Back to Journals » Infection and Drug Resistance » Volume 16
Bronchiolitis in Infants; Five Years’ Experience of a Teaching Hospital
Authors Alqahtani MH, Alqahtani MF , Asiri M, Alghamdi S, Alshagawi Z, Alzahrani S
Received 19 August 2022
Accepted for publication 16 August 2023
Published 28 August 2023 Volume 2023:16 Pages 5647—5664
DOI https://doi.org/10.2147/IDR.S385615
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Mohammad Hussain Alqahtani, Mohammad Faraj Alqahtani, Mohammed Asiri, Saad Alghamdi, Ziyad Alshagawi, Saleh Alzahrani
Pediatrics Department, Imam Abdulrahman Bin Faisal University King Fahd Hospital of the University, Al Khobar, Saudia Arabia
Correspondence: Mohammad Faraj Alqahtani, Pediatrics Department, Imam Abdulrahman Bin Faisal University King Fahd Hospital of the University, Al Khobar, Saudia Arabia, Tel +966508880030, Email [email protected]
Background: Bronchiolitis is a clinical syndrome affecting the lower respiratory tract of infants and toddlers < 2 years old. Variability in clinical profile and response to therapy in children with Bronchiolitis calls for studying the different clinical aspects of local patient population.
Aim: The goal of our study is to determine the clinical presentation, past medical history, hospitalization course and prognosis in children below two years of age who have been hospitalized in King Fahad University Hospital over the last five years.
Materials and Methods: A retrospective chart review based on electronic health records of all Bronchiolitis-related hospitalization of infants and toddlers below two years of age, covering the period between January 1, 2015, to April 26, 2020.
Results: Out of a total of 446 children < 2 years of age, 202 were female (45.4%), and 243 were male (54.6%). Although the length of hospital stay was almost equal between the sexes, there was a significant (p-value=0.01) increase in length of intensive care unit stay among females compared to males. Furthermore, there was a significant prolongation in the duration of ventilator usage among females (p value = 0.062). Out of fifty-five patients admitted to the ICU, 83.63% of them were 12 months of age and below.
Conclusion: Our results show a significant increase in length of ICU and ventilator use among females compared to males. It also shows that infants younger than 12 months account for most ICU admissions. These findings, among many others, may help pediatricians formulate a better diagnostic and therapeutic pathways.
Keywords: bronchiolitis, respiratory syncytial virus, RSV, lower respiratory tract infection
Introduction
Bronchiolitis is a broad term used to describes a spectrum of lower respiratory tract infections affecting the bronchioles. Bronchiolitis is a common cause of respiratory distress and a leading cause of hospitalization in infants and toddlers below two years of age.1 Bronchiolitis is characterized by upper respiratory symptoms (rhinorrhoea, reduced feeding, and low-grade fever) followed by lower respiratory infection and inflammation, which results in wheezing, crackles (rales), dyspnea, cough, and cyanosis once the infection spreads to the lower respiratory tract. However, the clinical presentation of Bronchiolitis is wildly varied. For example, apnea may be the only presenting symptom in certain patient populations, such as premature infants, infants younger than three months old and children with bronchopulmonary dysplasia.2 It is also essential to distinguish bronchiolitis from different conditions that may overlap with its clinical presentation, such as viral-triggered asthma, pneumonia, pertussis, congenital heart or pulmonary disease, foreign body aspiration and vascular ring.3 Although bronchiolitis can be associated with specific bacterial infections, it is typically caused by a viral aetiology; the most common cause is the respiratory syncytial virus.2 The management and prognosis of bronchiolitis are not divorced from its clinical context. Comorbidities, vaccination status, preterm birth, mode of birth, and causative agent can provide important insight into the treatment options and predict the disease’s progression. However, little data exist on the clinical profile of Saudi children with bronchiolitis. Studying different aspects of children with Bronchiolitis is of paramount importance to shedding light on the variability in clinical presentation and guiding better diagnostic and therapeutic decisions. Our goal is to provide a comprehensive data to aid in assessing discrepancies in presentation, clinical course, management, and outcomes in infants <2 years of age with bronchiolitis who have been admitted to the emergency room in King Fahad University Hospital in the last five years, which serves as a referral center for the eastern province in Saudi Arabia.
