Back to Journals » Journal of Pain Research » Volume 16
Bibliometric Analysis of Research on Migraine-Stroke Association from 2013 to 2023
Authors Zhang L , Zhang H, Zhou X, Zhao J, Wang X
Received 3 October 2023
Accepted for publication 22 November 2023
Published 1 December 2023 Volume 2023:16 Pages 4089—4112
DOI https://doi.org/10.2147/JPR.S438745
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Rushna Ali
Long Zhang,1,2,* Hongyan Zhang,3,4,* Xue Zhou,1 Jing Zhao,5 Xingchen Wang6
1First Clinical Medical College, Shandong University of Traditional Chinese Medicine, Jinan, Shandong, People’s Republic of China; 2Department of Traditional Chinese Medicine, Zibo TCM-Integrated Hospital, Zibo, Shandong, People’s Republic of China; 3Department of Traditional Chinese Medicine, Shanghai Sixth People’s Hospital, Shanghai, People’s Republic of China; 4Shaanxi Key Laboratory of Research on TCM Physical Constitution and Diseases Prevention and Treatment, Shaanxi University of Chinese Medicine, Xianyang, Shaanxi, People’s Republic of China; 5Experimental Center, Shandong University of Traditional Chinese Medicine, Jinan, Shandong, People’s Republic of China; 6Division of Neurology, the Second Affiliated Hospital of Shandong University of Traditional Chinese Medicine, Jinan, Shandong, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xingchen Wang, Division of Neurology, the Second Affiliated Hospital of Shandong University of Traditional Chinese Medicine, No. 1 Jingba Road, Jinan, Shandong, 250001, People’s Republic of China, Tel +86 0531 58261203, Email [email protected]
Background: Both migraine and stroke heavily burden individuals, health systems, and society. The migraine-stroke association is of concern and has been studied widely. Our objective is to explore and overview the current research status and emerging trends.
Materials and Methods: Studies on migraine-stroke association from January 2013 to May 2023 were retrieved and screened from the Web of Science Core Collection (WOSCC) database. Records fulfilling the selection criteria were downloaded and imported into CiteSpace for data mining and visualization.
Results: A total of 862 papers on migraine-stroke association were included. Annual publications grew slowly. The United States and European countries dominated research in this area. Harvard University published the largest number of articles, while the University of London was most active with other institutions. Ayata Cenk contributed the most articles, while KURTH T and NEUROLOGY were co-cited most. Research hotspots included migraine with aura, ischemic stroke, patent foramen ovale, cortical spreading depolarization, meta-analysis, cross-sectional study, and risk factors. Pathophysiology and small vessel disease represented research frontiers and emerging trends.
Conclusion: Our study scientifically outlines the migraine-stroke association over the past decade, presenting useful information.
Keywords: migraine with aura, ischemic stroke, patent foramen ovale, cortical spreading depolarization, pathophysiology, CiteSpace
Introduction
Migraine is a highly prevalent neurological disorder and one of the most disabling diseases worldwide,1 affecting approximately 15% of the total global population.2 It is more prevalent among women and has a particular impact on young adults, with peak prevalence occurring between the ages of 35 and 39.2,3 According to the 3rd edition of International Classification of Headache Disorders (ICHD-3), migraine headaches are classified into six subtypes, including (1) migraine without aura (MO), (2) migraine with aura (MA), (3) chronic migraine, (4) complications of migraine, (5) probable migraine, and (6) episodic syndromes that may be associated with migraine.4 MO and MA are the two most common subtypes.4 MO manifests as a unilateral, throbbing, moderate or severe headache with at least 5 attacks lasting 4–72 hours. MO is aggravated by routine physical activity and accompanied by nausea, photophobia and phonophobia. MA is characterized by unilateral, transient, and fully reversible neurological symptoms accompanied or followed by migraine-related symptoms, with at least two attacks. The aura symptoms usually manifest as visual, sensory, speech, motor, brainstem, and retinal deficits, lasting minutes.4 The cause of migraine is multifactorial, involving genetic, metabolic, endocrine, psychological, dietary, and environmental factors. Defined as a neurovascular disorder, migraine attacks are associated with neurologic dysfunction, abnormal vascular activity, and excessive neuropeptide release.5
Stroke is one of the leading diseases causing disability and death worldwide, posing a serious threat to human health.6 Briefly, stroke is an acute cerebrovascular disorder resulting in neurological deficits due to sudden rupture of blood vessels in the brain or occlusion of blood vessels supplying the brain, retina or spinal cord. Typical clinical manifestations of stroke are sudden onset of focal neurologic deficits, including unilateral numbness, weakness, or loss of vision; speech disturbances; dysphagia; diplopia; ataxia and vertigo.7 There are two main types of stroke: ischemic and hemorrhagic. Ischemic stroke is more prevalent than hemorrhagic stroke, accounting for approximately 87% of total strokes.8 Stroke is predominantly in elderly adults and is strongly associated with traditional vascular risk factors, such as hypertension, diabetes, obesity, smoking, and alcohol consumption.8 Ischemic stroke is mainly caused by artery-to-artery embolism from atherosclerotic plaque, embolism from the heart, and intracranial atherosclerosis with in-situ thrombosis.9 For younger stroke patients, cervical artery dissection is a common etiology. Severely decreased cerebral blood flow leads to cessation of neuronal electrical activity and clinical deficits. If reperfusion is not restored promptly, irreversible brain tissue lesions develop rapidly. The common causes of intracerebral hemorrhage are vasculopathy related to hypertension, cerebral amyloid angiopathy, anticoagulation, and vascular structural damage.7
Both migraine and stroke place a heavy burden on the individual and society.10,11 During the study of migraine and stroke, the association between the two has gradually attracted the attention of researchers. Migraine and stroke differ significantly in terms of predominant age, gender, and prognosis; however, growing evidence suggests a strong association between them.12 Although the findings on this association are not consistent, most suggest that the presence of migraine increases the risk of stroke.13 In the past decades, researchers have explored the migraine-stroke association from various aspects of epidemiology, genetics, neuroimaging, and pathophysiology. Although there have been many reviews that have systematically elucidated the progress of the research, to our knowledge, there is currently no bibliometric report that summarizes the field.
Bibliometrics allows quantitative analysis of a large number of published academic articles in a given field using a variety of tools to uncover valid information in the literature. Citespace, invented by Prof. Chaomei Chen, is an excellent visual bibliometric tool, consisting of three modules: collaboration network, co-occurrence network, and co-citation network.14,15 The collaboration network enables the visualization of the scientific outputs and collaborations of an element (country, institution, author) in the research field of the migraine-stroke association, helping researchers to understand the academic contributions of the element, find potential partners, and promote academic collaborations and exchanges. The co-citation network can visualize the academic influence of an element (author, journal, reference) in the field and help researchers identify key elements (reference, journal, researcher). The reference co-citation network and the keyword co-occurrence network compose the knowledge base of the field. By identifying high-frequency keywords and keywords with high centrality, CiteSpace can help researchers rapidly understand the research hotspots, key issues, and relevant research results in this field. Timeline and citation burst detection help researchers to explore research trends and future research directions through temporal localization.
There have been several bibliometric studies of migraine using CiteSpace, but no migraine-stroke association was investigated.16–18 In this study, we were the first to use CiteSpace software to conduct a bibliometric analysis of the literature collected from WOSCC to provide a comprehensive understanding of the migraine-stroke association. We have three objectives: firstly, to identify the contributions and collaborations of countries, institutions, journals, and individuals in the field of migraine-stroke association through the analysis of collaboration networks and co-citation networks (authors and journals); secondly, to explore the research hotspots through the analysis of keyword co-occurrence networks and co-citation networks (references); and thirdly, to explore the new hotspots and research trends through the burst detection.
Materials and Methods
Data Collection
All relevant data were retrieved from the WOSCC Database on August 19, 2023. The search strategy was as follows: #1 (TS=(stroke) OR TS= (“brain infarct”) OR TS= (“cerebral infarct”) OR TS= (“cerebrovascular disease”) OR TS= (“transient ischemic attack”) OR TS= (“intracranial hemorrhage”); #2 TS= (migraine); #1 AND #2. A total of 1810 articles were retrieved. The selection process was shown in Figure 1A, using the following criteria: Time frame for publication: From January 1st, 2013, to May 1st, 2023. Limited article types: article or review article. Limited languages: English. Exclusion criteria: meeting abstract; proceeding paper; editorial material; early access; book chapters; letter and correction; non-English studies. After the above screening, 1543 articles were left. Two authors independently read the records to exclude literature not relevant to the topic. Exclusion criteria: tension-type headache; trigeminal autonomic cephalalgias; secondary headaches; other studies that explicitly exclude migraine; studies that explicitly exclude stroke. Ultimately, a total of 862 retrieved records with cited references were exported to perform data mining.
 |
Figure 1 (A) Research flow chart. (B) Annual publications trends chart. |
Analysis Tool
CiteSpace 6.2.R4 (Advanced) was used to perform a bibliometric analysis. All 862 records were left after removing duplicates. The following parameters were changed: node type (choose as needed), selection criteria (top N=30), and pruning (pathfinder, pruning sliced and merged network). Other parameters: default.
In the network map generated by Citespace, each node represents an element that fulfills the selection criteria. The larger the node, the higher the frequency of that element. The links between different nodes represent co-occurrence relationships between different elements. The thicker the link, the stronger the intensity of co-occurrence. A node colored with a purple circle implies that the node has a betweenness centrality value of more than 0.10. Such nodes are important in the studied field serving as turning points or bridges. The solid line on the timeline represents the active duration of the cluster. In clustering maps, Q-values and S-values are very important. Q > 0.3 and S > 0.7 indicate that the clustering is well-structured and highly credible.19 The larger the cluster size, the smaller the ordinal number. In the citation burst map, the dark green solid line represents the active duration of the element, while the red solid line represents the burst duration.
