Back to Journals » Neuropsychiatric Disease and Treatment » Volume 20
Building and Validation of an Acute Event Prediction Model for Severe Mental Disorders
Authors Wang T, Wang L, Yao Y, Liu N, Peng A, Ling M, Ye F, Sun J
Received 7 December 2023
Accepted for publication 9 April 2024
Published 17 April 2024 Volume 2024:20 Pages 885—896
DOI https://doi.org/10.2147/NDT.S453838
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Ting Wang,1,2,* Lin Wang,1,* Yunliang Yao,2,* Nan Liu,1 Aiqin Peng,1 Min Ling,2 Fei Ye,1 JiaoJiao Sun1
1Affliated WuTaiShan Hospital of Medical College of Yangzhou University, Yangzhou Mental Health Center, Yangzhou, Jiangsu, People’s Republic of China; 2School of Medicine & Nursing, Huzhou University, Huzhou, Zhejiang, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Fei Ye; Jiaojiao Sun, Affiliated WuTaiShan Hospital of Medical College of Yangzhou University, Yangzhou mental health center, Yangzhou, Jiangsu, 225000, People’s Republic of China, Tel +8613645251172 ; +8615150805127, Email [email protected]; [email protected]
Background: The global incidence of acute events in psychiatric patients is intensifying, and models to successfully predict acute events have attracted much attention.
Objective: To explore the influence factors of acute incident severe mental disorders (SMDs) and the application of Rstudio statistical software, and build and verify a nomogram prediction model.
Methods: SMDs were taken as research objects. The questionnaire survey method was adopted to collect data. Patients with acute event independent factors were screened. R software multivariable Logistic regression model was constructed and a nomogram was drawn.
Results: A total of 342 patients with SMDs were hospitalized, and the number of patients who encountered acute events was 64, which accounted for 18.70% of all patients. Statistical significances were found in many aspects (all P ˂ 0.05). Such aspects included Medication adherence, disease diagnosis, marital status, caregivers, social support and the hospitalization environment (odds ratio (OR) = 4.08, 11.62, 12.06, 10.52, 0.04 and 0.61, respectively) were independent risk factors for the acute events of patients with SMDs. The prediction model was modeled, and the AUC was 0.77 and 0.80. The calibration curve shows that the model has good calibration. The clinical decision curve shows that the model has a good clinical effect.
Conclusion: The constructed risk prediction model shows good prediction effectiveness in the acute events of patients with SMDs, which is helpful for the early detection of clinical mental health staff at high risk of acute events.
Keywords: SMDs, acute event, influencing factors, predictive model and nomogram
Introduction
Severe mental disorders (SMDs) refer to serious mental illness symptoms that cause severe damage to the social adaptation function of patients. SMD patients cannot fully understand their own health and the objective reality or handle their own affairs of psychiatric disorders,1 including schizophrenia, bipolar disorder and major depression disorder.2,3 They usually use antipsychotic medication. Taking drugs is common, which however is associated with serious adverse consequences and leads to disability and premature death to a great extent.4 The clinical effect of this kind of individual patient depends on the accurate prediction of results.5 It is reported that the prevalence of Chinese SMD patients showed a trend of sustained growth. By 2018, the reported prevalence of SMD patients in China had amounted to 4.3 per thousand.6 The risk of acute events in SMDs is higher among the general population.7 The ability of SMD patients to identify or control damage often exerts a severe impact on society. Common psychiatric acute events include violence, suicide, self-injury, flight, etc.8
Clinical prediction models (CPMs) show good performance, with good diagnosis and calibration, and satisfactory validity and clinical utility.9 Based on clinical practice, individualization and automation, the diagnosis of a mental illness risk calculator has developed into the information automatic screening of electronic medical records to help identify individuals at risk of SMDs.10 However, the risk calculator is not the related data and online research of these patients in the case of acute events.11 SMDs involve some kinds of several serious mental illness, the heterogeneity of their patients is high, and such studies are widely involved worldwide. Studies on its prediction model are as follows: the construction and application of an analytical predictive model of impulsive behavior in hospitalized schizophrenia;12 the construction and evaluation of a suicide risk prediction model in patients with schizophrenia;13 and the suicide prediction of severe mental illness: development and validation of clinical prediction rule (OxMIS).14 However, most of the above studies are performed with a single or several influencing factors. To bridge this gap, this study intends to analyze the independent influencing factors of acute events in SMD and to construct a predictive model. A prediction model was built for early clinical mental health professionals to identify high-risk patients and take appropriate intervention measures according to their willingness, which maximized safety in the hospital.
