inflammation or infection can cause reactive platelet generation to intensify, and mean platelet volume can decrease due to high concentrations of circulating platelet growth factors, leading to increased platelet count and decreased mean platelet volume. The changes and degree of change in these two parameters are different in the state of infection. Using the ratio of these parameters as a new diagnostic indicator can provide additional information from routine blood parameters, and can provide valuable insights for the diagnosis of periprosthetic joint infection (PJI) in a simple, rapid, and inexpensive way.8–10 However, there is some controversy over its diagnostic effectiveness, Paziuk11 first used the PMR calculated by combining PLT and MPV markers for diagnosing PJI and compared the AUC, sensitivity, and specificity of PMR with ESR and CRP markers through retrospective case analysis. They found that the AUC of PMR (69%) was lower than that of CRP (87.2%) and ESR (85.1%), but had higher sensitivity and specificity (84.1%, 80.8%) than ESR and CRP. Klemt12 found that the AUC of PMR (0.86) was higher than that of CRP (0.813) and ESR (0.792). Huang13 and Tirumala5 also reported the good diagnostic value of PMR. However, Sahin14 came to a different conclusion. They calculated the cutoff value of platelet count/mean platelet volume ratio through ROC analysis as 35.3 and found that the sensitivity and specificity of PMR for periprosthetic joint infection were 75.9% and 78.8%, respectively. Compared with ESR and CRP, PMR had a lower area under the curve, lower sensitivity, and similar specificity, indicating its poor diagnostic performance.
In summary, in view of the controversy of PMR in the diagnosis of PJI, and considering that it may be due to the small sample size, differences in population regions, and different inclusion and exclusion criteria, this study is strictly in accordance with the latest 2018 International Consensus Conference (International Consensus Meeting, ICM) standard was used as the inclusion standard of PJI, and the whole southwestern region of Shandong Province in China was used as the radiation range to expand the sample size to 298 patients who underwent joint revision in the past ten years. By retrospectively collecting cases, to verify whether PMR has better diagnostic value than the internationally recognized diagnostic markers CRP and ESR for PJI, and to determine whether it can be used as a useful indicator to guide clinicians in diagnosing PJI.
Data and Methods
Study Design
This was a single-center retrospective study that included 288 patients who underwent revision surgery for aseptic loosening (AL) or periprosthetic joint infection (PJI) after hip or knee arthroplasty from January 2013 to January 2023 in our hospital. Our hospital is a university-affiliated hospital in Jining City, Shandong Province. The Department of Joint and Sports Medicine performs more than 4000 joint replacement operations every year. Conduct an electronic study to determine the practical value of PMR in the diagnosis of periprosthetic infection. This study was approved by the Medical Research Ethics Committee of the Affiliated Hospital of Jining Medical College (No 2022-09-C002), and the requirement for informed consent was waived due to the use of de-identified data. This study was conducted in accordance with the Declaration of Helsinki (2008 version). The definition of PJI was based on the 2018 International Consensus Meeting (ICM) criteria15 (Table 1).
 |
Table 1 The Evidence-Based Definition for Periprosthetic Joint Infection |
Inclusion and Exclusion Criteria
Inclusion criteria: a. Patients diagnosed with chronic PJI or aseptic loosening (AL) according to the 2018 International Consensus Meeting (ICM) criteria. b. Patients who underwent hip or knee revision surgery at our institution. c. Complete patient records. Exclusion criteria: a. Inflammation-related diseases, including rheumatoid arthritis, systemic lupus erythematosus, ankylosing spondylitis, etc. b. Periprosthetic fractures, dislocations, prosthetic fractures, resulting revisions. c. Severe hepatic and renal insufficiency or malignant tumors. d. Insufficient data on serum markers. e. Suffering from other infectious diseases, such as pneumonia, patients with superficial infections, urinary tract infections.
Data Extraction
All patients who required revision TKA or THA had their detailed baseline characteristics (gender, age, body mass index, affected joint), treatment history, clinical symptoms, diagnosis, past medical history, surgical treatment, antibiotic treatment, and preoperative laboratory serum biomarker levels (WBC, ESR, CRP, ALB, PLT, MPV) recorded from the electronic medical record database of our unit. Fasting venous blood samples were collected from all patients on the day after admission and sent to our hospital’s laboratory within 2 hours for complete blood count and coagulation tests. The results of the blood sample tests were recorded, and the PMR was calculated as a ratio index for diagnosing PJI. All data included were compared between PJI and AL groups. The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), diagnostic odds ratio (DOR), and other parameters were analyzed by constructing receiver operating characteristic (ROC) curves and calculating the area under the curve (AUC) to evaluate the diagnostic value of PMR. The diagnostic performance of PMR was compared quantitatively with traditional biomarkers ESR and CRP to determine whether this ratio model can improve the accuracy and reliability of PJI diagnosis.