Results
Analysis of Annual Publications
A total of 862 papers published from 2013 to 2023 were analyzed for annual volume. As shown in Figure 1B, the annual trend in the publications has been relatively stable in the past decade, with no particularly striking changes. The number of articles published per year fluctuated around 80 from 2013 to 2018. There was a slight increase from 2019 to 2022, no less than 85 articles per year. The peak was in 2021 when a total of 99 articles were published.
To further assess the value of annual publications, total citations in WOS at the date of retrieval were counted. As shown, articles published in 2015 had the most citations, with a total of 3370 times, followed by 2013 and 2014. Since objectively the earlier the article is published, the more likely it is to be cited. To exclude the effect of time, we calculated the average citations, which was the total citations divided by the time interval. 2015 remained the most cited year, followed by 2022 and 2021.
Visual Distribution of Countries (Regions) and Institutions
Collaborative networks of countries and regions were shown in Figure 2A, including 66 nodes, 401 links, and a density of 0.1869. 66 nodes represented 66 countries (regions) fulfilling the selection criteria, the top 10 of which were shown in Figure 2B. The United States contributed 293 articles ranking first, followed by Italy (n=115), Germany (n=92), and China (n=89). 8 of the top 10 productive countries were from Europe. In terms of betweenness centrality, the United States (0.60) also came in first place (Figure 2C). The other 4 countries with high centrality values (>0.10) were from Europe.
 |
Figure 2 (A) The collaborative network of countries (regions). (B) The top 10 high-productive countries (country frequency). (C) The top 5 countries with the highest centrality. |
The distribution networks of institutions were shown in Figure 3A. Node = 308, Link = 1470, Density = 0.0311. Nodes represented institutions. The top 10 institutions in frequency were listed in Figure 3B. Harvard University from the United States was at the top with 63 articles. 3 of the top 10 productive institutes were from the United States, 3 from Germany, 2 from France, 1 from the Netherlands, and 1 from Denmark. Despite having published only 10 articles, University of London ranked first in terms of centrality (0.17, Figure 3C), indicating that it collaborated widely with other institutions. The other institutions with high centrality (>0.1) were University of California System (0.13) Charite Universitatsmedizin Berlin (0.11), Assistance Publique Hopitaux Paris (0.11), and University of Utah (0.11).
 |
Figure 3 (A) The collaborative network of institutes. (B) The top 10 high-productive institutes. (C) The top 5 institutes with the highest centrality. |
The knowledge maps visualized the academic contributions and collaborations of countries or institutions. The findings showed that the study was dominated by developed countries and their institutions, especially the United States and European countries. The importance of migraine-stroke association has not been emphasized by developing countries, with insufficient research inputs and cooperation.
Analysis of Author Collaboration Network
A co-author map with 3417 nodes and 11,257 links was generated by CiteSpace (Figure 4A). Several scientific research groups were clearly represented in this map. Figure 4B showed the top 12 productive authors, among which Ayata Cenk (23 articles) ranked first, followed by Michel D (20 articles), Terwindt Gisela M (20 articles), and Kurth Tobias (19 articles).
 |
Figure 4 (A) The collaborative network of authors. (B) The top 12 high-productive authors. |
This knowledge map visualized the academic contributions and collaborations of the researchers. Despite numerous researchers participating in this field, the research groups were scattered and lacked wide collaboration. It should be noted that the analysis of researchers’ academic contributions is still incomplete and somewhat biased because CiteSpace cannot identify first authors, corresponding authors and other authors in this knowledge map.
Analysis of Co-Cited Authors
Another way to study the impact of authors on the field is through the analysis of co-cited authors. As presented in the author co-citation map (Figure 5A), there were 122 nodes and 792 links. A total of 15 authors had been cited more than 100 times, of which the top 10 were displayed in Figure 5B. The largest node in this map was KURTH T, cited 243 times. Following KURTH T, SACCO S (156 citations) and SILBERSTEIN SD (156 citations) also ranked top 3. In addition, KURTH T ranked first in terms of centrality (0.26, Figure 5C), followed by EIKERMANN-HAERTER K (0.22) and NOZARI A (0.22).
The top 10 cited authors with the strongest citation bursts were shown in Figure 5D. More attention was paid to MAHMOUD AN, ADELBORG K, ALTAMURA C, and HU XM at the latest stage. A meta-analysis with over 1.1 million subjects published by MAHMOUD AN in 2018 provided evidence of increased risk of stroke and myocardial infarction from migraine.20 This conclusion was supported by the cohort study of ADELBORG K.21 In addition to myocardial infarction and stroke, ADELBORG K et al found an association between migraine and an increased risk of atrial fibrillation or atrial flutter. Another earlier meta-analysis published in 2017 by HU XM failed to find an association between migraine and hemorrhagic stroke but supported an association between migraine and total or ischemic stroke.22 The observational study by ALTAMURA C et al found that estrogen therapy decreased effective vasomotor reactivity in MA, partially explaining estrogen’s increased risk of stroke in female migraineurs.23 Interestingly, protective cerebral hemodynamic alterations were observed in patients with MA in right-to-left shunt (RLS), suggesting that not all of the increased stroke risk in MA is due to harmful hemodynamic alterations. In another observational study, administration of erenumab did not affect endothelial function or cerebral vasomotor reactivity in MO.24
The analysis of co-cited authors highlighted the most influential authors in this field, whose findings were widely recognized. Citation burst detection showed authors with bursting trends in influence at different stages. We focused on four authors with current bursting trends and summarized their important findings.
Analysis of Co-Cited Journals
Academic journals are important platforms for publishing the latest scientific research progress and achievements and promoting academic exchanges and dissemination. By statistical analysis of co-cited journals, we can evaluate the influence of journals more objectively and discover the key sources of knowledge more efficiently in this field. This network map (Figure 6A) consisted of 59 nodes and 365 links. Among the top 10 co-cited journals in frequency listed in Figure 6B, NEUROLOGY ranked first with an impact factor (IF) of 9.9, followed by STROKE (IF=8.3), CEPHALALGIA (IF=4.9), and HEADACHE (IF=5). The other 6 journals had an impact factor of more than 10, including LANCET (IF=168.9), NEW ENGL J MED (IF=158.5), BMJ-BRIT MED J (IF=105.7), LANCET NEUROL IF=48), BRAIN (IF=14.5) and ANN NEUROL (IF=11.2). Journals with centrality >0.1 were shown in Figure 6C, including ANN NEUROL, BRAIN, NEW ENGL J MED, CIRCULATION (IF=37.8), LANCET and AM J MED (IF=5.9). The fact that only 59 journals met the selection criteria suggested that research in this area was somewhat less popular and more concentrated. However, relevant articles published in these high-quality journals hinted at the importance of research in this field.
 |
Figure 6 (A) The network of co-cited journals. (B) The top 10 co-cited journals in frequency. (C) The top 6 co-cited journals in centrality. (D) The dual-map overlays of co-cited journals. |
The distribution of major disciplines in the research field of the migraine-stroke association was displayed in the dual-map overlay of journals (Figure 6D). A total of five main citation paths were shown in this map. There was only one orange path (z=3.13, f =3424), representing that publications from the Molecular/Biology/Immunology field were primarily influenced by ones from the Molecular/Biology/Genetics field. Two green paths showed that publications from the Medicine/Medical/Clinical field were influenced by ones from the Health/Nursing/Medicines (z=2.55, f= 2864) and Psychology/Education/Society (z=1.67, f= 2008), respectively. Three pink pathways paths indicated that publications from the fields of Neurology/Sports/Ophthalmology were significantly influenced by publications from the fields of Molecular/ Biology/Genetics (z=4.23, f= 4490), Health/Nursing/Medicines (z=2.94, f= 3240), and Psychology/Education/ Society (z=2.73, f= 3040), respectively.
The analysis of co-cited journals highlighted the most influential journals in the field, where articles published were widely accepted. Journals with high centrality served as bridges between different studies and contributed significantly to the development of the field. It also revealed that these high-quality journals maintained a greater interest in the topic and were suitable for submissions by researchers in the field. The dual map overlay reflected the interplay between disciplines relevant to the field, exploring the migraine-stroke association from a variety of disciplinary perspectives.