Methods
Study Population
SMD patients in a tertiary hospital in Yangzhou were selected as investigation objects. The inclusion criteria are as follows: 1. Patients conformed to the diagnostic criteria of the international classification of diseases (the 10th edition revised; ICD-10);15 2. Patients were diagnosed with schizophrenia, bipolar disorder and major depression disorder; 3. Patients offered informed consent, and patients or their family members volunteered to join the study. The exclusion criteria are as follows: 1. Patients were accompanied by mental retardation, dementia, substance abuse or organic brain disorder; 2. Patients were diagnosed with severe body diseases or complications; 3. Patients with language or cognitive impairment cannot complete scales; 4. Patients withdrew informed consent. According to the Logistic regression analysis of the sample size calculation method,16 342 cases of this study were eventually included in the sample, given 10% invalid questionnaires. In accordance with the ratio of 7:3, modeling and validation groups contained 239 and 103 examples, respectively. The criteria for acute events during hospitalization are: violence during hospitalization, suicide and self-injury.
After a full explanation of the study, All participants joined voluntarily and signed an informed consent form before participation. The study protocol gained the approval of the Institutional Review Board (IRB) of the Yangzhou Wutai Mountain Hospital, Jiangsu Province (WTSLL2023001).
Definition of Variables
Questionnaire on General Information
With reference to relevant literature and through the discussion of the project design team, general data tables were completed. The following contents were included in tables: gender, age, nationality, occupation, cultural degree, marital status, living environment, medical payment method and religious belief.
Questionnaire on Medical Record Information
The questionnaire completed by investigators according to the medical records of patients included: times of hospitalization in the past year, total times of hospitalization, SMD type, always acute event type, age, course of disease, family history, the length of the environment, with or without escort, relationship with patients and escort patients taking antipsychotic drugs over the past year.
Brief Psychiatric Rating Scale
The Brief Psychiatric Rating Scale (BPRS)17,18 is used to assess the severity of mental illness patients’ mental symptoms: two negative symptoms including anxiety and depression, and the lack of energy and three positive symptoms including thought disorder, activation and hostile suspicion. The scale utilizes the seven-score rating of 1 = asymptomatic and 7 = very severe, with a total of 18 ~ 126 points. Patients’ symptoms will be more severe when the score is higher. The scale is composed of 18 entries, and Cronbach’s coefficient is 0.787 ~ 0.97.
Hamilton Depression Scale19,20
Easy to operate, the Hamilton Depression Scale (HAMD) consumes little time, and with good validity. It consists of 24 items. The reaction of 14 items can be divided into five grades from 0 (no symptoms) ~ 4 (extreme). According to the score of 0 ~ 4 points and response, 10 items are divided into three grades from 0 (no symptoms) ~ 2 (moderate). According to the score of 0 ~ 2 points and the possible range of 0 ~ 76 points, the severity of depression was positively related to the score of the scale.21 Patients’ symptoms will be more severe when the score is higher. It is generally thought that the total HAMD scores < 8, 8 ~ 20, 21 ~ 35 and > 35 are divided into normal state, underlying depression, depression and severe depression, respectively. Cronbach’s coefficient is 0.766.22
Hamilton Anxiety Scale23,24
The Hamilton Anxiety Scale (HAMA), an important tool used by a psychiatrist for the clinical diagnosis and disease degree of patients, can better reflect illness severity. It comprises 14 items. The reaction of patients is classified into five grades from 0 (no symptoms) ~ 4 (extreme). Each component has a score of 0 ~ 4 points within the possible range of 0 ~ 56 points. Higher scores show more severe symptoms. According to the evaluation, the total HAMA scores < 7, 7 ~ 14 and > 14 are divided into no anxiety, underlying anxiety and anxiety or obvious anxiety, respectively. Among patients, 21 of 29 were divided into serious or anxiety. Cronbach’s coefficient is 0.766.
