Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 11 » Issue 1
Bronchodilator response of advanced lung function parameters depending on COPD severity
Authors Jarenbäck L , Eriksson G , Peterson S, Ankerst J, Bjermer L , Tufvesson E
Received 28 April 2016
Accepted for publication 20 September 2016
Published 25 November 2016 Volume 2016:11(1) Pages 2939—2950
DOI https://doi.org/10.2147/COPD.S111573
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Richard Russell
Linnea Jarenbäck,1 Göran Eriksson,1 Stefan Peterson,2 Jaro Ankerst,1 Leif Bjermer,1 Ellen Tufvesson1
1Respiratory Medicine and Allergology, Department of Clinical Sciences Lund, Lund University, 2Regional Cancer Center South, Skåne University Hospital, Lund, Sweden
Background: COPD is defined as partly irreversible airflow obstruction. The response pattern of bronchodilators has not been followed in advanced lung function parameters.
Purpose: The aim of this study was to investigate bronchodilator response pattern in advanced lung function parameters in a continuous fashion along forced expiratory volume in 1 second (FEV1) percent predicted (%p) in COPD patients and controls.
Patients and methods: Eighty-one smokers/ex-smokers (41 controls and 40 COPD) performed spirometry, body plethysmography, impulse oscillometry and single-breath helium dilution carbon monoxide diffusion at baseline, after salbutamol inhalation and then after an additional inhalation of ipratropium.
Results: Most pulmonary function parameters showed a linear increase in response to decreased FEV1%p. The subjects were divided into groups of FEV1%p <65 and >65, and the findings from continuous analysis were verified. The exceptions to this linear response were inspiratory capacity (IC), forced vital capacity (FVC), FEV1/FVC and expiratory resistance (Rex), which showed a segmented response relationship to FEV1%p. IC and FVC, with break points (BP) of 57 and 58 FEV1%p respectively, showed no response above, but an incresed slope below the BP. In addition, in patients with FEV1%p <65 and >65, response of FEV1%p did not correlate to response of volume parameters.
Conclusion: Response of several advanced lung function parameters differs depending on patients’ baseline FEV1%p, and specifically response of volume parameters is most pronounced in COPD patients with FEV1%p <65. Volume and resistance responses do not follow the flow response measured with FEV1 and may thus be used as a complement to FEV1 reversibility to identify flow, volume and resistance responders.
Keywords: COPD, IOS, body plethysmography, bronchodilation, lung function, reversibility
Introduction
COPD is one of the world’s leading causes of death and is defined to have a progressive, partly irreversible airflow limitation due to a chronic inflammation in the airways. It is heterogenic in nature with varying degrees of emphysema and chronic bronchitis. COPD is diagnosed in patients using anamnesis and spirometry, but it is known that flow–volume spirometry mainly measures alterations in the central airways. Recently, it has been observed that destruction in the peripheral airways is present prior to changes observed by spirometry,1 and methods to measure the peripheral airway changes are necessary. We have previously shown that baseline impulse oscillometry (IOS) parameters seem to be more affected in moderate-to-severe COPD patients, while volume and diffusion parameters are more affected in severe and very severe COPD patients. In addition, we showed that the lung function parameters are widely spread in Global Initiative for chronic Obstructive Lung Disease (GOLD) stage 2.2 Post hoc investigations of this study identified break points (BPs) in the linear relationship between forced expiratory volume in 1 second (FEV1) percent predicted (%p) and advanced lung function parameters, identifying a change in the lung function pattern when FEV1%p drops below 65.3 However, how these patterns change due to bronchodilators is not known. The topic of whether the bronchodilator response in FEV1 is limited in COPD patients has been discussed,4 and studies have explored the reversibility of FEV1, forced vital capacity (FVC) and FEV1/FVC based on disease stage (based on GOLD stages).5,6 Other studies suggest that the reversibility of FEV1 is not a useful tool in COPD and that there might be many other relevant parameters when evaluating the response.4 In some studies, other advanced lung function parameters are used to evaluate the response,7–13 but there is no information about the clinically significant response and the parameters that are most effective to use. The use of volume parameters for assessing bronchodilator response in patients with hyperinflation has shown that bronchodilation decreases hyperinflation.14 The response of parameters of forced oscillometry (FOT) after salbutamol has recently been described in different GOLD stages. These data showed a significant response in milder stage of COPD compared to controls with a tendency of lower response in more advanced stage.15 However, the bronchodilator response of parameters measured by the closely related IOS method and volume parameters measured by body plethysmography in correlation to other parameters has not been investigated in relation to COPD disease severity based on FEV1%p.