Analysis of Co-Cited References
The co-cited references network map (Figure 7A) included 254 nodes and 1267 links. 254 nodes represented 254 co-cited references meeting the selection criteria. Table 1 lists the top 10 co-cited references in frequency. The two editions (including the third and beta one) of the International Classification of Headache Disorders published in Cephalalgia were used primarily as a basis for the subtype classification of migraine.4,25 The rest included 1 review, 2 randomized controlled trials (RCTs), 2 cohort studies, and 3 meta-analyses. The prospective cohort study published by Kurth T in BMJ-BRIT MED J (IF 105.7) in 2016 was the second most cited article, showing an association between migraine and increased risk and mortality of cardiovascular diseases in women.26 Another matched cohort study published by Adelborg K in BMJ-BRIT MED J (IF 105.7) in 2018 ranked fourth in citation counts. In this Danish population-based epidemiological study, migraine was found to be associated with cardio- and cerebrovascular disease, particularly stroke (both ischemic and hemorrhagic stroke).21 The risk of cardio- and cerebrovascular disease was higher in migraine with aura and in women. The PREMIUM RCT published by Tobis JM in J AM COLL CARDIOL (IF 24.0) in 2017 evaluated the efficacy of PFO closure in the treatment of migraine attacks.27 Although there was a reduction in headache days, the responder rate was not statistically significant compared to the control group. Another RCT study published by Mattle HP in EUR HEART J (IF 39.3) also failed to find significant efficacy of the PFO closure.28 Three meta-analyses published in 2010, 2013, and 2018 revealed positive associations between migraine and ischemic stroke, hemorrhagic stroke, and overall stroke, respectively.20,29,30 A review by Kurth T published in LANCET NEUROL (IF 48.0) in 2012 summarized the complex relationship between migraine and stroke in terms of epidemiology, neuroimaging, clinical features, and potential mechanisms.31
 |
Table 1 The Top 10 Co-Cited References in Frequency |
 |
Figure 7 (A) The network of co-cited references. (B) The cluster map of co-cited references. (C) The timeline map of co-cited references. |
There were 7 references (Table 2) with centrality values >0.10, consisting of 1 animal experimental study, 1 prospective cohort study, 2 reviews, and 3 meta-analyses. 4 of them were from the top 10 co-cited references in frequency, including Sacco S (2013, centrality=0.21),30 Mahmoud AN (2018, centrality=0.17),20 Kurth T (2012, centrality=0.16),31 and Kurth T (2016, centrality=0.15).26 These 4 articles served as significant tipping points or bridges connecting different point groups in the network. A meta-analysis published by Bashir A in Neurology (IF 9.9) in 2013 investigated the association between migraine and structural changes in the brain.32 Structural lesions in the brain included infarct-like lesions, white matter abnormalities, and volumetric changes in gray and white matter regions. The results showed that the incidence of cerebral structural changes was higher in migraine patients, especially those with aura. This suggested a possible link between migraine headaches and cerebrovascular disease. Mawet J et al summarize the clinical evidence and potential mechanisms for the connection between migraine and stroke.33 Preclinical experiments found increased vulnerability to ischemic depolarization in familial hemiplegic type 1 migraine transgenic mice, which may be an important mechanism for the increased risk of stroke.34
 |
Table 2 The Top 7 Co-Cited References in Centrality |
The analysis of co-cited references highlighted the core literature in the field, which has been widely recognized in the past decade. Articles with high centrality play an important role in bridging between various studies. The analysis of highly cited papers can help researchers understand key research findings and academic trends in the field.
Analysis of Clusters and Timeline Maps of Co-Cited References
By using keywords extracted from the co-cited references, a cluster network map was generated. Q =0.60 > 0.3, S =0.84 >0.7, suggesting the clusters were well-structured and reliable. The clusters with a size of no less than 10 were shown in Figure 7B. Most clusters were related to underlying mechanisms, including atrial fibrillation (#0), endothelial function (#1), patent foramen ovale (#2, #4), spreading depression (#3), and genome-wide association (#6). Clusters #5 gender and #7 estrogen emphasized the importance of gender, especially females.
Timeline maps (Figure 7C) were used to further investigate the time distribution of the top 10 clusters. As shown, Cluster #1 endothelial function, and #3 spreading depression were at the earliest stage. Cluster #5 gender, #6 genome-wide association study, and #7 estrogen were in the middle stage. Cluster #4 patent foramen ovale spanned the earliest and middle stages, while Cluster #0 atrial fibrillation spanned the middle and latest stages. Cluster #2 right-to-left shunt was at the latest stage, reflecting current hot topics.
Cluster analysis brought together highly homogeneous literature. Larger clusters had a higher level of interest and research volume, reflecting research hotspots. Timeline displayed the duration of an active cluster, indicating a temporal evolution of the hotspot.
Analysis of Co-Occurring Keywords
Keywords are representative terms for the topic and content of a scientific article. High-frequency keywords represent hotspots in a particular field. The evolution of keywords reflects trends in research hotspots. After merging synonymous phrases and pruning the network (parameter selection: pathfinder, pruning the sliced and merged network), a keyword co-occurrence network map with 127 nodes and 161 links was generated (Figure 8A). A total of 127 keywords met the selection criteria, 10 of which appeared over 100 times. The top 20 keywords in frequency were displayed in Table 3, among which the most popular keywords were “ischemic stroke”, “migraine with aura”, “cortical spreading depolarization”, “risk” and “patent foramen ovale”. The top 3 keywords (Table 3) in centrality were “patent foramen ovale”, “association”, and “subarachnoid hemorrhage”. The keyword “association” (n=61, centrality=0.44) played an important bridging role between migraine and stroke.
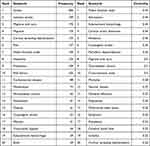 |
Table 3 The Top 20 Keywords in Frequency or Centrality |
Based on keyword analysis, the results were summarized as follows: Ischemic stroke (n=199, centrality=0.15) was the most popular stroke subtype, followed by cryptogenic stroke (n=52, centrality=0.36) and subarachnoid hemorrhage (n=39, centrality=0.44). Migraine with aura (n=170, centrality=0.30) was the most studied migraine subtype in this field. In terms of gender, more emphasis was placed on women (n=51, centrality=0.06). Patent foramen ovale (n=130, centrality=0.74) and cortical spreading depolarization (n=139, centrality=0.22) were the focus of research in the study of underlying mechanisms. Percutaneous closure and transcatheter closure further demonstrated the importance of patent foramen ovale, while peri-infarct depolarization highlighted the critical role of cortical spreading depolarization. These terms such as prevalence, mortality, cross-sectional studies, and meta-analysis evidenced the important role of epidemiology and evidence-based medicine in this area of research. Cardiovascular disease and risk factors with high frequencies were also hot topics of research in the field.
Keywords constituted an important part of the knowledge base. The keyword co-occurrence map visualized the keyword frequency size and the connection between them. High-frequency keywords were a direct reflection of research hotspots. Keywords with high centrality were key turning points between different topics and acted as bridges. By summary, we found that the hotspots of research focused on subtypes of the disease, research methods, potential mechanisms and risk factors.
Analysis of Keyword Clustering and Timeline
A keyword clustering network map was generated by using the LLR algorithm. Q=0.776>0.3, S=0.916>0.7, meeting a valid clustering. The clusters were shown in Figure 8B, including #0 risk factors, #1 subarachnoid hemorrhage, #2 acute ischemic stroke, #3 ischemic stroke, #4 cadasil, #5 childhood stroke, #6 cryptogenic stroke, #7 spreading depolarization, #8 neurological diseases, #9 patent foramen ovale, and #10 cortical spreading depression in descending order of size.
Timeline maps (Figure 8C) were established to further explore the temporal distribution of these clusters. Three clusters lasted the longest throughout the study, including #0 risk factors, #7 spreading depolarization, and #9 patent foramen ovale.
Larger clusters reflected the research hotspot. Timeline showed the temporal evolution of the clusters.
Analysis of Keywords with Citation Bursts
If a keyword is highly cited in a short period of time, it is the focus of attention for that time period. Burst detection enables the finding of burst words in different periods of time to explore hotspot trends. The top 12 keywords with the strongest citation bursts were shown in Figure 8D. The red line represented the duration of the keyword burst. The research hotspots were divided into three stages:
The early stage lasted from 2013 to 2014. Keywords with citation bursts included “intracerebral hemorrhage” and “atrial septal aneurysm”. The middle stage spanned from 2015 to 2018. “endothelial progenitor cells”, “epidemiology”, “oral contraceptive”, “burden”, “stroke mimic” and “united states” were the keywords of interest during this period. The latest stage covered the period from 2019 to 2023. There were 4 keywords with citation bursts, including “pathophysiology”, “outcm”, “mutation” and “small vessel disease”.
Keyword burst detection revealed research content with burst trends in different periods, reflecting the evolution of research hotspots. Current keywords with bursts reflect emerging research trends in the field, which can help researchers understand the research directions rapidly. Our results revealed a strongest current burst of pathophysiology, followed by small vessel disease.
Discussion
General Information
After removing irrelevant literature, we used CiteSpace to analyze 862 papers on the relationship between migraine and stroke over the past decade in different dimensions. In terms of publications, not many research papers were published during the decade, suggesting that the field was not a particularly hot research topic. However, many relevant articles published in high-quality journals attested to the high research value of the topic. Although the number was relatively stable annually, there was still a slow increase in the last five years compared to the first five years, indicating that the migraine-stroke association was receiving more and more attention from researchers. In terms of citations, 2015 peaked in both total citations and average citations, demonstrating the high level of acceptance of research findings in that year. This was supported by the fact that 8 of the 77 articles published in 2015 were cited more than 100 times.
The United States dominated this area, as it ranked first both in frequency and centrality. As the most prolific country, the United States was also the most active in cooperating with other countries. Countries from Europe played a significant role in this research since 8 of the top 10 countries in frequency were from Europe. Among them, Italy, Germany, and England contributed more and cooperated more with other countries, with higher frequency and centrality values. In Asia, China contributed the most articles, showing the importance Chinese researchers placed on the field. However, the centrality of China was less than 0.1, indicating insufficient cooperation with other countries, which needs to be improved in the future.
Two of the top three productive institutions were from the United States, which were Harvard University in first place and Massachusetts General Hospital in third place. Seven of the top ten productive institutions were from Europe, three from Germany, two from France, one from Netherlands, and one from Denmark. In terms of centrality, University of London came first, suggesting that it played an important role as a bridge in institutional collaboration. These developed countries and institutions have taken the lead in the development of this field. Developing countries and institutions are encouraged to place more importance on this research and strengthen more collaboration with the above countries and institutions.
In terms of individual contributions, Ayata Cenk, Terwindt Gisela M, and Ferrari Michel D were the top three productive authors, with 20 or more publications. KURTH T, SACCO S, and SILBERSTEIN SD were the most cited authors. In addition, KURTH T also had the highest centrality values. KURTH T and his research group were very interested in the relationship between migraine and cardio- and cerebrovascular diseases. They had been working on this area for many years and had published many high-quality articles that have been accepted by other researchers. Two of the most highly cited publications in the past decade were from KURTH T. Burst detection revealed that MAHMOUD AN, ADELBORG K, ALTAMURA C, and HU XM were recent high-impact authors. Our study visually analyzed the contributions and influence of researchers engaged in this field, providing a scientific assessment. Researchers can keep abreast of the progress of the field by learning about the important research findings of these influential researchers, or strengthen collaboration with these influential researchers to advance the field.
