Back to Journals » International Journal of General Medicine » Volume 16
Body Mass Index Profile and Its Association with Social Determinants Among Adolescents from Jazan, Saudi Arabia
Authors Gosadi IM , Abualgasem MM , Sultan YA, Bakri MY, Ageeli AM, Kaal AA, Khmees RA
Received 2 October 2023
Accepted for publication 21 December 2023
Published 27 December 2023 Volume 2023:16 Pages 6151—6162
DOI https://doi.org/10.2147/IJGM.S442898
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Sandul Yasobant
Ibrahim M Gosadi,1 Mohammed M Abualgasem,2 Yasser A Sultan,3 Mohammed Y Bakri,3 Amal M Ageeli,4 Abdulaziz A Kaal,5 Rola A Khmees6
1Department of Family and Community Medicine, Faculty of Medicine, Jazan University, Jazan, Saudi Arabia; 2Abu Arish General Hospital, Ministry of Health, Jazan, Saudi Arabia; 3Prince Mohammed Bin Nasser Hospital, Ministry of Health, Jazan, Saudi Arabia; 4Faculty of Medicine, Jazan University, Jazan, Saudi Arabia; 5Department of Radiology, King Fahd Central Hospital, Ministry of Health, Jazan, Saudi Arabia; 6Department of Family and Community Medicine, King Saud University Medical City, Riyadh, Saudi Arabia
Correspondence: Ibrahim M Gosadi, Faculty of Medicine, Jazan University, P.O. Box: 2349, Jazan, 82621, Saudi Arabia, Tel +966562137711, Email [email protected]
Purpose: Assess adolescents’ body mass index (BMI) profile and the association between BMI category and social determinants.
Methods: This cross-sectional study targeted adolescents aged between 12 and 19 from Jazan, Saudi Arabia. Data was collected via an online self-administered questionnaire during 2023. The tailored questionnaire measured items related to student demographics, their history of diagnosed chronic conditions, their familial history of chronic diseases, and their eating behavior. A standard chi-square test investigated the relationship between BMI category and social determinants.
Results: Five hundred and seventy students completed the study’s questionnaire. The mean age of the sample was 16 (SD: 1.9), and most of the respondents were female (60%). Among the recruited sample, 107 students (20%) are categorized as underweight, while 121 students (22%) are classified as either overweight or obese according to their age. The respondents’ eating behavior indicated that the most frequently consumed meal was dinner, and the majority skipped breakfast some days of the week. Nearly one-third of the sample exhibited emotional eating. Low consumption of healthier food options, such as fruits, vegetables, low-fat products, and whole grain products among the adolescents was noted. An assessment of BMI level distribution among the respondents according to their demographic characteristics indicated a higher frequency of overweight and obesity among male adolescents, students in the secondary level, students living with a lower number of siblings, and students with a parental history of diabetes, obesity, and dyslipidemia (p values < 0.05).
Conclusion: A high frequency of BMI abnormality among adolescents was detected. Dietary behavior among the respondents suggests the presence of several unhealthy behaviors. The results of the current study detected an important influence of the family on weight status among these adolescents.
Keywords: BMI, adolescents, underweight, overweight, obesity
Introduction
Overweight and obesity continue to be a challenge; a dramatic increase in their prevalence has been seen over the last five decades. According to the World Health Organization, obesity’s prevalence has tripled since 1975. By 2016, nearly two billion adults were overweight, of whom more than 650 million were affected by obesity. Furthermore, over 340 million children and adolescents aged between five and 19 are were overweight or obese by 2016.1 The increased incidence of obesity among children and adolescents demonstrates the need to make this a public health priority as it can be associated with a prediction of increased obesity in communities across the world.
