Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 16
Blood Lipid Disorders in Post-Operative Craniopharyngioma Children and Adolescents and the Improvement with Recombinant Human Growth Hormone Replacement
Authors Du HZ, Chen K, Zhang LY, Zhang YL, Wu DN, Guo XY, Duan L, Wang LJ, Yang HB, Chen S, Pan H , Zhu HJ
Received 11 June 2023
Accepted for publication 21 September 2023
Published 3 October 2023 Volume 2023:16 Pages 3075—3084
DOI https://doi.org/10.2147/DMSO.S425399
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Antonio Brunetti
Han-Ze Du,1,* Kang Chen,1,* Li-Yuan Zhang,1,* Yue-Lun Zhang,2 Dan-Ning Wu,1 Xiao-Yuan Guo,1 Lian Duan,1 Lin-Jie Wang,1 Hong-Bo Yang,1 Shi Chen,1 Hui Pan,1 Hui-Juan Zhu1
1Key Laboratory of Endocrinology of National Health Commission, Department of Endocrinology, State Key Laboratory of Complex Severe and Rare Diseases, Peking Union Medical College Hospital, Chinese Academy of Medical Science & Peking Union Medical College, Beijing, People’s Republic of China; 2Medical Research Center, Peking Union Medical College Hospital, Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hui Pan; Hui-Juan Zhu, Key Laboratory of Endocrinology of National Health Commission, Department of Endocrinology, State Key Laboratory of Complex Severe and Rare Diseases, Peking Union Medical College Hospital, Chinese Academy of Medical Science & Peking Union Medical College, No. 1 Shuaifuyuan, Wangfujing Street, Dongcheng District, Beijing, 100730, People’s Republic of China, Email [email protected]; [email protected]
Context: The high prevalence of hypothalamic obesity (HO) and dyslipidemia in individuals with craniopharyngioma (CP) following surgery is a cause for increasing concern. However, few studies have explored the lipid profile in pediatric CP patients, with inconsistent findings. In addition, the role of recombinant human growth hormone (rhGH) replacement remains unclear in these patients.
Objective: To compare the blood lipid profile among post-operative craniopharyngioma children and adolescents with that among healthy controls and to reveal the effects of rhGH replacement.
Methods: Data of 79 post-operative craniopharyngioma children and adolescents in our center were retrospectively collected. Sixty patients underwent rhGH replacement during the follow-ups. We selected 36 patients who received rhGH replacement therapy, while 20 patients received rhGH replacement for at least 1 year and had complete lipid data before and after treatment and compared them with 19 patients who did not receive rhGH replacement therapy.
Results: Craniopharyngioma patients had higher total cholesterol (TC) (5.17 vs 3.77 mmol/L), triglyceride (TG) (1.51 vs 0.73 mmol/L), and low-density lipoprotein cholesterol (LDL-C) (3.14 vs 2.10 mmol/L), and lower high-density lipoprotein cholesterol (HDL-C) (1.06 vs 1.39 mmol/L) than controls (all p < 0.001). The lipid profile of obese and non-obese patients was not significantly different. After rhGH replacement, TC was 0.90 mmol/L lower (p = 0.002) and LDL-C was 0.73 mmol/L lower (p = 0.010) than baseline. Although the baseline LDL-C was higher, patients with rhGH replacement had lower LDL-C (− 0.73 mmol/L adjusted for age and sex, p = 0.045) after the initiation of replacement compared with patients without rhGH replacement.
Conclusion: The lipid profile of obese and non-obese children and adolescents with craniopharyngioma was unfavorable, and rhGH replacement could improve their lipid profile.