NEUROLOGY was in first place among co-cited journals with an impact factor of 9.9. The median impact factor of the top 10 journals in frequency was 12.9, which implied that studies from high-quality journals had a greater impact on the development of this area. The fact that relevant research was published in high-quality journals also indicated the importance that high-quality journals place on the field. Our research help researchers to rapidly identify key journals and find important research results. Researchers can also publish their important findings in these key journals of interest to the field, promoting academic dissemination and disciplinary development.
The dual-map overlay of journals revealed that the migraine-stroke association was mainly focused on areas such as Molecular/Biology/Immunology, Medicine/Medical/Clinical, and Neurology/Sports/Ophthalmology, which were primarily influenced by areas such as Molecular/ Biology/Genetics, Health/Nursing/Medicines, and Psychology/Education/Society.
Research Hotspots in the Knowledge Base of Migraine-Stroke Association
Numerous terms from the reference co-citation network and the keyword co-occurrence network constituted a knowledge base for the migraine-stroke association field. The analysis of frequency, centrality, and clustering, combined with the context of knowledge, could help to explore the hot spots of research in the field. Our study revealed hotspots focusing on the following areas: (1) subtypes of related diseases; (2) research methods (3) potential mechanisms (4) risk factors. In migraine, MA was the key subtype. In stroke, ischemic stroke was the key subtype, followed by cryptogenic stroke and subarachnoid hemorrhage. In terms of research methods, meta-analysis and cross-sectional studies were hotspots, with the former having a high frequency and the latter having a high degree of centrality. In terms of mechanisms, cortical spreading depolarization and patent foramen ovale were focal points, both of which have high frequency and centrality. Traditional vascular factors have also been widely explored because of their close association with stroke.
Migraine with Aura and Ischemic Stroke
Epidemiologic studies and meta-analysis suggest an association between migraine and stroke.13 Migraineurs have a 40% increased risk of stroke compared to non-migraineurs.20 MA and ischemic stroke are the focus of the study with the strongest associations.29,35,36 In our study, MA was the most studied subtype of migraine (highest frequency), while ischemic stroke was the most studied subtype of stroke (highest frequency). In addition, both have high betweenness centrality values, suggesting that both play a bridging role in this area of research. Migraine’s impact on ischemic stroke risk is primarily found in young adults and women.2,37–39 In our study, the keyword “women” has the highest frequency and centrality among the genders, suggesting that women are the focus of research in this area. Smoking and oral contraceptives further increase the risk of stroke.40 Unfortunately, our study did not represent the young population. However, the keyword “age” had a high centrality (0.19, not shown in Table 3), suggesting age is also a key point. A recent multicenter cohort study showed that among all 851 patients with migrainous cerebral infarction, MA patients were more frequently women and younger in age.41 It was also shown that for young men, migraine increased the risk of ischemic stroke similarly to that of women.42 The risk of stroke in elderly migraineurs has also been explored, with conflicting results. Migraine increased the risk of stroke in some studies,39,43 while others failed to find a significant association.44–46 A recent prospective study suggested an elevated hazard ratio between migraine and overall stroke or ischemic stroke in middle-aged and elderly populations, however, it was not statistically significant.47
Migraine is associated with an increased risk of cryptogenic ischemic stroke.36,48 In particular, there is a strong correlation between MA and cryptogenic ischemic stroke in young patients.49 Some studies showed that migraine increased the risk of hemorrhagic stroke (subarachnoid hemorrhage and intracranial hemorrhage),20,21,30,50 However, there was still controversy.50,51 A recent meta-analysis involving 1,757,589 subjects showed an association between hemorrhagic stroke and migraine, especially migraine with aura.52
Risk Factors and Cardiovascular Disease
Some studies showed that conventional vascular risk factors did not contribute positively to the increased risk of ischemic stroke in migraines.53,54 There appears to be a negative correlation between diabetes and migraine.53 Stroke patients with MA are also less likely to have hypertension, diabetes, and dyslipidemia, which implies that migraine-induced risk of stroke is independent.41,55,56 However, dyslipidemia and smoking increase the Framingham risk score in migraineurs.53 Notably, there are two conditions in which traditional vascular risk factors still play an important role in stroke attacks, one in patients with CADASIL and the other in pregnant patients with migraine headaches. Smoking and diabetes are associated with earlier stroke in CADASIL,57,58 while hypertension increases the risk of stroke and cognitive decline in CADASIL.59,60 Risk factors such as high blood pressure, diabetes, and smoking are more prevalent in pregnant women with migraines, increasing the risk of ischemic stroke.61 In addition, migraine is associated with cardiovascular diseases (such as myocardial infarction and atrial fibrillation),21,62,63 and can also increase cardiovascular mortality.26,64 In particular, MA further increases the risk of myocardial infarction and cardiovascular mortality.52
Meta-Analysis and Cross-Sectional Study
Epidemiology and evidence-based medicine have played a key role in studying the relationship between migraine and stroke. Cross-sectional studies provide clues to explore the relationship and potential etiology between migraine and stroke by the distribution of the diseases. Case-control studies, prospective or retrospective cohort studies, and high-quality meta-analyses are more targeted to investigate the association between a factor and disease. A recent cross-sectional study showed that right-to-left shunt exacerbates photosensitivity in migraine patients and that the two are independently associated.65 Another cross-sectional study revealed a positive association between migraine and hypertension (Odds Ratio (OR) 1.25, 95% confidence intervals 1.03–1.53).66 In both recent meta-analyses, migraine has been shown to be associated with an increased risk of ischemic stroke. However, the two have reached different conclusions about the relationship between migraine and hemorrhagic stroke. This uncertainty may be related to factors such as different populations or migraine subtypes.13,52
Potential Mechanisms
Various potential mechanisms have been widely explored, including cortical spreading depolarization, patent foramen ovale (right-to-left shunt, paradoxical embolism), genetic susceptibility, endothelial dysfunction, vascular reactivity, atrial fibrillation, carotid artery dissection, and hormonal contraceptives.54,67,68 Among them, cortical spreading depolarization and patent foramen ovale are the focus of mechanism studies. Most studies suggest that the increased risk of stroke from migraine is independent of large vessel atherosclerosis and traditional vascular risk factors.37,41,55,69 A recent Mendelian randomization (MR) study found a link between genetic susceptibility to migraine and worse functional outcomes after ischemic stroke.70 However, more MR studies failed to find a causal relationship between genetic susceptibility to migraine and stroke.71–73
Patent Foramen Ovale
The foramen ovale is a vital pathway necessary for embryonic development and gradually closes to form a permanent atrial septum in most individuals postnatally. If complete closure is not achieved over 3 years old, the remaining channel is termed patent foramen ovale (PFO). Studies have found that the prevalence of PFO is 30% at ages (1–29), 25% at ages (30–79), and 20.2% at ages >80 years.74 Overall, the incidence of PFOs in adults is approximately 25%.75 Patent foramen ovale may be a common risk factor for migraine, stroke, and other arterial occlusions,76,77 while migraine and stroke are the neurological disorders most strongly associated with PFOs.
Although there is still no high-quality evidence to support a causal relationship between PFO and migraine, several studies have shown a bidirectional association between them.78 Individuals with MA have a higher prevalence of PFO (approximately 46.3% - 88.0%), whereas migraineurs without aura have a similar prevalence as the general population (approximately 16.2% - 34.9%).79 A systematic review of 5,572 subjects showed that the incidence of PFO in patients with migraine and MA was 3.36 and 2.46 times higher than that in the general population, respectively, whereas there was no difference between patients with MO and the general population.80 A multicenter case-control study of the Chinese population in 2018 showed that the incidence of RLS in the MA and MO groups was 63.8% and 39.9%, respectively, which was higher than that in the control group (29.4%).81
PFO is an emerging risk factor for stroke, especially in young adults. The results of meta-analysis showed a higher incidence of PFO in stroke patients compared to healthy individuals (OR 3.1).82 Approximately 5% of total strokes and 10% of strokes in young and middle-aged adults may be attributed to patent foramen ovale.83 PFO is strongly associated with cryptogenic stroke, with an incidence of 69%.84 Recent RCTs, such as RESPECT,85 CLOSE,86 REDUCE,87 and DEFENSE,88 have demonstrated the positive effect of PFO closure in preventing stroke recurrence. These studies have contributed to the definition of the concept of “PFO-associated stroke” and the refinement of strategies for secondary stroke prevention.83,89
The incidence of PFO in cryptogenic stroke with MA and cryptogenic stroke with frequent MA is 79% and 93%, respectively.84 In the MA population, PFO appears to be the most common source of embolism.90,91 The reversible ischemic hemidiaphragm is also smaller in migraine patients with aura.92 All these suggest that PFO may be a common risk factor and a bridge connecting MA and stroke.