Saudi Arabia is one of the countries where overweight and obesity present a main health challenge. According to the World Health Survey of Saudi Arabia, 58% of the adult population of Saudi Arabia is overweight or obese.2 The high occurrence of overweight and obesity among Saudis has been partially explained by the prevalence of metabolic syndrome in the country.3 Furthermore, a 2016 study that recruited a sample of 7,930 children and adolescents from Riyadh, Saudi Arabia, reported that the prevalence of overweight and obesity among the sample reached 13.4%, double the amount since 2004.4
Habbab and Bhutta conducted a recent systematic review of 51 articles investigating social determinants of overweight and obesity among adolescents in Saudi Arabia. Habbab and Bhutta indicated that adolescents’ dietary patterns, such as skipping breakfast, consuming fast food and soft drinks, and having a low intake of vegetables, were significantly associated with a higher prevalence of overweight and obesity. Physical inactivity and sedentary behavior were other contributing lifestyle factors. Furthermore, familial factors, such as family history of obesity, family size, parental education, and employment, were identified as risk factors for overweight and obesity among adolescents and are important factors influencing the condition’s frequency in Saudi Arabia.5
The World Health Survey of Saudi Arabia’s results detailed the presence of regional variations in the incidence of overweight and obesity among adults in Saudi Arabia. Saudi Arabia has 13 administrative regions; a higher occurrence of overweight and obesity was reported in the northern region of Al Jawf (70%) compared to the southwestern region of Jazan (49%). This variation in prevalence can be partially explained by discrepancies in socioeconomic characteristics between the country’s regions.2 Reports concerning regional variation in the prevalence of overweight and obesity among adolescents in Saudi Arabia are limited.
El Mouzan et al conducted a study to measure the frequency of overweight and obesity among children and adolescents in the Northern, Central, and Southern regions of Saudi Arabia between 2004 and 2005. They concluded that the prevalence of overweight varied between 13% and 21%, and the prevalence of obesity ranged between 6% and 9.3%; a higher incidence of overweight and obesity was noted in northern and central regions compared to southern regions. Though El Mouzan et al did not investigate factors associated with the lower prevalence of overweight and obesity among children and adolescents in the southern region, they explained the lower prevalence of overweight and obesity by the higher prevalence of underweight and stunting among adolescents in the south of Saudi Arabia.6
Variation of BMI profile between different communities can be partially explained by the variation of social determinants of health. This variation has been indicated to influence body weight of individuals at early stage of childhood and continues throughout the following stages of life where genetic factors, cultural believes, ethnicity, stigma, age, gender, living conditions, parents education, and stress associated with social and neighborhood influence, can interact to influence body weight levels.7 The social determinants associated with body weight among adolescents can collectively influence dietary habits and how adolescents get access to healthy food options, and have better physical activity opportunities, which can vary according to the support provided to adolescents by family, school, peers, and the community.8 Therefore, it is possible to argue that interaction of social determinants of health associated with body weight can incur higher risk of developing either underweight or overweight and obesity.
Public health programs targeting body weight among adolescents should target social determinants associated with malnutrition among adolescents. Malnutrition refers to either deficiency or excess in food intake leading to underweight or overweight and obesity.9 Undernutrition and overnutrition can be considered as a double burden public health issue in developing countries,10 such as Saudi Arabia.
It is possible to argue that the majority of the health literature related body weight among adolescents in Saudi Arabia is focusing on overweight and obesity. However, recent literature is indicating the importance of performing BMI profiling to measure body weight distribution among the adolescents in a comprehensive manner according to all BMI categories. For example, in a recent study that included a sample of 12,463 Saudi adolescents, it was indicated that the prevalence of underweight among the sample reached 15% where an association between underweight prevalence and distorted body image, weight loss attempt and eating behavior disorders was indicated.11 Additionally, some adolescents may be influenced by body weight perception and dissatisfaction which may lead them to adopt unhealthy weight loss practices.12
There is a lack of body mass index (BMI) profiling by percentile among adolescents in Jazan, in the southwest of Saudi Arabia; furthermore, the determinants associated with occurrences of underweight, normal weight, and overweight and obesity among this population are unknown. The current investigation provides BMI profiling among adolescents in the Jazan region of Saudi Arabia. It assesses the studied sample’s social characteristics and dietary habits associated with body weight. Finally, the association between social characteristics and BMI levels was evaluated to investigate factors related to the prevalence of underweight or overweight and obesity.
Methods
Study Design and Setting
This study was performed by utilizing a cross-sectional design. The Saudi Arabian school system has three levels: elementary, intermediate, and secondary. Adolescents from the Jazan region who were registered as intermediate or secondary students were targeted for this research. The study was initiated after securing ethical approval from the Standing Committee for Scientific Research of Jazan University (approval number REC-44/06/446, dated December 2022). Data collection was performed from the beginning of February until the end of March 2023.
Data collection was performed in online settings. A study information sheet was shared with the parents of the students via social media platforms. The information sheet was followed by an online written consent form to be read and approved by one of the parents. The approached parents could select to approve or reject the child’s participation, and the students were recruited after securing the informed consent of their parents. Those who refused were not provided access to the data collection tool and were directed elsewhere. The study was conducted in accordance with the Declaration of Helsinki.
