Back to Journals » Journal of Pain Research » Volume 15
Bibliometric and Visual Analysis of the Current Status and Trends of Postoperative Pain in Children from 1950–2021
Received 1 July 2022
Accepted for publication 4 October 2022
Published 14 October 2022 Volume 2022:15 Pages 3209—3222
DOI https://doi.org/10.2147/JPR.S380842
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Giorgio Veneziano
Cong Wang,1 Li-Dan Liu,1 Xue Bai2
1Department of Anesthesiology, Shengjing Hospital of China Medical University, Shenyang, People’s Republic of China; 2Department of Health Management, Shengjing Hospital of China Medical University, Shenyang, People’s Republic of China
Correspondence: Xue Bai, Department of Health Management, Shengjing Hospital of China Medical University, No. 36 Sanhao Street, Heping District, Shenyang, 110004, People’s Republic of China, Email [email protected]
Background: Postoperative pain in children has been overlooked for a long time. The knowledge structure, research hotspots and trends related to postoperative pain in children are unclear and have not been systematically summarized.
Purpose: We aimed to analyze the current state of research on postoperative pain in children and to conduct in-depth mining of the knowledge structure.
Methods: The PubMed database for publications on postoperative pain in children between 1950 and 2021 was searched. Bibliographic Item Co-Occurrence Matrix Builder (BICOMB) was performed to obtain the co-word matrix and co-occurrence matrix. The H-index method was used to extract high-frequency main Medical Subject Headings (MeSH) terms/subheadings.
Results: The high-frequency MeSH terms were analyzed by biclustering, strategic diagram and social network analyses. Totally, 4022 publications were retrieved. The analysis showed that 60 countries or regions published relevant documents, with the United States publishing the most significant number of papers. Totally, 811 journals published relevant papers, with Pediatric Anesthesia ranking first. Moreover, we extracted 43 high-frequency main MeSH terms/subheadings and clustered them into five categories: overview, aetiology and epidemiology, pharmacotherapy, opioid administration and dosing, and prevention and control of postoperative pain in children.
Conclusion: Pharmacological treatments, pain prevention and control are the focus of research and are becoming increasingly mature. Opioid stewardship and regional anesthesia is the trend and focus of future research. Our study offers a better understanding of the current status and knowledge structure of postoperative pain in children and provides a reference for improving postoperative pain management in children in the future.
Keywords: bibliometrics, visualization analysis, postoperative pain, children, status, trends
Introduction
Over the past decades, many parents and physicians have been under-aware of postoperative pain in children, with a greater focus on the completion of the surgery, and the pain experienced by children after surgery has been overlooked. The World Health Organization (WHO) states that postoperative pain in children is a public health problem in most countries of the world.1 Surveys on the incidence of moderate to severe postoperative pain in children are 21% to 64%.2,3 However, there are no universally accepted guidelines for the management of perioperative pain in children. Although the WHO has developed guidelines for “persistent pain in children”, they specifically exclude perioperative pain. In recent years, clinicians have become increasingly aware of the need for adequate analgesia for children after surgery.4 Adequate analgesia during the first 48 hours after surgery reduces the neuroendocrine stress response of the body, improves the prognosis of the children and reduces medical costs.5 However, the management of postoperative pain in children varies greatly around the world.
Management strategies for pain management are influenced by a variety of factors, including geography, culture, infrastructure, etc.6 Postoperative pain management involves multiple disciplines, including surgery, anesthesiology, nursing, addiction science, and parent and child psychology. In this context, it is extremely necessary to define minimum standards for postoperative analgesia in children. The WHO recommends a two-step management approach involving analgesic selection according to the severity of pain, for persistent pain in children and adolescents.1 Stepwise management is the basic standard for postoperative pain management in children, with a graded approach of primary, secondary, and advanced management according to different types of surgery. Combining multimodal analgesia further optimizes pain management. Enhanced psychological treatment for the child and parents will help to relieve postoperative pain in children.7
Bibliometrics and information visualization are important scientific research tools that are widely used in a variety of disciplines. The rapid development of bibliometric analysis software has made it easier for researchers to obtain scientific quantitative analysis, which is an important reference value for exploring the knowledge structure of disciplines, planning the layout of disciplines, and adjusting the direction of disciplines. A large amount of literature on postoperative pain in children has been published in recent years, which mainly includes assessment of postoperative pain in children, treatment with analgesic drugs, multimodal analgesia techniques, and multidisciplinary cooperation. Nevertheless, none of the studies comprehensively analyzed and elaborated the research status, research hotspots, and research trends of postoperative pain in children. Due to the inherent specificity of the pediatric population, such as rapid physical development and high psychological sensitivity and vulnerability, it is difficult to conduct large-scale clinical studies, and the vast majority of current evidence comes from single-center studies and isolated procedures. In this study, we used analytical tools to conduct a bibliometric analysis and mine the knowledge structure of the literature related to postoperative pain in children. These findings may provide a better understanding the field of postoperative pain in children and a reference for future investigations.