Methods
Ethics Statement
The study was reviewed and approved by the Institutional Review Board at Imam Abdulrahman bin Faisal University with IRB number (IRB-UGS-2020-01-292). We confirm that all data were obtained from a teaching hospital database and participants legal guardian consented for their data to be shared for teaching and research purposes. Also, we confirm that all data were retrieved anonymously, and the guidelines in the Declaration of Helsinki were followed.
Study Design
A retrospective study design was used. The recruited sample are all patients aged two years and below who were admitted to King Fahd Hospital of the University between 2015 and 2020 with the diagnosis of Bronchiolitis. The data were collected by reviewing the medical records of infants with bronchiolitis who were admitted to KFUH over the past five years.
Statistical Analysis
Using SPSS statistical analysis system, counts and percentages were used to summarize categorical variables. The mean ± standard deviation was used to summarize the distribution of continuous normal variables. The median and interquartile ranges were used for continuous non-normal variables. The Chi-square test of independence was used to assess the association between categorical variables. Unpaired t-test was used to compare the distribution of continuous variables between two groups, and one-way ANOVA was used in case of more than two groups. Hypothesis testing was performed at a 5% level of significance.
Results
A total of 445 patients were included in this retrospective study from the period of 2015 to 2020. However, due to data limitations, out of the 445 participants, only those who responded are analyzed in each section of the study.
The sample distribution is approximately equally distributed between males and females with slight male predominance (54.6% and 45.4%, respectively). The average age of the included respondents was 6.33 ± 5.24 months. The majority of the respondents presented during winter (66.5%, n = 296), and 18.2% presented during autumn (Figure 1). The remaining 11.5% and 3.82% were presented during spring and winter, respectively. Of the total population, preterm birth was reported in 9.21% (n = 41) (Table 1).
 |
Table 1 Demographic and Presentation Data of the Study Sample |
 |
Figure 1 Participant season of presentation. |
Out of 134 patients whose birth information were available, preterm birth was reported only in 30.6% (n = 41). In 180 participants for which the vaccination history was available, only 3.9% (n = 7) were not complaint to the immunization schedule. Out of 153 contributors, the family history of respiratory disease was reported in 32% (n = 49) of the patients and was absent in 68% (n = 104) (Table 1).
The most common comorbidity associated with bronchiolitis was reported to be bronchial asthma, which was present among 11.4% (n = 32) from 281 patients with available data. Followed by congenital anomalies, which was present in 10.8% (n = 32) out of 295 participants. The least reported related condition was comorbid immune deficiency diseases, which was present in only one participant (0.3%) out of 290 total respondents (Table 2, Figure 2).
 |
Table 2 Comorbidities in the Included Study Sample |
 |
Figure 2 Bronchiolitis associated comorbidities. |
The most common months for presentation were January (30.3%, n = 135) and December (21.6%, n = 96) followed by February (14.6%, n = 65) (Figure 3).
 |
Figure 3 Month of presentation. |
The most common symptoms at presentation were Shortness of breath (83.3%) and cough (81.7%). Fever was present in 60.8%. Wheezing and poor feeding were present in 37.7% and 37.6% of the included patients at presentation. Grunting was an initial presentation in only 5.2% of the patients (Figure 4).
 |
Figure 4 Symptoms of bronchiolitis. |
Productive cough was the most common nature of cough in presentation compared with the unproductive cough type (Figure 5). Also, according to the vital signs data at the patient initial presentation, fever was mostly a low-grade fever <= 38c (Figure 6).
 |
Figure 5 Nature of cough. |
 |
Figure 6 Grade of fever. |
Results showed that 44% (n = 196) had a negative test result for RSV and 41% (n = 181) had a positive test result. RSV testing was not done in the remaining 15% (n = 68). Thus, RSV was the causative agent in 41% of the cases, while the cause was unknown in the remaining 59% (Table 3) (Figure 7).
