Back to Journals » Journal of Pain Research » Volume 16
Bibliometric Analysis of Research on Temporomandibular Joint and Occlusion from 2000 to 2022
Authors Xiong X , Gao X , Zhong J, Hu S, Li Y, Zheng Y , Liu Y
Received 23 April 2023
Accepted for publication 26 July 2023
Published 16 August 2023 Volume 2023:16 Pages 2847—2860
DOI https://doi.org/10.2147/JPR.S418362
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Alexandre F DaSilva
Xin Xiong,1,2,* Xinlin Gao,1,* Jiawei Zhong,1 Shoushan Hu,1 Yijun Li,1 Yunhao Zheng,1 Yang Liu2
1State Key Laboratory of Oral Diseases & National Clinical Research Center for Oral Diseases & Department of Orthodontics, West China Hospital of Stomatology, Sichuan University, Chengdu, 610041, People’s Republic of China; 2State Key Laboratory of Oral Diseases & National Clinical Research Center for Oral Diseases & Department of Temporomandibular Joint, West China Hospital of Stomatology, Sichuan University, Chengdu, 610041, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yang Liu, State Key Laboratory of Oral Diseases and National Clinical Research Center for Oral Diseases, Department of Temporomandibular Joint, West China Hospital of Stomatology, Sichuan University, No. 14, 3rd Section, Renmin South Road, Chengdu, 610041, People’s Republic of China, Tel +86 028-85503898, Fax +86 018-85503898, Email [email protected]
Purpose: This study conducted a bibliometric analysis that comprehensively described publications on temporomandibular joint and occlusion from 1 January 2000 to 31 October 2022, aiming to reveal hotspots and predict future research trends.
Methods: A total of 2985 articles and reviews were retrieved from Web of Science Core Collection (WoSCC). Excel 2019, VOSviewer and CiteSpace software were used for visualizing analysis of research trends, authors, journals, institutions, countries, keywords and cited references.
Results: Both the annual publication counts and citation times increased significantly. Wang MQ was the most active author. Moreover, Manfredini D and Okeson JP were the most influential two. Journal of Oral Rehabilitation was the core journal. University of Sao Paulo was the most productive institutions. “Temporomandibular disorders” (TMDs), “temporomandibular joint” and “occlusion” were the top 3 keywords with the most frequencies. Keywords and references with burst showed that the causes of TMDs, diagnosis and treatments for TMDs as well as bruxism may be hotspots currently and in the future.
Conclusion: In this study, the research trends, the most productive and influential authors, journals, institutions, countries, in addition to keywords and cited references with burst in the field of temporomandibular joint and occlusion were revealed by a bibliometric analysis, which could help scholars to understand recent hotspots and future trends.
Keywords: bibliometric analysis, temporomandibular joint, occlusion, keywords analysis
Introduction
As one of the most complex joints in the human body, temporomandibular joint (TMJ) plays an important role in breathing, speaking, chewing and many other vital activities.1 However, many associated diseases would affect the normal physiological structures and functions of TMJ, the most prevalent among which are temporomandibular disorders (TMDs).2 As the third most common oral illness in society, TMDs are considered a heterogeneous collection of musculoskeletal and neuromuscular diseases involving the TMJ, muscles of mastication and/or related issues. Nevertheless, many patients suffered from excessive or even detrimental therapy and high expense on account of lacking accurate diagnosis and treatment for TMDs.1 To date, the high complexity, high prevalence and high cost of TMDs have attracted numerous scholars to research on fields related to TMDs.3,4 The correct ways to diagnose and cure TMDs still need to be explored and clarified.
Occlusion matters to TMJ as a central role in dental research.4 Clinically, “occlusion” means not only how teeth contact or near-contact in static positions but also the dynamic morpho-physiological interactions among all the elements of the stomatognathic system, including teeth and their supporting tissues, neuromuscular system, bones and TMJ.5 As part of TMJ functions, dental occlusion has been considered the key to treating TMDs for about 100 years.6 However, since the 1990s, an increasing number of clinical studies and reviews have demonstrated the importance of the biopsychosocial model of TMDs and encouraged dentists to de-emphasize occlusal features as the causal factors for TMDs.5–8 The association between TMDs and occlusion remains a controversial and meaningful topic.