We aimed to investigate the response of advanced lung function parameters, beyond FEV1, to short-acting bronchodilators in a continuous fashion over a broad range of FEV1%p. Hence, we identified the relevant parameters that are most important when assessing bronchodilator response and at which disease severity patients benefit most from the treatment.
Patients and methods
Study participants
A total of 81 volunteers (smokers and ex-smokers) were included in the study (Table 1) and were classified as controls (fixed ratio FEV1/FVC >0.7; n=41) or COPD patients (FEV1/FVC <0.7; n=40). After the continuous analysis, subjects were also divided into FEV1%p <65 and >65 (independent of FEV1/FVC) to assess subjects at different disease stages. This division was based on our previous study that indicates that the disease patterns change around FEV1%p of 65%p.3 All study participants refrained from their inhaled bronchodilators 8 hours (short-acting β2 agonist [SABA] or short-acting muscarinic antagonist [SAMA]) and 48 hours (long-acting β2 agonist [LABA] or long-acting muscarinic antagonist [LAMA]), respectively, before the visit. All participants had ≥10 pack-years and had no previous diagnoses of asthma or any other pulmonary disease (except COPD) or any lower respiratory infection/exacerbation within the last 3 weeks.
Study design
Study participants performed IOS (MasterScreen, Erich Jaeger GmbH, Würzburg, Germany) giving information about total airway resistance (R5), central airway resistance (R20), peripheral airway resistance (R5–R20), reactance at 5 Hz (X5), reactance area (AX) and resonance frequency (Fres).16 Body plethysmography with spirometry (MasterScreen Body, Erich Jaeger GmbH)17 provided information about flow and volume parameters, FEV1, FVC, FEV1/FVC, functional residual capacity (FRC), residual volume (RV), inspiratory capacity (IC) and total lung capacity (TLC), and resistance, including inspiratory resistance (Rin) and expiratory resistance (Rex). Single-breath helium dilution carbon monoxide diffusion (MasterScreen Diffusion, Erich Jaeger GmbH)18–20 was performed to obtain diffusion capacity of the lung for carbon monoxide (DL,CO), alveolar volume (VA), DL,CO/VA, RV, FRC and TLC. These measurements were performed at baseline, 10 minutes after inhalation of SABA (400 μg salbutamol; Buventol®, Easyhaler®) and then again 40 minutes after inhalation of additional SAMA (80 μg ipratropium; Atrovent®, Handihaler®) (Figure 1). Lung function measurements were performed according to manufacturer’s instructions and European Respiratory Society/American Thorax Society recommendations.19,21,22 The reference values used were established by Crapo et al23 (spirometry), Quanjer et al24 (body plethysmography and single breath) and Vogel25 (IOS). Study participants also filled the Clinical COPD Questionnaire.
  | Figure 1 Flowchart of the study design. |
This study was approved by the Regional Ethical Review Board in Lund (431/2008) and followed the guidelines set in the Declaration of Helsinki, and all study participants signed the informed consent.
Statistics
To detect BPs, a regression model allowing segmented relationships was performed as previously described.3 Shortly, this method estimates a new model having a segmented relationship from an existing linear regression (LR) model.3 Ordinary LR and a nonparametric fit by the loess (local regression) line are also used for visual purpose.26–28
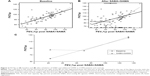
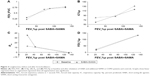
Figure 2A and B shows the FVC%p at baseline and after inhalation of SABA and additional SAMA, respectively, in relation to post-bronchodilator FEV1%p. The light gray line shows the smooth loess; the straight line the LR; and the broken line, where half the line is dotted, is the segmented linear regression (SLR). The dot in Figure 2B shows where the BP is with 95% confidence interval. BP is given as FEV1%p. The estimated LR (Figure 2A) or SLR (if significant over LR; Figure 2B) of each graph is then plotted into one graph to visualize the lung function before and after SABA+SAMA (Figure 2C), which shows a shift of the curves. This method is also applied in graphs in Figure 3A–D. LR and SLR were also investigated in the absolute response in Figure 4A–D.
All responses shown in Tables 2–4 and S1 are displayed as absolute response (Δ)29 and with parameters expressed as %p when possible.