 |
Table 3 RSV Testing Status |
 |
Figure 7 RSV Testing status. |
Results showed that 99.1% of the patients were admitted to the ward (n = 433), and 12.8% of patients were admitted to the ICU (n = 55). Invasive mechanical ventilation was used in 13.2% (n = 57) of the patients. 65% (n = 281) of the patients received an oxygen therapy wain, while nasal suctioning was utilized in 12.9% (n = 54) of the patients. Chest physiotherapy and moist steam therapy were done in 55.6% and 12.0% of the patients. More than 90% of the patients received fluid therapy, and 93.6% received bronchodilator therapy. Feeding or nutritional therapy was given in 38.2% of the patients (n = 161), while hypertonic saline was prescribed in 81.3% (n = 357). Corticosteroid therapy was used in 19.7% of the patients (n = 87) and antivirals were required in 1.8% (n = 8). Antibiotics and palivizumab were given in 72.6% and 0.7% of the patients, respectively. Apnea, respiratory failure, and secondary bacterial infection occurred in 1.2%, 4.9%, and 8.1%, respectively. No deaths occurred in the study sample (Table 4).
 |
Table 4 Bronchiolitis Management and Associated Complications |
The average length of hospital stay was 5.88 ± 3.25 days, while the average length of ICU stay was 3.93 ± 2.73 days. The average duration of invasive mechanical ventilation was 3.91 ± 2.95 days (Figure 8).
 |
Figure 8 Distribution of (A) ward admission duration (B) ICU admission duration (C) Ventilation duration. |
We assessed if being diagnosed with RSV positive bronchiolitis is associated with poor prognosis in comparison with RSV negative bronchiolitis. We used chi-square test and independent sample t-test, where the null hypothesis refers to that no significant association between RSV positive bronchiolitis and long admission period, the use for invasive ventilation, associated complication such as apnea and secondary bacterial infection, and the requirement for ICU admission (Table 5 and 6). The results revealed that there is no significant difference in length of ward admission related to RSV status (p = 0.137). There was no significant relation between the frequency of ICU admission and RSV status among bronchiolitis patients (p = 0.130). No significant relation between participant ventilator usage and RSV testing (p = 0.548). No significant correlation between apnea and RSV positivity (p = 0.212). No significant relation between testing positive for RSV and respiratory failure (p = 0.786) Also, no significant association between RSV and secondary bacterial infection (p = 0.254) (Figure 9).
 |
Table 5 Length of Ward Admission Based on RSV Status |
 |
Table 6 ICU Admission, and Bronchiolitis Complications Based on RSV Status |
 |
Figure 9 Bronchiolitis complications among RSV positive and negative patients. |
We assessed if antibiotics alone is associated with similar or good prognosis in comparison with Palivizumab administration. Chi-square test and independent sample t-test have been used, where the null hypothesis refer to that antibiotics administration is not associated with better prognosis in comparison with Palivizumab. Results showed that there was no significant difference in the length of ward admission related to infants who took antibiotics and infants who took Palivizumab only (p = 0.576) (Table 7). No significant relation between the intensive care unit admission and taking antibiotics in comparison with Palivizumab administration (p = 0.653). No significant relation between the requirement of ventilator and taking antibiotics in comparison with only Palivizumab administration (p = 0.532). No significant correlation between the development of apnea and antibiotics administration when comparing with taking Palivizumab only (p = 0.889). Also, there was no significant relation between the development respiratory failure and taking antibiotics in comparison with the administration of Palivizumab only (p = 0.704). No significant association between secondary bacterial infection and being treated with antibiotics or Palivizumab only (p = 0.633) (Table 8).
 |
Table 7 Length of Ward Admission Based on Antibiotics and Palivizumab Administration |
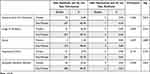 |
Table 8 ICU Admission, and Bronchiolitis Complications Based on Antibiotics and Palivizumab Administration |
We assessed the age factor correlation with the prognosis of bronchiolitis patients. Using Chi-square test and one way ANOVA, the null hypothesis refers to that young age of patients is not a predisposing factor to a poor prognosis. Patients were grouped into six age groups, from 0 months to 24 months. Results showed no significant difference in duration of ward admission (p = 0.359) among the six age groups, and no significant change in the intensive care unit admission (p = 0.344). Also, there was no significant between age and the usage of ventilators (p = 0.363), no significant association among young age groups and apnea (0.703), no significant relation between Respiratory Failure development and specific age group (p = 0.402), and no significant correlation between any of age groups and secondary bacterial infection (p = 0.596) (Table 9 and 10).