Bibliometrics is a credible method for analyzing large amounts of literature and its relevant metadata (eg, authors, keywords, citations) to reveal the historical development process and explore future trends in specific academic fields.9 Visualization tools such as CiteSpace and VOSviewer software could take full advantage of various data from publications for science mapping, making the process and results of bibliometric analysis clearer and more accessible. For example, a bibliometric analysis of TMDs has revealed the trend of global collaboration among TMD researchers and highlighted the focus areas such as anatomical factors, biopsychosocial factors and epidemiology of TMDs.3 As the debate over the effects of occlusion on TMDs is heated, at the same time, the number of publications on temporomandibular joint and occlusion has increased rapidly in the past two decades. Therefore, the present study comprehensively analyzed the research trends, authors, journals, institutions, countries, keywords and cited references of the related publications in the field of temporomandibular joint and occlusion from 2000 to 2022, aiming to demonstrate research hotspots and to indicate the future trends. Fresh scholars could get a quick understanding of the topic and conduct further research through the results.
Materials and Methods
Data Acquisition
Systematic search was conducted for the publications on temporomandibular joint and occlusion from 1 January 2000 to 31 October 2022 without language restrictions in the Web of Science Core Collection (WoSCC) of the Web of Science (WoS) database. The following search terms were used: (TS = (temporomandibular OR craniomandibular)) AND TS = (occlusion OR occlusal OR malocclusion).
The initial search identified a total of 3096 publications. Only articles and reviews were included after being filtered by the WoS document type filter. Other kinds of publications (eg, meeting abstract, letter) were eliminated. CiteSpace (Version 6.1.R3) was used to exclude duplications. Finally, 2985 publications were included in the present study (Figure 1).
 |
Figure 1 Search strategy and selection process. |
Analysis and Statistics
Excel 2019, CiteSpace and VOSviewer (Version 1.6.18) software were used to carry out bibliometric analyses. Annual publication counts and annual citation times of publications in the field of temporomandibular joint and occlusion from 2000 to 2022 were obtained from the WoS. The trendline was created using Excel 2019. VOSviewer was used to calculate the top 10 most productive authors, institutions, journals, and countries, and to construct co-occurrence or clustering maps for cited authors, cited journals, institutions and countries. CiteSpace was used to create co-citation and clustering visualization maps for references and keywords. The LLR algorithm (showing cluster labels by log-likelihood ratio) was chosen for cluster analysis, and themes were extracted from keywords.
In these maps, a node represented an object and different colors represented different years or clusters. The size of nodes reflected occurrence or citation times. The thicker and shorter the connecting line was, the closer the relationships between different nodes were.10
Keywords and references with burst were detected by burst detection in CiteSpace. The red bar in the time axis showed a burst period. Each detected keyword owned an important parameter value called strength. Larger strength meant more attention attached to a certain keyword or reference (the faster the cited times increased).
Results
Analysis of Research Trends
In total, the present research captured 2985 articles and reviews related to temporomandibular joint and occlusion from January 2000 to October 2022. Overall, the trend line formula of the annual publication counts was y = 51.059e0.0687x(R2=0.9288), showing that it is growing exponentially. The last 22 years could be split into two periods. The first period was from 2000 to 2016, when the annual publication counts and citation times increased slowly, and even decreased in some years. The second period lasted from 2017 to 2022 when publication counts and citation times grew steadily. The five-year growth rates of annual publication counts and citation times in 2021 were 89.86% and 100.51%, respectively, compared with those in 2016. Above all, the field of temporomandibular joint and occlusion received increasing attention and developed rapidly (Figure 2).
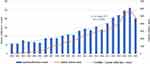 |
Figure 2 Annual publication counts and annual citation counts in the field of temporomandibular joint and occlusion during 2000–2022. |
Analysis of Authors and Journals
The top 10 most productive authors with their total and average citation times are shown in Table 1. Wang MQ was the most active author with the most publications (41) and total citation times (580). However, with fewer publications, Wolford LM had the most average citation times (23.69 times per publication). In the field of temporomandibular joint and occlusion from 2000 to 2022, the clustering map of cited authors showed that cited authors were divided into 4 clusters (Figure 3A). Manfredini D and Okeson JP were the most two influential authors. They belonged to the same cluster and collaborated closely.