Materials and Methods
Data Collection and Retrieval Strategy
The original data for this paper were all obtained from the PubMed database. The PubMed was chosen as the data source for two reasons: (1) PubMed is a national library of medicine with a free authoritative database of medical literature on health and medical information; and (2) Medline, a subset of PubMed, is indexed with Medical Subject Headings (MeSH) terms, which are a set of normalized words that can reflect the content of an article. Co-word clustering analysis can be implemented according to these terms. The search was conducted on December 31, 2021, and was completed within one day to ensure that the results were as up-to-date as possible. There are no language restrictions on the literature search and download process. The search strategy of our study was: pain, postoperative [MeSH terms] AND child [MeSH terms]. There was no time limit, the type of literature was limited to “Journal Article”, and the search results were filtered. A total of 4032 publications were identified from PubMed. The titles and abstracts of the publications were filtered based on relevance and selection criteria. The inclusion criteria were mainly concerned with postoperative pain in children. The exclusion criteria included 1) animal studies, 2) use of sedation in the intensive care unit, 3) including adults, 4) not within the prescribed age range, and 5) retracted articles. Two investigators performed independent reviews and assessments and reached an agreement on inclusion analysis. The 90% of papers were agreed upon by the two investigators, representing strong concordance. Before reaching a consensus, all discrepancies present would be discussed concerning the study objectives, and 4022 relevant articles were finally identified, saving the literature in “.TXT” format.
BICOMB Co-Word Analysis
The documents in.TXT format downloaded from the PubMed database were imported into the Bibliographic Item Co-Occurrence Matrix Builder (BICOMB) software developed by Professor Lei Cui8 of the China Medical University to extract the data. The key fields were set as main MeSH terms/subheadings, and the main MeSH terms/subheadings were excavated and investigated to extract and count the frequencies of all the main MeSH terms/subheadings. In this study, the H-index method was used to obtain high-frequency MeSH terms and the information related to year, country and periodical were also counted, and the co-word matrix and co-occurrence matrix of high-frequency MeSH terms were generated.
Biclustering Analysis of High-Frequency Main MeSH Terms/Subheadings
In this study, the graphical clustering toolkit (gCluto) 1.0 developed by Rasmussen from the University of Minnesota was used to import the co-word matrix of high-frequency main MeSH terms/subheadings.9 The clustering method was chosen as Repeated Bi-section (RB), the number of clusters was set to 5, and the remaining parameters were chosen as the default values. A biclustering visualization analysis was performed, a mountain visualization and visualization matrix were drawn, and the number of clusters, intra-cluster similarity, and intra-cluster standard deviation (SD) was calculated.10 The mountain visualization is three-dimensional mountain clustering graphs produced by the multidimensional scaling manner. The color of the mountain peaks is inversely proportional to the intra-cluster SD, with red representing small SD and blue representing large SD. The height of the mountain is proportional to the intra-cluster similarity, the steeper the peak, the greater the intra-cluster similarity. The volume of the mountain is proportional to the number of MeSH terms within the cluster. The distance between the peaks reflects the correlation between clusters, and clusters with strong correlations appear to be gathered and overlapping. The values of the original data of the matrix in the visualization matrix are replaced by colors, and the depth of colors represents the frequency of MeSH terms, the darker the color, the higher the frequency. The rows of the visualization matrix represent the clusters of high-frequency main MeSH terms/subheadings, and the columns represent the PMID clusters corresponding to the source literature.
Strategic Diagram Analysis
The principle of strategic diagram analysis is to visualize the internal and external links between different topics based on co-occurrence matrix and clustering, to quantitatively evaluate the significance and development degree of different topics in a specific field, and to investigate the research hotspots and frontiers and development trends in a specific field.11 The two-dimensional diagram drawn with the parameters of centrality and density is the strategic diagram, with the horizontal axis representing centrality and the vertical axis representing density. Centrality represents the strength of a topic’s connection with other topics. A higher value indicates that the topic is more closely associated with other topics and is at the core of the research topic. Density represents the strength of connection within a single topic. The value of density indicates the degree of the topic maturity. The higher value of the density, the higher degree of maturity.