 |
Table 9 Length of Ward Admission Based on the Age Group |
 |
Table 10 ICU Admission, and Bronchiolitis Complications Based on the Age Group |
We evaluated the clinical impact of corticosteroids administration among bronchiolitis patients and compare them with those who did not receive corticosteroids during their management process (Table 11).
 |
Table 11 Length of Ward Admission Based on Corticosteroids Administration Status |
The result revealed significant difference in the duration of ward admission (p = 0.026), patient who received corticosteroids stayed in the hospital shorter than those who did not take steroids. Also, we found that corticosteroids administration is associated with less ICU admission (p = 0.0001), less requirement for ventilators (p = 0.0001), and less risk of development of respiratory failure (p=0.001) (Table 12, Figure 10).
 |
Table 12 ICU Admission, and Bronchiolitis Complications Based on Corticosteroids Administration Status |
 |
Figure 10 Bronchiolitis complications based on corticosteroids administration. |
However, there was no significant association between corticosteroids administration and less incidence of apnea (p = 0.262), or secondary bacterial infection (p = 0.371).
We assessed the relation between the month of bronchiolitis presentation and the status of RSV testing. We found significant relation between the month of presentation and the RSV status (p=0.0001) (Table 13, Figure 11). RSV positive cases tend to peak in December and January, while RSV negative patients tend to present in January and February.
 |
Table 13 RSV Status Based on Month of Presentation |
 |
Figure 11 RSV status among months of presentation. |
Discussion
This retrospective cohort study includes 445 participants ageing below 24 months who presented to King Fahad Hospital of the University (KFHU) from 2015 to 2020 with the diagnosis of Bronchiolitis. We concluded that bronchiolitis has almost equal prevalence among male and females with slight nonsignificant male predominance. Also, bronchiolitis tends to peak during winter with more than half of the cases being diagnosed during that season. Specifically, bronchiolitis diagnoses usually rise in January, December, and February, respectively. We found no clear association between the history of preterm birth, lack of adherence to the vaccination schedules, and the history of respiratory illness in the family with the risk of acquiring bronchiolitis. Also, the results revealed that congenital anomalies, congenital cardiovascular disease, congenital respiratory diseases, congenital neuromuscular diseases, immunodeficiency, and bronchial asthma are not a predisposing factor to harboring bronchiolitis below the age of two years. The commonest presenting symptoms for bronchiolitis in the studies sample were shortness of breath, cough, and fever. Coughs are more likely to be productive in nature, and the fever usually a low-grade fever.
In our study, it was found that a notable proportion of participants, specifically 15.30%, were not subjected to RSV (Respiratory Syncytial Virus) testing. Among the cases that were tested, it was observed that bronchiolitis was caused by RSV in 40.70% of the cases. Intriguingly, another 44% of the cases were attributed to alternative causative agents. RSV-positive cases typically exhibit a peak occurrence during the months of December and January, whereas patients who test negative for RSV tend to present more commonly in January and February.