Pittsburgh Sleep Quality Index25
The Pittsburgh Sleep Quality Index (PSQI) covers 19 self-evaluations and five review items. A total of seven entries used for scoring are included: I. sleep quality, II. sleep time, III. sleep duration, IV. sleep efficiency, V. sleep disorders, VI. hypnotic drugs and VII. daytime dysfunction. Each dimension has a score of 0 ~ 3 points, and the total score is 0 ~ 21 points. The total score is the sum of seven components. The score > 7 points indicates a sleep obstacle. The higher the score is, the worse the sleep quality will be. Cronbach’s coefficient is 0.842.
Morisky Medication Adherence Scale-826
The Morisky Medication Adherence Scale-8 (MMAS-8) is divided into three dimensions and composed of eight items. Items 1 ~ 7 are given the options of “yes” and “no”, with a score of 0 and 1 point. Item 8 includes five-level scoring, namely, 1 = never, 0.75 = sometimes, 0.5 = occasionally, 0.25 = often and 0 = all the time. The scale has a score of 8 points and three levels: ˂ 6, 6 ~ 7 and 8 points for poor, moderate and good medication adherence, respectively. Cronbach’s coefficient is 0.835.27
Social Support-Rating Scale28
The Social Support-Rating Scale (SSRS) is divided into three dimensions and composed of 10 items. Items 1 ~ 4 and 8 ~ 10 choose the options of 1, 2, 3 and 4, respectively, with a score of 1, 2 and 4 points. Item 5 has the options of A, B, C and D. Each option has a score of 1 ~ 4 points from no to full support, respectively. Items 6 ~ 7 have the answers of “no source” for 0 and “the following sources”. Higher scores indicate feelings of higher social support.29 Cronbach’s coefficient is 0.92.30
Insight and Treatment Attitude Questionnaire31
Divided into two dimensions and composed of 11 items, the Insight and Treatment Attitude Questionnaire (ITAQ) uses the three-grade scoring method, namely 0, 1 and 2 = no, partial and complete self-knowledge, respectively. The total score is 22 points. The higher the score is, the more complete the self-knowledge will be. The score from the known source can be divided into three levels: 20 points or more, 6 ~ 19 and 5 points or less indicate complete, partial and no self-knowledge, respectively. Cronbach’s coefficient is 0.869.32
Statistical Analysis
SPSS 25.0 statistical software was used for the statistical analysis of data. Statistics that obeyed normal distribution were expressed by x + s, and those that followed skewness distribution were expressed by the median (quartile). Frequency and composition ratio were used to describe classification variables. A t-test was used to compare the measurement data obeying normal distribution between groups. A rank sum test was used to compare the measurement data without obeying normal distribution between groups. Classification variables between groups were compared using the x2 test. Multivariable Logistic regression analysis was performed to pick out the independent risk factors for the suicidal ideation of patients. A risk prediction model was constructed with R4.1.2 software. A nomogram was drawn to visualize the Logistic regression model. The prediction ability of the receiver operating characteristic curve (ROC) evaluation model and the internal validation of the model were verified by the Bootstrap validation method. P < 0.05 or 0.01 for the difference was of statistical significance.