Social Network Analysis
Social networks are social structures composed of individuals (or organizations) called “nodes” that are linked together by one or more specific types of interdependence.12 The main purpose of social network analysis is to represent the location of research nodes in a multi-relation network and the grid structure containing multiple relations. Network analysis could provide a clear understanding of the role of nodes in the social structure. In the present study, after a co-occurrence matrix of 43 high-frequency main MeSH terms/subheadings was formed by the BICOMB software, a social network analysis was constructed using Ucinet 6.0 software13 to interpret the structure of knowledge in the field of postoperative pain in children. Thereafter, the high-frequency main MeSH terms/subheadings network was visualized using NetDraw 2.084 software (Analytic Technologies Co., Lexington, KY, USA) and presented on a two-dimensional map. The high-frequency main MeSH terms/subheadings networks were represented as nodes, and co-occurrence frequencies were represented as line segments. The density of high-frequency main MeSH terms/subheadings is used to measure the closeness of the network. The location of high-frequency main MeSH terms/subheadings was assessed by measuring three centralities (closeness degree, betweenness degree, and degree) of each node to understand the network structure of postoperative pain in children. The diagram process of literature retrieval, study selection and analysis are shown in Figure 1.
Results
Overall Distribution
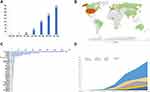
According to the search strategy, duplicates and literature that did not meet the inclusion criteria were omitted, and a total of 4022 publications were finally identified. Overall, there was an increasing trend in the publication of literature on postoperative pain in children (Figure 2A). The statistics (Figure 2B and C) showed that a total of (or only) 60 countries or regions published research papers related to pain in children from 1950 to 2021. In terms of the number of publications, the United States had the maximum number of publications, with 1472, accounting for 36.60% of the total (1472/4022), and was the most dominant country in the field of pediatric pain research. The countries ranked 2–10 were England, France, Germany, Ireland, Russia, Japan, Italy, Netherlands, and Switzerland, respectively. According to the area chart (Figure 2D), we found that there had been a surge in studies of pain in children in the United States, England, Germany, and Ireland over the last 30 years, indicating that pain in children has gradually become a focus of researchers’ attention. Interestingly, France showed an exponential increase from 1980–2010, while the number of studies gradually decreased after 2010. A total of 811 journals published literature related to pediatric pain from 1950 to 2021. This study showed (Table 1) that the top 15 journals in terms of the number of publications published a total of 1324 relevant papers, accounting for 32.92% of the total (1324/4022). Among them, Pediatric Anaesthesia published 366 papers, accounting for 9.1% of the total (366/4022), with the most significant number of publications. The journal is published by Arnette-Blackwell, France Paris.
 |
Table 1 Core Published Journals of Postoperative Pain in Children Research from 1950–2021 |
Analysis of Research Hotspots Based on MeSH Terms Cluster
A total of 3159 main MeSH terms/subheadings were counted using BICOMB, and 43 high-frequency main MeSH terms/subheadings were extracted based on the H-index method (the cumulative percentage was 41.32%) (Table 2). The co-occurrence analysis was performed for the 43 high-frequency main MeSH terms/subheadings to form a co-word matrix with 43 rows × 2877 columns. Thereafter, the co-word matrix was imported into gCluto software for clustering analysis. According to the actual clustering effect, the 43 high-frequency main MeSH terms/subheadings were finally chosen to be clustered into five categories. The visualization matrix was shown in Figure 3A. The horizontal direction (rows) of the visualization matrix was the clustering of the 43 high-frequency main MeSH terms/subheadings. As revealed from the clustering results, the number of main MeSH terms/subheadings within each cluster had little difference. The vertical direction (columns) was the clustering of 4022 documents, and the PMID numbers of the documents were represented by the corresponding columns at the top of the figure The visualized mountain map was shown in Figure 3B, and the clustering effect was more satisfactory from the overall layout.
 |
Table 2 High-Frequency MeSh Major Topic/Subheadings from the Included Papers on Postoperative Pain in Children |
Cluster 0 included seven high-frequency main MeSH terms/subheadings with towering peaks and a light red peak color. This cluster was an overview study of pain in children. Cluster 1 included seven high-frequency main MeSH terms/subheadings with medium peak height and yellow peak color, indicating that the topic similarity and the literature distribution were in the middle. This cluster was an etiological and epidemiological study of postoperative pain in children. Cluster 2 included 11 high-frequency main MeSH terms/subheadings, with the most prominent peak volume and a dark red peak color, indicating that the studies were more concentrated. This cluster was a study of pharmacological treatment of postoperative pain in children. Cluster 3 included eight high-frequency main MeSH terms/subheadings, with medium volume and light red peak color, and medium intracluster similarity. Clusters 3 and 4 had a few consecutive peaks, which may overlap with each other. The cluster was mainly focused on opioid administration and dosage studies. Cluster 4 included ten high-frequency main MeSH terms/subheadings with gentle mountains and similar color peaks to cluster 3, indicating looser research and a wider distribution of literature. This cluster was for studies on the prevention and control of postoperative pain in children.