In a study done in Abha, Saudi Arabia in 2005, A similar percentage of RSV positive bronchiolitis was observed.4 In another study conducted in Saudi Arabia, which involved the analysis of 282 subjects, it was found that 128 samples (45.4%) tested positive for RSV. The majority of these positive specimens were obtained from patients who were younger than one year old, accounting for 51.3% of the cases. Furthermore, there was a significant association between RSV infection and patients below two years of age, with 47.2% of this age group testing positive for RSV (P = 0.019).5
A third study over the course of a six-year research conducted in Saudi Arabia, a total of 643 hospitalized cases of Acute Lower Respiratory Infection (ALRI) were examined. Among the collected samples, RSV virus was identified in 295 cases, resulting in an overall detection rate of 45.8%).6
In a fourth Saudi study, out of 4575 inpatients and outpatients with acute respiratory symptoms, 19.3% of the nasopharyngeal aspirate samples tested positive for RSV. The distribution of cases revealed that 55% were male and 45% were female. The majority of RSV-positive cases were found within the age group of 0 to 6 months, accounting for 58.9% of the cases, followed by the age group of over 6 to 12 months, comprising 19.8% of the cases. Analysis of seasonal patterns demonstrated that RSV cases were most prevalent during the winter and early spring months.7 During the period of 1991–1992 in Riyadh, out of the 127 studied sample, it was found that 54% of the studied cases tested positive for RSV.8 Another study conducted in Riyadh, which included 485 ALRI patients under the age of 2, detected RSV in 70% of the samples.9 RSV accounted for 79% of the total 1429 ALRI cases in children under the age of 5 who were hospitalized in another study from Riyadh between 1993 and 1996.10 Out of 256 sample cases hospitalized with ARI in Riyadh from 1993 to 1996, RSV was detected in 29%.11 In the case of children admitted for ALRI from Abha during 1997–2001, RSV was found to be positive in 40% of the 51 cases.4 In a study from Al-Qassim, RSV was detected in 45% of the 282 samples collected from children admitted to a hospital with ALRI during 2003–2004.5 Another investigation from Riyadh identified RSV in 7% of 10,617 ARI cases.12 A study conducted in Najran on 135 patients diagnosed as acute respiratory tract infection, the result showed that 33 cases were having a RSV infection (24%).13 A study from Riyadh reported a high percentage of RSV (97.4%) among a total of 1115 ARTI viral-infected samples, and a 23.5% proportion of RSV among all the studied ARTI sample (4611).14 An investigation in Jazan by Abdulhaq and colleagues showed a low percentage of RSV positivity among the study sample out of total 182 participant. However, RSV is (13.6%) prevalent among 75 positive viral-infected samples.15 Lastly, a recent study conducted in Riyadh analyzed 2266 pediatric patients and revealed that RSV was positive in 29% of the cases.16
Upon admission, approximately 13% of the patients were transferred to the Intensive Care Unit (ICU), while a nearly equivalent percentage required invasive ventilation. In comparison to a study done in Abha, Saudi Arabia in 2005 over 161 patients, around 5% were admitted to ICU and only 2.5% required the usage of ventilation.4
The majority of patients (over 90%) received a combination of bronchodilators and intravenous (IV) fluids as part of their treatment regimen. Additionally, more than 80% of patients were administered hypertonic saline, and approximately 70% were prescribed antibiotics. Notably, Palivizumab was administered to only three patients, while eight patients received antiviral treatment. Nevertheless, the recent AAP Updates Guidelines on Bronchiolitis strongly discourage the use of salbutamol or adrenaline in the treatment of bronchiolitis.17
Upon analyzing the various management options and their impact on the length of hospital stay, our study revealed that the use of antibiotics and corticosteroids did not lead to a decrease in hospital stay duration. Surprisingly, patients who received either of these medications actually had longer hospital stays compared to those who did not receive them. Conversely, we observed no significant difference in the length of hospital stay between patients who underwent hypertonic saline and those who did not receive this treatment. These findings underscore the need for a critical evaluation of the potential benefits and risks associated with antibiotic and corticosteroid use in the context of hospital stay duration, while also highlighting the limited impact of hypertonic saline on length of hospital stay. However, studies suggests that hypertonic saline is associated with reduction in length of hospital stay in about 26% of bronchiolitis cases.17
In our study, we analyzed the average length of stay for patients based on their gender and identified interesting patterns. The data revealed that the average length of stay was comparable between males and females, with males staying for approximately 6.01 days and females for 5.67 days. However, an intriguing finding emerged when examining the Intensive Care Unit (ICU) stay duration. Among the patients requiring ICU care, there was a significant prolongation in the length of stay for females compared to males (p-value=0.01). This disparity highlights a potential gender-specific factor influencing the severity or management of patients’ conditions within the ICU setting.