 |
Table 1 The Top 10 Most Productive Authors and Countries Contributing to the Research on Temporomandibular Joint and Occlusion in WoSCC |
Table 2 shows the most productive journals in the field of temporomandibular joint and occlusion from 2000 to 2022. Journal of Oral Rehabilitation had the most publications and citation times, indicating that it is the core journal in the field. Although European Journal of Orthodontics ranked tenth, its average citation times were the highest (30.98), demonstrating the high quality of its publications. As is shown in the cluster analysis of cited journals, Journal of Oral Rehabilitation and American Journal of Orthodontics and Dental Orthopedics were the two most influential journals (Figure 3B). In addition, various disciplines were related to temporomandibular joint and occlusion. Function and rehabilitation of temporomandibular joint: Journal of Oral Rehabilitation (with 226 publications and 6646 citations) and Cranio-the Journal of Craniomandibular & Sleep Practice (with 183 publications and 1821 citations). Orthodontics: American Journal of Orthodontics and Dental Orthopedics (with 146 publications and 3375 citations) and Angle Orthodontist (with 78 publications and 2020 citations). Prosthodontics: Journal of Prosthetic Dentistry (with 65 publications and 1202 citations). Oral and maxillofacial surgery: Journal of Oral and Maxillofacial Surgery (with 116 publications and 2601 citations) and International Journal of Oral and Maxillofacial Surgery (with 67 publications and 1372 citations). Scholars might prefer these journals when conducting research or submitting articles related to temporomandibular joint and occlusion. It is also essential to consider the integrity and complexity of the field.
 |
Table 2 The Top 10 Most Productive Journals Contributing to the Research on Temporomandibular Joint and Occlusion in WoSCC |
Analysis of Institutions and Countries
In the last 22 years, the institution named the University of Sao Paulo published the most articles (91 publications) in the field of TMJ and occlusion, followed by the Fourth Military Medical University (71) and Sichuan University (70) (Table 3). University of Gothenburg was the 10th most productive institution, but it is worth highlighting that its average citation times ranked first. On the contrary, Sichuan University published more articles, but its average citation times ranked last among the top 10. As is shown in Figure 3, University of Gothenburg has been involved in the field for more than 10 years, accumulating lots of influence. Sichuan University was the youngest institution in the field.
 |
Table 3 The Top 10 Most Productive Institutions Contributing to the Research on Temporomandibular Joint and Occlusion in WoSCC |
The top 10 most productive countries in the field of temporomandibular joint and occlusion are shown in Table 1. The United States was the first with the most publications and citation times (484, 11,616). Sweden had the highest average citation times, indicating its influence. The co-occurrence analysis of countries demonstrated that the United States was the main research force in the field and cooperated closely with the People’s Republic of China, Brazil, Germany, Italy, etc. (Figure 3D). Moreover, the United States and Germany published articles in this field earlier. The People’s Republic of China and India were later.
Analysis of Keywords
The co-occurrence and cluster analysis maps of the keywords of the publications in the field of temporomandibular joint and occlusion are shown in (Figure 4A and B), respectively. The main research focus was “temporomandibular disorders”, which had a tight connection with “occlusion”, “dysfunction”, “symptom”, “pain” and so on. The second hotspot was “temporomandibular joint”, having a close relationship with “malocclusion”, “occlusal splint”, “sign”, “orthognathic surgery” and so on. All the keywords were clustered into 7 parts. Themes were “orthognathic surgery”, “electromyography”, “myofascial pain”, “sign”, “temporomandibular joint”, “cartilage”, “rheumatoid arthritis”, “physiological occlusion”, illustrating that research in the field focused on the temporomandibular joint, occlusal function, related diseases and orthognathic surgeries. The clustering areas were highly overlapping, showing a great deal crossover among different orientations of research.
The top 25 keywords with the strongest burst could be roughly divided into 3 parts according to their burst years (Figure 5). The first phase was from 2000 to 2010. The main keywords were “mandibular dysfunction”, “young adult”, “symptom” and “functional occlusion”, emphasizing research on patients with temporomandibular joint and occlusion dysfunction. The second one lasted from 2010 to 2016, and “masticatory muscle activity”, “research diagnostic criteria”, “closed treatment”, as well as “risk” were important keywords with burst. Scholars began to study the causes of related diseases, their diagnostic criteria and treatments. The third phase occurred from 2016 to 2022, with “diagnostic criteria”, “surgery” and “cone beam computed tomography” being the main keywords. In recent years, researchers in the field of temporomandibular joint and occlusion concentrated on diagnosis standards and surgical treatment for relevant diseases.
 |
Figure 5 The top 25 keywords with strongest burst in the field of temporomandibular joint and occlusion during 2000–2022. |
Analysis of References
The co-occurrence and cluster analysis networks of cited references are shown in (Figure 6A and B), respectively. The more purple the node was, the older the reference was. The greener, the newer. From 2000 to 2010, the cited references were mainly included in the “orthodontic treatment” and “complete dentures” clusters. In 2010–2016, “splint” and “clenching” were the only two clusters. In the last 6 years, “physiotherapy”, “occlusion” and “juvenile idiopathic arthritis” were the three main clusters.