Normally distributed (FEV1, FVC, FVC%p and IC%p) paired data were analyzed using analysis of variance with Bonferroni’s multiple comparison test, and uneven distributed paired data were analyzed using Friedman test with Dunn’s multiple comparison test. Normally distributed unpaired data were analyzed using Unpaired students t-test, and uneven distributed unpaired data were analyzed using Mann–Whitney U test. Data are presented as median with interquartile range. A P-value <0.05 was considered significant. Statistical calculations were performed in R or GraphPad Prism (version 5).
Results
Continuous analysis of lung function at baseline and after inhalation of SABA with additional SAMA
Most of the parameters that show linearity or segmented linearity at baseline maintain this pattern even after inhalation of SABA with additional SAMA, except FVC%p (Figure 2), FEV1/FVC (Figure 3A), IC%p (Figure 3B) and Rex (Figure 3C).
FVC%p and IC%p change from favoring linear relationship at baseline to segmented relationship after inhalation of SABA+SAMA, while Rex changes from being segmented at baseline to linear after inhalation of SABA+SAMA. FEV1/FVC shows BPs at both tests, but the BP is much lower after inhalation of SABA+SAMA.
Continuous analysis of absolute response to SABA with additional SAMA
The bronchodilator response to SABA+SAMA was analyzed for LR and SLR, and the following parameters showed a significant SLR (BP within parenthesis; Figure 4; Table 2), ie, the same parameters change their pattern as described earlier (Figure 3): ΔFVC%p (58%; Figure 4A), ΔFEV1/FVC (52%; Figure 4B), ΔIC% (57%; Figure 4C) and ΔRex (44%; Figure 4D).
All the four parameters showed a significant slope at the left side of the BP (= at low FEV1%p), while the slope to the right (= at high FEV1%p) was not significant (Table 2).
The following parameters showed a significant LR slope when the response was linearly increasing to a decrease in FEV1%p (Table 2): ΔRV%p, ΔFRC%p, ΔRin, ΔRtot%p, ΔDL,CO%p, ΔR5%p, ΔR5–R20%p and ΔAX.
The remaining parameters showed no significant LR slope or SLR (Table 2), but ΔFEV1%p, ΔX5%p and ΔDL,CO/VA%p showed significant intercepts, indicating a similar response over the severity range. ΔTLC%p, ΔR20%p and ΔVA%p showed no significant slope or intercept, indicating an insignificant response over the severity range.
Response to SABA with additional SAMA in subjects with FEV1%p <65 or >65
In our previous study,3 several parameters had BPs around FEV1 65%p. A related pattern is shown in this study, investigating the continuous relationship between the bronchodilator response and FEV1%p. To investigate the potential difference in the bronchodilator response (compared to baseline) of the different lung function parameters, the subjects were therefore further divided into groups of FEV1%p <65 and >65 (Tables 1 and 3).
Some of the lung volume parameters showed a significant bronchodilator response only in patients with FEV1%p <65 (Table 3): RV%p and FVC%p.
Other lung function parameters showed a significant bronchodilator response in both the groups (FEV1%p <65 and >65) (Table 3): FEV1%p, FRC%p, IC%p, FEV1, R5%p, R5–R20%p, X5%p, AX, Fres, Rin, Rex and Rtot%p.
All the above parameters showed a significantly higher bronchodilator response for the group below FEV1%p <65, except: FEV1, IC%p, R20%p and Fres.
The remaining parameters showed no response to the bronchodilator (or very little; data not shown): TLC%p, DL,CO%p, VA%p and DL,CO/VA%p.
Correlation between response in flow, volume, resistance and reactance parameters to SABA with additional SAMA
The correlations between ΔFEV1%p (flow), ΔFVC%p (flow volume), ΔRV%p (volume), ΔRtot%p (resistance), R5–R20%p (peripheral resistance) and ΔAX (reactance) were investigated to define the relationship within the response of different lung function parameters. In subjects with FEV1%p <65, ΔFEV1%p correlated only with ΔFVC%p, while ΔFVC%p, ΔRV%p, ΔRtot%p and ΔAX correlated with most of each other (Table 4). In contrast, in subjects with FEV1%p >65, ΔFEV1%p correlated with ΔFVC%p, ΔR5–R20%p and ΔAX, while no correlations were found among ΔFVC%p, ΔRV%p, ΔRtot%p and ΔAX (Table 4).