Data Collection Tool
Data was collected via a self-administered questionnaire; it measured items related to student demographics, their history of diagnosed chronic conditions, paternal history of chronic diseases, and their eating behavior. The students were asked about their age, gender, body weight, height, residence location, family size, and whether or not they were living with their parents. They were also asked whether they were diagnosed with chronic conditions that might influence body weight among children, including dental illnesses, mental illnesses, obesity, asthma, blood disorders such as thalassemia and sickle cell diseases, and diabetes.
Items measuring eating behavior associated with BMI levels were adopted from the Saudi Guidelines for Prevention and Management of Obesity, such as the frequency of consuming meals, choice of consuming low-fat food, whole grain products, low-calorie food items, and eating atmosphere such as eating with the family or eating while watching TV.13 Furthermore, items measuring cognitive restraints, uncontrolled eating, and emotional eating were adapted from the Three-Factor Eating Questionnaire.14 A consultant in nutritional epidemiology reviewed the data collection form to evaluate its content. A pilot study of the questionnaire on a sample of 10 male and female students was conducted to assess the clarity of the questionnaire and the time needed to complete it. Cronbach’s alpha test was performed to test the reliability of questionnaire items assessing the eating behavior of the participants and generated a value of 0.69, indicating reasonable internal reliability.
Data Collection Process
Data was collected by converting the questionnaire to an online data collection form. A web link was generated to facilitate the distribution of the questionnaire on social media platforms to reach the targeted population’s parents. Parents who agreed to participate were asked to share the questionnaire web link with their acquaintances to reach the required sample size. Participants were included in the study if they were students registered in intermediate or secondary schools in the Jazan region and if their parents gave consent to participate.
Snowballing non-random sampling was used to reach the required sample size. The necessary sample size was established using the StatCalc function of Epi Info designed by the United States Centers for Disease Control and Prevention. Since there was no published data about BMI profiles of adolescents in the Jazan region, estimates of adult BMI profiles were used to calculate the required sample size. Based on current evidence from The World Health Survey of Saudi Arabia,2 which indicated that the prevalence of overweight and obesity among adults in the region is 49%, a sample size of 500 participants was estimated assuming a 5% margin of error, 95% confidence level, and 30% of responses not meeting the inclusion criteria.
Data Analysis
The data was analyzed using the IBM Statistical Package for the Social Sciences, version 24.0. Frequencies and proportions were used to summarize binary and categorical data. Continuous data were summarized via means, medians, standard deviations, and interquartile ranges, depending on their distribution. A standard chi-square test investigated the relationship between BMI category and social determinants.
BMI levels were calculated by dividing the reported weight in kilograms by squared height in meters to enable performing BMI profiling of the respondent students. The BMI Percentile Calculator for Child and Teen from the Centers for Disease Control and Prevention was used to categorize the sample into underweight, normal weight, and overweight and obese participants. A chi-square test or Fisher’s Exact tests were used to evaluate the statistical variation between the demographic characteristics of students depending on their BMI category. A p-value of < 0.05 was used to indicate statistical significance.
Results
There were 714 total responses, of whom 144 were excluded due to not securing parental consent or not meeting the inclusion criteria. Five hundred and seventy students completed the study’s questionnaire, indicating a response rate of 80%. Demographic characteristics, BMI profile, and history of diagnosed chronic diseases are displayed in Table 1. The mean age of the sample was 16 (SD: 1.9), and the majority of the respondents were female (60%). The distribution of the recruited students is nearly equal concerning the residence area. However, more students from the secondary level participated in the study (68%) in comparison to students from intermediate level. When the students were asked whether they were living with both of their parents, 13 students (2.3%) indicated that they were living with the father only, while 67 students indicated that they were living with the mother only (12%). Just over half of the students indicated that the number of siblings in the family is four or less (56%).
 |
Table 1 Demographic Characteristics, BMI Profile, and History of Chronic Diseases Among 570 Intermediate and Secondary School Students from Jazan, Saudi Arabia |
The distribution of the recruited students according to their BMI levels showed a noteworthy variation. Among the recruited sample, 107 students (20%) are categorized as underweight, while 121 students (22%) are classified as either overweight or obese according to their age; 58% of the sample had normal body weight levels. When the students were asked about their diagnosed morbidities, the responses indicated that the most frequently diagnosed disease was asthma (6%), followed by dental issues (5.8%) and obesity (4%). Table 2 displays the students’ responses about their parents’ history of diagnosed chronic diseases. The most frequently reported chronic conditions among the parents were hypertension and diabetes.
