Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 17
Bronchoscopic Treatment of Giant Emphysematous Bullae with Endobronchial Silicone Plugs
Authors Lin H, Zhang H, Yang D, Chen X, Chen Y, Song D, Cai C, Zeng Y
Received 15 April 2022
Accepted for publication 21 July 2022
Published 3 August 2022 Volume 2022:17 Pages 1743—1750
DOI https://doi.org/10.2147/COPD.S369803
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Richard Russell
Huihuang Lin,1,* Huaping Zhang,1,* Dongyong Yang,1,* Xiaoyang Chen,1,* Yunfeng Chen,1,* Duanhong Song,1 Chi Cai,2 Yiming Zeng1
1Department of Pulmonary and Critical Care Medicine, the Second Affiliated Hospital of Fujian Medical University, Center of Respiratory Medicine of Fujian Province, Quanzhou, People’s Republic of China; 2Department of Radiology, the Second Affiliated Hospital of Fujian Medical University, Quanzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yiming Zeng, Department of Pulmonary and Critical Care Medicine, the Second Affiliated Hospital of Fujian Medical University, Center of Respiratory Medicine of Fujian Province, No. 34, Zhongshanbei Road, Licheng District, Quanzhou, People’s Republic of China, Tel +86 13515042402, Fax +86 0595 22770258, Email [email protected]
Purpose: Surgical bullectomy is the standard treatment of giant emphysematous bulla (GEB). However, bronchoscopic treatment should be considered as an alternative approach for patients who are unfit for surgical treatment. The study aimed to evaluate the clinical efficacy of endobronchial occlusion for the treatment of GEB using silicone plugs.
Methods: This retrospective study recruited four patients with GEB who were unsuitable for surgery. Preoperative planning was performed using high-resolution computed tomography and a virtual bronchoscopic navigation system. Customized silicone plugs were then placed in the target airway via bronchoscopy to cause GEB regression and atelectasis.
Results: All procedures were completed successfully in four patients. Three months after the procedures, compared with baseline, increases in the mean forced expiratory volume in 1 s (from 1.20 L/s to 1.33 L/s), forced vital capacity (from 2.63 L to 2.90 L), diffusion lung capacity for carbon monoxide (from 29% to 41% of the predicted value) and 6-minute walking test (from 412 m to 474 m) were observed. Additionally, the mean total lung capacity (from 6.80 L to 6.35 L), residual volume (from 3.97 L to 3.52 L), and St. George’s Respiratory Questionnaire scores (from 67 to 45) were all lower than baseline data.
Conclusion: Our preliminary results demonstrated that the endobronchial placement of silicone plugs could be a low-cost, safe, and effective choice for the treatment of GEB in surgically unfit patients.
Keywords: giant bulla, bronchoscopy, silicone spigot, endobronchial occlusion
Introduction
Giant emphysematous bulla (GEB) is a large bulla occupying at least 30% of the hemithorax.1 GEB can compress adjacent normal parenchyma and impair gas exchange, resulting in dyspnea on exertion and, sometimes, pneumothorax.2 Surgical treatments, including bullectomy, lobectomy, and pneumonectomy, have been recommended as the standard approaches for eliminating giant bullae.3 However, when a patient refuses surgery or is not a suitable candidate for surgery, these forms of resection are inappropriate.
In recent years, several endoscopic methods have been used as safer and less invasive treatment options for GEB.4–9 Endobronchial valve (EBV) placement is currently the most commonly reported bronchoscopic approach for patients with GEB who are not suitable candidates for surgery. Although EBV placement has been proven to be effective and safe, some limitations should be noted. The most frequent complication associated with this technique is pneumothorax; the incidence of which ranged from 4% to 18%.10–12 Another study reported that >80% of the cases experienced pneumothorax within 2 days of EBV placement, due to the rapid re-expansion of the compressed adjacent lung.13 EBV-related pneumothorax might be fatal in patients with advanced emphysema and limited pulmonary reserve.14 The cost of EBV is another factor that needs to be considered. A previous study reported that for each patient with GEB, an average of three valves are required for placement into a target bronchus.5 The average cost of this treatment in China is approximately US$ 15,000. Occasionally (10% of cases), the EBVs are removed due to pneumothorax, cough, or valve migration.15 Therefore, the cost of the procedure could be a significant burden for some patients, especially in developing countries.