Results
General Information on Research Objects
Of 342 hospitalized patients with SMDs, 114 (26.5%) in patients reported acute events, including 87 and 27 (28.9% and 21.0%) in modeling and validation groups, respectively. The accident rate between the two groups showed no statistically significant difference. The general data of research objects are shown in Table 1.
 |
Table 1 Patient Clinical Characteristics |
Single Factor Analysis of Hospitalized SMD Patients Encountering Acute Events
The single factor analysis results showed that the incidence age, hospitalization time, drug kinds, MMAS-8, SSRS, ITAQ, PSQI, HAMD, disease diagnosis, hospital environment, occupation, marital status, caregivers and childhood bad situation of hospitalized patients with SMDs were statistically significant (P < 0.05). Details are presented in Table 2.
 |
Table 2 Univariate Statistics of Patients |
Multivariate Logistic Regression Analysis of the Influence Factors of hospitalized Patients with SMD Acute Incidents
Whether acute events occurred in hospitalized patients with SMDs was used as an independent variable. Values were assigned to multiple classification variables (Table 3). In single factor analysis, variables with P < 0.05 dependent variables for multivariable Logistic regression analysis of variables. Multi-factor analysis results showed that disease diagnosis, marital status, caregivers and hospital environment were independent risk factors for the accurate events of hospitalized patients with SMD. Among them, disease diagnosis and marital status were protective factors. Details are shown in Table 4.
 |
Table 3 Variables Assignment Table of Logistic Stepwise Regression Analysis |
 |
Table 4 Multivariate Logistic Regression Analysis of Patients |
Building the Nomogram of the Risk Prediction Model for Patients with SMDs
Based on the Logistic regression model: Z = 1.80–0.16 * MMAS-8 −0.90 * disease diagnosis −1.28 * marital status +1.73 * caregivers +5.80 * SSRS +8.43 * the hospital environment, R software was used to build and visualize a nomogram, as shown in Figure 1.
The specific condition of each risk factor in the nomogram corresponds to corresponding points. The total score was obtained by adding the scores of five indicators to the model. A vertical line was drawn where the total score was obtained, The value corresponding to the intersection position of the vertical line and the “occurrence probability of acute events” was the risk of acute events in hospitalized SMD patients.
Validation of the Risk Prediction Model of Hospitalized SMD Patients Encountering Acute Events
Distinguishing Ability
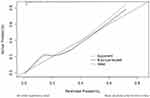
Prediction variables were used as a test, and hospitalized SMD patients encountering acute events were taken as state variables to draw the ROC curve. The modeling prediction model set of the AUC value is 0.77. When the best cutoff value was taken, the Yoden index was 0.62, and sensitivity and specificity were 0.90 and 0.72, respectively. The AUC value of the prediction model in the validation group was 0.80. When the best cutoff value index was 0.57, sensitivity and specificity were 0.81 and 0.76, respectively. That prediction model showed better performance, as shown in Figure 2.
Calibration Ability
The calibration ability of the risk prediction model for the risk of acute events in hospitalized patients with SMDs was evaluated using the Hosmer-Lemeshow (H-L) goodness-of-fit test. The result showed x2 = 8.08, p = 0.43. In the prediction of hospitalized SMD patients encountering acute events, the predicted and actual occurrence probabilities of the model showed no statistical difference, which indicated its better calibration ability, as shown in Figure 3.
Clinical Decision Curve Analysis
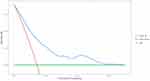
Clinical decision curve analysis (DCA) is used to evaluate the clinical efficacy of the risk prediction model for the acute events of hospitalized patients with SMDs. It is also used to determine the use of the clinical prediction model to inform whether clinical decisions do more harm than good. It can be seen from Figure 4 that higher clinical utility can be obtained when the probability is 0.01 ~ 0.90.
Discussion
Present Situation Analysis of Hospitalized SMD Patients Encountering Acute Events
The survey of 342 hospitalized patients with SMDs showed that the incidence of acute events was 18.70%. Wang and Chen33–37 claimed that “differences exist between the results”. The possible reasons are as follows: 1. Differences were found between research objects, which were related to the different inclusion and exclusion criteria of different studies. The research objects of this study were hospitalized patients diagnosed with SMDs. 2. Differences were found in assessment scales. 3. Events mismatched the standard evaluation, and the evaluation standard of the outcome variable in this research was: accurate events occurred in patients with SMDs during hospitalization.