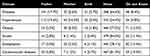 |
Table 2 Reported Diagnosed Chronic Diseases Among Parents of 570 Intermediate and Secondary School Students from Jazan, Saudi Arabia |
Table 3 displays the frequency of consuming daily meals. When the students were asked about the timing of consuming meals, they indicated that the meal most frequently consumed daily was dinner (57%), followed by lunch (56%). Only 226 students (40%) indicated that they have breakfast daily. The proportion of students who reported eating daily in-between meals varied between 16% for brunch, 19% for supper, and 20% for a snack after dinner.
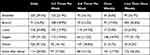 |
Table 3 Frequency of Consumption of Daily Meals Among 570 Intermediate and Secondary School Students from Jazan, Saudi Arabia |
The eating behavior of the respondents is summarized in Table 4. Nearly one-third of the sample (161 students) indicated that they consume food when they are not feeling hungry, either always or most of the time. Similarly, nearly one-third of the sample stated that they cannot resist the desire to eat, either always or most of the time. When the students were asked whether they tend to eat more when they feel anxious or depressed, 154 (27%) students reported that they do tend to eat more when feeling anxious or depressed, always or most of the time. One hundred students (17%) indicated that they are always aware when they consume large amounts of food. Over half of the sample reported never selecting low-calorie food items and never preferring whole-grain bread.
 |
Table 4 Eating Behavior of 570 Intermediate and Secondary School Students from Jazan, Saudi Arabia |
When the participants were asked about the frequency of consuming fruits and vegetables, 332 (58%) of the students indicated that they do not consume any fruits and vegetables daily. Additionally, the participants were asked whether they tend to eat restaurant meals; nearly one-third of the sample (164) indicated that they do consume food bought from restaurants most days of the week. Table 5 displays the frequency of consuming energy-dense food items; more than 40% of the sample reported consumption of these items daily or four or more days during the week. Finally, when the participants were asked about their drink preference while eating, more than half of the sample (59%) noted their preference for sugar-sweetened soft drinks or fruit drinks, and only 25.8% of the students reported preferring water while eating.
 |
Table 5 Frequency of Consuming Specific Food Items Among 570 Intermediate and Secondary School Students from Jazan, Saudi Arabia |
Table 6 shows the associations between the students’ demographic characteristics and BMI levels. Statistically significant differences were detected concerning the distribution of BMI levels according to gender, education level, number of siblings in the family, and parental history of diagnosed diabetes, obesity, and dyslipidemia (p values < 0.05). A higher frequency of overweight or obesity was detected among male students compared to females and among secondary school levels compared to intermediate school levels. Moreover, fewer siblings were associated with a higher frequency of overweight and obesity. A higher occurrence of overweight and obesity was noted among students who reported that either one of the parents or both were affected with diabetes, obesity, or dyslipidemia.
 |
Table 6 Association Between Demographic Characteristics and BMI Level Among 570 Intermediate and Secondary School Students from Jazan, Saudi Arabia |
Discussion
The current investigation was a cross-sectional assessment of BMI profiles among adolescents in the Jazan region. Over half of the sample exhibited normal body weights for their age; the remaining were underweight, overweight, or obese. The most frequently diagnosed condition among the adolescents was asthma, and the most commonly diagnosed condition among their parents was hypertension and diabetes. The adolescents’ eating behavior indicated that the most frequently consumed meal was dinner; most skipped breakfast some days of the week. Nearly one-third of the sample disclosed emotional eating. Low consumption of healthier food options, such as fruits, vegetables, low-fat products, and whole grain products among the adolescents was noted. Assessment of the distribution of BMI levels according to demographic characteristics indicates a higher frequency of overweight and obesity among male adolescents, students in the secondary level, students living with fewer siblings, and students with parental history of diabetes, obesity, and dyslipidemia.