Keywords: craniopharyngioma, dyslipidemias, obesity, human growth hormone, hypothalamic obesity
Introduction
Craniopharyngiomas (CPs) are brain tumors arising from the remnants of Rathke’s pouch,1 accounting for about 10% of childhood brain tumors. Approximately 30–50% of the CP cases were seen in children and adolescents.2,3 CPs are usually located at the sellar region and the patients often have pituitary hormone deficiency, which can be caused by the tumor per se or by treatments such as surgery and/or radiotherapy.1 Notably, physical destruction of the hypothalamus can cause abnormal weight gain, known as hypothalamic obesity (HO), and about half of the CP children develop HO after such a surgery.4
This change in the rate of weight gain is rapid and can be detected within weeks or months. In addition to the damage of hypothalamus and pituitary, the lack of pituitary hormones and the change of lifestyle are also important factors in the occurrence of obesity. Obesity and impaired lipid metabolism are associated with high risks of cardiovascular diseases (CVDs), which explains the higher mortality among CP patients than the general population.5–7 A better understanding of abnormal lipid metabolism in CP patients may reveal the origin of obesity. However, few studies have explored the lipid profile in pediatric CP patients, with inconsistent findings. Some authors found that triglyceride (TG) was significantly higher in CP children than in healthy controls,4,8 others demonstrated that TG, low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C) were not significantly different between CP patients and controls.9
Growth hormone (GH) deficiency is common among CP patients.1 While recombinant human GH (rhGH) replacement has been found to favour the height of CP patients,10 its effect on lipid profile has not yet been thoroughly studied. While a few studies have described the results among adult patients,11–13 only one study tried to explore the effects of rhGH replacement on metabolic parameters in pediatric CP patients; unfortunately, it failed to draw definite conclusions due to its small sample size and cross-sectional design.4 Thus, the effects of rhGH replacement on the blood lipid of CP children remained unclear.
The aim of our present study was to compare the blood lipid profiles of post-operative CP children and adolescents with those of age-, sex-, and body mass index (BMI)-matched healthy controls. We also reveal the effects of rhGH on lipid profile in post-operative CP children and adolescents.
Methods
Subjects
The follow-up data of CP patients who were treated in our center from 2009 to 2020 were retrospectively collected. Patients who met the following criteria were included: (i) having undergone CP resection in our center or other institutions; (ii) aged ≤20 years at the first visit to our hospital; and (iii) having blood lipid profile measured at least once in our center. The data at the first visit in our center were used for the comparisons with healthy controls. None of the patients were taking lipid-lowering drugs at the first visit. For each patient, two age-, sex-, and BMI-matched (age ± 2 years, BMI ± 1 kg/m2) controls were randomly selected from a database of health check-ups for students from primary and secondary schools in Pinggu District, Beijing, China. The study involving human participants was reviewed and approved by the Ethics Committee of our hospital (K2917).
Laboratory Measurements
Lipid profile including total cholesterol (TC), TG, HDL-C, and LDL-C was measured using an automatic analyzer (Cobas 8000, Roche). The blood samples of all follow-up visits were determined by fasting in the morning. Insulin-like growth factor 1 (IGF-1) was measured with chemiluminescence assay (Immulite 2000, Siemens).
Anthropometric Measurements
Body height and weight were measured with light clothing, and BMI was calculated accordingly. The standard deviation score (SDS) for BMI was determined according to the reference curves of Chinese children and adolescents.14 BMI ≥85th and <95th percentile was considered to be overweight, and BMI ≥95th percentile was considered to be obese.
Pituitary Hormone Deficiency
Thyroid-stimulating hormone deficiency: the decrease of free thyroxine (FT4) was accompanied by normal or decreased thyrotropin.15 Adrenocorticotropic hormone deficiency: when cortisol (COR) <3µg/dL in the morning, or ITT blood glucose <40mg/dL (2.2mmol/L), COR <18 µg/dL.16 Central diabetes insipidus is defined as the concomitant presence of inappropriate hypotonic polyuria (urine output >3 L/24 h and urine specific gravity <1.005) in the presence of high or normal serum sodium (>145 mmol/L).17 Gonadotropin deficiency: decreased FSH and LH in children; testosterone (TEST) decreased with abnormal follicle-stimulating hormone (FSH), luteinizing hormone (LH), and prolactin (PRL) levels in adult male patients, and estradiol (E2) decreased with normal or decreased FSH and LH or abnormal PRL in female patients.18
rhGH Replacement
Data of 79 post-operative CP children and adolescents in our center during the period from 2009 to 2020 were retrospectively collected. Sixty of them underwent rhGH replacement during the follow-ups, and 36 patients had records of blood lipid measurement both before and after the initiation of rhGH replacement. Among these 36 patients, 20 patients received the rhGH replacement for at least 1 year (rhGH replacement group). The remaining 19 patients did not receive any rhGH replacement (non-rhGH replacement group). The changes in blood lipid profile in these two groups were observed and compared. We started GH replacements when the patients were: One year after surgery, the tumor did not recur or progress, and the height was lower than −2 standard deviation (SD).19
Statistical Analysis
Normality of the variables was tested by Shapiro–Wilk test. Normal variables were reported as mean ± standard deviation (SD) and non-normal variables as median (the first quartile, the third quartile). Differences in baseline characteristics were measured by standardized difference, and variables with standardized difference below 10% were considered to be balanced. Comparisons of lipid profiles between CP patients and controls and comparisons of parameters before and after rhGH replacement were conducted by paired t-test or Wilcoxon test. Obese and non-obese CP patients were compared by unpaired t-test or Mann–Whitney U-test. Linear mixed model (LMM) was used to compare the lipid profile during follow-ups in patients with or without rhGH replacement after adjusting for confounding factors. A P-value below 0.05 was considered statistically significant.