The top 30 cited references with the strongest burst are shown in Figure 7. The reference with the largest strength was Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications: Recommendations of the International RDC/TMD Consortium Network and Orofacial Pain Special Interest Group by Schiffman et al in 2014, presenting the clinical and experimental usage of new Axis I and Axis II DC/TMD as well as how it was developed.11
 |
Figure 7 The top 30 cited references with strongest burst in the field of temporomandibular joint and occlusion during 2000–2022. |
Many recent publications were detected as references with burst and have lasted until now, which were as follows. “Temporomandibular disorders and dental occlusion. A systematic review of association studies: end of an era?” by Manfredini et al in 2017 reviewed many relevant publications and concluded that dental occlusion could not be regarded as a major factor for temporomandibular disorders.7 “International consensus on the assessment of bruxism: Report of a work in progress” by Lobbezoo et al in 2018, further defined sleep and awake bruxism, respectively, found approaches to assess bruxism and developed a research agenda.12 “Occlusal stabilization splint for patients with temporomandibular disorders: Meta-analysis of short-and long-term effects” by Pficer et al in 2017, employed subgroup analyses and meta-regression. The results showed that stabilization splints were beneficial to TMD patients in the short term.13 Other three publications were “Painful Temporomandibular Disorder: Decade of Discovery from OPPERA Studies” by Slade et al in 2016, “The Evolution of TMD Diagnosis: Past, Present, Future” by Ohrbach et al in 2016 and “Management of pain in patients with temporomandibular disorder (TMD): challenges and solutions” by Gil-Martinez et al in 2018.14–16
Discussion
Causes of TMDs
Two of the most recent references, Slade GD (2016) and Manfredini D (2017) were both related to the causes of TMDs.7,14 The most cited references about the causes of TMDs focus on the relationship between occlusion and TMDs.7,17,18
Occlusion-related factors have long been regarded as the primary causes of TMDs. Before the 1990s, based on the concepts of gnathology, lots of scholars were devoted to constructing “ideal” occlusion to relieve or curing TMDs.5,6 But currently, controversies still exist between dental occlusion and TMDs. In the most cited reference, the multifactorial model of TMDs was recommended and occlusion was just considered as a cofactor.17 Excellent evidence showed that occlusion was less related to TMDs than non-occlusal factors.18 Slade GD (2016) was a summary of various risk factors for TMDs. Based on the multi-factor etiological model for TMDs, it was found that diverse genetic and environmental factors and their complicated interactions resulted in TMDs.14 Furthermore, Manfredini D (2017) assessed 25 articles, of which only two were of high quality and the rest were moderate, and found that features of dental occlusion could not be considered major causes of TMDs due to lack of evidence, similar to the conclusions of some recent reviews.7,19,20 It seemed more appropriate to consider occlusal features as risk factors instead of primary TMD causes. However, it should be noted that the absence of convincing evidence might not mean no associations exist between TMDs and occlusion. Recently, associations between occlusion and TMDs continue to be reported.21,22 Researchers are still trying to clarify the relationship between occlusal factors and TMDs.