The current study’s findings can be compared to similar local or international studies. The investigation identified a higher prevalence of overweight and obesity among male students than females. The current findings are different from El Mouzan et al’s; they recruited a sample of 1,073 adolescents aged between 13 and 18 from the Southwest of Saudi Arabia (including the Jazan and Aseer regions) and detected a higher occurrence of overweight among females (21%) compared to males (17%).6 Though reasons for the variation can be partially attributed to sampling variation, it could suggest a change in BMI profile since the study by El Mouzan was conducted nearly 20 years before the measurements performed in the current study. Similarly, another study conducted in the Aseer region in 2000 identified a similar higher prevalence of overweight and obesity among female adolescents compared to male adolescents.15 Finally, research on 1,869 adolescents from the Aseer region identified a higher prevalence of obesity among females (29.4%) than males (20.6%). Although the study was published in 2011,16 the exact measurement period was not declared, thus limiting the ability to evaluate variation in BMI profiles between different assessment periods.
The current study identified several adolescent dietary behaviors that can increase the risk of having abnormal BMI, including skipping breakfast, higher consumption of energy-dense food, and lower consumption of healthier food items. The current findings are supported by Habbab and Bhutta’s systematic review, which measured social determinants of overweight and obesity among adolescents in Saudi Arabia.5 Habbab and Bhutta identified several practices associated with overweight and obesity among these adolescents, such as skipping breakfast, consuming fast food and soft drinks, and having a low intake of vegetables, which are similar to the findings of current study.
Studies that assessed the frequency of underweight in Saudi Arabia are limited. The current investigation identified a prevalence of 20% among the recruited sample. A nationwide study by Hijji et al recruited a sample of 12,463 adolescents from 282 schools from all administrative regions in Saudi Arabia between 2011 and 2012. It indicated that the prevalence of underweight was 15%, which is lower than the incidence of underweight detected in current investigation.11 Furthermore, Hijji et al indicated that the prevalence of underweight among males (18%) was higher than among females (12.4%), which is different from current study’s findings in which the proportions of underweight among male and female adolescents were equal. Additionally, Hijji et al identified a higher occurrence of underweight among households with a higher number of siblings, similar to the current study’s findings, where a higher prevalence of underweight was seen among families with a larger number of siblings.
The data indicate that the current sample of adolescents consumes more frequent meals at night than during the day. Though current study did not assess the association between overweight and obesity according to the preferred eating time, the current evidence suggests an association between chronotype and risk of raised BMI among adolescents. In a recent systematic review and meta-analysis, which involved 15 studies that assessed the relationship between obesity and chronotype among adolescents, it was noted that adolescents with an evening chronotype have a higher risk of unhealthy eating behavior and overweight and obesity.17
The current study identified a higher frequency of overweight and obesity among adolescents with a parental history of diabetes, obesity, and dyslipidemia. Several international investigations support the current findings. A study of 11,050 12-year-old children from Sweden demonstrated that parental diabetes was associated with an increased risk of overweight among the sample.18 Similarly, another study involving a sample of 20,151 European parents and 10,967 of their children noted that parental diabetes and parental overweight and obesity were associated with higher odds of overweight and obesity among the children.19 Additionally, in a systematic review that involved 23 studies conducted in different parts of the world, it was concluded that parental obesity plays a vital role in increasing the risk of childhood obesity.20 Finally, a European study involving 12,193 children from six European countries showed that the odds of childhood obesity increase when both parents are obese compared to the odds of childhood obesity if only one parent is affected, demonstrating the importance of considering the whole family when developing childhood obesity prevention programs.21
The current findings indicate the presence of several dietary habits and social factors that can influence body weight among the recruited adolescence. The main dietary habits identified in the current sample were related to opting to consume food during the night time more than the morning time, high risk of emotional eating, and low consumption of healthier food items such as fruits, vegetables, whole grain products, and low fat products. Additionally, our findings indicate that certain social factors can be associated with BMI level of the recruited adolescents such as gender, age, family condition, and having a parental history of metabolic diseases. These findings indicate the importance of addressing dietary habits of adolescents and related social determinants when developing interventions related to BMI in adolescents.
The current evidence indicates that the prevalence of obesity and overweight has been increasing in Saudi Arabia during the last four decades. In response to this increase, several public health initiatives were implemented. In a review by Almubark et al which assessed interventions applied in Saudi Arabia to address overweight and obesity in the country, it was reported that 8 public health initiatives were implemented between 1999 and 2019. Majority of these initiatives were focusing on promotion of physical activity and it can be noted that the implementation of each of these initiatives was performed individually by governmental, or non-governmental agencies indicating limited multi-sectorial collaboration.22 Additionally, Almubark et al concluded that no formal evaluation of the effectiveness of these programs was identified, indicating an area for further assessment, especially with the current rates of BMI abnormalities.