Results
A total of 79 patients were included according to the inclusion criteria, including 50 boys (63.3%) and 29 (36.7%) girls aged 12.5 (8.5, 14.8) years. They underwent their surgeries at the age of 8.3 (5.3, 12.2) years, and the median time since the surgeries was 26 [8, 58] months. Three of the patients (3.8%) underwent radiotherapy. Among the pituitary hormone deficiencies, thyroid-stimulating hormone deficiency was the most common type (n = 76, 96.2%), followed by adrenocorticotropic hormone deficiency (n = 73, 92.4%), central diabetes insipidus (n = 68, 86.1%), and gonadotropin deficiency (n = 23, 29.1%).
CP Patients versus Healthy Controls
Data on BMI at the first visit were available in 66 patients, among whom 60 patients were paired to age-, sex-, and BMI-matched controls. The remaining six patients had no matched controls due to their younger age or higher BMI. CP patients had significantly higher TC, TG, and LDL (all P<0.001) and lower HDL (P<0.001) than healthy controls (Table 1).
 |
Table 1 Comparison of Clinical Characteristics and Lipid Profile of Craniopharyngioma Patients and Healthy Controls |
Obese CP Patients versus Non-Obese CP Patients
The 66 patients with BMI data had a mean BMI of 22.95 ± 4.59 kg/m2 and a mean BMI-SDS of 1.5 ± 1.5. Patients were also divided into obese group (n = 44, including 31 [47.0%] obese patients and 13 [19.7%] overweight patients) and non-obese group (n = 22), and the clinical characteristics and lipid profiles were compared between these two groups (Table 2). Patients in the obese group were younger, and their intervals between the surgery and the first visit in our hospital were shorter. TC, TG, HDL, and LDL were not significantly different between these two groups, but LDL tended to be higher in the obese group, although the difference was not statistically significant (P=0.056). Notably, post-operative patients in the non-obese group still had significantly higher TC, TG, and LDL than healthy controls (Table 3).
 |
Table 2 Comparison of Clinical Characteristics and Lipid Profiles of Obese and Non-Obese Craniopharyngioma Patients |
 |
Table 3 Comparison of Clinical Characteristics and Lipid Profile of Non-Obese Craniopharyngioma Patients and Healthy Controls |
Before versus After rhGH Replacement
For the 20 CP patients in the rhGH replacement group, the duration of rhGH replacement was 33 (21, 48) months. The lipid profile at the first visit after the cessation of rhGH replacement or the last visit during the replacement was compared with that at the last follow-up before the initiation of rhGH replacement (set as the baseline). As listed in Table 4, TC reduced by 0.90 ± 1.13 mmol/L (P=0.002) and LDL-C reduced by 0.73 ± 1.14 mmol/L (P=0.010) compared with the baseline values, while the changes of TG and HDL-C were not statistically significant. IGF-1 also significantly increased after rhGH replacement (P=0.004), but the correlation between the change in IGF-1 and the change in TC or LDL-C was not significant (Pearson r = 0.098, P = 0.697 and Pearson r = 0.217, P = 0.387). The changes in BMI and BMI SDS before and after rhGH replacement were not statistically significant.
 |
Table 4 The Comparison of Lipid Profile Before and After rhGH Replacement Among Craniopharyngioma Patients with rhGH Replacement of at Least 1 Year (n = 20) |
rhGH Replacement Group versus Non-rhGH Replacement Group
After the initiation of rhGH replacement in the rhGH replacement group, the median time of follow-up was 49 (32, 75) months, and the median number of blood lipid measurements was 2 (1, 3) times. In contrast, the non-rhGH replacement group had a median follow-up period of 7 [6, 21] months and a median blood lipid measurement of 2 (2, 3) times.