Diagnosis and Treatments for TMDs
Three of the most recent references with burst, Ohrbach R (2016), Pficer JK (2017) and Gil-Martinez A (2018) were all related to the diagnosis and treatments for TMDs.13,15,16
The most cited reference related to the diagnosis and treatments for TMDs mentioned Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) and imaging for diagnosis, echoing two of the most recent keywords with burst, “diagnostic criteria” and “cone beam computed tomography”.23 RDC/TMD is one of the most commonly used tools to classify, diagnose and evaluate TMDs. Based on the biopsychosocial model for TMDs, RDC/TMD system consists of two axes, of which one is for clinical symptoms and another is for psychosocial and disability factors.15 In 2014, an updated version of RDC/TMD, Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) was published. According to the presence or absence of pain and specific clinical findings, DC/TMD includes the twelve most common diagnoses of TMDs.11,24 For example, TMD patients with familiar and located pain in the masseter or temporalis upon the site of palpation could be diagnosed as local myalgia. After expansion, DC/TMD has become a more valid and evidence-based system for clinical practice.15 However, patients usually have several disorders and symptoms of pain-related disorders could vary in different individuals, which adds difficulty to the accurate diagnosis by DC/TMD.1 Also, DC/TMD showed low validity for diagnosing some types of disc displacements and degenerative joint diseases, where the imaging might be necessary as supplementary.11,25
Compared with traditional computed tomography (CT) examination, cone beam computed tomography (CBCT) has the same accuracy for TMD diagnosis while radiating less and costing less time.26 However, clinicians are advised to perform CBCT only when the results are quite significant for them to choose treatments due to its poor specificity.27 A systematic review demonstrated that CBCT may be appropriate for TMD patients with TMJ arthralgia and joint noises.28 CBCT could be used to assess degenerative joint diseases by detecting bony changes of TMJ.26 Besides clinical examinations, radiological images could assist clinicians to make a definitive diagnosis of degenerative joint lesions such as osteophytes and sclerosis.27 Torre A. et al reviewed that CBCT was widely used for TMJ diagnosis, but studies assessing diagnostic thinking efficacy and therapeutic efficacy of CBCT were needed.29 As for disc displacement disorders, magnetic resonance imaging (MRI) was recognized as the gold standard now. Notably, high-quality MR images, open-mouth images and consistent definition of normal disc position could positively affect observers’ performances.29
Treatments for TMDs are various, yet no common sense and no convincing clinical practice guidelines based on evidence exist at present. The most cited reference on the diagnosis and treatments for TMDs and Pficer JK (2017) both mentioned occlusal splints as a conservative treatment for TMDs.13,23 It was revealed that occlusal stabilization splints had more significant effects in short term than other control groups and recommended that more well-designed randomized controlled trials (RCTs) on long-term effects were needed. Significantly, a much-referenced publication about oral splints referred to the placebo theory of oral splints.30 Occlusal splints might improve TMDs by placebo effects because non-occluding/placebo splints could also positively affect TMD patients in most cases. However, TMD patients with occlusal splints showed greater treatment satisfaction, although placebo splints seemed to work as well as occlusal ones in reducing TMD pain.31 Moreover, a recent study found that the efficacy of placebo splints might not maintain for long.32 Oral splints were probably more effective than placebo, but the mechanism was still unclear.
In response to one of the most recent keywords “oral health”, a much-cited publication on treatments for TMDs focused on the biopsychosocial model of TMDs.8 The biopsychosocial model for TMDs expected to manage patients with chronic diseases by rehabilitation concepts, instead of pursuing permanent cures. Patient-centered interventions improving quality of life gained more popularity.33 An increasing number of clinicians get access to patients’ subjective feelings about TMD pain through patient-reported outcomes (PROs) so that they could better reduce the biopsychosocial impacts of TMDs.34 The Oral Health Impact Profile (OHIP) scale is the most common PRO measurement tool for patients’ oral health-related quality of life (OHRQoL) which could be divided into four dimensions, orofacial function, pain, appearance and psychological status.35 Based on OHIP, Durham et al created a TMD-specific scale called OHIP-TMDs and confirmed its good validity and reliability.36,37 To some extent, OHRQoL has become an evaluation index for treatments. Song et al reviewed that most TMD treatments seem to improve patients’ quality of life to some extent.38 However, the statement was slightly ambiguous. Further studies should pay more attention to disease-specific OHRQoL measures and accurate diagnoses for TMDs based on internationally accepted criteria.