Statistical Analysis
SPSS 27.0 software and R software were used for data entry and statistical analysis. Categorical variables were expressed as frequencies and percentages, and differences in categorical variables were evaluated using chi-square tests and Fisher’s exact tests. Continuous variables were expressed as means and standard deviations. Quantitative data were evaluated using Mann–Whitney U-tests (if the data were skewed or the variances were unequal) and independent sample t-tests (if the data were normally distributed). The clinical characteristics of the PJI group and AL group were compared using independent sample t-tests or chi-square tests. Differences were considered statistically significant at P < 0.05. The relationship between biomarkers and PJI was evaluated using Mann–Whitney U-tests and multivariate logistic regression (forward likelihood ratio method). Covariates such as surgical joint, age, gender, and BMI were included in the multivariate model to adjust for confounding effects.
Results
Population Characteristics
A total of 253 patients were included and divided into two groups according to the 2018 International Consensus Meeting (ICM) criteria: 1) PJI group, consisting of 116 patients diagnosed with PJI based on the standard criteria; and 2) AL group, consisting of 137 patients who underwent revision THA due to aseptic complications. (Figure 1) Demographic data were normally distributed, and there were no statistically significant differences in baseline characteristics such as age and gender between the study cohorts. The differences in the levels of ESR, CRP, PLT, MPV, and PMR between the two groups were compared. In the PJI group, an increase in the average levels of PLT and PMR ratio and a decrease in the average level of MPV were observed. The proportion of patients with knee joint problems was higher than that in the AL group (75 (64.7%) > 22 (16.1%)), and the differences were statistically significant (all P <0.05). (See Table 2 for the differences in patient characteristics and biomarker levels.) At the same time, we compared the diagnostic ability of the biomarkers ESR, CRP, and PMR, and calculated the best cut-off value, sensitivity, specificity, PPV, and NPV for each biomarker based on the Youden index (Table 3), using the area under the ROC curve. In addition, to further improve sensitivity and specificity, we combined traditional biomarkers into a predictive model, including blood indicators (ESR and CRP) and the ratio indicator PMR, to evaluate their diagnostic value in predicting PJI. When PMR was combined with ESR and CRP for detection, the AUC increased from 0.752 to 0.910. (Figure 2) The sensitivity, specificity, PPV, and NPV of the new combination were 84.5%, 84.7%, 75.0%, and 60.98%, respectively. Compared with using PMR, CRP, and ESR alone, the combined use of ratio biomarkers showed good diagnostic value (P <0.001).
 |
Table 2 Patient Demographics and Biomarker Values |
 |
Table 3 Receiving Operating Characteristic Curve (ROC) Analysis of Serum Biomarkers in the Diagnosis of Periprosthetic Joint Infection |
 |
Figure 1 The flow diagram of study enrollment. Abbreviations: PJR, periprosthetic joint infection; AL, aseptic loosening. |
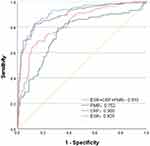 |
Figure 2 The ROC curves of PMR, ESR, CRP for the diagnosis of PJI. |
Discussion
Periprosthetic joint infection (PJI) is one of the most serious complications after joint replacement surgery. Considering the negative impact of PJI, early diagnosis and treatment are crucial. Recent studies have shown that new biomarkers such as leukocyte esterase (LE), calprotectin, procalcitonin, α-defensin, and next-generation sequencing show promising diagnostic performance, but these tests are expensive, require specialized equipment, cannot be implemented in all institutions, and cannot serve as a single gold standard for diagnosing PJI.16 The use of other diagnostic criteria such as Synovial fluid examination, clinical examination, intraoperative tissue examination, and culture can significantly improve diagnostic accuracy, but many of these procedures are time-consuming, expensive, and invasive. Therefore, finding reliable, accurate, and convenient potential biomarkers for diagnosing PJI is key to preoperative diagnosis and developing appropriate treatment plans. In most institutions, some important systemic parameters can be obtained through blood tests, including ESR, CRP, monocyte count, neutrophil count, lymphocyte count, platelet count, and mean platelet volume (MPV). These biomarkers have relatively low invasiveness, short turnover time, high throughput, moderate complexity, low cost, and ready availability, providing a new potential method for many clinicians to consider obtaining more accurate information for diagnosing PJI through single testing. PLT/MPV, as a ratio index, combines two indicators to obtain additional information during routine testing. In theory, its repeatability and accuracy should be better than that of a single biomarker. As a combined ratio index, platelet-to-mean platelet volume ratio (PLT/MPV) allows for the synergistic analysis of two conventional serum biomarkers to obtain additional information without incurring extra costs. The repeatability and accuracy of PLT/MPV are superior to those of single biomarkers, thereby further improving diagnostic accuracy.
