Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 17
Blood Eosinophils in Chinese COPD Participants and Response to Treatment with Combination Low-Dose Theophylline and Prednisone: A Post-Hoc Analysis of the TASCS Trial
Authors Bradbury T , Di Tanna GL , Scaria A, Martin A, Wen FQ, Zhong NS, Zheng JP , Barnes PJ, Celli B, Berend N, Jenkins CR
Received 22 September 2021
Accepted for publication 24 December 2021
Published 5 February 2022 Volume 2022:17 Pages 273—282
DOI https://doi.org/10.2147/COPD.S339889
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Professor Min Zhang
Thomas Bradbury,1 Gian Luca Di Tanna,1 Anish Scaria,1 Allison Martin,1 Fu-Qiang Wen,2 Nan-Shan Zhong,3 Jin-Ping Zheng,3 Peter J Barnes,4 Bartolome Celli,5 Norbert Berend,1 Christine R Jenkins1 On behalf of the TASCS Investigators
1Respiratory Group, The George Institute for Global Health, Sydney, NSW 2042, Australia; 2West China Hospital, Sichuan University, Chengdu, People’s Republic of China; 3State Key Laboratory of Respiratory Disease, National Clinical Research Centre for Respiratory Disease, First Affiliated Hospital of Guangzhou Medical University, Guangzhou, People’s Republic of China; 4National Heart & Lung Institute, Imperial College, London, UK; 5Pulmonary and Critical Care Division, Brigham and Women’s Hospital and Harvard Medical School, Boston, MA, USA
Correspondence: Thomas Bradbury
Respiratory Group, The George Institute for Global Health, Level 5, 1 King St, Newtown, Sydney, NSW 2042, Australia
, Tel +61 2 8052 4413
, Email [email protected]
Background and Objectives: The burden of chronic obstructive pulmonary disease (COPD) disproportionately affects patients in low to middle-income countries. Although the Theophylline and Steroids in COPD Study (TASCS) showed no clinical benefit from administering low-dose theophylline and prednisone in COPD patients compared to placebo, it was hypothesized that those with elevated blood eosinophil counts would receive clinical benefit from the intervention.
Methods: This was a post-hoc analysis of the TASCS dataset – a double-blinded, placebo-controlled trial conducted in patients with moderate–severe COPD in China. Participants were allocated 1:1:1 to low-dose oral theophylline (100mg bd) and prednisone (5mg qd; PrT), theophylline (100mg bd) and prednisone-matched placebo (TP), or double-matched placebo (DP) groups and followed-up for 48 weeks. A baseline count of ≥ 300 eosinophils/μL blood was categorized as elevated/eosinophilic, and the primary outcome was the annualized moderate-severe exacerbation rate.
Results: Of 1487 participants eligible for analysis, 325 (22%) were eosinophilic. These participants were predominantly male (82%), had a mean (SD) age of 64 (± 8) years and a predicted forced expiratory volume in 1s (FEV1) of 43% (± 16). The annualized moderate–severe exacerbation rate was significantly higher in the PrT group compared to the pooled results of the TP and DP groups (incidence rate ratio = 1.6; ([95% CI 1.06– 1.76]) p = 0.016). Changes in spirometry values and reported disease impact scores (St. George’s Respiratory Questionnaire and COPD Assessment Test) at week 48 were not significantly different between groups.
Conclusion: Combination low-dose theophylline and prednisone was associated with a significant increase in the annual moderate-severe exacerbation rate in participants with a blood eosinophil count ≥ 300 cells/μL compared to placebo.
Keywords: eosinophil, COPD, clinical trial, China, theophylline, prednisone
Introduction
Chronic obstructive pulmonary disease (COPD) continues to be a major cause of morbidity and mortality worldwide, with an estimated prevalence of approximately 3% of the global community in 2019.1 Current guidelines recommend use of long-acting bronchodilators to reduce symptoms and exacerbations, with the addition of inhaled corticosteroids when exacerbations become more frequent, particularly if blood eosinophil counts are raised above 300 cells/µL.2 For significant portions of the global patient population, these pharmacotherapies are often under-utilized due to limited access and affordability – necessitating the use of low-cost alternatives where available.