Results of Strategic Diagram Analysis
Based on the results of the co-word clustering analysis and the co-occurrence matrix of high-frequency main MeSH terms/subheadings, the centrality and density of each cluster were calculated. Thereafter, the two-dimensional strategic diagram was plotted using the centrality and density (Figure 4). Clusters 2 and 4 located in Quadrant I had high centrality and density, indicating that the research on pharmacological treatment and prevention and control of postoperative pain in children had a relatively mature level of research. In addition, they also had extensive links with the remaining clusters and belonged to the core themes of postoperative pain in children. Clusters 0 and 1 in Quadrant III had low centrality and density values, indicating that the research of the overview and the study of etiological and epidemiological postoperative pain in children were immature, and the connection with other research themes was not close. Cluster 3 in Quadrant IV had low density and loose internal structure; however, it was relatively concerned in the hot topics of children’s postoperative pain research compared with other themes, indicating that the administration and dosage of opioids needed to be further developed and improved.
Results of Social Network Analysis
The density value of the studies related to postoperative pain in children was calculated to be 0.64, indicating that the studies were overall closely connected. Social network analysis knowledge structure was constructed using closeness degree, betweenness degree and degree as centrality parameters (Table 3 and Figure 5). In the 1950–2021 children’s postoperative pain network, a total of 18 high-frequency main MeSH terms/subheadings had high centrality above the mean. “Pain, Postoperative/*prevention & control” had the highest degree of centrality.
 |
Table 3 Social Network Analysis of the Studies Related to Postoperative Pain in Children |
Discussion
Data on the present trends, research hotspots, and changes in research themes on the postoperative pain in children is limited. In the present study, the trends over the past 70 years in this research were investigated using the PubMed database. Our analysis showed that 60 countries or regions published relevant documents, with the United States publishing the most significant number of papers. Five categories, including overview, aetiology and epidemiology, pharmacotherapy, opioid administration and dosing, and prevention and control of postoperative pain in children, are described based on the 43 high-frequency main MeSH terms/subheadings. After bibliometric analysis, co-word biclustering analysis, strategic diagram analysis, and social network analysis, we observed that opioid stewardship and regional anesthesia were the trend and focus of future research. Our study may provide a meaningful insight into the current status and knowledge structure of postoperative pain in children and offer an orientation for improving postoperative pain treatment in children in the future investigation.
The issue of pediatric pain received little attention until the first World Congress on Pediatric Pain in Seattle in 1988. However, current practice regarding managing postoperative pain in children varies widely worldwide, and even in more affluent regions, there are no uniform clinical practice guidelines. Clustering is a method to simplify complex data into a few categories, ie, the process of grouping and categorizing a large amount of data to understand the intrinsic structure of a data set based on the qualitative or quantitative characteristics of the data itself, and describing each data set. The classification results are intuitive and more detailed, comprehensive and reasonable than traditional classification methods. Therefore, we investigated the current trends, research hotspots, and changes in research themes on the postoperative pain in children using clustering data analysis. A total of 4022 publications were identified using the high-frequency MeSH terms. These publications were then analyzed by biclustering, strategic diagram and social network analyses. As indicated in our results, we observed that there was an increasing trend in the number of literature published by a total of (or only) 60 countries or regions from 1950 to 2021, with the United States having the maximum number of publications, followed by England, France, Germany, Ireland, Russia, Japan, Italy, Netherlands, and Switzerland. In addition, the results showed that a total of 811 journals published relevant papers, with Pediatric Anesthesia ranking first. These researches are mainly focused on pharmacotherapy, opioid administration and dosing, postoperative pain prevention and control, multimodal analgesia, and pain assessment methods in children.
Cluster 0 is an overview of postoperative pain in children. It mainly covers several aspects of postoperative pain management and treatment, the psychology of the child and parents, postoperative care, etc. Pain assessment in children is known to be very difficult and is influenced by numerous factors such as the child’s cognitive level, language skills, and cultural background.14,15 Pain assessment in children mainly relies on the subjective assessment of the nursing team and the parents.16 The main pain grading tools include physiological measures, observational and behavioral measures, self-reports, and parental reports.17 Some studies have demonstrated that physiological measures are usually not associated with self-reported pain, and behavioral measures usually reflect fear and anxiety rather than pain.18 Therefore, self-report is recommended as the gold standard for pain assessment in children older than age 6 years.19 However, self-assessment is not as reliable in preschool children, and needs to be combined with an observational assessment method.19 This showed that no single factor assessment was reliable and a combination of multiple measures was usually used in clinical practice. Birnie et al recommended the use of the following eight scales, including the Numerical Rating Scale (NRS)-11, the Color Analog Scale (CAS), the Facial Pain Scale-Revised (FPS-R), the Pieces of Hurt, the Oucher Photographic Scale and Numeric scales, the Visual Analog Scale (VAS) and the Wong-Baker faces scale.20 Parental influence is critical in the developmental pattern of children’s pain memory,21 as children’s memories are most susceptible to distortion due to hint effects. Conducting individualized instruction for children and parents can improve postoperative pain in children. Parents are encouraged to use non-pharmacological therapies, such as distraction and psychoeducation, to reduce the child’s pain perception.6 Non-pharmacological treatment of postoperative pain in children may be one of the hot spots for future research.