In our study, we evaluated the baseline characteristics of 253 patients and compared the levels of ESR, CRP, and PML biomarkers between the PJI and AL groups. We then assessed the diagnostic performance of each indicator by drawing ROC curves and calculating sensitivity, specificity, and the Youden index. We found that the diagnostic performance of PMR (AUC=0.752) was significantly lower than that of ESR (AUC=0.825) and CRP (AUC=0.900), with lower sensitivity (79.3%) and specificity (68.6%) than ESR and CRP, confirming that PMR has a lower practical value than ESR and CRP in the diagnosis of PJI. However, an AUC > 0.7 indicates that it has some role, and combining ESR and CRP increased the AUC from 0.752 to 0.910, with both sensitivity and specificity above 80%, demonstrating excellent diagnostic performance.
Although ratios or combined biomarkers have potential diagnostic value for PJI, the number of studies on this topic is still limited. Through the analysis of previous studies on PMR, it was found that the conclusions on the diagnostic efficacy of PJI were controversial (Table 4), possibly due to limitations in the validation of ratio or combined indicators. First, most studies are retrospective, and all retrospective study designs are subject to inherent limitations, including reporting and recall biases, which can lead to selection bias. Second, peripheral blood ratio biomarkers are influenced not only by bacterial species but also by other factors such as medication use, disease status, age, and some unobserved comorbidities. Third, different diagnostic criteria for excluding PJI, small sample sizes, and different cutoff values proposed for each parameter may lead to heterogeneity between some of the evaluated results, which may alter the ability of these diagnostic tools to differentiate between infectious and aseptic loosening and thus change their accuracy. Fourth, the use of ratios or combined indicators increases the computational burden, which may be cumbersome.
 |
Table 4 Characteristics of Previous Studies on PMR Diagnosis |
The PMR ratio combines two pathological and physiological indicators, PLT and MPV, which are associated with inflammation or infection, but its diagnostic performance is significantly lower than that of established serum parameters such as ESR and CRP, and cannot be used as an independent diagnostic indicator for PJI. However, PMR as a novel inexpensive, rapid, minimally invasive serological ratio marker has been found to have higher diagnostic efficacy when combined with other inflammatory markers as a new diagnostic combination. Ratios or combined diagnostic indicators may have become new benchmarks for diagnosing PJI. In the future, through sequential or parallel trials, these ratio markers can be incorporated into diagnostic algorithms with other indicators, and further large-scale, prospective, multicenter studies can refine research results. Therefore, by selecting appropriate indicators for ratio or combination can increase the sensitivity and specificity of diagnostic tests, assisting physicians in early identification or exclusion of PJI and improving clinical diagnostic performance.
Conclusion
Based on the above results and analysis, the diagnostic performance of PMR is significantly lower than that of ESR and CRP, so it is not a perfect detection index in the diagnosis of PJI. However, it can be used as an auxiliary diagnostic indicator, combined with other serological indicators such as ESR and CRP, to improve the diagnostic accuracy of PJI.
Abbreviations
CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; WBC, white blood cell; LE, leukocyte; PMN (%); Polymorphonuclear Neutrophils (%); BMI, Body Mass Index; PLT, blood platelet; MPV, Mean Platelet Volume; PMR, Platelet count /mean platelet volume; AUC, area under the curve; PPV, Positive Predictive Value; NPV, Negative Predictive Value; DOR, diagnostic odds ratio; PLR, Positive likelihood ratio; NLR, Negative likelihood ratio; MLR, monocyte/lymphocyte ratio.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
This study conformed to the guidelines of the Helsinki Declaration. Ethics approval was obtained by the Research Ethics Committee of the Institutional Review Committee of Jining Medical College Affiliated Hospital.
Acknowledgments
We acknowledge that all the participants participated in this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests.