The findings of the current study indicate that the prevalence of abnormal BMI among adolescents in the studied population is distributed nearly equally between underweight, and overweight and obesity (20% vs 22%). The identified dietary habits and social determinants associated with BMI among the recruited sample indicates the importance of addressing BMI abnormalities in a holistic manner, rather than concentering on one abnormality or one risk factor in each initiative, such as concentrating on the importance of walking and exercise.
The current identified associations between BMI and social factors among the recruited adolescents suggests a strong family influence such as family size and parental history of chronic diseases. This indicates the importance of addressing families in Saudi Arabia in any public health interventions aiming to address BMI abnormalities. Additionally, adolescents can be highly influenced by school environment and peer pressure, including bullying and stigmatization, leading them to adopt unhealthy eating practices and abnormal weight perception.23 Furthermore, adolescents can be exposed to higher levels of body weight related stigma and stress when considering the risk of exposure to body weight shaming messages in the social media.24,25 It is possible to argue that initiatives that include application of an intervention on individual basis among adolescents in Saudi Arabia might be less successful in comparison to initiatives that address several social determinants associated with BMI of adolescents while ensuring multi-sectorial collaboration.
Public health interventions aiming to address BMI abnormalities among adolescents should develop a strategy to identify groups with high risk of developing BMI abnormalities, and to ensure multi-sectorial collaboration that involve families, schools, communities, healthcare providers, and proper utilization of the media to promote healthy lifestyle among the adolescents. Finally, public health interventions aiming to address BMI abnormalities should be followed by subjective assessment of the effectiveness of these initiative to allow for proper planning for future subsequent public health initiatives.
Strengths and Limitations
The current study had multiple areas of strengths and weaknesses. The main strengths were related to using an online approach to enhance the study’s ability to reach a sample of adolescents with various degrees of body weight, including underweight, normal weight, and overweight and obese adolescents. The current study provides a baseline for BMI profiling among adolescents, which is important to the future study of variations in adolescent BMI trends. The study’s main weakness was the possibility of selection bias by utilizing an online approach. Nonetheless, it can be argued that the younger population in Saudi Arabia has good access to internet services and can thus participate in the study. Finally, there is a possibility of measurement bias concerning the utilization of self-reported body weight and height compared to the utilization of objective assessments of the height and weight of the participants.
Conclusion
The current investigation detected a relatively higher frequency of BMI abnormality among adolescents in the region, including a high prevalence of underweight or overweight and obesity. Dietary behavior among the recruited adolescents suggests the presence of several unhealthy behaviors, such as skipping breakfast and high consumption of energy-dense food items. The current research found that the family was an important influence on adolescents’ weight status. The health authorities in Jazan are advised to implement strategies that ensure the whole family’s involvement when addressing adolescents’ BMI abnormalities.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study received no support from any funding source.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Wold Health Organization. Obesity and overweight. 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
2. Saudi Ministry of Health. World health survey; 2019. Available from: https://www.moh.gov.sa/en/Ministry/Statistics/Population-Health-Indicators/Documents/World-Health-Survey-Saudi-Arabia.pdf.
3. Gosadi IM. Assessment of the environmental and genetic factors influencing prevalence of metabolic syndrome in Saudi Arabia. Saudi Med J. 2016;37(1):12–20. doi:10.15537/smj.2016.1.12675
4. Al-Hussaini A, Bashir MS, Khormi M, et al. Overweight and obesity among Saudi children and adolescents: where do we stand today? Saudi J Gastroenterol. 2019;25(4):229–235. doi:10.4103/sjg.SJG_617_18
5. Habbab RM, Bhutta ZA. Prevalence and social determinants of overweight and obesity in adolescents in Saudi Arabia: a systematic review. Clin Obesity. 2020;10(6):e12400. doi:10.1111/cob.12400
6. El Mouzan MI, Al Herbish AS, Al Salloum AA, Al Omar AA, Qurachi MM. Regional variation in prevalence of overweight and obesity in Saudi children and adolescents. Saudi J Gastroenterol. 2012;18(2):129–132. doi:10.4103/1319-3767.93818
7. Cockerham WC. Theoretical approaches to research on the social determinants of obesity. Am J Prev Med. 2022;63(1 Suppl 1):S8–S17. doi:10.1016/j.amepre.2022.01.030
8. Centers for Disease Control and Prevention. Causes of Obesity; 2022. Available from: https://www.cdc.gov/obesity/basics/causes.html.