Cluster 1 is an etiologic and epidemiologic study of postoperative pain in children. This part was relatively independent and immature, and we speculated that this part was likely to be a future research trend. Postoperative pain has been reported to occur in 44–93% of children.2,22 Poor postoperative pain control can have long-term adverse psychological and cognitive effects on children. A variety of factors, including age, gender, and family, can influence the experience of postoperative pain.23 Among them, the size of the surgical trauma and the length of the surgery is closely related to the level of pain; therefore, the type of surgery is a key factor in postoperative pain.24 Tonsillectomy and adenoidectomy are the most common pediatric surgery with a higher incidence and longer duration of pain.25 These types of surgery have the largest number of publications. Notably, children with tonsil and adenoidal hypertrophy are often associated with obstructive sleep apnea-hypopnea syndrome (OSAHS),26 and analgesic medications should be chosen more carefully. Based on the available evidence, a combination of acetaminophen and non-steroidal anti-inflammatory drugs (NSAIDs) is recommended for the relief of postoperative pain in children. Debate continues regarding the risk of bleeding with NSAIDs, but most evidence supports their safety and efficacy. Several studies have shown that improvements in surgical techniques can alleviate postoperative pain. For example, intracapsular tonsillectomy27 and laparoendoscopic single-site surgery (LESS) have been shown to reduce the severity and duration of pain.28
The topic of pharmacological treatment of postoperative pain has been continuously studied throughout the research field. Pharmacotherapy is located at the center of the entire network and is intensively and increasingly studied. Pharmacotherapy for postoperative pain plays a crucial role in the overall knowledge structure, representing the overall direction of this research field. To be precise, the overall and ultimate goal is to reduce the incidence of postoperative pain in children through pharmacotherapy, namely Cluster 2. Studies on the safety and efficacy of analgesic drugs have focused on opioids, local anesthetics, NSAIDs, acetaminophen, ketamine, and tramadol.29 Opioids are the most widely used and definitive effect for postoperative pain in children,30 which have the highest number of publications. The Food and Drug Administration (FDA) suggested restricting the use of codeine and tramadol in pediatric patients under 12 years of age.31 NSAIDs can be used for moderate-to-severe pain and reduce the use of opioids. However, at the same time, NSAIDs may cause bleeding.32 Acetaminophen is the most commonly used analgesic for acute pain. The main advantage of acetaminophen over NSAIDs is the lesser effect on coagulation.33 Ketamine is often used as an adjuvant in pediatric sacral nerve blocks to enhance the effect of the sacral block. Nevertheless, due to its potential to cause neuronal apoptosis and current guidelines recommend a conservative dose of 0.5 mg/kg.34
In recent years, there has been a gradual rise in the number of publications about the administration and dosing of opioids, suggesting that perioperative opioid use will be a research trend and hotspot for postoperative pain in children, regarded as Cluster 3. Opioids are effective in controlling perioperative pain in children. However, due to the pharmacokinetic and pharmacodynamic characteristics of opioids, dose adjustment based on age, weight and individual response is required to optimize analgesia and minimize adverse effects.35 Given the iatrogenic risk factors of opioids, the use of opioids should be minimized after many routine pediatric surgical procedures.36 The incidence of adverse events for opioid prescriptions in the pediatric population has been estimated at 38.3/per 100,000, and the number of children hospitalized for opioid overdose has increased by 200% in recent years.37 In the United States, one in five deaths among young people is linked to opioids.38 The American College of Surgeons (ACS) has called on physicians to change their opioid use habits to prevent opioid overdoses and abuse while providing pain relief.39 Studies have shown that opioids do not need to be prescribed for children after inguinal hernia repair, appendectomy, or adenoidectomy/tonsillectomy because those non-opioid analgesics can meet analgesic needs.40 Opioid-induced hyperalgesia (OIH) has been widely demonstrated in scoliosis surgery and may lead to prolonged opioid use after surgery (POUS) and chronic postoperative pain. The use of epidural analgesia in scoliosis surgery is safe and effective, providing not only intraoperative anesthesia with somatosensory evoked potential (SSEP) monitoring capabilities but also better postoperative pain control and minimizing opioid overdose and abuse.41 Thoracic segmental epidural analgesia is also indicated for children undergoing funnel chest surgery. A recent meta-analysis reported that the postoperative use of acetaminophen or NSAIDs in children reduces opioid dose requirements.42 Therefore, multimodal analgesia is recommended for postoperative pain management in children,43 while reducing the dose requirement of a single drug through different analgesic mechanisms, thus minimizing dose-dependent adverse effects.