Rarely, GEB resolves spontaneously following infection.16–18 The closure of communication between bullae and airway after airway inflammation might result in a closed space, and the absorption of air within the bullae can cause shrinkage of the GEB over time. Based on spontaneous GEB regression, we hypothesized that an endobronchial plug could be used for the treatment of GEB. The endobronchial Watanabe spigot (EWS) is a commercial product in Japan and has been used as an occluder device in the endobronchial treatment of persistent bronchial fistula and pulmonary air leaks,19–21 whereas the placement of endobronchial silicon plugs for the treatment of GEB has not been tested.
Since EWS is not available in China, we designed a conical silicone spigot as an alternate blocker for bronchoscopic treatment in patients with GEB. In this study, we evaluated the efficacy of customized silicone plugs as bronchoscopic occluders in deflating the giant bullae in surgically unfit patients with GEB.
Methods
Study Design
This was a retrospective study that aimed to evaluate the clinical efficacy of endoscopic silicon plug occlusion treatment in patients with GEB at the Second Affiliated Hospital of Fujian Medical University. The research ethics board of the hospital approved this study, and all patients were aware of the treatment plans and provided written informed consent.
Study Population
Four male patients with a mean age of 61 years were enrolled in this study. The clinical characteristics of these patients at baseline are shown in Table 1.
 |
Table 1 Clinical Evaluation Outcomes at Baseline and 3 Months After Endobronchial Occlusion Using the Silicone Plugs |
All patients had been diagnosed with chronic obstructive pulmonary disease (COPD) groups C or D and had worsening airflow limitation. Each patient had experienced a pneumothorax on more than two occasions. In all cases, the GEB occupied more than one-third of the hemithorax.
Due to progressively increasing dyspnea at exertion and recurrent history of pneumothorax, the patients were admitted to our hospital for the treatment of GEB. Following a multidisciplinary team discussion, we decided that surgical bullectomy was unsuitable due to the severe reduction of diffusion lung capacity (in each patient, this was <35% of the predicted value). Additionally, all patients were reluctant to accept the risk of the surgical procedure and, therefore, selected bronchoscopic treatment. Furthermore, considering the cost of EBV, the patients refused the endoscopic placement of EBV. Therefore, each patient underwent the bronchoscopic placement of customized silicon plugs to treat GEB.
Clinical Evaluation
Clinical evaluation included the pulmonary function test, 6-minute walking test (6MWT), and St. George’s Respiratory Questionnaire (SGRQ). We performed chest high-resolution computed tomography (HRCT) on each patient and paid particular attention to confirming complete or near-complete (>90%) interlobular fissures (as a surrogate for the absence of collateral ventilation) in the target lobe site of GEB. During the treatment and follow-up, we documented all symptoms, including temperature, breathing, and cough. If necessary, a review bronchoscopy was performed to assess the location of spigots. In addition to preoperative function evaluation at baseline, the same examinations were repeated 3 months after the procedure.
Occluder Device Description
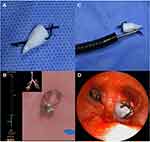
The bronchial silicone plug used in this study was obtained from a silicone implant (Kangning Medical Device, Shanghai, China). The material was trimmed into a cone-shaped silicone spigot of an appropriate size to occlude the target bronchus. To grasp the blocker efficiently with the grasping forceps, we tied a string of knots (1 cm in length) using 0# surgical sutures in the tip of the conical silicone spigot. At the bottom of the occluder, we tied a second knot to remove the silicone spigot, if the patient could not tolerate the spigot (Figure 1A).
Operative Procedure
Before the bronchoscopic procedures, the location of the GEB was identified using HRCT and a virtual bronchoscopic navigation (VBN) system (LungPro®, Broncus, USA). In addition to assisting in determining the bronchoscopic route, the three-dimensional VBN system could help evaluate the diameter of the bronchus of the target lobe to facilitate trimming of the silicone plug (Figure 1B). Placement of the silicone spigot could be performed under local or general anesthesia. Briefly, a grasping forceps (FB-35C-1, Olympus, Japan) was introduced through the 2.8-mm diameter working channel of a flexible bronchoscope (BF1T-260, Olympus, Japan). The silicone plug was then grasped using the grasping forces (Figure 1C) and inserted into the target bronchus by adjusting the direction and angle. Spigots were placed in the target bronchus that corresponded to the GEB based on individual anatomy (Figure 1D).