Risk Factors for Hospitalized SMD Patients Encountering Acute Events
The acute events of patients are a social, psychological and environmental outcome of the combined action of multiple factors.38 Getting familiar with the management of these risk factors of hospitalized patients with SMD acute incidents has important significance for forecasting early warning and intervention.
Social Demographic Factors
In this study, it was found that marital status, caregivers, the hospital environment and social support were independent influence factors for the acute events of SMD patients. Medication adherence and marital status were protective factors. Married, parents’ care, low social support score and living in a closed room were lower risks of acute events in SMD patients. Research by Liu, Zheng et al39–41 proved the viewpoint of the first three factors. The reasons may be as follows: 1. Families and society may not change various aspects of requirements for married patients in the disease state, which causes psychological stress to be larger than normal. This in turn leads to more moods in patients and the increased occurrence probability of acute events. 2. Parents play an irreplaceable role in the childhood of children. Parents’ care and company as a spiritual pillar can make patients experience a sense of security, alleviate their negative moods and increase the enthusiasm of patients about treatment to maintain the stability of the disease. 3. Items in all closed-end rooms were provided for SMD patients by the hospital during hospitalization. These closed-end rooms were wider in range than semi-enclosed wards, with more stringent schedules. In addition, 24-hour monitoring was performed in the disease’s acute stage. Therefore, the occurrence rate of acute events in totally enclosed wards was lower than that in semi-closed ones. In this study, however, the idea of social support was different from those of Zeng et al.42 The reasons may be as follows: 1. The research objects in the hospital environment were arranged in fully and semi-closed wards. The vast majority of patients were in fully enclosed wards without family members during hospitalization. 2. Patients with SMDs were subjected to small psychological pressure due to the lack of good social support, which thus led to the decreasing risk of acute events.
Disease Diagnosis
In this research, it was shown that disease diagnosis was not only an independent influence factor but also a protective factor for the acute events of SMDs, which was similar to the results of V JM, Hj et al43,44 The reasons are as follows: 1. The symptoms of schizophrenia are one of the most serious SMDs. 2. Schizophrenia can give rise to abnormal behavior and thought disorders in patients. Thus, these patients are prone to various types of acute events. The death rate of schizophrenia is higher than that of other types of SMD. 3. Bipolar disorder is a chronic recurrent SMD.45 Thus, the incidence of acute events is lower than those of other types of SMD.
Medication Adherence
In this study, it was proved that the medication compliance of SMD patients, an independent factor of acute events, was similar to the results of Stentzel and Chen et al46,47 The possible reasons are as follows 1. Medication compliance affects such patients in stable condition. Patients in poor condition are more prone to acute events when the fluctuation in condition is more frequent. 2. The increase in family care burden and economic pressure exerts enormous pressure on patients and family spirit. As a result, patients are prone to urgent events.
Ideal prediction effect of the risk prediction model of SMDs in patients with acute events.
In this research, R software was used to construct a Logistic regression model and draw a diagram. The sensitivity and specificity of modeling and validation groups were high. The AUC values of both groups were greater than 0.75. This shows that the model has an ideal prediction effect and is beneficial for mental health professionals to screen the acute events of high-risk SMD crowds during hospitalization. Meanwhile, calibration and clinical decision curves were used to evaluate the calibration degree and clinical effectiveness of the model. The result shows that the model can be used for clinical diagnosis and treatment activities, with good clinical application value.