With the spread of ultrasound technology, the development of multimodal analgesic protocols, and the accumulation of experience, the prevention and control of postoperative pain in children have matured, categorized as Cluster 4. The safety and effectiveness of local anesthetic techniques administered to children have been demonstrated.44 Nerve blocks have become an important part of modern postoperative analgesic practice in children. Studies have displayed that nerve blocks not only reduce postoperative pain in children but also reduce the use of opioids and non-opioid analgesics.45,46 Before the widespread use of ultrasound guidance, larger doses of local anesthetics were usually required to achieve a reliable block by stimulating the nerve, which might cause an increased incidence of vascular
puncture and local anesthetic systemic toxicity. In recent years, the development of ultrasound-guided peripheral nerve block (UGPNB) has facilitated the widespread use of local anesthetic techniques in children.47 The tissue structure can be displayed under ultrasound guidance, and the delivery of local anesthetic drugs can be more precise. Pharmacokinetic and pharmacodynamic guidelines for the safe administration of local anesthetics have also contributed to the development of local anesthesia practice in children, with bupivacaine receiving significant attention and the most relevant literature reports. Furthermore, there is intermediate evidence that local anesthesia reduces the risk of persistent postoperative pain.48 Despite the significant advantages of ultrasound-guided administration of regional anesthesia, significant variation has been reported in the use of regional anesthesia in children.49 As we can see from the results of social network analysis, nodes “Pain, Postoperative/*prevention & control” had the highest degree of centrality. This indicated that they were popular keywords in this field. In addition, nodes “Pain, Postoperative/*prevention and control” belonged to Cluster 4. From the analysis of strategic coordinates, it can be seen that this part of research is in the research center and relatively mature. Because the main content in Cluster 4 is “The safety and effectiveness of regional anesthetic techniques and local anesthetics”, therefore, we predicted that there might be a huge potential for the development of regional anesthesia.
However, some limitations should be noted. First, our data were only collected from the PubMed, and thus, other studies from other databases were not included and analyzed in the research. Second, only articles were included in the present study, and other investigation hotspots may have been missed. Third, biclustering analysis was implemented according to the highly frequent keywords, which may lead to some novel but less frequent subjects being overlooked. Last, visualization software, such as gCLUTO and Ucinet, can only process data from one database at a time, which may result in biased outcomes. Therefore, we should improve the search strategy, include more article types, identify new frequent keywords, and apply more advanced visualization software in the further research.
Conclusion
This study is the first time to analyze postoperative pain in children using a co-word clustering approach. The pharmacological treatment of postoperative pain in children and the prevention and control of pain are currently at the core of this research field and are becoming increasingly mature. Opioid overdose and abuse in the pediatric population have attracted significant international attention, and opioid stewardship is a priority for future research. In addition, it is extremely necessary to develop consensus guidelines for opioid prescribing. Regional anesthesia has great potential for development. Nonpharmacologic intervention for the treatment of postoperative pain in children is an emerging topic. The aetiology and epidemiology of postoperative pain in children are still immature, and future research should be strengthened and intensified.
Acknowledgments
Thanks to the Library of China Medical University for providing electronic data resources, and thanks to all the peer reviewers for their opinions and suggestions.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. Persisting pain in children package: WHO guidelines on the pharmacological treatment of persisting pain in children with medical illnesses; 2012.
2. Groenewald CB, Rabbitts JA, Schroeder DR, et al. Prevalence of moderate-severe pain in hospitalized children. Paediatr Anaesth. 2012;22(7):661–668. doi:10.1111/j.1460-9592.2012.03807.x
3. Kozlowski LJ, Kost-Byerly S, Colantuoni E, et al. Pain prevalence, intensity, assessment and management in a hospitalized pediatric population. Pain Manag Nurs. 2014;15(1):22–35. doi:10.1016/j.pmn.2012.04.003
4. Walker SM. Pain after surgery in children: clinical recommendations. Curr Opin Anaesthesiol. 2015;28(5):570–576. doi:10.1097/ACO.0000000000000227
5. Bonnet F, Marret E. Influence of anaesthetic and analgesic techniques on outcome after surgery. Br J Anaesth. 2005;95(1):52–58. doi:10.1093/bja/aei038
6. Makhlouf MM, Garibay ER, Jenkins BN, et al. Postoperative pain: factors and tools to improve pain management in children. Pain Manag. 2019;9(4):389–397. doi:10.2217/pmt-2018-0079
7. Davidson F, Snow S, Hayden JA, et al. Psychological interventions in managing postoperative pain in children: a systematic review. Pain. 2016;157:1872–1886.