Previous in vitro and in vivo studies had suggested that the activity of histone deacetylase-2 (HDAC2), a nuclear enzyme that inhibits inflammatory gene expression, is markedly reduced in COPD. By interfering with the anti-inflammatory effects of corticosteroids, HDAC2 can be increased by low concentrations of theophylline, restoring corticosteroid responsiveness.3–6 Thus, it was hypothesized that theophylline could promote anti-inflammatory gene expression and restore sensitivity to glucocorticosteroids in COPD patients, hence improving their response to prednisone. In the absence of access to gold standard bronchodilator therapy, this pharmacologic synergism could potentially provide an affordable and highly accessible management strategy for COPD patients in resource-poor settings.
The “Theophylline And Steroids in COPD Study” (TASCS) was a multicenter randomized control trial undertaken in China to determine if the effect observed in vitro translated into clinical benefit in a large randomized controlled trial. Neither TASCS, nor the “Theophylline With Inhaled Corticosteroids” (TWICS) trial observed a significant treatment effect with the addition of low doses of theophylline with regards to exacerbation rate or risk, lung function or disease-related quality of life and symptom impact questionnaire scores.7,8
However, the pathological heterogeneity of COPD opens the possibility for further investigation of patient subpopulations in whom beneficial effects might occur. Post-hoc analyses of data from randomized controlled trials for COPD pharmacotherapy have previously demonstrated that an elevated blood eosinophil count is associated with an enhanced response to inhaled corticosteroids (ICS).9–15 We performed this post-hoc analysis to determine if a novel maintenance therapy of combination low-dose theophylline and an oral corticosteroid was associated with a reduction in exacerbation frequency in participants with COPD and elevated blood eosinophil counts.
Methods
TASCS has been reported previously.8 Briefly, TASCS (NCT02261727) was a 48-week, multicenter, double-blinded, randomized, parallel study conducted at urban and regional hospitals around China. Study protocol and informed consent procedures were centrally approved by The University of Sydney Human Research Ethics Committee (protocol no. 2012/082) and the institutional review board at each site. All patients provided written informed consent prior to undertaking any study-specific procedures. The study was performed in accordance with the Declaration of Helsinki and Good Clinical Practice.
The primary objective was to determine if a combination of oral prednisone 5mg qd and low-dose theophylline 100mg bd (PrT) was superior to placebo in reducing the annualized rate of acute exacerbations of COPD (AECOPD) at 48 weeks compared to the pooled results (herein referred to as Pooled Placebo; PP) of the double-placebo and low-dose theophylline 100mg and placebo study groups.
Other secondary objectives included change in St. George Respiratory Questionnaire (SGRQ) score, COPD Assessment Test (CAT) score, post-bronchodilator spirometry, safety, and time to first acute exacerbation of COPD.
Participants
Consented and eligible participants were aged 40 to 80 years with a clinical diagnosis of COPD and were current or former smokers with at least 10 pack years or 10 years exposure to other sources of combusted biomass. At screening and baseline, participants had a post-bronchodilator FEV1 <70% predicted and an FEV1/FVC ratio <0.7, and in the prior 12 months had experienced at least one AECOPD that was treated with systemic corticosteroids and/or antibiotics or had led to hospitalization. A full list of inclusion and exclusion criteria can be found in the primary publication.8 Participants were included in this analysis if they had blood eosinophil counts recorded at the screening visit, had been randomized to a treatment group, and had been in follow-up for at least 2 weeks before trial discontinuation.
Endpoints and Assessments
The primary efficacy endpoint was the annualized moderate-severe AECOPD rate. These events were identified when the participant experienced a worsening in health for at least two consecutive days with two or more major symptoms (dyspnea, sputum volume increase, sputum purulence) or a worsening of one major symptom with any one minor symptom (sore throat, nasal discharge, nasal congestion, fever without other cause, cough or wheeze). Severity of the event was graded as (I) mild if addressed with any form of symptomatic treatment, (II) moderate if managed with systemic corticosteroids and/or antibiotics and (III) severe if it resulted in emergency department presentation or hospitalization. Secondary endpoints were the overall and severity-stratified AECOPD rates, time to first AECOPD, the change in FEV1 and the SGRQ and CAT questionnaire scores at 48 weeks. Adherence to intervention was reported as ≥80% (high), ≥60% to <80% (moderate) and <60% (low).