Bruxism
One of the most recent references with burst, Lobbezoo F (2018) indicated that “bruxism” was another hotspot in the field of temporomandibular joint and occlusion.12
The two most cited publications about bruxism both focused on the etiology of bruxism.39,40 Lobbezoo et al divided the causes of bruxism into peripheral/morphological (eg, malocclusion) and central/psychosocial & biological (eg, stress and anxiety) ones, demonstrating that central causes play more significant roles. For example, depression and anxiety could increase the risk of bruxism by acting as stressors to stimulate individuals to release adrenaline, leading to higher muscle tension.41,42 However, abnormalities in dental occlusion have historically been thought as the main causal factors for bruxism by affecting muscle activity in the past. However, the relationship between occlusion and bruxism rarely seemed to be supported by convincing evidence-based data. In 2012, a review by Lobbezoo et al concluded that no proof could show a causal relationship between bruxism and malocclusion.43 Although Ribeiro-Lages et al recently concluded that associations exist between bruxism and crowding, other than Angle class I, II and III malocclusions, the quality of the studies was also unsatisfactory mostly due to the changing diagnosis for bruxism and too many cofounders in the analysis.44 Similar conclusions were also reached in research on the relationship between bruxism and TMDs. Different ways to assess SB could greatly affect the final research results on whether any association exists between SB and TMDs.45 Four kinds of assessment approaches for bruxism were introduced in Lobbezoo F (2018). Nevertheless, reliable assessment ways for bruxism were still in need.
The limitations of bibliometrics could be listed as follows: (1) In the present study, publications were acquired from WoSCC and considered as the whole literature in a period in the field, but eligible publications in other databases were excluded. (2) Synonyms like “temporomandibular disorders” and “craniomandibular disorders” could only be merged as one word by manual work rather than software function. In case of negligence, the results would be biased. (3) To make the analysis maps clearer, we should make some adjustments and try not to change their meanings. However, the incomplete functions of bibliometric tools make the process difficult and time-consuming. (4) Researchers might explain the same analysis maps differently, so the interpretations for the results of the bibliometric analysis might be inevitably subjective.
Conclusions
In the present study, we conducted a bibliometric analysis for publications on temporomandibular joint and occlusion from 2000 to 2022. The findings could be concluded as follows:
Annual publications and citation times increased obviously. Journal of Oral Rehabilitation was the most impactful journal in this field. Author analysis indicated that Wang MQ was the most productive and Manfredini D the most influential. The top 3 most productive institutions were University of Sao Paulo, The Fourth Military Medical University and Sichuan University. “Temporomandibular disorders” (TMDs), “temporomandibular joint” and “occlusion” were the top 3 keywords with the most frequencies.
Keywords and references with burst showed that the causes of TMDs, diagnosis and treatments for TMDs as well as bruxism may be current and future hotspots. The associations among TMDs, occlusion and SB were the main controversial issues. To clarify the associations, scholars should make efforts to unify the concepts and definitions of terms, establish common standard diagnostic criteria for TMDs and bruxism, and conduct research with more convincing evidence.
Data Sharing Statement
The raw data can be directly obtained from the WOS Core Collection database.
Funding
This work was supported by the Natural Science Foundation of Sichuan Province [23NSFSC1708], Technology Innovation Project of Science and Technology Bureau of Chengdu [2022-YF05 −01691-SN] and Clinical Research Project of West China Hospital of Stomatology, Sichuan University [RD-03-202005, LCYJ2023-YF-3 and LCYJ-2023-YY-2].
Disclosure
The authors report no conflicts of interest in this work.
References