8. Li F, Li M. Mapping publication trends and identifying hot spots of research on Internet health information seeking behavior: a quantitative and co-word biclustering analysis. J Med Internet Res. 2015;17(3):e81. doi:10.2196/jmir.3326
9. Rasmussen M, Karypis G. gCLUTO--An interactive clustering, visualization, and analysis system; 2004.
10. Bai X, Song Z, Zhou Y, et al. Bibliometrics and visual analysis of the research status and trends of postpartum depression from 2000 to 2020. Front Psychol. 2021;12:665181. doi:10.3389/fpsyg.2021.665181
11. Wei W, Ge J, Xu S, et al. Knowledge maps of disaster medicine in china based on co-word analysis. Disaster Med Public Health Prep. 2019;13(03):405–409. doi:10.1017/dmp.2018.63
12. Pandia MK, Bihari A. Important author analysis in research professionals’ relationship network based on social network analysis metrics. In: Computational Intelligence in Data Mining. Springer; Vol. 3, 2015:185–194.
13. Scott J. Software review: a toolkit for social network analysis. Acta Sociol. 1996;39(2):211–216. doi:10.1177/000169939603900205
14. Zieliński J, Morawska-Kochman M, Zatoński T. Pain assessment and management in children in the postoperative period: a review of the most commonly used postoperative pain assessment tools, new diagnostic methods and the latest guidelines for postoperative pain therapy in children. Adv Clin Exp Med. 2020;29(3):365–374. doi:10.17219/acem/112600
15. Carter B. Communicating pain: the challenge of pain assessment in children with profound cognitive impairment. Compr Child Adolesc Nurs. 2020;43(1):10–14. doi:10.1080/24694193.2020.1715105
16. Andersen RD, Nakstad B, Jylli L, et al. The complexities of nurses’ pain assessment in hospitalized preverbal children. Pain Manag Nurs. 2019;20(4):337–344. doi:10.1016/j.pmn.2018.11.060
17. Manworren RC, Stinson J. Pediatric pain measurement, assessment, and evaluation. Semin Pediatr Neurol. 2016;23(3):189–200. doi:10.1016/j.spen.2016.10.001
18. Huguet A, Stinson JN, McGrath PJ. Measurement of self-reported pain intensity in children and adolescents. J Psychosom Res. 2010;68(4):329–336. doi:10.1016/j.jpsychores.2009.06.003
19. Beltramini A, Milojevic K, Pateron D. Pain assessment in newborns, infants, and children. Pediatr Ann. 2017;46(10):e387–e395. doi:10.3928/19382359-20170921-03
20. Birnie KA, Hundert AS, Lalloo C, et al. Recommendations for selection of self-report pain intensity measures in children and adolescents: a systematic review and quality assessment of measurement properties. Pain. 2019;160(1):5–18. doi:10.1097/j.pain.0000000000001377
21. Noel M, Pavlova M, Lund T, et al. The role of narrative in the development of children’s pain memories: influences of father- and mother-child reminiscing on children’s recall of pain. Pain. 2019;160:1866–1875.
22. Power NM, Howard RF, Wade AM, et al. Pain and behaviour changes in children following surgery. Arch Dis Child. 2012;97(10):879–884. doi:10.1136/archdischild-2011-301378
23. Cai Y, Lopata L, Roh A, et al. Factors influencing postoperative pain following discharge in pediatric ambulatory surgery patients. J Clin Anesth. 2017;39:100–104. doi:10.1016/j.jclinane.2017.03.033
24. Lovich-Sapola J, Smith CE, Brandt CP. Postoperative pain control. Surg Clin North Am. 2015;95(2):301–318. doi:10.1016/j.suc.2014.10.002
25. van Munster J, Zamanipoor Najafabadi AH, Schoones JW, et al. The impact of new evidence on regional variation in paediatric tonsillectomy and adenoidectomy: a historical review. J Laryngol Otol. 2020;134(12):1036–1043. doi:10.1017/S002221512000273X
26. Shen L, Lin Z, Lin X, et al. Risk factors associated with obstructive sleep apnea-hypopnea syndrome in Chinese children: a single center retrospective case-control study. PLoS One. 2018;13(9):e0203695. doi:10.1371/journal.pone.0203695
27. Cohen MS, Getz AE, Isaacson G, et al. Intracapsular vs. extracapsular tonsillectomy: a comparison of pain. Laryngoscope. 2007;117(10):1855–1858. doi:10.1097/MLG.0b013e318123ee40
28. Yamada Y, Naitoh Y, Kobayashi K, et al. Laparoendoscopic single-site surgery for pediatric urologic disease. J Endourol. 2016;30(1):24–27. doi:10.1089/end.2015.0130
29. Pérez EV, Lizama GR, Cárdenas VG. Current trends and new strategies in acute postoperative pain management in children. Med Res Arch. 2021;9:32.