Response in volume, resistance and reactance correlated with each other but not with FEV1%p. To visualize the relationships and the individual responses, ΔRV%p was plotted against ΔFEV1%p (Figure 5). Some patients were both flow and volume responders, while some were either flow or volume responders, but no clear grouping could be demonstrated. Flow responders were defined as having a response in FEV1%p above the median response in this cohort, while volume responders were defined as having a response in RV%p above the median response in this cohort. With this definition, 18 subjects (11 controls and 7 COPD) were classified as neither flow nor volume responders (nonresponders in Figure 5).
Analysis of response to only SABA
All patients were also tested for the response to only SABA. A similar pattern was seen for the “continuous analysis of lung function at baseline and after inhalation of SABA” and for the “continuous analysis of absolute response to SABA” (Table S1) as for the double bronchodilators. Although FEV1/FVC did not show any response, DL,CO%p and R5%p did not have a significant slope, while R20%p did have. For “response to SABA in subjects with FEV1%p <65 or >65”, there seemed to be less effect of only SABA on several parameters compared to SABA+SAMA (Table S2). When looking at the “correlations between flow/volume/resistance/reactance response to SABA”, a similar pattern was observed for SABA+SAMA with few correlations to ΔFEV1 in the FEV1%p <65 group, but to all except volume in the FEV1%p >65 group (Table S3).
Discussion
In this study, we found that several volume and resistance parameters (measured by body plethysmography and IOS) differ from the response pattern seen in FEV1%p. We found that parameters reflecting volume response were more prominent in patients with more severe stage of COPD, while resistance parameters were more significant in less advanced stage. Most of the resistance and reactance parameters from IOS and body plethysmography responded to SABA, while the volume parameters were affected only mainly in patients with FEV1%p <65 or in patients who needed not only SABA but also the addition of SAMA to gain a significant effect.
The overall clinical aim in COPD should be to improve function in the small peripheral airways both by improving flow and by decreasing the degree of alveolar hypoventilation (flow responders) as well as decreasing air trapping and hyperinflation (volume responders). The degree of air trapping relates to the degree of dyspnea and the functional aspects, including BODE index as a composite score.30 In order to evaluate the effect of bronchodilators, it is thus important to go beyond the information provided by FEV1, mainly reflecting flow resistance in the central airways.4 These results indicate that the use of FEV1%p as a tool to investigate the effect of bronchodilators is not representative of the changes occurring in the respiratory system. Also, the bronchodilator response of many parameters, such as RV and Rtot, tends to be greater in patients with more severe disease (lower FEV1%p) and not correlating to the FEV1%p response. The addition of SAMA to SABA seems to be most effective in more severe patients whose volume parameters are affected, although data show that the combination of therapies can be beneficial to patients already in an early stage.
Regarding the response of IOS parameters, most of the parameters showed a better response with more severe disease, as previously stated. This is almost in accordance with the findings of da Costa et al15 regarding bronchodilator response using FOT, since we had more patients with milder disease.
Response to SABA was 1.4%–4% (40–120 mL), which is very low compared to the clinically relevant response.31 Additional inhalation of SAMA increased the response, especially in patients with FEV1%p <65, to 6% (210 mL). The continuous analysis did not detect higher response in more severe patients (nonsignificant slope), but the intercept was significant and thereby in accordance with the response analysis. Calverley et al4 questioned the clinical relevance of reversibility tests in COPD, which is in line with our SABA data, showing the importance of not only using double bronchodilators for optimal bronchodilation but also addition of other parameters measuring volume, resistance and reactance.
Only patients with lower FEV1%p (FEV1%p <65) showed a significant response in RV%p and FVC%p, and this improvement also differed significantly compared to subjects with FEV1%p >65. ΔFVC%p showed a significant SLR with BP at FEV1%p at 57, with no improvement in patients over this BP. This suggests that these improvements are a trait only in patients with more severe COPD and that there is no use in measuring at least FVC%p response over FEV1%p at 57. ΔRV%p showed a highly significant LR, crossing the X-axis around FEV1%p at 100%, implying that the response is very low in high FEV1%p but gradually increases as the disease progresses.
All parameters (except for Fres) that were significantly reversible in both groups to SABA and SABA+SAMA showed a significantly higher improvement in patients with more severe COPD. These data imply that the main effects of bronchodilators on lung function parameters other than FEV1%p are in the more severe group.