Conclusions
To sum up, this study focused on exploring the characteristics of patients with acute events in low- and high-risk SMDs. The results showed that the risk of acute events occurring in patients who were married, with good medication adherence, SMDs diagnosed with bipolar disorder, parents’ care, a lower score of social support and living in totally closed wards during hospitalization in the Psychiatry Department was low. The forecast model of acute events can be applied to the screening and evaluation of potential SMD patients. The acute event prediction model can be used to screen and evaluate SMD patients who encounter acute events. In addition, individualized intervening measures were taken according to different groups. This can more effectively reduce the occurrence and severity of acute events in SMD patients hospitalized in psychiatric medical units, and improve medical efficiency.
The research objects include only patients of this hospital. In the future, researchers should face some problems in clinical research in the field of psychiatry, pay attention to reasonable and strict experimental design, and provide the basis for optimal clinical decisions. In the meantime, multicenter and multi-zone large sample studies can be conducted to constantly adjust to improve accuracy and be more in line with clinical practice for wide application in mental hospital wards.
Data Sharing Statement
All data of this study can be obtained by contacting the Email address of the corresponding author. The Email address of the corresponding author is [email protected].
Ethics Statement
This study was approved by the Ethics Committee of the Yangzhou Wutai Mountain Hospital (WTSLL2023001). All participants signed the informed consent form before entering the study, and all procedures performed in this study involving human participants were in accordance with the Declaration of HelsinkiEthics approval and consent to.
Acknowledgments
This study were supported by the 2022 annual hospital project funding fund of Yangzhou Wutai Mountain Hospital in Jiangsu Province (Ting Wang WTS2022021) and the 2023 Annual Medical Scientific Research Project of Yangzhou Municipal Health Commission (2023-2-35). The MMAS-8 Scale (US Copyright Registration No. TX0008632533), content, name, and trademarks are protected by US copyright and trademark laws. Permission for use of the scale and its coding is required. A license agreement is available from MMAR, LLC., www.moriskyscale.com.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wang Y, Li C, Song P. Analysis of death and life reduction of patients with severe mental disorders in Ningbo from 2016 to 2020. Preventive Med. 2022;34(12):1224–1229. doi:10.19485/j.cnki.issn2096-5087.2022.12.007
2. Nunes KG, da Rocha NS. da Rocha NS.Resilience in severe mental disorders: correlations to clinical measures and quality of life in hospitalized patients with major depression, bipolar disorder, and schizophrenia. Qual Life Res. 2022;31(2):507–516. doi:10.1007/s11136-021-02920-3
3. Forma F, Koep E, White J, Belland A. Impact of treatment-related discussions on healthcare resource use and costs among patients with severe mental illness. Curr Med Res Opin. 2021;1. doi:10.1080/03007995.2021.1943341
4. Mokdad AH, Ballestros K, Echko M, Glenn S, Olsen HE. The State of US Health, 1990–2016: burden of Diseases, Injuries, and Risk Factors Among US States. JAMA. 2018;319(14):1444–1472. doi:10.1001/jama.2018.0158
5. Fusar-Poli P, Mcgorry PD, Kane JM. Improving outcomes of first‐episode psychosis: an overview. World Psychiatry. 2017;16(3):251–265. doi:10.1002/wps.20446
6. Xia Y, Li Y, Jing X. Study on the perfection of the operation mechanism of infectious disease prevention and control system in Shanghai and Shaanxi. Prevent Med Forum. 2019;25(4):4.
7. Han J, Sun S, Huang X. Ethnic source inference study of four populations in Inner Mongolia based on 27-plex SNPs. Chin J Foren Med. 2020;35(3):5.
8. Yue S. Training for psychiatric nurses in dealing with stress. J Pract Nurs. 1997;08:31–32.
9. Wang L, Li N, Heizhati M, et al. Prevalence and predictive nomogram of depression among hypertensive patients in primary care: a cross-sectional study in less developed Northwest China. Medicine. 2021;100(4):e24422. doi:10.1097/MD.0000000000024422
10. Fusar-Poli P, Rutigliano G, Stahl D, et al. Development and validation of a clinically based risk calculator for the transdiagnostic prediction of psychosis. JAMA Psychiatry. 2017;74(5):493–500. doi:10.1001/jamapsychiatry.2017.0284
11. Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi:10.1016/S0140-6736(20)30460-8
12. Wang M, Zhu X, Li L. Construction and application of a risk prediction model for impulsive behavior in hospitalized schizophrenia. J Clin Psychiatry. 2023;33(02):133–136.