30. Brasher C, Gafsous B, Dugue S, et al. Postoperative pain management in children and infants: an update. Paediatr Drugs. 2014;16(2):129–140. doi:10.1007/s40272-013-0062-0
31. Administration UFaD. FDA drug safety communication: FDA restricts use of prescription codeine pain and cough medicines and tramadol pain medicines in children; recommends against use in breastfeeding women;
32. Bindu S, Mazumder S, Bandyopadhyay U. Non-steroidal anti-inflammatory drugs (NSAIDs) and organ damage: a current perspective. Biochem Pharmacol. 2020;180:114147. doi:10.1016/j.bcp.2020.114147
33. Lee Y, Rodriguez C, Dionne RA. The role of COX-2 in acute pain and the use of selective COX-2 inhibitors for acute pain relief. Curr Pharm Des. 2005;2005(11):1737–1755.
34. Radvansky BM, Shah K, Parikh A, et al. Role of ketamine in acute postoperative pain management: a narrative review. Biomed Res Int. 2015;2015:749837. doi:10.1155/2015/749837
35. Thigpen JC, Odle BL, Harirforoosh S. Opioids: a review of pharmacokinetics and pharmacodynamics in neonates, infants, and children. Eur J Drug Metab Pharmacokinet. 2019;44(5):591–609. doi:10.1007/s13318-019-00552-0
36. Calderon T, Hedges E, Livingston MH, et al. Opioid stewardship in pediatric surgery: approaching zero. J Pediatr Surg. 2021;56(3):573–579. doi:10.1016/j.jpedsurg.2020.08.035
37. Gaither JR, Leventhal JM, Ryan SA, et al. National trends in hospitalizations for opioid poisonings among children and adolescents, 1997 to 2012. JAMA Pediatr. 2016;170(12):1195–1201. doi:10.1001/jamapediatrics.2016.2154
38. Gomes T, Tadrous M, Mamdani MM, et al. The burden of opioid-related mortality in the United States. JAMA Netw Open. 2018;1(2):e180217. doi:10.1001/jamanetworkopen.2018.0217
39. Hu QL, Dworsky JQ, Beck AC, et al. Perioperative pain management after ambulatory abdominal surgery: an American college of surgeons systematic review. J Am Coll Surg. 2020;231(5):572–601.e527. doi:10.1016/j.jamcollsurg.2020.07.755
40. Piper KN, Baxter KJ, Wetzel M, et al. Provider education decreases opioid prescribing after pediatric umbilical hernia repair. J Pediatr Surg. 2020;55(7):1319–1323. doi:10.1016/j.jpedsurg.2019.04.035
41. Tobias JD. A review of intrathecal and epidural analgesia after spinal surgery in children. Anesth Analg. 2004;98:956–965. doi:10.1213/01.ANE.0000107938.80562.75
42. Michelet D, Andreu-Gallien J, Bensalah T, et al. A meta-analysis of the use of nonsteroidal antiinflammatory drugs for pediatric postoperative pain. Anesth Analg. 2012;114(2):393–406. doi:10.1213/ANE.0b013e31823d0b45
43. Duedahl TH, Hansen EH. A qualitative systematic review of morphine treatment in children with postoperative pain. Paediatr Anaesth. 2007;17(8):756–774. doi:10.1111/j.1460-9592.2007.02213.x
44. Gunter JB. Benefit and risks of local anesthetics in infants and children. Paediatr Drugs. 2002;4(10):649–672. doi:10.2165/00128072-200204100-00003
45. Mitra S, Carlyle D, Kodumudi G, et al. New advances in acute postoperative pain management. Curr Pain Headache Rep. 2018;22(5):35. doi:10.1007/s11916-018-0690-8
46. Lukosiene L, Rugyte DC, Macas A, et al. Postoperative pain management in pediatric patients undergoing minimally invasive repair of pectus excavatum: the role of intercostal block. J Pediatr Surg. 2013;48(12):2425–2430. doi:10.1016/j.jpedsurg.2013.08.016
47. Veneziano G, Betran R, Bhalla T, et al. Peripheral regional anesthesia in infants and children: an update. Anaesth Pain Intensive Care. 2019;2019:59–71.
48. Levene JL, Weinstein EJ, Cohen MS, et al. Local anesthetics and regional anesthesia versus conventional analgesia for preventing persistent postoperative pain in adults and children: a Cochrane systematic review and meta-analysis update. J Clin Anesth. 2019;55:116–127. doi:10.1016/j.jclinane.2018.12.043
49. Monahan A, Deer J, Robles A, et al. Regional anesthesia in babies and children. Int Anesthesiol Clin. 2019;57(4):e1–e23. doi:10.1097/AIA.0000000000000254
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.