When the correlations and relationship of the difference in bronchodilator response were investigated, we observed a bronchodilator effect in the volume, resistance and reactance, beyond what can be measured with ΔFEV1%p. Data suggest that it might be beneficial to use RV%p in addition to FEV1%p when evaluating response to bronchodilators, since this parameter did not correlate with FEV1%p but with those of the peripheral airways (R5–R20%p, AX) in patients with FEV1%p <65. This also implies that there might be an importance in measuring the response but that more parameters should be evaluated to provide a fair picture of the response pattern. To visualize if a patient is a flow or a volume responder, the ratio of ΔRV%p/ΔFEV1%p may be used, since there seems to be patients being only flow responders, only volume responders, or both flow and volume responders. However, this method should be further verified to define a stable limit, dividing nonresponders from responders. Here, we used the median in the population. Another approach could be using zero response or a set limit (eg, what is clinical relevant). Further characterization of these patient subgroups in a clinical context would be of interest. This could also be applied to identify resistance and reactance parameters by using ΔAX/ΔFEV1%p and ΔRtot%p (or ΔR5–R20%p)/ΔFEV1%p, respectively.
Many lung function parameters did significantly improve, and many improvements were significantly better in the FEV1%p <65 group than in the subjects with FEV1%p >65, and this is supported by the fact that many parameters showed LR and SLR in the same direction. This also implies that the changes, even those in the peripheral airways, are only partially irreversible and that patients below the BP could benefit from bronchodilators even if they are not reversible in FEV1%p.
A limitation of this study is not only the number of patients but also the distribution of disease severity. Due to difficulties in performing all maneuvers repeatedly or difficulties refraining from medications, the population is a bit skewed toward the milder/moderate disease.
By identifying the parameters that show an effect in response to bronchodilators, it is possible to obtain a deeper understanding about what happens in the airways when bronchodilators are inhaled. By studying these parameters, it would be possible to measure the effectiveness of bronchodilators in different phenotypes/severities of COPD patients. A future perspective is to elucidate if these data hold true in a longitudinal study with long-acting bronchodilators to connect the effects in lung function parameters to those of clinical symptoms and dyspnea.
Conclusion
Some lung function parameters are significantly reversible along FEV1%p, while resistance and volume parameters show different response patterns along the FEV response curve. Measuring the response to resistance may be more informative in milder stages, while volume response parameters are more important in patients with lower FEV1%p. Thus, knowing that the bronchodilator effect in volume and resistance does not follow the FEV1%p response, those parameters should therefore be considered when characterizing patients according to bronchodilator response. This approach can help us in gaining insight into individualizing the diagnosis and therapy of COPD.
Acknowledgments
The authors would like to thank the staff at the Lung and Allergy Research Unit, Skåne, and also Dr Anders Olin for help and support. This work was supported by independent research grants from the Swedish Heart and Lung Foundation, Swedish Research Council, Evy and Gunnar Sandberg’s Foundation, Crafoord Foundation, and Royal Physiographic Society in Lund.
Disclosure
The authors report no conflicts of interest in this work.
References
Frantz S, Nihlen U, Dencker M, Engstrom G, Lofdahl CG, Wollmer P. Impulse oscillometry may be of value in detecting early manifestations of COPD. Respir Med. 2012;106(8):1116–1123. | ||
Jarenback L, Ankerst J, Bjermer L, Tufvesson E. Flow-volume parameters in COPD related to extended measurements of lung volume, diffusion, and resistance. Pulm Med. 2013;2013:782052. | ||
Eriksson G, Jarenbäck L, Peterson S, Ankerst J, Bjermer L, Tufvesson E. A new approach to assess COPD by identifying lung function break-points. Int J Chron Obstruct Pulmon Dis. 2015;10:2193–2202. | ||
Calverley PM, Albert P, Walker PP. Bronchodilator reversibility in chronic obstructive pulmonary disease: use and limitations. Lancet Respir Med. 2013;1(7):564–573. | ||
Albert P, Agusti A, Edwards L, et al. Bronchodilator responsiveness as a phenotypic characteristic of established chronic obstructive pulmonary disease. Thorax. 2012;67(8):701–708. | ||