Statistical Methods
The primary analysis group was defined by an absolute count of ≥300 eosinophils/µL of blood (referred to as ≥300). Secondary exploratory groupings were defined by a cut-off of ≥150 eosinophils/µL and ≥3% of total white blood cell (WBC) count.
All comparisons were made between the PrT and PP groups unless specified otherwise. Statistical significance was defined as p < 0.05. Difference in AECOPD count between treatment groups was assessed with a hierarchical negative binomial regression model (with recruiting site as random effect) adjusted for a pre-defined fixed-effects covariates set including age, sex, region, baseline percentage predicted post-bronchodilator FEV1, baseline FEV1 reversibility (% improvement in FEV1 after nebulized short-acting β2-agonist) and smoking status. Analysis was repeated with fixed effects only to obtain the adjusted, annualized AECOPD rates. In both models, the offset was the natural log follow-up time of each participant.
Secondary endpoints were lung function values obtained by spirometry, CAT and SGRQ, which were analyzed using multilevel mixed-effects linear regression with the similar fixed effects covariates as the primary outcome model. Cox Proportional Hazards Regression was used to assess risk of exacerbation. Univariable predictors of eosinophilia were also tested for using linear regression, ordinal or binomial logistic regression where appropriate. All analyses were conducted using Stata 16.1 (StataCorp LLC. 2019. Stata Statistical Software: Release 16.1. College Station, TX, USA).
Results
Participant enrolment commenced in June 2014 and the final patient completed the study in May 2018. Of the original 1670 randomized participants in the TASCS trial, 1487 participants had absolute blood eosinophil counts recorded at baseline, were randomized to a treatment group and remained in the study for 2 or more weeks. The median blood eosinophil count for this sample was 150 cells/µL (Interquartile limits (IQL) 8–26), with values of 15 cells/µL (IQL 8–27) and 160 cells/µL (IQL 80–260) for the PP and PrT groups, respectively.
At baseline, 325 (22%) of the included participants had blood eosinophil counts exceeding ≥300 cells/µL (Table 1). Within this participant group, the treatment allocation was proportionate to the full sample (PrT: n = 101, PP: n = 224) and the disposition of participants was similar. A total of 776 (52%) participants had counts exceeding ≥150 eosinophils/µL, and 571 (38%) had blood eosinophil percentages ≥3%.
 |
Table 1 Demographics of Participants in the TASCS Sample at Baseline Who Had Blood Eosinophil Counts Recorded, Stratified by Eosinophilic Status (≥300 Cells/µL) and Treatment Group |
Baseline Eosinophils and Exacerbation Rate by Treatment Group
At trial completion 51 of the 325 participants with a baseline blood eosinophil count ≥300 cells/µL had withdrawn from the study (34 [15%] in the PP group; 17 [17%] in the PrT group; Figure S1). Of the 325 subgroup participants, 160 (49%) of the participants with a baseline blood eosinophil count ≥300 cells/µL had experienced one or more AECOPDs. The PrT treatment group had 58 participants report 117 events, whilst the PP group had 102 participants reporting 187 events.
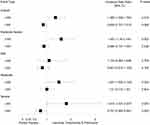
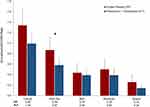
The PrT participants had significantly higher annualized moderate, severe, moderate-severe and overall AECOPD rates compared to their counterparts in the PP group (Figure 1). When the analysis was repeated without “site” as a random effect, it was found that only the moderate-severe AECOPD rate remained significantly different between the PrT and PP (p = 0.037) groups (Figure 2).