The underlying mechanisms of PFO susceptibility to stroke are primarily relevant to RLS and in-situ thrombus. RLS allows paradoxical thrombus, vasoactive substances, and deoxygenated venous blood to bypass filtration in the pulmonary circulation and enter the systemic circulation, triggering a variety of pathological changes. Microemboli such as small particles and air bubbles in the venous circulation can induce cortical spreading depolarization, causing migraine attacks or strokes. The size, location, and obstruction duration of the embolus determine the severity of its consequences.93 Juxtacortical FLAIR hyperintensities are more commonly found in migraineurs with PFO on neuroimaging.94,95 A recent small single-center cross-sectional study showed that the incidence of in situ thrombus within the PFO was 83.7% in the stroke group, 57.1% in the migraine group, and 0% in the asymptomatic group, suggesting that in situ thrombus plays an important role in the pathogenesis of PFO-associated stroke and migraine.96
Cortical Spreading Depolarization (CSD)
Cortical spreading depolarization, previously also known as cortical spreading depression, is a slow-propagating diffuse depolarizing wave (2 −5 mm/min) that occurs in neurons and neuroglia for about 1 minute, followed by several minutes of suppression of EEG activity.97,98 It was shown to be initiated by spontaneous glutamatergic plumes.99 As one of the important pathological mechanisms of early central nervous system injury, spreading depolarization can induce MA.100,101 During MA, blood flow was observed to evolve from transient hyperperfusion to prolonged hypoperfusion in brain regions associated with aura symptoms.102
Besides MA, the spreading-depolarization continuum can occur in a variety of acute cerebral injury situations including stroke and traumatic brain injury.34,103,104 In patients with traumatic brain injury, CSD was recorded by cortical electroencephalography, independently associated with poor neurological prognosis.105 CSD is a common mechanism between MA and stroke.106 In a mouse model of familial hemiplegic type 1 migraine mutation, susceptibility to peri-infarct depolarization was increased during stroke.34 Migraine patients more susceptible to CSD seemed to be more susceptible to stroke.64 Animal studies have shown that CSD may cause cerebral ischemia. In rat models, CSD combined with endothelin-1 (a cerebral vasoconstrictor factor) caused selective neuronal necrosis in a micro area, suggesting that CSD can induce cerebral ischemic injury in the presence of vasospasm.107 Microembolism (including air microemboli and particulate) was a triggering factor for CSD and was found to reduce cerebral blood flow.108 Brief microembolism could trigger CSD and MA attacks, while long-lasting stable microemboli could cause cerebral infarction.109
Our study revealed research hotspots through bibliometric analysis and elaborated in detail. Researchers can rapidly identify academic topics, key issues, and research progress, and further conduct more in-depth studies. In addition, our findings help clinicians to further realize the importance of subtypes. More standardized diagnosis of subtypes in clinical practice can greatly improve the accuracy of clinical data and the quality of epidemiological studies.
Emerging Research Frontiers and Trends
Keyword burst detection highlights terms that have been highly cited in a given time period. Keywords that have been strongly cited currently represent emerging research hotspots and trends in the field. More attention has been paid to “pathophysiology”, “outcm”, “mutation” and “small vessel disease” in recent years. Pathophysiology and small vessel disease are still in a strong citation burst at the moment, representing an emerging research trend.
Pathophysiology
Pathophysiology is the bridge between basic and clinical medicine. The research on the etiology, pathogenesis, and functional changes of migraine can provide theoretical support for the prevention and treatment of migraine and an in-depth exploration of migraine-stroke association. No identified pathophysiological mechanism has yet been found for the association between migraine and stroke, however, researchers have still explored extensively.
Neuroimaging studies showed the involvement of CSD-like phenomena in the pathophysiology of the MA cascade.110 Liesl N Close et al elaborated on the connections between calcitonin gene-related peptides (CGRP) and cortical spreading depression, proposing a pathophysiological hypothesis that CGRP activity is induced by cortical spreading depression in migraine.111 CGRP antagonists may block the protective effects of CGRP in response to severe vasospasm.112 Flow-mediated dilation (FMD) technical measurements showed that migraineurs had higher ratios of FMD, suggesting that endothelial dysfunction may be one of the underlying mechanisms of migraine attacks.113 In plateau residents, 71% of PFO patients showed ischemic lesions on cranial MRI, a much higher occurrence than that in healthy controls (19%).114 The diameter of PFOs was correlated with the incidence and number but not the location of cerebral ischemic lesions. Single and multiple cerebral ischemic lesions were observed in patients with PFO diameters of less than 2 mm and more than 4 mm, respectively.114 Nevertheless, in a retrospective case-control study, researchers failed to find a higher incidence of high-risk PFOs in the Stoke + MA group, arguing that they were not the primary contributors to the increased risk of MA stroke.56
In addition, researchers have explored several pathophysiological features of late-life migraine,115 pediatric migraine,116 and obstetrics and gynecology migraine.117 Research on the causes of migraine chronicity and the association of migraine with myocardial infarction,52 brain white matter lesions,118 and dementia may also help researchers gain a deeper understanding of the pathophysiological mechanisms underlying migraine.119–121
Small Vessel Disease and CADASIL
Evidence has shown a negative correlation between migraine with aura and small vessel disease (SVD).55 However, there are different types of SVDs. A rare inherited SVD, cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL), is strongly associated with migraine and ischemic stroke. Most of the burst of SVD in recent years is attributable to CADASIL studies. CADASIL is originated by Notch3 mutations. Mutant NOTCH3 proteins accumulate in the extracellular regions and granular osmiophilic materials (GOM) deposit around vascular smooth muscle cells, leading to the thickening of small vessel walls and degeneration of smooth muscle cells. The typical clinical characteristics of CADASIL include MA, recurrent subcortical ischemic events (transient ischemic attacks and strokes), and cognitive deficits with eventual progression to vascular dementia.60 Although CADASIL is a rare disorder, it has received attention due to its significant reduction in life expectancy.122 Only one in five elderly CADASIL patients (>65 years) still remain neurologically intact.123
CADASIL phenotypes vary widely in different populations, affected by genetics and other factors (eg, diabetes mellitus).58 A study demonstrated differences in CADASIL between Asian and Caucasian populations by analyzing genetic spectrum and clinical data. Asians were found to be most commonly affected by the R544C and R607C mutations, with clinical manifestations more prone to cerebral ischemic events and cognitive impairment. Caucasians were most commonly affected by the R1006C and R141C mutations, with clinical manifestations of migraine and psychiatric disorders.124 R169C and R182C are the most common mutations in Greek CADASIL patients, with clinical symptoms similar to those of the Caucasian population.125
In terms of mechanisms, it was found that the brains of CADASIL patients were poorly tolerant to ischemia and hypoxia.126 This was supported by animal experiments in which mice with Notch3 mutations had increased susceptibility to ischemic injury and larger post-stroke infarcts.127 Impaired neurovascular interactions were demonstrated in an in vitro model of CADASIL induced pluripotent stem cell (IPSC), which reduced blood-brain barrier function.128 Evidence suggested that cerebral blood flow (CBF) in CADASIL patients declined by 6% within two years, a significantly greater decline than in the healthy population (0.45%).129 Cerebral hemodynamic dysfunction and poor hemodynamic reserve predispose to multiple acute subcortical infarcts.126 Similarly, coronary microvascular dysfunction and attenuated coronary flow reserve were also found in young and mildly symptomatic patients with CADASIL.130 Severe periventricular and deep white matter lesions were associated with dementia in a study of CADASIL patients from Japan.131
Our study indicates that pathophysiology and CADASIL are current emerging hot research directions. Research advances during the burst period were elaborated, which will help researchers follow the latest research trends and better plan their future research. Pathophysiology had a higher strength, suggesting more attention to it. More pathophysiologic studies are needed in the future to further explore the migraine-stroke association.
Limitations
Some limitations should be noted. Firstly, the data source is relatively homogenous. We searched only literature from the WOSCC database and may have missed some studies from other databases. Secondly, only articles from the last decade were included, resulting in a small sample size. Thirdly, non-English studies were excluded. Fourthly, CiteSpace software could not recognize first authors, corresponding authors, and other authors in the author collaboration network, which biases the evaluation of individual contributions to the field. Fifthly, due to the time required to publish and cite literature, there may be a time delay, leading to the possibility that the latest findings and developments may not yet be reflected in the analysis. Finally, the analysis of literature is primarily based on the citation relationships. Some high-quality studies may not be widely cited for a variety of reasons, resulting in an underestimation of their academic value.
Conclusion
In this study, we visually analyzed the literature on the migraine-stroke relation over the past decade. Annual publications grew slowly. The United States and European countries dominated research in this area. Harvard University was the most productive institution, while the University of London was most active with other institutions. Ayata Cenk contributed the most articles, while KURTH T and NEUROLOGY were co-cited most. Research hotspots included migraine with aura, ischemic stroke, patent foramen ovale, cortical spreading depolarization, meta-analysis, cross-sectional study, and risk factors. Pathophysiology and small vessel disease represented research frontiers and emerging trends.
Our study scientifically outlines the migraine-stroke association over the past decade, presenting useful information. Nevertheless, the association between migraine and stroke is complex and the underlying mechanisms are unclear. This is supported by inconsistencies in epidemiologic data and genetic evidence. There are many challenges to studying this association, such as misdiagnosis, selection bias, limitations of the genetic database, insufficient attention from clinicians, and lack of characteristic imaging and biomarkers. More attention has been paid to the study of pathophysiology. More high-quality studies are needed in the future to explore the pathogenesis of migraine and its association with stroke.
Abbreviations
CADASIL, cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy; CBF, cerebral blood flow; CGRP, calcitonin gene-related peptides; CSD, Cortical spreading depolarization; FMD, flow-mediated dilation; GOM, granular osmiophilic materials; ICHD-3, the 3rd edition of International Classification of Headache Disorders; IF, impact factor; IPSC, induced pluripotent stem cell; MA, migraine with aura; MO, migraine without aura; MR, Mendelian randomization; OR, Odds Ratio; PFO, patent foramen ovale; RCT, randomized controlled trial; RLS, right-to-left shunt; SVD, small vessel disease; WOSCC, Web of Science Core Collection.
Acknowledgments
Thanks to Chaomei Chen for inventing CiteSpace.