The clinical characteristics and lipid profile at the first visit are shown in Table 5. Age, sex and BMI SDS were imbalanced between these two groups, while the IGF-1 was balanced. As for the lipid profile, the rhGH replacement group had significantly higher TC, HDL-C and LDL-C and significantly lower TG at the first visit.
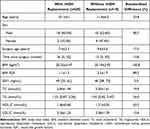 |
Table 5 Clinical Characteristics and Lipid Profile of Craniopharyngioma Patients with and without rhGH Replacement at the First Follow-Up |
The visits after the initiation of rhGH replacement in the rhGH replacement group and all the visits in the non-rhGH replacement group were used in the linear mixed models (LMMs) (Table 6). After adjusting for age, TG was 0.77 mmol/L lower (P=0.020), and LDL-C was 0.68 mmol/L lower (P=0.033) in the rhGH replacement group than in the non-rhGH replacement group, while TC and HDL-C showed no significant difference. After further adjusting for sex, LDL-C was still significantly lower in the rhGH replacement group (P=0.045). Furthermore, LDL-C tended to be lower in the rhGH replacement group after adjusting for both age and BMI SDS, although the difference was not statistically significant (P=0.063). HDL-C was significantly higher in the rhGH replacement group only after adjusting for age and sex.
 |
Table 6 Difference in Lipid Profile During Follow-Ups Between Patients with and without rhGH Replacement |
Discussion
To the best of our knowledge, this is the largest study to compare the lipid profile of CP patients with that of healthy controls. We confirmed that the lipid profile was more unfavorable in children and adolescents with CP than in healthy controls. CP patients had improved lipid profiles after rhGH replacement, and their lipid profiles during the follow-ups were more favorable than those of CP patients without rhGH replacement.
Obesity is a risk factor for a host of metabolic disturbances that involve conditions such as cardiovascular diseases, type 2 diabetes, cancer, and, most recently, COVID-19.20 Lipid metabolism is controlled by independent sympathetic and parasympathetic neurons derived from the paraventricular nucleus and suprachiasmatic nucleus, with sympathetic neurons inhibiting its decomposition and parasympathetic neurons promoting its decomposition. In CP patients receiving surgery and/or radiotherapy, damage to the hypothalamus causes the injury of suprachiasmatic nucleus region, resulting in abnormal appetite control, reduced energy expenditure, and impairment of the autonomic nervous system,21 known as hypothalamic obesity (HO), which can greatly undermine the quality of life of CP patients.1 In addition, the prevalence of obesity among children and adolescents with CP after surgery ranged from 53% to 73%,4,22,23 which was similar to our findings.
The lipid profile of pediatric CP patients has been investigated in literature but with contradictory findings. In two studies, pediatric CP patients had higher TG and lower HDL-C/TC ratio compared with age-, sex-, BMI-, and pubertal stage-matched healthy controls,4,8 but TG was not significantly different in another study with similar design, probably due to the limited number of subjects.9 Data on HDL-C in pediatric CP patients were available in two studies, but no significant difference was reported.8,9 Only one study reported the data of LDL-C, and the difference was not significant.9 Since CP is rarely seen in clinical settings, the limited number of CP patients made the conclusions of relevant studies less persuasive. With a larger sample size, our current study had more reliable findings. However, considering the heterogenous nature of CP and the unavailability of pre-operative data in our present study, we are not sure whether other factors related to metabolic status such as pre-operative BMI and the extent of hypothalamus involvement in our present study differed from those in previous studies.24,25
It was found in our present study that pediatric post-operative CP patients had unfavorable lipid profile, with TG, TC, HDL-C, and LDL-C significantly different from those in healthy controls. Obese and non-obese CP patients had similarly affected lipid profile, and non-obese patients also had poorer lipid profile than healthy controls, indicating dyslipidemia in post-operative CP children might be generally independent of obesity. A previous study has demonstrated that childhood-onset CP patients had abnormal lipid profile in their adulthood,11 and our study showed that dyslipidemia was also present in the childhood. The long-lasting dyslipidemia may partly explain the increased risk for CVD among CP patients. Therefore, monitoring and management of lipid profile should be timely initiated for children and adolescents with CPs, even if their BMI is normal.