Alternative definitions of eosinophilia in COPD participants were also explored. At ≥150 cells/µL and ≥3% no significant difference in the moderate-severe AECOPD rate was observed between the treatment groups (Figures S2 and S3). This was also the case when absolute blood eosinophil count and eosinophils as a percentage of total WBCs were analyzed as continuous variables. Within the PrT arm of the study, participants with a baseline blood eosinophil count ≥300 cells/µL the moderate-severe AECOPD rate was significantly higher than those with a cell count <300/µL of blood (Table S2A). The differences between these subgroups within the pooled placebo group were not significant (Table S2B).
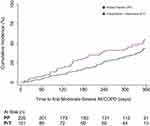
Treatment allocation did not determine risk of experiencing an AECOPD of any severity, nor for the moderate-severe endpoint (Figures 3 and S4). The median time to first moderate-severe AECOPD for the PrT and PP groups within the ≥300 cells/µL group was 148.0 (IQR 98–278) and 200 (IQR 84–232) days, respectively. Similarly, no significant differences in AECOPD risk were observed in the ≥150 cells/µL and ≥3% groups between treatments (Figures S5 and S6).
Secondary Endpoints
Change in post-bronchodilator spirometry values from baseline to study completion was similar for treatment allocation groups. Within the ≥300 cells/µL participant group the difference in the adjusted mean decline of FEV1 at 48 weeks was 18mL [95% CI −70 – 28] in the PP group and 7mL [−0.8–5] in the PrT group (P = 0.75). Similarly, no significant difference was observed between treatment groups for change in percent predicted FEV1, change in absolute and percent predicted FVC, and the change in FEV1/FVC ratio (Table 2).
 |
Table 2 Secondary Outcomes (Means, 95% CI) at Study Completion by Treatment Groups (Pooled Placebo and Prednisone & Theophylline) in Participants with Blood Eosinophil Counts ≥300 Cells/µL |
At study completion, the changes from baseline CAT score, SGRQ total score (and sub-domains) were not significantly different between PrT and PP.
Analyses repeated with participants in the ≥150 and ≥3% groups demonstrated similar non-significance between changes in these secondary outcomes between treatment arms (Table S1).
Participant Disposition
Treatment group allocation did not predict premature study discontinuation, neither in the three eosinophil groups; ≥300 (OR 0.88 [0.47–1.67], p = 0.71), ≥150 (OR 1.13 [0.75–1.70], p = 0.554) and ≥3% (OR 0.94 [0.59–1.47], p = 0.788).
Intervention adherence was likewise not associated with eosinophil count at baseline or by inclusion in the ≥300 (OR 1.3 [0.84–2.02], p = 0.247) or ≥3% (OR 1.26 [0.85–1.76], p = 0.083) groups. However, membership in the ≥150 blood eosinophil group was associated with a higher level of adherence (OR 1.51 [1.06–2.14], p = 0.022).
Predictors of Eosinophilia
At baseline, the strongest univariate predictors of an eosinophil count ≥300 cells/µL were increased total WBC, monocyte, lymphocyte and neutrophil counts, as well as male sex, having a higher predicted post-bronchodilator FVC, higher absolute post-bronchodilator FEV1, higher BMI, and a lower respiration rate (Table 3). Unit increases in blood eosinophil count occurred in parallel to increases in monocytes, lymphocytes, neutrophils, FVC (absolute and %predicted) and absolute FEV1. Both analyses also showed elevations of blood eosinophils predicted by male sex and a higher absolute FEV1 reversibility (Table S3).
 |
Table 3 Baseline Univariate Predictors of a Blood Eosinophil Count of ≥300 Cells/µL in the TASCS Trial Sample |
Discussion
This study demonstrated that in Chinese participants with “Global Initiative for Chronic Obstructive Lung Disease (GOLD)” grade II–IV COPD and blood eosinophilia (≥300 cells/µL), who were randomized to receive low-dose oral theophylline with prednisone, experienced a significant increase in moderate-severe AECOPDs compared to the participants randomized to placebo. Rates of hospitalization and out-of-hospital use of antibiotics and/or oral corticosteroids due to AECOPD were also both significantly higher in the double-treatment group compared to pooled placebo.