1. Yost O, Liverman CT, English R, Mackey S, Bond EC. Temporomandibular Disorders: Priorities for Research and Care. National Academies Press; 2020. doi:10.17226/25652
2. Acri TM, Shin K, Seol D, et al. Tissue engineering for the temporomandibular joint. Adv Healthc Mater. 2019;8(2):e1801236. doi:10.1002/adhm.201801236
3. Bai B, Bai X, Wang C. Mapping research trends of temporomandibular disorders from 2010 to 2019: a bibliometric analysis. J Oral Rehabil. 2021;48(5):517–530. doi:10.1111/joor.13143
4. de Kanter R, Battistuzzi P, Truin GJ. Temporomandibular disorders:“occlusion” matters!. Pain Res Manag. 2018;2018:8746858. doi:10.1155/2018/8746858
5. Turp JC, Greene CS, Strub JR. Dental occlusion: a critical reflection on past, present and future concepts. J Oral Rehabil. 2008;35(6):446–453. doi:10.1111/j.0305-182X.2007.01820.x
6. Kandasamy S, Greene CS. The evolution of temporomandibular disorders: a shift from experience to evidence. J Oral Pathol Med. 2020;49(6):461–469. doi:10.1111/jop.13080
7. Manfredini D, Lombardo L, Siciliani G. Temporomandibular disorders and dental occlusion. A systematic review of association studies: end of an era? J Oral Rehabil. 2017;44(11):908–923. doi:10.1111/joor.12531
8. Suvinen TI, Reade PC, Kemppainen P, et al. Review of aetiological concepts of temporomandibular pain disorders: towards a biopsychosocial model for integration of physical disorder factors with psychological and psychosocial illness impact factors. Eur J Pain. 2005;9(6):613–633. doi:10.1016/j.ejpain.2005.01.012
9. Ninkov A, Frank JR, Maggio LA. Bibliometrics: methods for studying academic publishing. Perspect Med Educ. 2022;11(3):173–176. doi:10.1007/s40037-021-00695-4
10. Chen C. Science mapping: a systematic review of the literature. J Data Inf Sci. 2017;2(2):1–40. doi:10.1515/jdis-2017-0006
11. Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the international RDC/TMD consortium network and orofacial pain special interest groupdagger. J Oral Facial Pain Headache. 2014;28(1):6–27. doi:10.11607/jop.1151
12. Lobbezoo F, Ahlberg J, Raphael KG, et al. International consensus on the assessment of bruxism: report of a work in progress. J Oral Rehabil. 2018;45(11):837–844. doi:10.1111/joor.12663
13. Kuzmanovic Pficer J, Dodic S, Lazic V, et al. Occlusal stabilization splint for patients with temporomandibular disorders: meta-analysis of short and long term effects. PLoS One. 2017;12(2):e0171296. doi:10.1371/journal.pone.0171296
14. Slade GD, Ohrbach R, Greenspan JD, et al. Painful temporomandibular disorder: decade of discovery from OPPERA studies. J Dent Res. 2016;95(10):1084–1092. doi:10.1177/0022034516653743
15. Ohrbach R, Dworkin SF. The evolution of TMD diagnosis: past, present, future. J Dent Res. 2016;95(10):1093–1101. doi:10.1177/0022034516653922
16. Gil-Martinez A, Paris-Alemany A, Lopez-de-Uralde-Villanueva I, et al. Management of pain in patients with temporomandibular disorder (TMD): challenges and solutions. J Pain Res. 2018;11:571–587. doi:10.2147/JPR.S127950
17. Pullinger AG, Seligman DA. Quantification and validation of predictive values of occlusal variables in temporomandibular disorders using a multifactorial analysis. J Prosthet Dent. 2000;83(1):66–75. doi:10.1016/s0022-3913(00)70090-4
18. Turp JC, Schindler H. The dental occlusion as a suspected cause for TMDs: epidemiological and etiological considerations. J Oral Rehabil. 2012;39(7):502–512. doi:10.1111/j.1365-2842.2012.02304.x
19. Kalladka M, Young A, Thomas D, et al. The relation of temporomandibular disorders and dental occlusion: a narrative review. Quintessence Int. 2022;53(5):450–459. doi:10.3290/j.qi.b2793201
20. Alqhtani N, Alshammery D, AlOtaibi N, et al. Correlations between mandibular asymmetries and temporomandibular disorders: a systematic review. J Int Soc Prev Community Dent. 2021;11(5):481–489. doi:10.4103/jispcd.JISPCD_130_21
21. Zuniga-Herrera ID, Herrera-Atoche JR, Escoffie-Ramirez M, et al. Malocclusion complexity as an associated factor for temporomandibular disorders. A case-control study. Cranio. 2021:1–6. doi: 10.1080/08869634.2020.1868907.
22. Tervahauta E, Narhi L, Pirttiniemi P, et al. Prevalence of sagittal molar and canine relationships, asymmetries and midline shift in relation to temporomandibular disorders (TMD) in a Finnish adult population. Acta Odontol Scand. 2022;80(6):470–480. doi:10.1080/00016357.2022.2036364