13. Wang X, Gao L, Shi L. Construction and evaluation of a suicide risk prediction model in patients with schizophrenia. J Psychiatry. 2023;36(02):123–127.
14. Fazel S, Wolf A, Larsson H, et al. The prediction of suicide in severe mental illness: development and validation of a clinical prediction rule (OxMIS). Transl Psychiatry. 2019;9(1):98. doi:10.1038/s41398-019-0428-3
15. Liu P. The ICD-10 Classification of Psychiatric and Behavioral Disorders. People’s Health Press; 1995.
16. Fusar-Poli P, Davies C, Rutigliano G, Stahl D, Bonoldi I, McGuire P. Transdiagnostic individualized clinically based risk calculator for the detection of individuals at risk and the prediction of psychosis: model refinement including nonlinear effects of age. Front Psychiatry. 2019;10:313. doi:10.3389/fpsyt.2019.00313
17. Zhang Mingyuan Y. A Brief Psychiatric Scale (BPRS). Shanghai Psychiatr Med. 1984;3:2.
18. Zhang M. The Psychiatric Rating Scale Manual. Hunan Science and Technology Press; 1998.
19. Zhou J, Wang Y. Evaluation and analysis of the anxiety and depression scale. Chin J Ment Health. 2006;20(10):1. doi:10.3321/j.issn:1000-6729.2006.10.011
20. Wittchen HU, Kessler RC, Brandenburg N. P.4.a.005 Should the duration requirement for generalized anxiety disorder be changed? - Evidence from the national comorbidity survey replication. Eur. Neuropsychopharmacol. 2006;16:S450. doi:10.1016/S0924-977X(06)70586-7
21. Ma S. Clinical Medical Psychology. The Science and Technology Press of China; 1999.
22. Feng X, Xin Y, Huiling S. Reliability and validity test of patient health questionnaire depression scale 9 in acne patients. Chin J Dermatol. 2019;52(7):461–466. doi:10.3760/cma.j.issn.0412-4030.2019.07.004
23. Maier W, Buller R, Philipp M, Heuser I. The Hamilton anxiety scale: reliability, validity and sensitivity to change in anxiety and depressive disorders. J Affect Disord. 1988;14(1):61–68. doi:10.1016/0165-0327(88)90072-9
24. Liu B. Study on the value of empathy intervention for anxiety and depression in children with autism. Psychol Month. 2021;16(4):115–116. doi:10.19738/j.cnki.psy.2021.04.054
25. Aledavood T, Torous J, Triana Hoyos AM, Naslund JA, Onnela JP, Keshavan M. Smartphone-based tracking of sleep in depression, anxiety, and psychotic disorders. Curr Psychiatry Rep. 2019;21(7):49. doi:10.1007/s11920-019-1043-y
26. Berlowitz DR, Foy CG, Kazis LE, Bolin L, Lonroy LB, Fitzpatrick P, et al. For the SPRINT Study Research Group. Impact of intensive blood pressure therapy on patient-reported outcomes: outcomes results from the SPRINT study. N Engl J Med 2017; 377:733–744
27. Bress AP, Bellows BK, King J, Beddhu HR, Zhang S, et al. For the SPRINT Research Group and the SPRINT Economics and Health Related Quality of Life Subcommittee. Cost- effectiveness of intensive versus standard blood pressure control. N Engl J Med 2017; 377:745–755.
28. Xiao water source. Theoretical basis and research application of the social support rating scale. J Clin Psychiatr Med. 1994;4(2):3.