The overall findings of this analysis were unexpected, as existing disease models and in vitro studies had suggested that the proposed synergistic anti-inflammatory action of low-dose theophylline and prednisone would benefit participants with an elevated eosinophil count. Retrospective cohort studies and post-hoc analyses of clinical trials have found that regular administration of inhaled corticosteroid therapy is associated with an inverse relationship between exacerbation risk and frequency and blood eosinophil counts.9–15 This has formed the basis for the current GOLD recommendation that patients with frequent exacerbations and blood eosinophil counts exceeding ≥300 cells/µL adopt combination pharmacotherapy containing an inhaled corticosteroid added to long acting bronchodilator(s).2 Though this is congruent with Chinese guidelines,16,17 inhaled corticosteroid therapy is only used in any capacity by 0–1% of the patient population. By contrast, use of theophylline as a maintenance or rescue medication is prevalent, and is an affordable alternative to the gold standard recommendation of fixed-dose inhaled bronchodilators with an optional ICS component.18,19
The results of this analysis are difficult to contextualize and interpret as available literature exploring the characteristics of this region-specific patient subgroup is incomplete. Previous studies have reported some similarities, associating eosinophilia with elevated monocytes and lymphocytes, but also observing an inverse relationship with blood neutrophils.20–22 Globally, analyses of the COPDgene, ECLIPSE, SPIROMICS datasets have found variable associations between these inflammatory cells and increased blood eosinophil counts in stable COPD participants – though male predisposition is evident in most studies.23–26
While the mechanism for the observed treatment effect is unclear, it is possible that the study participants with eosinophilia defined by a blood eosinophil count ≥300 cells/µL display a hitherto unrecognized clinical phenotype. This is supported by the presence of superior lung function, male predisposition, and concurrently elevated total WBC, monocyte, neutrophil and lymphocyte counts. It is possible that raised eosinophils in the study’s Chinese COPD sample, which were associated with a higher overall WBC, may represent a state of low-grade inflammation which is not suppressed by corticosteroids. Another aspect to consider is that the TASCS sample is not representative of typical clinical trials for COPD pharmacotherapies, instead recruiting from a Chinese population with representation from never-smokers and regionally situated patients.(27)
Alternatively, it may be that this subset of participants had elevated blood eosinophil counts not originating from an underlying COPD phenotype, but instead an undiagnosed infection at baseline. This would account for the commensurate increases in the overall and individual components of the WBC counts. Subsequently, initiation of steroid-mediated systemic immunosuppression could have provided newly acquired or existing pathogens the opportunity to persist and lead to an exacerbation. This has some precedent, as a recent meta-analysis of seven studies investigating the use of concomitant administration of theophylline with inhaled corticosteroids found that their coadministration may lead to an increased risk of COPD-related hospitalization and mortality in the patient population.28 Relevant to this may also be evidence from studies such as TORCH, which demonstrated the risk of pneumonia through regular use of inhaled corticosteroids. A recent cohort study reported that rheumatoid arthritis participants prescribed low-dose systemic glucocorticosteroids were significantly more likely to be admitted to hospital for infection.29,30 With the existing TASCS data, it was not possible to determine if this proposed mechanism is responsible, as no sputum samples were collected, and complete blood counts were not conducted post-randomisation.
Eosinophils are the primary innate immune cell for parasitic infection, so undiagnosed parasitism may be a potential confounder for the false-positive detection of an eosinophilic COPD phenotype. A statement by the “Asian Pacific Society of Respirology” suggests the screening of patients for infection prior to addition of a corticosteroid component to a maintenance pharmacotherapy regimen.31 Though parasitic infections are endemic in a number of the provinces where recruitment occurred,32 the randomized trial design and analysis cofactors used would minimize this effect. The rate of eosinophilia observed in the sample was also similar to past COPD studies conducted in China.33 Observational studies conducted in other regions where gastrointestinal parasites are endemic have found that screening out COPD patients with comorbid infection still leaves a significant proportion of the patient population with eosinophil counts of ≥300 cells/μL of blood.34,35
Though these results are intriguing, the interpretation of treatment effect must be considered against some limitations. This was a pre-specified post-hoc analysis that aimed to identify a treatment effect in a subset (n = 325 of 1487) of the trial participants, and was underpowered compared to the primary analysis of the TASCS dataset.8 Some variance may also be attributable to the differences between the 37 recruiting sites. A relevant example is that sites were permitted to use their own clinical chemistry and blood cell ranges when determining if a participant’s values precluded them from trial participation. While this was mitigated using a robust multi-level mixed-effects model adjusted for site as a random effect and region as a fixed effect, it may account for a small portion of study outcome variance. As there are very few studies from Chinese populations that clearly define the different COPD phenotypes, and characteristic eosinophil profiles in the context of their response to treatment, it is also hard to compare and contextualize these results. Given the major burden of disease in China, these studies are urgently required to better define the COPD population in the context of their unique combination of geographic location, environmental exposures, genetics and culturally specific factors.