Schermer T, Heijdra Y, Zadel S, et al. Flow and volume responses after routine salbutamol reversibility testing in mild to very severe COPD. Respir Med. 2007;101(6):1355–1362. | ||
Borrill ZL, Houghton CM, Woodcock AA, Vestbo J, Singh D. Measuring bronchodilation in COPD clinical trials. Br J Clin Pharmacol. 2005;59(4):379–384. | ||
Borrill ZL, Houghton CM, Tal-Singer R, et al. The use of plethysmography and oscillometry to compare long-acting bronchodilators in patients with COPD. Br J Clin Pharmacol. 2008;65(2):244–252. | ||
Zerah F, Lorino AM, Lorino H, Harf A, Macquin-Mavier I. Forced oscillation technique vs spirometry to assess bronchodilatation in patients with asthma and COPD. Chest. 1995;108(1):41–47. | ||
Timmins SC, Diba C, Schoeffel RE, Salome CM, King GG, Thamrin C. Changes in oscillatory impedance and nitrogen washout with combination fluticasone/salmeterol therapy in COPD. Respir Med. 2014;108(2):344–350. | ||
Abe T, Setoguchi Y, Kono Y, et al. Effects of inhaled tiotropium plus transdermal tulobuterol versus tiotropium alone on impulse oscillation system (IOS)-assessed measures of peripheral airway resistance and reactance, lung function and quality of life in patients with COPD: a randomized crossover study. Pulm Pharmacol Ther. 2011;24(5):617–624. | ||
Mineshita M, Shikama Y, Nakajima H, et al; COPD EXHALATION Investigators. The application of impulse oscillation system for the evaluation of treatment effects in patients with COPD. Respir Physiol Neurobiol. 2014;202:1–5. | ||
Sinojia R, Shaikh M, Kodgule R, et al. Priming of beta-2 agonist and antimuscarinic induced physiological responses induced by 1200mg/day NAC in moderate to severe COPD patients: a pilot study. Respir Physiol Neurobiol. 2014;191:52–59. | ||
Newton MF, O’Donnell DE, Forkert L. Response of lung volumes to inhaled salbutamol in a large population of patients with severe hyperinflation. Chest. 2002;121(4):1042–1050. | ||
da Costa GM, Faria AC, Di Mango AM, Lopes AJ, Lopes de Melo P. Respiratory impedance and response to salbutamol in healthy individuals and patients with COPD. Respiration. 2014;88(2):101–111. | ||
Oostveen E, MacLeod D, Lorino H, et al; ERS Task Force on Respiratory Impedance Measurements. The forced oscillation technique in clinical practice: methodology, recommendations and future developments. Eur Respir J. 2003;22(6):1026–1041. | ||
Goldman MD, Smith HJ, Ulmer WT. Whole-body plethysmography. Eur Respir Monogr. 2005;31:15–43. | ||
Hughes JMB. Pulmonary gas exchange. Eur Respir Monogr. 2005;31:106–126. | ||
Macintyre N, Crapo RO, Viegi G, et al. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J. 2005;26(4):720–735. | ||
Horstman M, Mertens F, Stam H. Transfer factor for carbon monoxide. Eur Respir Monogr. 2005;31:127–145. | ||
Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J. 2005;26(2):319–338. | ||
Wanger J, Clausen JL, Coates A, et al. Standardisation of the measurement of lung volumes. Eur Respir J. 2005;26(3):511–522. | ||
Crapo RO, Morris AH, Gardner RM. Reference spirometric values using techniques and equipment that meet ATS recommendations. Am Rev Respir Dis. 1981;123(6):659–664. | ||
Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC. Lung volumes and forced ventilatory flows. Report working party standardization of lung function tests, European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur Respir J Suppl. 1993;16:5–40. | ||
Vogel S. Implementation der Sollwertgleichungen für IOS. “Impuls-Oszillometrie” pmi-Verlag. 1994:S.148– S.152. German. | ||
Muggeo VM. Estimating regression models with unknown break-points. Stat Med. 2003;22(19):3055–3071. | ||
Muggeo VM. Segmented: an R package to fit regression models with broken-line relationships. R News. 2008;8/1:20–25. | ||
Cleveland WS, Grosse E, Shyu WM. Local regression models. In: Chambers SJM, Hastie TJ, editors. Statistical Models. Wadsworth & Brooks/Cole; 1992:309–376. | ||
Brand PL, Quanjer PH, Postma DS, et al. Interpretation of bronchodilator response in patients with obstructive airways disease. The Dutch Chronic Non-Specific Lung Disease (CNSLD) Study Group. Thorax. 1992;47(6):429–436. | ||
Lee YK, Oh Y, Lee J, et al; KOLD Study Group. Quantitative assessment of emphysema, air trapping, and airway thickening on computed tomography. Lung. 2008;186:157. | ||
Tan WC, Vollmer WM, Lamprecht B, et al. Worldwide patterns of bronchodilator responsiveness: results from the burden of obstructive lung disease study. Thorax. 2012;67(8):718–726. |
Supplementary materials
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.