29. Zhai Q, Hu C, Yang L. Study on the correlation between social support situation and mental disorders. J Capit Med Univ. 2018;39(5):5. doi:10.3969/j.issn.1006-7795.2018.05.005
30. Li Y. Credit validity analysis of firefighter applied social support rating scale. Chin J Health Psychol. 2017;25(9):4. doi:10.13342/j.cnki.cjhp.2017.09.018
31. Krupchanka D. Insight and schizophrenia; 2012.
32. Gao H, Yu X. Credit validity determination of the self-awareness and treatment attitude questionnaire. Chin J Ment Health. 1998;12(2):2.
33. Wang M, Yu R, Tang W. Study on risk factors for violent behavior in hospitalized schizophrenia. J Clin Psychiatr Med. 2022;32(06):476–478.
34. Yang K, Xiao S, Li X, Liao C, Dai J. Behavior of suicide during hospitalization in patients with schizophrenia. Ment Health Sichuan Province. 2015;28(05):430–435. doi:10.11886/j.issn.1007-3256.2015.05.014
35. Deng L, Huang J, Yang X. Study of external walking behavior in patients with mental illness. Chin Contempor Med. 2017;24(16):17–19+32.
36. Sun S. Analysis of risk factors for suicidal behavior in patients with depressive episodes of bipolar disorder. Chin Gener Med. 2022;20(08):1319–1322. doi:10.16766/j.cnki.issn.1674-4152.002586
37. Chen F, Dai Y, Zhu W. Analysis of risk factors for aggressive behavior in patients with bipolar disorder. J Clin Psychosom Dis. 2022;28(05):135–138.
38. Liu N, Zhang Y, Huang G. Progress in the behavioral genetics of violent aggression. Int J Psychiatr. 2009;36(1):3.
39. Liu C, Lu C, Zhang QQ, et al. Analysis of factors influencing high-risk behaviors in patients with severe mental disorders. Preventive Med. 2019;31(01):51–54+58. doi:10.19485/j.cnki.issn2096-5087.2019.01.012
40. Zheng F, Lin Y, Wei Q, Zeng Z, Xiong D, Wu S. A cross-sectional analysis of registry data of severe mental disorders in Fuzhou, China: current status and prospects. BMC Psychiatry. 2022;22(1):790. doi:10.1186/s12888-022-04364-6
41. Christensen MK, Lim CCW, Saha S, et al. The cost of mental disorders: a systematic review. Epidemiol Psychiatr Sci. 2020:
42. Zeng F, Liu P, Jiang P, et al. Investigation and analysis of The Guardian care burden of 1218 patients with severe mental disorders. Chin Nurs J. 2019;54(01):95–99. doi:10.3761/j.issn.0254-1769.2019.01.020
43. Vermeulen JM, van Rooijen G, van de Kerkhof MPJ, Sutterland AL, Correll CU, de Haan L. Clozapine and long-term mortality risk in patients with schizophrenia: a systematic review and meta-analysis of studies lasting 1.1-12.5 years. Schizophr Bull. 2019;45(2):315–329. doi:10.1093/schbul/sby052
44. Hjorthøj C, Stürup AE, McGrath JJ, Nordentoft M. Years of potential life lost and life expectancy in schizophrenia: a systematic review and meta-analysis. Lancet Psychiatry. 2017;4(4):295–301. doi:10.1016/S2215-0366(17)30078-0
45. Feng X. Status-Background-Assessment-Suggestions The impact of nursing communication patterns on the level of mania in patients with manic episodes of bipolar disorder. Shanxi Med J. 2022;51(3):354–356.
46. Stentzel U, van den Berg N, Schulze LN, et al. Predictors of medication adherence among patients with severe psychiatric disorders: findings from the baseline assessment of a randomized controlled trial(Tecla). BMC Psychiatry. 2018;18(1):155. doi:10.1186/s12888-018-1737-4
47. Chen Y, Feng H, Zhuang X, et al. Family burden of schizophrenia care and quality of life and its associated factors. Chin J Ment Health. 2017;31(3):203–207.
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.