We also explored the effect of rhGH replacement on lipid profile in children and adolescents with CP. Blood lipids change with age in the childhood.26 Unlike height and weight, there have not yet been widely accepted reference curves of blood lipids for children and adolescents in China, and how the lipid profile of CP patients changes with age remains unclear. Moreover, our study had a retrospective design, with imbalanced baseline characteristics. Therefore, we used LMMs to adjust for the age and BMI or sex, which has been found to be related to the lipid profile.26,27 We found that patients with rhGH replacement had lower LDL-C after the initiation of replacement after adjusting for age, and this tendency still existed after adjusting for more confounding factors, which was also consistent with the self-controlled result. Considering the fact that the baseline LDL-C was even higher in the rhGH replacement group, we assume that rhGH replacement may indeed lower LDL-C in pediatric CP patients. In addition, due to the limited number of patients, the statistical power of our data was compromised in the models adjusting for more confounding factors, and the interaction between the rhGH replacement and the change of lipid profile with age was not analyzed. It is still unclear whether the rates of change of blood lipids over time were different among patients with and without rhGH replacement.
The effects of rhGH replacement on CP patients are complicated. While most studies revealed that rhGH replacement was beneficial to body height in pediatric patients, its influences on weight and BMI were inconsistent across studies,10,28–30 suggesting the responses of the metabolic status to rhGH replacement can be highly variable among CP patients. Some studies have attempted to explore the effect of rhGH replacement on the lipid profile of adult CP patients. Two studies demonstrated that TC and LDL-C were significantly lowered after rhGH replacement,11,12 while such changes were not significant in another study.13 rhGH may have different effects on height or body composition when used in children and adults or in childhood-onset and adult-onset CP patients.10,31 In our present study, rhGH replacement showed beneficial effects on the lipid profile of children and adolescents with CPs, which was similar to findings in adults.11,12
A small number of articles have investigated the role of rhGH replacement in pediatric CP patients. There had been concerns that it might increase the recurrence rates of CPs, but recent studies clarified that physiological doses of rhGH were safe for CP patients.10,32 Previous studies showed that rhGH replacement in pediatric CPs could improve the height and quality of life.10,28–30 In our present study, rhGH replacement partly reversed the unfavorable lipid profile, especially LDL-C, in pediatric CP patients, which may reduce the long-term risk for CVDs. Moreover, although some studies found that rhGH replacement increased BMI in CP patients,11,12 our data and some other studies did not support this observation.13,28–30 We believe that the benefits of rhGH replacement outweigh its risks. Moreover, the improvement of lipid metabolism by rhGH also suggests a potential role of rhGH in the treatment of dyslipidemia.
Our present study had some limitations. As pre-operative data were not available in most of our patients, we could neither compare the lipid profile before and after the surgeries nor could we analyze the influences of factors such as hypothalamus involvement, duration of disease, and pre-operative BMI on the post-operative lipid profile. Besides, the baseline data before rhGH treatment were not available in some patients with rhGH replacement, and therefore the number of patients in the rhGH replacement group was limited, making it impossible to perform more rigorous analyses (eg, the interaction between the rhGH replacement and the rate of change of lipid profile with age).
In conclusion, blood lipid disorders are common in children and adolescents with obese or non-obese post-operative CPs, and the lipid profile is unfavorable in both CPs. rhGH replacement may improve lipid profile in these patients. Dyslipidemia should not be ignored during childhood, even in pediatric CP patients without obesity. Future studies should consider preoperative data and larger sample sizes to improve the understanding for the effects of rhGH replacement therapy on lipid profile.
Abbreviations
rhGH, Recombinant human growth hormone; CPs, Craniopharyngiomas; HO, Hypothalamic obesity; CVD, Cardiovascular disease; SDS, Standard deviation score; TC, Total cholesterol; TG, Triglyceride; HDL-C, High-density lipoprotein cholesterol; LDL-C, Low-density lipoprotein cholesterol; LMM, Linear mixed model.
Data Sharing Statement
The datasets generated and/or analyzed during this study are not publicly available because they contain information that could compromise the privacy of the research participants. The data are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
The study involving human participants was reviewed and approved by the Ethics Committee of Peking Union Medical College Hospital (K2917), which conformed to the provision of the Declaration of Helsinki. After explaining the purpose of the study, written informed consent was obtained from each study participant. Assent was also obtained from adolescent participants and legal guardian.
Consent to Participate
All participants provided written informed consent and completed the questionnaires as required.
Acknowledgments
We sincerely thank the teachers at the Peking Union Medical College Hospital for their help with this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by the National High Level Hospital Clinical Research Funding (2022-PUMCH-154).
Disclosure
The authors declared no conflicts of interest in this work.