Results
Intraoperative results
The procedures were completed successfully and well tolerated in all four patients. GEB was located in the right upper lobe in two cases, in the right middle lobe in one case, and left lower lobe in one case. A median of two silicone spigots (range, 1–3 spigots) were placed to occlude the entire lobe in each patient with complete fissure, with a median procedural time of 16 minutes (range, 5–30 minutes). The median postoperative hospital stay was 3 days (range, 1–7 days).
Functional Results
The functional results are listed in Table 1 and Figure 2. Three months after the procedure, compared with baseline, increases in the mean forced expiratory volume in 1 s (FEV1) (from 1.20 L/s to 1.33 L/s), forced vital capacity (FVC) (from 2.63 L to 2.90 L), diffusion lung capacity for carbon monoxide (DLCO) (from 29% to 41% of the predicted value), and 6MWT (from 412 m to 474 m) were observed. The mean total lung capacity (TLC) (from 6.80 L to 6.35 L) and residual volume (RV) (from 3.97 L to 3.52 L) were lower than those measured at baseline.
Chest Imaging
Chest CT was performed at baseline and 3 months after treatment. The repeated CT findings showed different degrees of bulla atelectasis with re-expansion of the adjacent lung in all four patients. For GEB located near the diaphragm, the reduction in hyperinflation of GEB restored the diaphragm to a more domed physiological configuration. Representative CT images are shown in Figures 3 and 4.
Quality of Life
During the follow-up period, each patient reported that their symptoms of exertional dyspnea had improved. Additionally, improvements were evident in SGRQ scores (Figure 2), with a 22-point greater reduction at 3 months after silicone plug treatment than at baseline (from 67 to 45).
Complications
On the second day after the procedure, one patient experienced an infective acute exacerbation of COPD. This was fully resolved following the administration of an appropriate antibiotic (fluoroquinolone) and prednisolone. The other three patients did not experience any adverse events following the placement of the spigots.
Discussion
A bulla is defined as an airspace measuring >1 cm in diameter in the lung.22 Generally, a small bulla only needs clinical follow-up. However, over time, the bulla may increase in size to become more than one-third of the hemithorax, resulting in an impairment of lung function with associated worsening dyspnea, exercise limitation, and recurrent pneumothorax. Pharmacological treatment is not effective for patients with GEB, and surgery is regarded as the preferred option, with significant improvement in lung function and exercise capacity.23,24 In addition to an FEV1 <50% of the predicted value, the physiological parameters that were predictive for selecting patients with GEB with beneficial results after surgery included eucapnia and a normal DLCO.25 However, patients who undergo resection of GEB may suffer postoperative complications, including prolonged air leaks, pneumonia, atrial fibrillation, and massive subcutaneous emphysema,24 which are considered to be high risk in the compromised patients.
In our study, all four patients with GEB experienced pneumothorax on more than two occasions with poor quality of life. Therefore, for all patients, GEB had to be treated. Two patients (Case 1 and Case 3) had greater FEV1 than half of the predicted value, and the DLCO of all patients was <35% of the predicted value. Therefore, surgical treatment was considered to be unsuitable.25,26 Additionally, these patients refused to undergo conventional surgery due to procedure-related mortality and morbidity. Based on these considerations, bronchoscopic treatment was regarded as an alternative approach.
Our customized endobronchial plug has the following features. (1) The material originates from facial silicone implants and has good biocompatibility. (2) The silicone spigot can be freely trimmed on-site into various sizes to suit the corresponding target bronchus. (3) The rough surface after trimming can fix the plugs into the bronchial tree. (4) The conical design allows us to adjust the direction and angle of the spigot into the distal airways. (5) With the two knots tied at the tip and bottom, the spigot can be easily guided into the appropriate position and removed as necessary through bronchoscopic grasping forceps. (6) The treatment is a cost-effective procedure, because the average cost per customized spigot is US$10; and (7) air absorption in a closed GEB is a slow process after the obliteration of communication. Hence, the lung volume will not “immediately” emerge as a rapid shift to cause pneumothorax.
By evaluating changes in pulmonary function before and 3 months after treatment in patients with GEB, we observed a significant increase in FEV1 and a significant reduction in TLC and RV. The improvements observed in these lung function parameters may be interpreted as a reduction in lung overinflation, re-expansion of the adjacent lung, and an upshift of the compressed diaphragm. Additionally, the pulmonary diffusion capacity improved significantly after treatment. This improvement may be associated with the reduction in both dead space and ventilation–perfusion mismatch. Correspondingly, the patients exhibited significant efficacy in exercise capacity and quality of life.