9. World Health Organization. Malnutrition. Available from: https://www.who.int/health-topics/malnutrition#tab=tab_1.
10. Abdullah A. The double burden of undernutrition and overnutrition in developing countries: an update. Current Obesity Reports. 2015;4(3):337–349. doi:10.1007/s13679-015-0170-y
11. Hijji TM, Saleheen H, AlBuhairan FS. Underweight, body image, and weight loss measures among adolescents in Saudi Arabia: is it a fad or is there more going on? International Journal of Pediatrics & Adolescent Medicine. 2021;8(1):18–24. doi:10.1016/j.ijpam.2020.01.002
12. Martini MCS, Assumpção D, Barros MBA, Mattei J, Barros Filho AA. Prevalence of body weight dissatisfaction among adolescents: a systematic review. Rev Paul Pediatr. 2022;41:e2021204.
13. Al-Shehri FS, Moqbel MM, Al-Khaldi YM, et al. Prevention and management of obesity: Saudi guideline update. Saudi J Obesity. 2016;4(1):15. doi:10.4103/2347-2618.184970
14. de Lauzon B, Romon M, Deschamps V, et al. The three-factor eating questionnaire-R18 is able to distinguish among different eating patterns in a general population. J Nutr. 2004;134(9):2372–2380. doi:10.1093/jn/134.9.2372
15. Farghaly NF, Ghazali BM, Al-Wabel HM, Sadek AA, Abbag FI. Life style and nutrition and their impact on health of Saudi school students in Abha, Southwestern region of Saudi Arabia. Saudi Med J. 2007;28(3):415–421.
16. Mahfouz AA, Shatoor AS, Hassanein MA, Mohamed A, Farheen A. Gender differences in cardiovascular risk factors among adolescents in Aseer region, southwestern Saudi Arabia. J Saudi Heart Assoc. 2012;24(2):61–67. doi:10.1016/j.jsha.2011.09.002
17. Rodríguez-Cortés FJ, Morales-Cané I, Rodríguez-Muñoz PM, et al. Individual circadian preference, eating disorders and obesity in children and adolescents: a dangerous liaison? A systematic review and a meta-analysis. Children. 2022;9(2):doi:10.3390/children9020167
18. Tojjar J, Norström F, Myléus A, Carlsson A. The impact of parental diabetes on the prevalence of childhood obesity. Child Obes. 2020;16(4):258–264. doi:10.1089/chi.2019.0278
19. Vitoratou DI, Mavrogianni C, Karatzi K, et al. Do parental risk factors for type 2 diabetes predict offspring risk of overweight and obesity? The feel4diabetes study. Nutrition. 2023;107:111900. doi:10.1016/j.nut.2022.111900
20. Lee JS, Jin MH, Lee HJ. Global relationship between parent and child obesity: a systematic review and meta-analysis. Clin Exp Pediatr. 2022;65(1):35–46. doi:10.3345/cep.2020.01620
21. Moschonis G, Siopis G, Anastasiou C, et al. Prevalence of childhood obesity by country, family socio-demographics, and parental obesity in Europe: the feel4diabetes study. Nutrients. 2022;14(9):1830. doi:10.3390/nu14091830
22. Almubark RA, Alqahtani SA. Obesity epidemiology and interventions in Saudi Arabia. East Mediterr Health J. 2023;29(12):987–994. doi:10.26719/emhj.23.086
23. Skogen IB, Båtevik FO, Krumsvik RJ, Høydal KL. Weight-based victimization and physical activity among adolescents with overweight or obesity: a scoping review of quantitative and qualitative evidence. Front Sport Active Liv. 2022;4:732737. doi:10.3389/fspor.2022.732737
24. Lessard LM, Puhl RM. Adolescents’ exposure to and experiences of weight stigma during the COVID-19 pandemic. J Pediatr Psychol. 2021;46(8):950–959. doi:10.1093/jpepsy/jsab071
25. Clark O, Lee MM, Jingree ML, et al. Weight stigma and social media: evidence and public health solutions. Front Nutr. 2021;8:739056. doi:10.3389/fnut.2021.739056
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