References
1. Kapadia BH, Berg RA, Daley JA., et al. Periprosthetic joint infection. Lancet. 2016;387:386–394. doi:10.1016/S0140-6736(14)61798-0
2. Koupenova M, Clancy L, Corkrey HA, Freedman JE. Circulating platelets as mediators of immunity, inflammation, and thrombosis. Circ Res. 2018;122:337–351. doi:10.1161/CIRCRESAHA.117.310795
3. Xu H, Xie J, Yang J, et al. Plasma fibrinogen and platelet count are referable tools for diagnosing periprosthetic joint infection: a single-center retrospective cohort study. J Arthroplasty. 2020;35:1361–1367. doi:10.1016/j.arth.2019.12.015
4. Greig D, Trikha R, Sekimura T, et al. Platelet deficiency represents a modifiable risk factor for periprosthetic joint infection in a preclinical mouse model. J Bone Joint Surg Am. 2021;103:1016–1025. doi:10.2106/JBJS.20.01428
5. Tirumala V, Klemt C, Xiong L, et al. Diagnostic utility of platelet count/lymphocyte count ratio and platelet count/mean platelet volume ratio in periprosthetic joint infection following total knee arthroplasty. J Arthroplasty. 2021;36:291–297. doi:10.1016/j.arth.2020.07.038
6. Djordjevic D, Rondovic G, Surbatovic M, et al. Neutrophil-to-lymphocyte ratio, monocyte-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and mean platelet volume-to-platelet count ratio as biomarkers in critically Ill and injured patients: which ratio to choose to predict outcome and nature of bacteremia? Mediators Inflamm. 2018;2018:3758068. doi:10.1155/2018/3758068
7. Wang Z, Mao H-J, Qiu X-S, Chen Y-X, Xu G-Y. Diagnostic value of platelet indices in infected nonunion: a retrospective study. J Orthop Surg. 2022;17:200. doi:10.1186/s13018-022-03096-3
8. Balta O, Altınayak H, Aytekin K, et al. Mean platelet volume to platelet count ratio as a predictor of mortality in unstable pertrochanteric fracture treated with short proximal femoral anterograde nail. Indian J Orthop. 2022;56:1181–1191. doi:10.1007/s43465-022-00613-8
9. Ösken A, Hacı R, Dinç Asarcıklı L, et al. Mean platelet volume/platelet count ratio as a predictor of stent thrombosis in patients with ST-segment–elevation myocardial infarction. Ir J Med Sci. 2021;190:1095–1102. doi:10.1007/s11845-021-02626-y
10. Vélez-Páez JL, Legua P, Vélez-Páez P, et al. Mean platelet volume and mean platelet volume to platelet count ratio as predictors of severity and mortality in sepsis. PLoS One. 2022;17:e0262356. doi:10.1371/journal.pone.0262356
11. Paziuk T, Rondon AJ, Goswami K, Tan TL, Parvizi J. A novel adjunct indicator of periprosthetic joint infection: platelet count and mean platelet volume. J Arthroplasty. 2020;35:836–839. doi:10.1016/j.arth.2019.10.012
12. Klemt C, Tirumala V, Smith EJ, Xiong L, Kwon Y-M. Complete blood platelet and lymphocyte ratios increase diagnostic accuracy of periprosthetic joint infection following total Hip arthroplasty. Arch Orthop Trauma Surg. 2022;143:1441–1449. doi:10.1007/s00402-021-04309-w
13. Huang J-C, Chen X, Qiang S, et al. Exciting performance of plasma fibrinogen in periprosthetic joint infection diagnosis. Orthop Surg. 2021;13:812–816. doi:10.1111/os.12964
14. Sahin E, Karaismailoglu B, Ozsahin MK, Guven MF, Kaynak G. Low value of platelet count to mean platelet volume ratio to diagnose chronic PJI: a case control study. Orthop Traumatol Surg Res. 2021;107:102899. doi:10.1016/j.otsr.2021.102899
15. Saeed K, McLaren AC, Schwarz EM, et al. 2018 international consensus meeting on musculoskeletal infection: summary from the biofilm workgroup and consensus on biofilm related musculoskeletal infections. J Orthop Res. 2019;37:1007–1017. doi:10.1002/jor.24229
16. Yang F, Zhao C, Huang R, et al. Plasma fibrinogen in the diagnosis of periprosthetic joint infection. Sci Rep. 2021;11:677. doi:10.1038/s41598-020-80547-z
17. Festa E, Ascione T, Bernasconi A, et al. Diagnostic performance of neutrophil to lymphocyte ratio, monocyte to lymphocyte ratio, platelet to lymphocyte ratio, and platelet to mean platelet volume ratio in periprosthetic hip and knee infections: a systematic review and meta-analysis. Diagn Basel Switz. 2022;12:2033.
18. Balato G, Ascione T, Festa E, et al. The diagnostic accuracy of neutrophils to lymphocytes ratio, platelets to lymphocytes ratio, monocytes to lymphocytes ratio, and platelets to mean platelet volume ratio in diagnosing periprosthetic knee infections. are gender-specific cutoff values needed? J Arthroplasty. 2022;38(5):918–924. doi:10.1016/j.arth.2022.11.014
19. Wang R, Shi G, Zhang H, et al. Globulin and albumin/globulin ratios as potential biomarkers for the diagnosis of acute and chronic peri-prosthetic joint infections: a retrospective study. Surg Infect. 2023;24:58–65. doi:10.1089/sur.2022.215
20. Maimaiti Z, Xu C, Fu J, et al. The potential value of monocyte to lymphocyte ratio, platelet to mean platelet volume ratio in the diagnosis of periprosthetic joint infections. Orthop Surg. 2022;14:306–314. doi:10.1111/os.12992
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