Funding
This work was supported by the Hospital level project of Shanghai Sixth People’s Hospital (ynlc201827), Natural Science Foundation of Shandong Province (ZR2020MH156), and Shaanxi Key Laboratory of Research on TCM Physical Constitution and Diseases Prevention and Treatment (KF202310).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Steiner TJ, Stovner LJ, Jensen R, Uluduz D, Katsarava Z. Migraine remains second among the world’s causes of disability, and first among young women: findings from GBD2019. J Headache Pain. 2020;21(1):137. doi:10.1186/s10194-020-01208-0
2. Stovner LJ, Nichols E, Steiner TJ. Global, regional, and national burden of migraine and tension-type headache, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17(11):954–976. doi:10.1016/s1474-4422(18)30322-3
3. Tietjen GE, Maly EF. Migraine and Ischemic Stroke in Women. A Narrative Review. Headache. 2020;60(5):843–863. doi:10.1111/head.13796
4. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders. Cephalalgia. 2018;38(1):1–211. doi:10.1177/0333102417738202
5. Charles A. The pathophysiology of migraine: implications for clinical management. Lancet Neurol. 2018;17(2):174–182. doi:10.1016/s1474-4422(17)30435-0
6. Bonkhoff AK, Schirmer MD, Bretzner M, et al. Outcome after acute ischemic stroke is linked to sex-specific lesion patterns. Nat Commun. 2021;12(1):3289. doi:10.1038/s41467-021-23492-3
7. Hankey GJ. Stroke. Lancet. 2017;389(10069):641–654. doi:10.1016/s0140-6736(16)30962-x
8. Tsao CW, Aday AW, Almarzooq ZI, et al. Heart Disease and Stroke Statistics-2023 Update: a Report From the American Heart Association. Circulation. 2023;147(8):e93–e621. doi:10.1161/cir.0000000000001123
9. Campbell BCV, Khatri P. Stroke. Lancet. 2020;396(10244):129–142. doi:10.1016/s0140-6736(20)31179-x
10. Ashina M, Katsarava Z, Do TP, et al. Migraine: epidemiology and systems of care. Lancet. 2021;397(10283):1485–1495. doi:10.1016/s0140-6736(20)32160-7
11. Feigin VL, Stark BA, Johnson CO. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021;20(10):795–820. doi:10.1016/s1474-4422(21)00252-0
12. Øie LR, Kurth T, Gulati S, Dodick DW. Migraine and risk of stroke. J Neurol Neurosurg Psychiatry. 2020;91(6):593–604. doi:10.1136/jnnp-2018-318254
13. Zhang S, Liu H, Shi T. Association between migraine and risk of stroke: a systematic review and meta-analysis. Neurol Sci. 2022;43(8):4875–4889. doi:10.1007/s10072-022-06074-z
14. Chen C. Searching for intellectual turning points: progressive knowledge domain visualization. Proc Natl Acad Sci U S A. 2004;1(Suppl 1):5303–5310. doi:10.1073/pnas.0307513100
15. Chen CM, CiteSpace II. Detecting and visualizing emerging trends and transient patterns in scientific literature. J Am Soc Inf Sci Technol. 2006;57(3):359–377. doi:10.1002/asi.20317
16. Zhao Y, Huang L, Liu M, Gao H, Li W. Scientific Knowledge Graph of Acupuncture for Migraine: a Bibliometric Analysis from 2000 to 2019. J Pain Res. 2021;14:1985–2000. doi:10.2147/jpr.S314174
17. Zhao T, Guo J, Song Y, et al. A Bibliometric Analysis of Research Trends of Acupuncture Therapy in the Treatment of Migraine from 2000 to 2020. J Pain Res. 2021;14:1399–1414. doi:10.2147/jpr.S306594
18. Song X, Wang J, Bai L, Zou W. Bibliometric Analysis of 100 Most Highly Cited Publications on Acupuncture for Migraine. J Pain Res. 2023;16:725–747. doi:10.2147/jpr.S396909
19. Sabé M, Sulstarova A, Chen C, et al. A century of research on neuromodulation interventions: a scientometric analysis of trends and knowledge maps. Neurosci Biobehav Rev. 2023;152:105300. doi:10.1016/j.neubiorev.2023.105300
20. Mahmoud AN, Mentias A, Elgendy AY, et al. Migraine and the risk of cardiovascular and cerebrovascular events: a meta-analysis of 16 cohort studies including 1 152 407 subjects. BMJ Open. 2018;8(3):e020498. doi:10.1136/bmjopen-2017-020498
21. Adelborg K, Szépligeti SK, Holland-Bill L, et al. Migraine and risk of cardiovascular diseases: Danish population based matched cohort study. BMJ. 2018;360:k96. doi:10.1136/bmj.k96
22. Hu X, Zhou Y, Zhao H, Peng C. Migraine and the risk of stroke: an updated meta-analysis of prospective cohort studies. Neurol Sci. 2017;38(1):33–40. doi:10.1007/s10072-016-2746-z
23. Altamura C, Paolucci M, Brunelli N, et al. Right-to-left shunts and hormonal therapy influence cerebral vasomotor reactivity in patients with migraine with aura. PLoS One. 2019;14(8):e0220637. doi:10.1371/journal.pone.0220637
24. Altamura C, Viticchi G, Fallacara A, et al. Erenumab does not alter cerebral hemodynamics and endothelial function in migraine without aura. Cephalalgia. 2021;41(1):90–98. doi:10.1177/0333102420956692
25. Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia. 2013;33(9):629–808. doi:10.1177/0333102413485658
26. Kurth T, Winter AC, Eliassen AH, et al. Migraine and risk of cardiovascular disease in women: prospective cohort study. BMJ. 2016;353:i2610. doi:10.1136/bmj.i2610
27. Tobis JM, Charles A, Silberstein SD, et al. Percutaneous Closure of Patent Foramen Ovale in Patients With Migraine: the PREMIUM Trial. J Am Coll Cardiol. 2017;70(22):2766–2774. doi:10.1016/j.jacc.2017.09.1105
28. Mattle HP, Evers S, Hildick-Smith D, et al. Percutaneous closure of patent foramen ovale in migraine with aura, a randomized controlled trial. Eur Heart J. 2016;37(26):2029–2036. doi:10.1093/eurheartj/ehw027
29. Spector JT, Kahn SR, Jones MR, Jayakumar M, Dalal D, Nazarian S. Migraine headache and ischemic stroke risk: an updated meta-analysis. Am J Med. 2010;123(7):612–624. doi:10.1016/j.amjmed.2009.12.021
30. Sacco S, Ornello R, Ripa P, Pistoia F, Carolei A. Migraine and hemorrhagic stroke: a meta-analysis. Stroke. 2013;44(11):3032–3038. doi:10.1161/strokeaha.113.002465
31. Kurth T, Chabriat H, Bousser MG. Migraine and stroke: a complex association with clinical implications. Lancet Neurol. 2012;11(1):92–100. doi:10.1016/s1474-4422(11)70266-6
32. Bashir A, Lipton RB, Ashina S, Ashina M. Migraine and structural changes in the brain: a systematic review and meta-analysis. Neurology. 2013;81(14):1260–1268. doi:10.1212/WNL.0b013e3182a6cb32
33. Mawet J, Kurth T, Ayata C. Migraine and stroke: in search of shared mechanisms. Cephalalgia. 2015;35(2):165–181. doi:10.1177/0333102414550106
34. Eikermann-Haerter K, Lee JH, Yuzawa I, et al. Migraine mutations increase stroke vulnerability by facilitating ischemic depolarizations. Circulation. 2012;125(2):335–345. doi:10.1161/circulationaha.111.045096
35. Sacco S, Kurth T. Migraine and the risk for stroke and cardiovascular disease. Curr Cardiol Rep. 2014;16(9):524. doi:10.1007/s11886-014-0524-1
36. Li L, Schulz UG, Kuker W, Rothwell PM. Age-specific association of migraine with cryptogenic TIA and stroke: population-based study. Neurology. 2015;85(17):1444–1451. doi:10.1212/wnl.0000000000002059
37. Linstra KM, van Os HJA, Ruigrok YM, et al. Sex Differences in Risk Profile, Stroke Cause and Outcome in Ischemic Stroke Patients With and Without Migraine. Front Neurosci. 2021;15:740639. doi:10.3389/fnins.2021.740639
38. Peng KP, Chen YT, Fuh JL, Tang CH, Wang SJ. Migraine and incidence of ischemic stroke: a nationwide population-based study. Cephalalgia. 2017;37(4):327–335. doi:10.1177/0333102416642602
39. Lee SY, Lim JS, Oh DJ, Kong IG, Choi HG. Risk of ischaemic stroke in patients with migraine: a longitudinal follow-up study using a national sample cohort in South Korea. BMJ Open. 2019;9(4):e027701. doi:10.1136/bmjopen-2018-027701
40. Chiang MC, Dumitrascu OM, Chhabra N, Chiang CC. Migraine with Visual aura and the Risk of Stroke- a Narrative Review. J Stroke Cerebrovasc Dis. 2021;30(11):106067. doi:10.1016/j.jstrokecerebrovasdis.2021.106067
41. Altamura C, Viticchi G, Rizzo AC, et al. Stroke territory and atherosclerosis in ischemic stroke patients with a history of migraine with aura. Front Neurol. 2023;14:1142424. doi:10.3389/fneur.2023.1142424
42. Hvitfeldt Fuglsang C, Pedersen L, Schmidt M, Vandenbroucke JP, Bøtker HE, Sørensen HT. Migraine and risk of premature myocardial infarction and stroke among men and women: a Danish population-based cohort study. PLoS Med. 2023;20(6):e1004238. doi:10.1371/journal.pmed.1004238