References
1. Müller HL, Merchant TE, Warmuth-Metz M, et al. Craniopharyngioma. Nat Rev Dis Primers. 2019;5(1):75. doi:10.1038/s41572-019-0125-9
2. Bunin GR, Surawicz TS, Witman PA, et al. The descriptive epidemiology of craniopharyngioma. J Neurosurg. 1998;89(4):547–551. doi:10.3171/jns.1998.89.4.0547
3. Kuratsu J, Ushio Y. Epidemiological study of primary intracranial tumors: a regional survey in Kumamoto Prefecture in the southern part of Japan. J Neurosurg. 1996;84(6):946–950. doi:10.3171/jns.1996.84.6.0946
4. Srinivasan S, Ogle GD, Garnett SP, et al. Features of the metabolic syndrome after childhood craniopharyngioma. J Clin Endocrinol Metab. 2004;89(1):81–86. doi:10.1210/jc.2003-030442
5. Erfurth EM, Holmer H, Fjalldal SB. Mortality and morbidity in adult craniopharyngioma. Pituitary. 2013;16(1):46–55. doi:10.1007/s11102-012-0428-2
6. Bülow B, Attewell R, Hagmar L, et al. Postoperative prognosis in craniopharyngioma with respect to cardiovascular mortality, survival, and tumor recurrence. J Clin Endocrinol Metab. 1998;83(11):3897–3904. doi:10.1210/jcem.83.11.5240
7. Abdu TA, Neary R, Elhadd TA, et al. Coronary risk in growth hormone deficient hypopituitary adults: increased predicted risk is due largely to lipid profile abnormalities. Clin Endocrinol. 2001;55(2):209–216. doi:10.1046/j.1365-2265.2001.01320.x
8. Sahakitrungruang T, Klomchan T, Supornsilchai V, et al. Obesity, metabolic syndrome, and insulin dynamics in children after craniopharyngioma surgery. Eur J Pediatr. 2011;170(6):763–769. doi:10.1007/s00431-010-1347-8
9. Simoneau-Roy J, O’Gorman C, Pencharz P, et al. Insulin sensitivity and secretion in children and adolescents with hypothalamic obesity following treatment for craniopharyngioma. Clin Endocrinol. 2010;72(3):364–370. doi:10.1111/j.1365-2265.2009.03639.x
10. Boekhoff S, Bogusz A, Sterkenburg AS, et al. Long-term effects of growth hormone replacement therapy in childhood-onset craniopharyngioma: results of the German Craniopharyngioma Registry (HIT-Endo). Eur J Endocrinol. 2018;179(5):331–341. doi:10.1530/EJE-18-0505
11. Yuen KC, Koltowska-Häggström M, Cook DM, et al. Clinical characteristics and effects of GH replacement therapy in adults with childhood-onset craniopharyngioma compared with those in adults with other causes of childhood-onset hypothalamic-pituitary dysfunction. Eur J Endocrinol. 2013;169(4):511–519. doi:10.1530/EJE-13-0280
12. Verhelst J, Kendall-Taylor P, Erfurth EM, et al. Baseline characteristics and response to 2 years of growth hormone (GH) replacement of hypopituitary patients with GH deficiency due to adult-onset craniopharyngioma in comparison with patients with nonfunctioning pituitary adenoma: data from KIMS (Pfizer International Metabolic Database). J Clin Endocrinol Metab. 2005;90(8):4636–4643. doi:10.1210/jc.2005-0185
13. Profka E, Giavoli C, Bergamaschi S, et al. Analysis of short- and long-term metabolic effects of growth hormone replacement therapy in adult patients with craniopharyngioma and non-functioning pituitary adenoma. J Endocrinol Invest. 2015;38(4):413–420. doi:10.1007/s40618-014-0196-0
14. Li H, Ji CY, Zong XN, et al. Body mass index growth curves for Chinese children and adolescents aged 0 to 18 years. Zhonghua Er Ke Za Zhi. 2009;47(7):493–498.