Conclusion
In summary, this post-hoc analysis of data from the TASCS trial shows that in Chinese COPD participants with an elevated blood eosinophil count, concomitant oral theophylline and prednisone was associated with increased frequency of acute exacerbations compared to participants receiving placebo. Although a precise explanation for this finding is lacking, the long-term coadministration of these pharmacotherapies is cautioned in this subgroup of COPD patients until further research is conducted.
Data Sharing Statement
Access may be considered by the protocol steering committee and sponsor upon request.
Acknowledgments
The authors would like to thank the participants and the TASCS Investigators and research assistants at the 37 participating centers (principal investigators and sites are listed in Table S4).
Funding
The conduct of the original TASCS trial was financially funded by the National Health and Medical Research Council, Australia. Financial funding and in-kind support was also provided by the State Key Lab of Respiratory Diseases and Guangzhou Institute of Respiratory Diseases, China; West China Hospital, Chengdu, China.
Disclosure
Anish Scaria, Allison Martin, Nanshan Zhong, Fu-Qiang Wen and Jinping Zheng declare no potential conflicts of interest in this work. Thomas Bradbury reports being the recipient of a 3-year top-up academic scholarship funded by GlaxoSmithKline. Gian Luca Di Tanna reports personal fees from Amgen, outside the submitted work. Peter J Barnes reports receiving consulting and speaking fees from AstraZeneca, Boehringer Ingelheim, Novartis, EpiEndo, and Teva Pharmaceuticals. Bartolome Celli reports receiving speaking fees from AstraZeneca and GlaxoSmithKline and consulting fees from Astra Zeneca, GlaxoSmithKline, Novartis, Chiesi, Pulmonx, Regeneron and Sanofi Aventis. Norbert Berend reports holding GlaxoSmithKline stock or stock options and being a part time employee of GlaxoSmithKline. Christine R Jenkins reports her position as chair of the board of the Lung Foundation of Australia, and as a member of two data safety monitoring boards (one paid and one unpaid). She also reports receiving fees for work done on behalf of multiple manufacturers of COPD medications for advisory board meetings, lectures, advice and the development of educational materials. The authors report no other conflicts of interest in this work.
References
1. Vos T, Lim SS, Abbafati C, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–1222.
2. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for prevention, diagnosis and management of COPD. GOLD; 2021. Available from: https://goldcopd.org.
3. Cosio BG, Tsaprouni L, Ito K, Jazrawi E, Adcock IM, Barnes PJ. Theophylline restores histone deacetylase activity and steroid responses in COPD macrophages. J Exp Med. 2004;200(5):689–695. doi:10.1084/jem.20040416
4. Ito K, Ito M, Elliott WM, et al. Decreased histone deacetylase activity in chronic obstructive pulmonary disease. N Engl J Med. 2005;352(19):1967–1976. doi:10.1056/NEJMoa041892
5. Barnes PJ. Role of HDAC2 in the pathophysiology of COPD. Annu Rev Physiol. 2009;71(1):451–464. doi:10.1146/annurev.physiol.010908.163257
6. Cosio BG, Iglesias A, Rios A, et al. Low-dose theophylline enhances the anti-inflammatory effects of steroids during exacerbations of COPD. Thorax. 2009;64(5):424–429. doi:10.1136/thx.2008.103432
7. Devereux G, Cotton S, Fielding S, et al. Effect of theophylline as adjunct to inhaled corticosteroids on exacerbations in patients with COPD: a randomized clinical trial. JAMA. 2018;320(15):1548–1559. doi:10.1001/jama.2018.14432
8. Jenkins CR, Wen F-Q, Martin A, et al. The effect of low dose corticosteroids and Theophylline on the risk of acute exacerbations of COPD. The TASCS randomised controlled trial. Eur Respir J. 2020;57:2003338.