After the procedure, repeated chest CT scans indicated imaging changes in the GEB volume in all patients. Case 1 had noticeable atelectasis of the bulla on the seventh day after treatment (Figure 3A and B), whereas others showed radiological improvement until 3 months after the placement of endobronchial spigots. Coincidentally, Case 1 was the only one to experience an infectious complication. As outlined above, the placement of silicone plugs could isolate the bronchus that communicates with the GEB. Furthermore, obstructive airway inflammation after endobronchial treatment might favor the regression of the bulla. Notably, the silicone spigot-associated inflammation needs to be cured; if not, the plugs need to be removed.
None of the four patients developed pneumothorax after the procedure. The study further demonstrated that the technique was safe for the management of GEB with a slow reduction in lung volume following endobronchial occlusion of the entire lobe. To prevent the migration of plugs, the size of the spigot was designed to be slightly larger than the diameter of the airway. Due to the elasticity of the bronchial wall and silicone material, the plug could be tightly inserted into the target bronchus. Therefore, none of the spigots used in our study showed any evidence of migration.
The use of VBN was another advantage of the procedure. Locating the giant bulla was a challenge for endobronchial occlusion treatment in patients with GEB, and the bronchial tree may be transposed to a different location due to the compression of the GEB. The operator may misjudge the target lobe based solely on HRCT findings. VBN can help to accurately determine the location of the GEB and automatically plan the appropriate path to the target lobe, especially when location of GEB is difficult depending on the HRCT. Therefore, VBN can assist and improve the efficiency of this procedure.
Conclusion
Our preliminary results demonstrated that the bronchoscopic placement of silicone plugs in the treatment of GEB was feasible and associated with improvements in lung function, exercise capacity, and quality of life. This technique may be considered as a safe, effective, and low-cost alternative for surgically unfit patients with GEB. In the future, a prospective clinical trial with a larger population size and long-term follow-up will be required to confirm the safety and efficacy of this technique.
Ethics Approval and Informed Consent
The study was performed in accordance with the principles stated in the declaration of Helsinki and approved by the Second Affiliated Hospital of Fujian Medical University Ethics Committee (number FYFE2021-51). The authors confirm that all participants provide written informed consent and give their consents for images and all other clinical information to be published.
Acknowledgments
We gratefully acknowledge the support of patients who were involved in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Meyers BF, Patterson GA. Chronic obstructive pulmonary disease. 10: bullectomy, lung volume reduction surgery, and transplantation for patients with chronic obstructive pulmonary disease. Thorax. 2003;58(7):634–638. doi:10.1136/thorax.58.7.634
2. Greenberg JA, Singhal S, Kaiser LR. Giant bullous lung disease: evaluation, selection, techniques, and outcomes. Chest Surg Clin N Am. 2003;13(4):631–649. doi:10.1016/S1052-3359(03)00095-4
3. Nickoladze GD. Functional results of surgery for bullous emphysema. Chest. 1992;101(1):119–122. doi:10.1378/chest.101.1.119
4. Noppen M, Tellings JC, Dekeukeleire T, et al. Successful treatment of a giant emphysematous bulla by bronchoscopic placement of endobronchial valves. Chest. 2006;130(5):1563–1565. doi:10.1378/chest.130.5.1563
5. Mario S, Alfonso F, Giovanni V, Di CVG, Gaetana M, Paolo L. Endobronchial treatment of giant emphysematous bullae with one-way valves: a new approach for surgically unfit patients. Eur J Cardiothorac Surg. 2011;40(6):1425–1431. doi:10.1016/j.ejcts.2011.03.046
6. Tian Q, An Y, Xiao BB, Chen LA. Treatment of giant emphysematous bulla with endobronchial valves in patients with chronic obstructive pulmonary disease: a case series. J Thorac Dis. 2014;6(12):1674–1680. doi:10.3978/j.issn.2072-1439.2014.11.07