43. McKinley EC, Lay CL, Rosenson RS, et al. Risk for ischemic stroke and coronary heart disease associated with migraine and migraine medication among older adults. J Headache Pain. 2021;22(1):124. doi:10.1186/s10194-021-01338-z
44. Androulakis XM, Sen S, Kodumuri N, et al. Migraine Age of Onset and Association With Ischemic Stroke in Late Life: 20 Years Follow-Up in ARIC. Headache. 2019;59(4):556–566. doi:10.1111/head.13468
45. Norton J, Portet F, Gabelle A, et al. Are migraine and non-migrainous headache risk factors for stroke in the elderly? Findings from a 12-year cohort follow-up. Eur J Neurol. 2016;23(9):1463–1470. doi:10.1111/ene.13060
46. Monteith TS, Gardener H, Rundek T, Elkind MS, Sacco RL. Migraine and risk of stroke in older adults: northern Manhattan Study. Neurology. 2015;85(8):715–721. doi:10.1212/wnl.0000000000001854
47. Acarsoy C, Fani L, Al-Hassany L, et al. Migraine and the risk of stroke in a middle-aged and elderly population: a prospective cohort study. Cephalalgia. 2023;43(1):3331024221132008. doi:10.1177/03331024221132008
48. Mazzoleni V, Grassi M, Lodigiani C, et al. Migraine and Cryptogenic Ischemic Stroke. Ann Neurol. 2021;89(3):627–629. doi:10.1002/ana.25996
49. Martinez-Majander N, Artto V, Ylikotila P, et al. Association between Migraine and Cryptogenic Ischemic Stroke in Young Adults. Ann Neurol. 2021;89(2):242–253. doi:10.1002/ana.25937
50. Albieri V, Olsen TS, Andersen KK. Risk of Stroke in Migraineurs Using Triptans. Associations with Age, Sex, Stroke Severity and Subtype. EBioMedicine. 2016;6:199–205. doi:10.1016/j.ebiom.2016.02.039
51. Gaist D, González-Pérez A, Ashina M, Rodríguez LA. Migraine and risk of hemorrhagic stroke: a study based on data from general practice. J Headache Pain. 2014;15(1):74. doi:10.1186/1129-2377-15-74
52. CYH N, Tan BYQ, Teo YN, et al. Myocardial infarction, stroke and cardiovascular mortality among migraine patients: a systematic review and meta-analysis. J Neurol. 2022;269(5):2346–2358. doi:10.1007/s00415-021-10930-x
53. Sacco S, Pistoia F, Degan D, Carolei A. Conventional vascular risk factors: their role in the association between migraine and cardiovascular diseases. Cephalalgia. 2015;35(2):146–164. doi:10.1177/0333102414559551
54. Ornello R, Frattale I, Caponnetto V, Pistoia F, Sacco S. Cerebral vascular reactivity and the migraine-stroke relationship: a narrative review. J Neurol Sci. 2020;414:116887. doi:10.1016/j.jns.2020.116887
55. Gollion C, Gazagnes J, Fabry V, Barbieux-Guillot M, Lerebours F, Larrue V. Atrial fibrillation and migraine with aura in young adults with ischemic stroke. Cephalalgia. 2021;41(3):375–382. doi:10.1177/0333102420970880
56. Altamura C, Cascio Rizzo A, Viticchi G, et al. Shorter visual aura characterizes young and middle-aged stroke patients with migraine with aura. J Neurol. 2022;269(2):897–906. doi:10.1007/s00415-021-10671-x
57. Adib-Samii P, Brice G, Martin RJ, Markus HS. Clinical spectrum of CADASIL and the effect of cardiovascular risk factors on phenotype: study in 200 consecutively recruited individuals. Stroke. 2010;41(4):630–634. doi:10.1161/strokeaha.109.568402
58. Ospina C, Arboleda-Velasquez JF, Aguirre-Acevedo DC, et al. Genetic and nongenetic factors associated with CADASIL: a retrospective cohort study. J Neurol Sci. 2020;419:117178. doi:10.1016/j.jns.2020.117178
59. Ciolli L, Pescini F, Salvadori E, et al. Influence of vascular risk factors and neuropsychological profile on functional performances in CADASIL: results from the MIcrovascular LEukoencephalopathy Study (MILES). Eur J Neurol. 2014;21(1):65–71. doi:10.1111/ene.12241
60. Locatelli M, Padovani A, Pezzini A. Pathophysiological Mechanisms and Potential Therapeutic Targets in Cerebral Autosomal Dominant Arteriopathy With Subcortical Infarcts and Leukoencephalopathy (CADASIL). Front Pharmacol. 2020;11:321. doi:10.3389/fphar.2020.00321
61. Bushnell CD, Jamison M, James AH. Migraines during pregnancy linked to stroke and vascular diseases: US population based case-control study. BMJ. 2009;338:b664. doi:10.1136/bmj.b664
62. Sacco S, Ornello R, Ripa P, et al. Migraine and risk of ischaemic heart disease: a systematic review and meta-analysis of observational studies. Eur J Neurol. 2015;22(6):1001–1011. doi:10.1111/ene.12701
63. Sen S, Androulakis XM, Duda V, et al. Migraine with visual aura is a risk factor for incident atrial fibrillation: a cohort study. Neurology. 2018;91(24):e2202–e2210. doi:10.1212/wnl.0000000000006650
64. Kurth T, Rist PM, Ridker PM, Kotler G, Bubes V, Buring JE. Association of Migraine With Aura and Other Risk Factors With Incident Cardiovascular Disease in Women. JAMA. 2020;323(22):2281–2289. doi:10.1001/jama.2020.7172
65. Dong B, Ji S, Li Y, et al. Connection between right-to-left shunt and photosensitivity: a community-based cross-sectional study. Front Neurol. 2023;14:1177879. doi:10.3389/fneur.2023.1177879
66. Zhang J, Mao Y, Li Y, et al. Association between migraine or severe headache and hypertension among US adults: a cross-sectional study. Nutr, Metab Cardiovasc Dis. 2023;33(2):350–358. doi:10.1016/j.numecd.2022.11.014
67. Paolucci M, Altamura C, Vernieri F. The Role of Endothelial Dysfunction in the Pathophysiology and Cerebrovascular Effects of Migraine: a Narrative Review. J Clin Neurol. 2021;17(2):164–175. doi:10.3988/jcn.2021.17.2.164
68. Sacco S, Harriott AM, Ayata C, et al. Microembolism and Other Links Between Migraine and Stroke: clinical and Pathophysiologic Update. Neurology. 2023;100(15):716–726. doi:10.1212/wnl.0000000000201699
69. Gollion C, Guidolin B, Lerebours F, Rousseau V, Barbieux-Guillot M, Larrue V. Migraine and large artery atherosclerosis in young adults with ischemic stroke. Headache. 2022;62(2):191–197. doi:10.1111/head.14265
70. Wang M, Daghlas I, Zhang Z, Ye D, Li S, Liu D. Genetic liability to migraine and functional outcome after ischemic stroke. Eur Stroke J. 2023;8(2):517–521. doi:10.1177/23969873231164728
71. Lee KJ, Lee SJ, Bae HJ, Sung J. Exploring the causal inference of migraine on stroke: a Mendelian randomization study. Eur J Neurol. 2022;29(1):335–338. doi:10.1111/ene.15101
72. Shu MJ, Li JR, Zhu YC, Shen H. Migraine and Ischemic Stroke: a Mendelian Randomization Study. Neurol Ther. 2022;11(1):237–246. doi:10.1007/s40120-021-00310-y
73. Daghals I, Sargurupremraj M, Danning R, et al. Migraine, Stroke, and Cervical Arterial Dissection: shared Genetics for a Triad of Brain Disorders With Vascular Involvement. Neurol Genet. 2022;8(1):e653. doi:10.1212/nxg.0000000000000653
74. McKenzie JA, Edwards WD, Hagler DJ. Anatomy of the patent foramen ovale for the interventionalist. Catheter Cardiovasc Interv. 2009;73(6):821–826. doi:10.1002/ccd.21889
75. Homma S, Messé SR, Rundek T, et al. Patent foramen ovale. Nat Rev Dis Primers. 2016;2:15086. doi:10.1038/nrdp.2015.86
76. Mojadidi MK, Zaman MO, Elgendy IY, et al. Cryptogenic Stroke and Patent Foramen Ovale. J Am Coll Cardiol. 2018;71(9):1035–1043. doi:10.1016/j.jacc.2017.12.059
77. Pristipino C, Sievert H, D’Ascenzo F, et al. European position paper on the management of patients with patent foramen ovale. General approach and left circulation thromboembolism. Eur Heart J. 2019;40(38):3182–3195. doi:10.1093/eurheartj/ehy649
78. Schwedt TJ, Demaerschalk BM, Dodick DW. Patent foramen ovale and migraine: a quantitative systematic review. Cephalalgia. 2008;28(5):531–540. doi:10.1111/j.1468-2982.2008.01554.x
79. Liu K, Wang BZ, Hao Y, Song S, Pan M. The Correlation Between Migraine and Patent Foramen Ovale. Front Neurol. 2020;11:543485. doi:10.3389/fneur.2020.543485
80. Takagi H, Umemoto T. A meta-analysis of case-control studies of the association of migraine and patent foramen ovale. J Cardiol. 2016;67(6):493–503. doi:10.1016/j.jjcc.2015.09.016
81. Wang SB, Liu KD, Yang Y, et al. Prevalence and extent of right-to-left shunt on contrast-enhanced transcranial Doppler in Chinese patients with migraine in a multicentre case-control study. Cephalalgia. 2018;38(4):690–696. doi:10.1177/0333102417708203
82. Koutroulou I, Tsivgoulis G, Tsalikakis D, Karacostas D, Grigoriadis N, Karapanayiotides T. Epidemiology of Patent Foramen Ovale in General Population and in Stroke Patients: a Narrative Review. Front Neurol. 2020;11:281. doi:10.3389/fneur.2020.00281