9. Bafadhel M, Peterson S, De Blas MA, et al. Predictors of exacerbation risk and response to budesonide in patients with chronic obstructive pulmonary disease: a post-hoc analysis of three randomised trials. Lancet Respir Med. 2018;6(2):117–126. doi:10.1016/S2213-2600(18)30006-7
10. Barnes NC, Sharma R, Lettis S, Calverley PMA. Blood eosinophils as a marker of response to inhaled corticosteroids in COPD. Eur Respir J. 2016;47(5):1374. doi:10.1183/13993003.01370-2015
11. Ferguson GT, Rabe KF, Martinez FJ, et al. Triple therapy with budesonide/glycopyrrolate/formoterol fumarate with co-suspension delivery technology versus dual therapies in chronic obstructive pulmonary disease (KRONOS): a double-blind, parallel-group, multicentre, Phase 3 randomised controlled trial. Lancet Respir Med. 2018;6(10):747–758. doi:10.1016/S2213-2600(18)30327-8
12. Papi A, Vestbo J, Fabbri L, et al. Extrafine inhaled triple therapy versus dual bronchodilator therapy in chronic obstructive pulmonary disease (TRIBUTE): a double-blind, parallel group, randomised controlled trial. Lancet. 2018;391(10125):1076–1084. doi:10.1016/S0140-6736(18)30206-X
13. Siddiqui SH, Guasconi A, Vestbo J, et al. Blood eosinophils: a biomarker of response to extrafine Beclomethasone/Formoterol in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2015;192(4):523–525. doi:10.1164/rccm.201502-0235LE
14. Vestbo J, Papi A, Corradi M, et al. Single inhaler extrafine triple therapy versus long-acting muscarinic antagonist therapy for chronic obstructive pulmonary disease (TRINITY): a double-blind, parallel group, randomised controlled trial. Lancet. 2017;389(10082):1919–1929. doi:10.1016/S0140-6736(17)30188-5
15. Watz H, Tetzlaff K, Wouters EF, et al. Blood eosinophil count and exacerbations in severe chronic obstructive pulmonary disease after withdrawal of inhaled corticosteroids: a post-hoc analysis of the WISDOM trial. Lancet Respir Med. 2016;4(5):390–398. doi:10.1016/S2213-2600(16)00100-4
16. Cheng S-L, Lin C-H. COPD guidelines in the Asia-pacific regions: similarities and differences. Diagnostics. 2021;11(7):1153. doi:10.3390/diagnostics11071153
17. Chronic Obstructive Pulmonary Disease Group of Chinese Thoracic Society; Chronic Obstructive Pulmonary Disease Committee of Chinese Association of Chest Physicians. [Guidelines for diagnosis and treatment of Chronic Obstructive Pulmonary Disease (2021 Revised Edition)]. Chin J Tuberc Respir Dis. 2021;44(3):170–205. doi:10.3760/cma.j.cn112147-20210109-00031
18. Bao H, Jia G, Cong S, et al. Phenotype and management of chronic obstructive pulmonary disease patients in general population in China: a nationally cross-sectional study. NPJ Prim Care Respir Med. 2021;31(1):32. doi:10.1038/s41533-021-00243-x
19. Lou P, Zhu Y, Chen P, et al. Vulnerability, beliefs, treatments and economic burden of chronic obstructive pulmonary disease in rural areas in China: a cross-sectional study. BMC Public Health. 2012;12(1):287. doi:10.1186/1471-2458-12-287
20. Wu HX, Zhuo KQ, Cheng DY. Peripheral blood eosinophil as a biomarker in outcomes of acute exacerbation of Chronic Obstructive Pulmonary Disease. Int J Chron Obstruct Pulmon Dis. 2019;14:3003–3015. doi:10.2147/COPD.S226783