15. Alexopoulou O, Beguin C, De Nayer P, et al. Clinical and hormonal characteristics of central hypothyroidism at diagnosis and during follow-up in adult patients. Eur J Endocrinol. 2004;150(1):1–8. doi:10.1530/eje.0.1500001
16. Fleseriu M, Hashim IA, Karavitaki N, et al. Hormonal replacement in hypopituitarism in adults: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2016;101(11):3888–3921. doi:10.1210/jc.2016-2118
17. Burke WT, Cote DJ, Penn DL, et al. Diabetes insipidus after endoscopic transsphenoidal surgery. Neurosurgery. 2020;87(5):949–955. doi:10.1093/neuros/nyaa148
18. Brambilla DJ, Matsumoto AM, Araujo AB, et al. The effect of diurnal variation on clinical measurement of serum testosterone and other sex hormone levels in men. J Clin Endocrinol Metab. 2009;94(3):907–913. doi:10.1210/jc.2008-1902
19. The Expert Consensus Preparation Committee for Craniopharyngioma Treatment, along with the Pediatric Neurosurgery Group of the Chinese Society of Neurosurgery. Expert Consensus on Long-term Endocrine Therapy for patients with craniopharyngioma. Chin Med J. 2018;98(1):8.
20. Aghili SMM, Ebrahimpur M, Arjmand B, et al. Obesity in COVID-19 era, implications for mechanisms, comorbidities, and prognosis: a review and meta-analysis. Int J Obes. 2021;45(5):1–19.
21. Otte A, Müller HL. Childhood-onset craniopharyngioma. J Clin Endocrinol Metab. 2021;106(10):e3820–e3836. doi:10.1210/clinem/dgab397
22. Kalina MA, Skala-Zamorowska E, Kalina-Faska B, et al. Practical approach to childhood craniopharyngioma: a role of an endocrinologist and a general paediatrician. Childs Nerv Syst. 2009;25(9):1053–1060. doi:10.1007/s00381-009-0931-6
23. Poretti A, Grotzer MA, Ribi K, et al. Outcome of craniopharyngioma in children: long-term complications and quality of life. Dev Med Child Neurol. 2004;46(4):220–229. doi:10.1111/j.1469-8749.2004.tb00476.x
24. Müller HL, Gebhardt U, Teske C, et al. Post-operative hypothalamic lesions and obesity in childhood craniopharyngioma: results of the multinational prospective trial KRANIOPHARYNGEOM 2000 after 3-year follow-up. Eur J Endocrinol. 2011;165(1):17–24. doi:10.1530/EJE-11-0158
25. Müller HL, Bueb K, Bartels U, et al. Obesity after childhood craniopharyngioma--German multicenter study on pre-operative risk factors and quality of life. Klin Padiatr. 2001;213(4):244–249. doi:10.1055/s-2001-16855
26. Li Y, Ma Y, Luo J, et al. Identifying reference values for serum lipids in Chinese children and adolescents aged 6–17 years old: a national multicenter study. J Clin Lipidol. 2021;15(3):477–487. doi:10.1016/j.jacl.2021.02.001
27. DeStefano F, Berg RL, Griese GG. Determinants of serum lipid and lipoprotein concentrations in children. Epidemiology. 1995;6(4):446–449. doi:10.1097/00001648-199507000-00024
28. Heinks K, Boekhoff S, Hoffmann A, et al. Quality of life and growth after childhood craniopharyngioma: results of the multinational trial KRANIOPHARYNGEOM 2007. Endocrine. 2018;59(2):364–372. doi:10.1007/s12020-017-1489-9
29. Price DA, Wilton P, Jönsson P, et al. Efficacy and safety of growth hormone treatment in children with prior craniopharyngioma: an analysis of the Pharmacia and Upjohn International Growth Database (KIGS) from 1988 to 1996. Horm Res. 1998;49(2):91–97. doi:10.1159/000023133
30. Geffner M, Lundberg M, Koltowska-Häggström M, et al. Changes in height, weight, and body mass index in children with craniopharyngioma after three years of growth hormone therapy: analysis of KIGS (Pfizer International Growth Database). J Clin Endocrinol Metab. 2004;89(11):5435–5440. doi:10.1210/jc.2004-0667
31. Attanasio AF, Bates PC, Ho KK, et al. Human growth hormone replacement in adult hypopituitary patients: long-term effects on body composition and lipid status--3-year results from the HypoCCS Database. J Clin Endocrinol Metab. 2002;87(4):1600–1606. doi:10.1210/jcem.87.4.8429
32. Smith TR, Cote DJ, Jane JA, et al. Physiological growth hormone replacement and rate of recurrence of craniopharyngioma: the Genentech National Cooperative Growth Study. J Neurosurg Pediatr. 2016;18(4):408–412. doi:10.3171/2016.4.PEDS16112
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