Additionally, we investigated the ventilator requirement among the patients and found that it was similar between males and females, indicating that the mechanical ventilation was not influenced by gender. However, when examining the clinical presentation, we discovered notable gender-based differences. Males demonstrated a higher prevalence of wheezing compared to females (p-value=0.003), suggesting a potential sex-related variation in the respiratory manifestations of the patients. Moreover, males also exhibited a higher frequency of a runny nose compared to females (p-value=0.029), indicating a gender-specific trend in the presenting symptoms.
Among the cases of bronchiolitis analyzed in our study, a total of 61 cases were identified as complicated bronchiolitis. The most common complication observed was secondary bacterial infection, affecting 35 individuals, followed by respiratory failure, which was reported in 21 cases. Interestingly, our data revealed a significant correlation between younger age and the occurrence of secondary bacterial infections (p = 0.01), with patients in the early months of life experiencing the highest rate of such infections. Additionally, our study found that bronchiolitis recurrence was reported in 17 patients, accounting for 3.8% of the total sample size of 445 patients.
Our study revealed that the status of being RSV positive or negative did not show any association with a longer duration of admission, an increased likelihood of requiring ICU admission or ventilation, or an elevated risk of developing apnea, respiratory failure, or secondary bacterial infection. These findings suggest that the presence or absence of RSV infection does not significantly impact these clinical outcomes in the context of our study population.
Upon analyzing the treatment regimens administered to patients, we observed no substantial disparities in terms of the length of ward admission, the requirement for ICU admission or ventilation, and the occurrence of apnea, respiratory failure, and secondary bacterial infection between patients who received antibiotics without palivizumab and those who received palivizumab without antibiotics. These findings indicate that the combination of antibiotics and palivizumab did not have a significant impact on these clinical outcomes compared to the use of either treatment alone.
Despite our study assessing the efficacy of corticosteroid administration in bronchiolitis patients, we found compelling evidence supporting its benefits. Patients who received corticosteroids exhibited a significantly shorter duration of ward admission (p = 0.026), a reduced likelihood of requiring ICU admission (p = 0.0001), and a decreased use of ventilation (p = 0.0001). Moreover, the use of corticosteroids was associated with a decreased risk of developing respiratory failure. These findings emphasize the potential positive impact of corticosteroid treatment in managing bronchiolitis, highlighting its ability to potentially shorten hospital stays, minimize severe complications, and improve patient outcomes. Nonetheless, according to the Cochrane database and AAP, it has been concluded that neither systemic nor inhaled steroids provide any clinical advantage in terms of reducing the rate of hospital admission or the length of hospitalization.17
A retrospective cohort review study done in Riyadh for Bronchiolitis in a total of 141 children showed that cough is the most common presenting symptom in 96% of patients. In our study, cough presented as the second most common symptom after Shortness of breath.18 The patients usually present with high-grade fever which is found in 78% of patients. This finding is inconsistent with our result, high-grade fever was only presents in 24.7% of those presenting with fever, with the low-grade fever being more prevalent 75.30%.18
Out of the 141 patients in the Riyadh study, only four patients required ICU admission, and the same patients required ventilator usage. In our study, out of the 445 patients, only 55 patients were admitted to ICU, and 57 patients required ventilator use.18 A total of 83 patients did RSV testing, and it was positive in 45 patients (54%). In our study, RSV testing for 377 patients, and the test was positive in 181 (41%).18
Bronchodilators were the most commonly used management option in the Riyadh study which were prescribed for 111 patients (78%). This finding is consistent with our results, which revealed that bronchodilator is the most common management option used in 412 (93.6%).18 The other management methods used in the Riyadh study are oxygen in 39 patients (27.7%), hypertonic saline in 38 cases (26%) and antibiotics in 25 patients (17.7%). On the other hand, our study showed a significant variation in usage frequency with hypertonic saline used in 357 patients (81.3%), antibiotics prescribed for 321 patients (72.6%) and oxygen used in 280 patients (65%).18 With the same results as our study result, the Riyadh study showed no mortality among the patients.18
We also compared our data to different epidemiological studies outside Saudi Arabia to help relate our results to other different geographical areas. In a study done in Mexico, we found no significant variation in between the age of onset; in their study, the average age is 6.6 ± 5.7 months, while in ours, it was 6.33 ± 5.24 months. Moreover, the gender was predominately male in both studies, 60.5% in Mexico and 54.5 in ours.19
RSV bronchiolitis was the most causative agent in both studies, 41.17% in the Mexico study, and ours was 41%.