21. Zhang Y, Liang L-R, Zhang S, et al. Blood eosinophilia and its stability in hospitalized COPD exacerbations are associated with lower risk of all-cause mortality. Int J Chron Obstruct Pulmon Dis. 2020;15:1123–1134. doi:10.2147/COPD.S245056
22. Zeng Q, Wang H, Wang K, Zhou H, Wang T, Wen F. Eosinophilic phenotype was associated with better early clinical remission in elderly patients but not middle-aged patients with acute exacerbations of COPD. Int J Clin Pract. 2021;75(9):e14415. doi:10.1111/ijcp.14415
23. Yun JH, Lamb A, Chase R, et al. Blood eosinophil count thresholds and exacerbations in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2018;141(6):2037–47.e10. doi:10.1016/j.jaci.2018.04.010
24. Hastie AT, Martinez FJ, Curtis JL, et al. Association of sputum and blood eosinophil concentrations with clinical measures of COPD severity: an analysis of the SPIROMICS cohort. Lancet Respir Med. 2017;5(12):956–967. doi:10.1016/S2213-2600(17)30432-0
25. DiSantostefano RL, Hinds D, Van Le H, Barnes NC. Relationship between blood eosinophils and clinical characteristics in a cross-sectional study of a US population-based COPD cohort. Respir Med. 2016;112:88–96. doi:10.1016/j.rmed.2016.01.013
26. Zysman M, Deslee G, Caillaud D, et al. Relationship between blood eosinophils, clinical characteristics, and mortality in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:1819–1824. doi:10.2147/COPD.S129787
27. Kruis AL, Ställberg B, Jones RCM, et al. Primary care COPD patients compared with large pharmaceutically-sponsored COPD studies: an UNLOCK validation study. PLoS One. 2014;9(3):e90145.
28. Shuai T, Zhang C, Zhang M, et al. Low-dose theophylline in addition to ICS therapy in COPD patients: a systematic review and meta-analysis. PLoS One. 2021;16(5):e0251348. doi:10.1371/journal.pone.0251348
29. Calverley PMA, Anderson JA, Celli B, et al. Salmeterol and fluticasone propionate and survival in Chronic Obstructive Pulmonary Disease (TORCH). N Engl J Med. 2007;356(8):775–789. doi:10.1056/NEJMoa063070
30. George MD, Baker JF, Winthrop K, et al. Risk for serious infection with low-dose glucocorticoids in patients with rheumatoid arthritis. Ann Intern Med. 2020;173(11):870–878. doi:10.7326/M20-1594
31. Rhee CK, Chau NQ, Yunus F, Matsunaga K, Perng D-W. Management of COPD in Asia: a position statement of the Asian Pacific Society of Respirology. Respirology. 2019;24(10):1018–1025. doi:10.1111/resp.13633
32. Chen Y-D, Zhou C-H, Zhu -H-H, et al. National survey on the current status of important human parasitic diseases in China in 2015. Zhongguo Ji Sheng Chong Xue Yu Ji Sheng Chong Bing Za Zhi. 2020;38(1):5–12.
33. Zheng J, Jian W, Su L, Xue W. Blood eosinophil levels in Chinese patients with Chronic Obstructive Pulmonary Disease: pooled analysis of 7 Phase 3/4 randomized controlled trials. B24 biomarkers in COPD.
34. Saiphoklang N, Chomchoey C. Eosinophilia and parasitic infestations in patients with chronic obstructive pulmonary disease. Sci Rep. 2020;10(1):12490. doi:10.1038/s41598-020-69541-7
35. Juthong S, Kaenmuang P. Association between blood eosinophils with exacerbation and patient-reported outcomes in chronic obstructive pulmonary disease patients in an endemic area for parasitic infections: a prospective study. J Thorac Dis. 2020;12(9):4868–4876. doi:10.21037/jtd-19-4101
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.