7. Zoumot Z, Kemp SV, Caneja C, Singh S, Shah PL. Bronchoscopic intrabullous autologous blood instillation: a novel approach for the treatment of giant bullae. Ann Thorac Surg. 2013;96(4):1488–1491. doi:10.1016/j.athoracsur.2013.03.108
8. Hetzel J, Boeckeler M, Lewis RA, Horger M, Haentschel M. Use of 3-D navigation to target the site of autologous blood installation for lung volume reduction in bullous emphysema. Chron Resp Dis. 2020;17:1479973120903556. doi:10.1177/1479973120903556
9. Bhattacharyya P, Sarkar D, Nag S, Ghosh S, Roychoudhury S. Transbronchial decompression of emphysematous bullae: a new therapeutic approach. Eur Respir J. 2007;29(5):1003–1006. doi:10.1183/09031936.00030106
10. Klooster K, ten Hacken NH, Hartman JE, Kerstjens HA, van Rikxoort EM, Slebos DJ. Endobronchial valves for emphysema without interlobar collateral ventilation. N Engl J Med. 2015;373(24):2325–2335. doi:10.1056/NEJMoa1507807
11. Sciurba FC, Ernst A, Herth FJ, et al. A randomized study of endobronchial valves for advanced emphysema. N Engl J Med. 2010;363(13):1233–1244. doi:10.1056/NEJMoa0900928
12. Herth FJ, Eberhardt R, Gompelmann D, et al. Radiological and clinical outcomes of using Chartis to plan endobronchial valve treatment. Eur Respir J. 2013;41(2):302–308. doi:10.1183/09031936.00015312
13. Skowasch D, Fertl A, Schwick B, et al. A long-term follow-up investigation of endobronchial valves in emphysema (the LIVE study): study protocol and six-month interim analysis results of a prospective five-year observational study. Respiration. 2016;92(2):118–126. doi:10.1159/000448119
14. Zoumot Z, Davey C, Jordan S, et al. Endobronchial valves for patients with heterogeneous emphysema and without interlobar collateral ventilation: open label treatment following the BeLieVeR-HIFi study. Thorax. 2017;72(3):277–279. doi:10.1136/thoraxjnl-2016-208865
15. Gompelmann D, Gerovasili V, Kontogianni K, et al. Endoscopic valve removal >180 days since implantation in patients with severe emphysema. Respiration. 2018;96(4):348–354. doi:10.1159/000489887
16. Wahbi ZK, Arnold AG. Spontaneous closure of a large emphysematous bulla. Respir Med. 1995;89(5):377–379. doi:10.1016/0954-6111(95)90012-8
17. Bradshaw DA, Murray KM, Amundson DE. Spontaneous regression of a giant pulmonary bulla. Thorax. 1996;51(5):549–550. doi:10.1136/thx.51.5.549
18. Scarlata S, Cesari M, Caridi I, Chiurco D, Antonelli-Incalzi R. Spontaneous resolution of a giant pulmonary bulla in an older woman: role of functional assessment. Respiration. 2011;81(1):59–62. doi:10.1159/000317334
19. Watanabe Y, Matsuo K, Tamaoki A, Komoto R, Hiraki S. Bronchial occlusion with endobronchial Watanabe spigot. J Bronchology Interv Pulmonol. 2003;10(4):264–267.
20. Sasada S, Tamura K, Chang YS, et al. Clinical evaluation of endoscopic bronchial occlusion with silicone spigots for the management of persistent pulmonary air leaks. Intern Med. 2011;50(11):1169–1173. doi:10.2169/internalmedicine.50.5016
21. Levent D, Filizs K, Emel E, Levent K, Sedat A. Endobronchial Watanabe spigot embolisation in the treatment of bronchopleural fistula due to tuberculous empyema in intensive care unit. Ann Thorac Cardiovasc Surg. 2013;19(2):140–143. doi:10.5761/atcs.cr.11.01760
22. Report CGS. Terminology, definition, and classification of chronic pulmonary emphysema and related conditions. Thorax. 1959;14(4):286–299. doi:10.1136/thx.14.4.286
23. Palla A, Desideri M, Rossi G, et al. Elective surgery for giant bullous emphysema: a 5-year clinical and functional follow-up. Chest. 2005;128(4):2043–2050. doi:10.1378/chest.128.4.2043
24. Schipper PH, Meyers BF, Battafarano RJ, Guthrie TJ, Patterson GA, Cooper JD. Outcomes after resection of giant emphysematous bullae. Ann Thorac Surg. 2004;78(3):976–982. doi:10.1016/j.athoracsur.2004.04.005
25. Snider GL. Reduction pneumoplasty for giant bullous emphysema. Implications for surgical treatment of nonbullous emphysema. Chest. 1996;109(2):540–548. doi:10.1378/chest.109.2.540
26. Nakahara K, Nakaoka K, Ohno K, et al. Functional indications for bullectomy of giant bulla. Ann Thorac Surg. 1983;35(5):480–487. doi:10.1016/S0003-4975(10)60419-5
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.