Our data were also compared to a systemic review by20 regarding the epidemiological burden of RSV bronchiolitis. The results of that systemic review showed, 83% of RSV patients were below the age of six months in comparison to 61.7% in our study.
The length of stay was also similar between our study and the systemic review, 5.88 Days to 5 days, respectively. However, the ICU admission rate differed between our study and the average of the studies included in the systemic review, 12.3% to 5.05%, respectively.
The variations between our result and other local and global results may be attributed to the different geographical areas, sample sizes and weather differences. Furthermore, in the absence of global consensus regarding bronchiolitis management, different hospital protocols for the management constitute a significant factor in results variation. Moreover, preemptive ICU admission and ventilator usage can be influenced by subjective clinical judgment and available hospital resources.
Limitations
This study has many limitations, such as the COVID −19 pandemic where it made data collection much harder due to the safety precautions that were undertaken by King Fahad Hospital Of the University (KFHU), limiting the time of access to the hospital database, which in turn prolonged the data collection period.
Due to the study’s retrospective design, our primary source of data was KHFU databases, where we encountered many digital data inadequacies.
Some of the study’s variables were not reported or acquired at the time of the patient presentation, making the data collection process more difficult.
Conclusion
In conclusion, Bronchiolitis has been a major burden on health care systems around the world for the past 20 years. This study identifies the variation in the clinical presentation between children with bronchiolitis who presented to KFHU between 2015 and 2020. The studied sample in this research had a wide range of clinical presentations from very mild to life-threatening. Although the male sex is generally considered a risk factor for more severe disease, we found that females had a longer ICU stay and ventilator use duration. Furthermore, we identified that the first few months of life were more associated with bronchiolitis infection as almost 84% of our patients were younger than 12 months and 37% were younger than three months. Moreover, ICU admissions in KFHU were significantly higher than other local and global ICU Admissions rates where we reviewed an average in a systemic review was 5.05%, and our hospital had 12.3%, more than two times the systemic review average.
Finally, clinicians should pay more attention to the high-risk group to reduce the bronchiolitis load in the health care systems.
Application
Several real-world applications of our research can be applied to reach a significant development in the care provided to bronchiolitis patients. An example of our research’s real-world applications is a better prediction of the burden of Bronchiolitis in KFHU. Furthermore, it may be used as reference data for future researchers. Finally, it will help KFHU physicians recognize the local pattern in the presentation of Bronchiolitis.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hasegawa K, Tsugawa Y, Brown DF, et al. Trends in Bronchiolitis Hospitalizations in the United States, 2000–2009. Pediatrics. 2013;132(1):X3. doi:10.1542/peds.2012-3877d
2. Drysdale SB, Green CA, Sande CJ. Best practice in the prevention and management of paediatric respiratory syncytial virus infection. Therapeutic Adv Infectious Dis. 2016;3(2):63–71. doi:10.1177/2049936116630243
3. Coffin SE. Bronchiolitis: in-Patient Focus. Pediatr Clin North Am. 2005;52(4):1047–1057. doi:10.1016/j.pcl.2005.04.002
4. Al-Shehri MA, Sadeq A, Quli K. Bronchiolitis in Abha, Southwest Saudi Arabia: viral etiology and predictors for hospital admission. West Afr J Med. 2005;24(4):299–304. doi:10.4314/wajm.v24i4.28193
5. Meqdam MM, Subaih SH. Rapid detection and clinical features of infants and young children with acute lower respiratory tract infection due to respiratory syncytial virus. FEMS Immunol Med Microbiol. 2006;47(1):129–133. doi:10.1111/j.1574-695X.2006.00073.x
6. Bukhari EE, Elhazmi MM. Viral agents causing acute lower respiratory tract infections in hospitalized children at a tertiary care center in Saudi Arabia. Saudi Med J. 2013;34(11):1151–1155.