23. Gauer RL, Semidey MJ. Diagnosis and treatment of temporomandibular disorders. Am Fam Physician. 2015;91(6):378–386.
24. List T, Jensen RH. Temporomandibular disorders: old ideas and new concepts. Cephalalgia. 2017;37(7):692–704. doi:10.1177/0333102416686302
25. Li DTS, Leung YY. Temporomandibular disorders: current concepts and controversies in diagnosis and management. Diagnostics. 2021;11(3). doi:10.3390/diagnostics11030459
26. Larheim TA, Abrahamsson AK, Kristensen M, et al. Temporomandibular joint diagnostics using CBCT. Dentomaxillofac Radiol. 2015;44(1):20140235. doi:10.1259/dmfr.20140235
27. Dygas S, Szarmach I, Radej I. Assessment of the morphology and degenerative changes in the temporomandibular joint using CBCT according to the orthodontic approach: a scoping review. Biomed Res Int. 2022;2022:6863014. doi:10.1155/2022/6863014
28. Wu M, Almeida FT, Friesen R. A systematic review on the association between clinical symptoms and CBCT findings in symptomatic TMJ degenerative joint disease. J Oral Facial Pain Headache. 2021;35(4):332–345. doi:10.11607/ofph.2953
29. Larheim TA, Hol C, Ottersen MK, et al. The role of imaging in the diagnosis of temporomandibular joint pathology. Oral Maxillofac Surg Clin North Am. 2018;30(3):239–249. doi:10.1016/j.coms.2018.04.001
30. Klasser GD, Greene CS. Oral appliances in the management of temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107(2):212–223. doi:10.1016/j.tripleo.2008.10.007
31. Alkhutari AS, Alyahya A, Rodrigues Conti PC, et al. Is the therapeutic effect of occlusal stabilization appliances more than just placebo effect in the management of painful temporomandibular disorders? A network meta-analysis of randomized clinical trials. J Prosthet Dent. 2021;126(1):24–32. doi:10.1016/j.prosdent.2020.08.015
32. Vrbanovic E, Alajbeg IZ. Long-term effectiveness of occlusal splint therapy compared to placebo in patients with chronic temporomandibular disorders. Acta Stomatol Croat. 2019;53(3):195–206. doi:10.15644/asc53/3/1
33. Dahlstrom L, Carlsson GE. Temporomandibular disorders and oral health-related quality of life. A systematic review. Acta Odontol Scand. 2010;68(2):80–85. doi:10.3109/00016350903431118
34. Haggman-Henrikson B, Lobbezoo F, Durham J, et al. The Voice of the Patient in Orofacial Pain Management. J Evid Based Dent Pract. 2022;22(1S):101648. doi:10.1016/j.jebdp.2021.101648
35. John MT, Rener-Sitar K, Baba K, et al. Patterns of impaired oral health-related quality of life dimensions. J Oral Rehabil. 2016;43(7):519–527. doi:10.1111/joor.12396
36. Durham J, Steele JG, Wassell RW, et al. Creating a patient-based condition-specific outcome measure for temporomandibular disorders (TMDs): oral health impact profile for TMDs (OHIP-TMDs). J Oral Rehabil. 2011;38(12):871–883. doi:10.1111/j.1365-2842.2011.02233.x
37. Yule PL, Durham J, Playford H, et al. OHIP-TMDs: a patient-reported outcome measure for temporomandibular disorders. Community Dent Oral Epidemiol. 2015;43(5):461–470. doi:10.1111/cdoe.12171
38. Song YL, Yap AU. Outcomes of therapeutic TMD interventions on oral health related quality of life: a qualitative systematic review. Quintessence Int. 2018;49(6):487–496. doi:10.3290/j.qi.a40340
39. Lavigne GJ, Khoury S, Abe S, et al. Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil. 2008;35(7):476–494. doi:10.1111/j.1365-2842.2008.01881.x
40. Lobbezoo F, Naeije M. Bruxism is mainly regulated centrally, not peripherally. J Oral Rehabil. 2001;28(12):1085–1091. doi:10.1046/j.1365-2842.2001.00839.x
41. Gungormus Z, Erciyas K. Evaluation of the relationship between anxiety and depression and bruxism. J Int Med Res. 2009;37(2):547–550. doi:10.1177/147323000903700231
42. Wieckiewicz M, Paradowska-Stolarz A, Wieckiewicz W. Psychosocial aspects of bruxism: the most paramount factor influencing teeth grinding. Biomed Res Int. 2014;2014:469187. doi:10.1155/2014/469187
43. Lobbezoo F, Ahlberg J, Manfredini D, et al. Are bruxism and the bite causally related? J Oral Rehabil. 2012;39(7):489–501. doi:10.1111/j.1365-2842.2012.02298.x
44. Ribeiro-Lages MB, Martins ML, Magno MB, et al. Is there association between dental malocclusion and bruxism? A systematic review and meta-analysis. J Oral Rehabil. 2020;47(10):1304–1318. doi:10.1111/joor.12971
45. Manfredini D, Lobbezoo F. Sleep bruxism and temporomandibular disorders: a scoping review of the literature. J Dent. 2021;111:103711. doi:10.1016/j.jdent.2021.103711
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