7. Shier MK, Mona AB. Respiratory syncytial virus infection in patients visiting King Khalid University Hospital. Menoufia Med J. 2005;18:11.
8. Jamjoom GA, Al-Semrani AM, Board A, Al-Frayh AR, Artz F, Al-Mobaireek KF. Respiratory syncytial virus infection in young children hospitalized with respiratory illness in Riyadh. J Trop Pediatr. 1993;39(6):346–349. doi:10.1093/tropej/39.6.346
9. Chowdhury D, Al-Howasi M, Ramia S, Al-Frayh AR, Khalil M, Chowdhury S. Respiratory syncytial virus in Saudi patients admitted to hospital with bronchiolitis: use of direct fluorescent antibody tests as a rapid diagnostic tool. Ann Saudi Med. 1996;16(1):90–92. doi:10.5144/0256-4947.1996.90
10. Bakir TM, Halawani M, Ramia S. Viral aetiology and epidemiology of acute respiratory infections in hospitalized Saudi children. J Trop Pediatr. 1998;44(2):100–103. doi:10.1093/tropej/44.2.100
11. Al-Hajjar S, Akhter J, Al Jumaah S, Qadri SH. Respiratory viruses in children attending a major referral centre in Saudi Arabia. Ann Trop Paediatr. 1998;18(2):87–92. doi:10.1080/02724936.1998.11747933
12. Akhter JA, Al-Johani S, Dugaishm F, Al-Hefdi R, Al-Hassan I. Etiology of respiratory viral infections using rapid virus isolation methods at a tertiary care center in Riyadh, Saudi Arabia. Saudi Pharm J. 2009;17(2):177–181.
13. Al-Ayed MS, Asaad AM, Qureshi MA, Ameen MS. Viral etiology of respiratory infections in children in southwestern Saudi Arabia using multiplex reverse-transcriptase polymerase chain reaction. Saudi Med J. 2014;35(11):1348.
14. Albogami SS, Alotaibi MR, Alsahli SA, Masuadi E, Alshaalan M. Seasonal variations of respiratory viruses detected from children with respiratory tract infections in Riyadh, Saudi Arabia. J Infect Public Health. 2018;11:183–186. doi:10.1016/j.jiph.2017.06.001
15. Abdulhaq AA, Basode VK, Hashem AM, et al. Patterns of human respiratory viruses and lack of MERS-coronavirus in patients with acute upper respiratory tract infections in southwestern province of Saudi Arabia. Adv Virol. 2017;2017:57.
16. Eifan SA, Hanif A, AlJohani SM, Atif M. Respiratory tract viral infections and coinfections identified by Anyplex™ II RV16 detection kit in pediatric patients at a Riyadh tertiary care hospital. Biomed Res Int. 2017;2017:1–10. doi:10.1155/2017/1928795
17. Alharbi AS, Alqwaiee M, Al-Hindi MY, et al. Bronchiolitis in children: the Saudi initiative of bronchiolitis diagnosis, management, and prevention (SIBRO). Ann Thorac Med. 2018;13(3):127.
18. Ahmad SA, Mujawar Q, Al Othman M, Bin SH, Alsarfandi MA. Clinical profile of Bronchiolitis in infants younger than 90 days in Saudi Arabia. J Em Trauma Shock. 2014;7(1):49–52. doi:10.4103/0974-2700.125641
19. Robledo-Aceves M, Moreno-Peregrina MDJ, Velarde-Rivera F, et al. Risk factors for severe bronchiolitis caused by respiratory virus infections among Mexican children in an emergency department. Medicine. 2018;97(9):e0057. doi:10.1097/md.0000000000010057
20. Bont L, Checchia PA, Fauroux B, et al. Defining the Epidemiology and Burden of Severe Respiratory Syncytial Virus Infection Among Infants and Children in Western Countries. Infectious Dis Therapy. 2016;5(3):271–298. doi:10.1007/s40121-016-0123-0
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