83. Elgendy AY, Saver JL, Amin Z, et al. Proposal for Updated Nomenclature and Classification of Potential Causative Mechanism in Patent Foramen Ovale-Associated Stroke. JAMA Neurol. 2020;77(7):878–886. doi:10.1001/jamaneurol.2020.0458
84. West BH, Noureddin N, Mamzhi Y, et al. Frequency of Patent Foramen Ovale and Migraine in Patients With Cryptogenic Stroke. Stroke. 2018;49(5):1123–1128. doi:10.1161/strokeaha.117.020160
85. Saver JL, Carroll JD, Thaler DE, et al. Long-Term Outcomes of Patent Foramen Ovale Closure or Medical Therapy after Stroke. N Engl J Med. 2017;377(11):1022–1032. doi:10.1056/NEJMoa1610057
86. Mas JL, Derumeaux G, Guillon B, et al. Patent Foramen Ovale Closure or Anticoagulation vs. Antiplatelets after Stroke. N Engl J Med. 2017;377(11):1011–1021. doi:10.1056/NEJMoa1705915
87. Søndergaard L, Kasner SE, Rhodes JF, et al. Patent Foramen Ovale Closure or Antiplatelet Therapy for Cryptogenic Stroke. N Engl J Med. 2017;377(11):1033–1042. doi:10.1056/NEJMoa1707404
88. Lee PH, Song JK, Kim JS, et al. Cryptogenic Stroke and High-Risk Patent Foramen Ovale: the DEFENSE-PFO Trial. J Am Coll Cardiol. 2018;71(20):2335–2342. doi:10.1016/j.jacc.2018.02.046
89. Mac Grory B, Ohman EM, Feng W, et al. Advances in the management of cardioembolic stroke associated with patent foramen ovale. BMJ. 2022;376:e063161. doi:10.1136/bmj-2020-063161
90. Androulakis XM, Kodumuri N, Giamberardino LD, et al. Ischemic stroke subtypes and migraine with visual aura in the ARIC study. Neurology. 2016;87(24):2527–2532. doi:10.1212/wnl.0000000000003428
91. Gollion C, Larrue V. Cardiac sources of cerebral embolism in people with migraine. Eur J Neurol. 2021;28(4):e29. doi:10.1111/ene.14739
92. Pezzini A, Busto G, Zedde M, et al. Vulnerability to Infarction During Cerebral Ischemia in Migraine Sufferers. Stroke. 2018;49(3):573–578. doi:10.1161/strokeaha.118.020554
93. Sharma A, Gheewala N, Silver P. Role of patent foramen ovale in migraine etiology and treatment: a review. Echocardiography. 2011;28(8):913–917. doi:10.1111/j.1540-8175.2011.01460.x
94. Kang KW, Kim JT, Chang J, et al. Transient sulcal hyperintensities on fluid-attenuated inversion recovery in migraine with aura: transient sulcal hyperintensities in migraine. Headache. 2012;52(9):1430–1433. doi:10.1111/j.1526-4610.2012.02230.x
95. Yoon GJ, Kim JT, Chang J, et al. Right-to-left shunts as a cause of juxtacortical spots in patients with migraine. Eur J Neurol. 2012;19(8):1086–1092. doi:10.1111/j.1468-1331.2012.03680.x
96. Yan C, Li H, Wang C, et al. Frequency and Size of In Situ Thrombus Within Patent Foramen Ovale. Stroke. 2023;54(5):1205–1213. doi:10.1161/strokeaha.122.041524
97. Ayata C, Lauritzen M. Spreading Depression, Spreading Depolarizations, and the Cerebral Vasculature. Physiol Rev. 2015;95(3):953–993. doi:10.1152/physrev.00027.2014
98. Kissoon NR, Cutrer FM. Aura and Other Neurologic Dysfunction in or with Migraine. Headache. 2017;57(7):1179–1194. doi:10.1111/head.13101
99. Parker PD, Suryavanshi P, Melone M, et al. Non-canonical glutamate signaling in a genetic model of migraine with aura. Neuron. 2021;109(4):611–628.e618. doi:10.1016/j.neuron.2020.11.018
100. Charles AC, Baca SM. Cortical spreading depression and migraine. Nat Rev Neurol. 2013;9(11):637–644. doi:10.1038/nrneurol.2013.192
101. Dreier JP, Fabricius M, Ayata C, et al. Recording, analysis, and interpretation of spreading depolarizations in neurointensive care: review and recommendations of the COSBID research group. J Cereb Blood Flow Metab. 2017;37(5):1595–1625. doi:10.1177/0271678x16654496
102. Hansen JM, Baca SM, Vanvalkenburgh P, Charles A. Distinctive anatomical and physiological features of migraine aura revealed by 18 years of recording. Brain. 2013;136(Pt 12):3589–3595. doi:10.1093/brain/awt309
103. Lauritzen M, Dreier JP, Fabricius M, Hartings JA, Graf R, Strong AJ. Clinical relevance of cortical spreading depression in neurological disorders: migraine, malignant stroke, subarachnoid and intracranial hemorrhage, and traumatic brain injury. J Cereb Blood Flow Metab. 2011;31(1):17–35. doi:10.1038/jcbfm.2010.191
104. Lemale CL, Lückl J, Horst V, et al. Migraine Aura, Transient Ischemic Attacks, Stroke, and Dying of the Brain Share the Same Key Pathophysiological Process in Neurons Driven by Gibbs-Donnan Forces, Namely Spreading Depolarization. Front Cell Neurosci. 2022;16:837650. doi:10.3389/fncel.2022.837650
105. Hartings JA, Andaluz N, Bullock MR, et al. Prognostic Value of Spreading Depolarizations in Patients With Severe Traumatic Brain Injury. JAMA Neurol. 2020;77(4):489–499. doi:10.1001/jamaneurol.2019.4476
106. Giniatullin R, Khazipov R, van den Maagdenberg A, Jolkkonen J. Editorial: common and distinct mechanisms of migraine and stroke. Front Cell Neurosci. 2023;17:1171836. doi:10.3389/fncel.2023.1171836
107. Dreier JP, Kleeberg J, Alam M, et al. Endothelin-1-induced spreading depression in rats is associated with a microarea of selective neuronal necrosis. Exp Biol Med (Maywood). 2007;232(2):204–213.
108. Nozari A, Dilekoz E, Sukhotinsky I, et al. Microemboli may link spreading depression, migraine aura, and patent foramen ovale. Ann Neurol. 2010;67(2):221–229. doi:10.1002/ana.21871
109. Dönmez-Demir B, Yemisci M, Kılıç K, et al. Microembolism of single cortical arterioles can induce spreading depression and ischemic injury; a potential trigger for migraine and related MRI lesions. Brain Res. 2018;1679:84–90. doi:10.1016/j.brainres.2017.11.023
110. Hadjikhani N, Vincent M. Neuroimaging clues of migraine aura. J Headache Pain. 2019;20(1):32. doi:10.1186/s10194-019-0983-2
111. Close LN, Eftekhari S, Wang M, Charles AC, Russo AF. Cortical spreading depression as a site of origin for migraine: role of CGRP. Cephalalgia. 2019;39(3):428–434. doi:10.1177/0333102418774299
112. Grell AS, Haanes KA, Johansson SE, Edvinsson L, Sams A. Fremanezumab inhibits vasodilatory effects of CGRP and capsaicin in rat cerebral artery - Potential role in conditions of severe vasoconstriction. Eur J Pharmacol. 2019;864:172726. doi:10.1016/j.ejphar.2019.172726
113. Dogru MT, Dilekoz E, Alpua M, et al. Endothelial and Autonomic Functions in Patients with Migraine. Pain Med. 2020;21(2):e222–e231. doi:10.1093/pm/pnz223
114. Liu G, Feng Z, Feng F, Xue C, Liu F, Xie X. The correlation between patent foramen ovale and brain ischemia in plateau residents. BMC Cardiovasc Disord. 2021;21(1):381. doi:10.1186/s12872-021-02172-6
115. Dees B, Coleman-Jackson R, Hershey LA. Managing migraine and other headache syndromes in those over 50. Maturitas. 2013;76(3):243–246. doi:10.1016/j.maturitas.2013.04.009
116. Kellner-Weldon F, Lehmann VF, Breiding PS, et al. Findings in susceptibility weighted imaging in pediatric patients with migraine with aura. Eur J Paediatr Neurol. 2020;28:221–227. doi:10.1016/j.ejpn.2020.05.008
117. Tanos V, Raad EA, Berry KE, Toney ZA. Review of migraine incidence and management in obstetrics and gynaecology. Eur J Obstet Gynecol Reprod Biol. 2019;240:248–255. doi:10.1016/j.ejogrb.2019.07.021
118. Hoogeveen ES, Arkink EB, van der Grond J, et al. MRI evaluation of the relationship between carotid artery endothelial shear stress and brain white matter lesions in migraine. J Cereb Blood Flow Metab. 2020;40(5):1040–1047. doi:10.1177/0271678x19857810
119. Tekgol Uzuner G, Yalın OO, Uluduz D, Ozge A, Uzuner N. Migraine and cardiovascular risk factors: a clinic-based study. Clin Neurol Neurosurg. 2021;200:106375. doi:10.1016/j.clineuro.2020.106375
120. Tsao YC, Wang YF, Fuh JL, et al. Non-aura visual disturbance with high visual aura rating scale scores has stronger association with migraine chronification than typical aura. Cephalalgia. 2022;42(14):1487–1497. doi:10.1177/03331024221123074
121. George KM, Folsom AR, Sharrett AR, et al. Migraine Headache and Risk of Dementia in the Atherosclerosis Risk in Communities Neurocognitive Study. Headache. 2020;60(5):946–953. doi:10.1111/head.13794
122. Di Donato I, Bianchi S, De Stefano N, et al. Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy (CADASIL) as a model of small vessel disease: update on clinical, diagnostic, and management aspects. BMC Med. 2017;15(1):41. doi:10.1186/s12916-017-0778-8
123. Zhang R, Ouin E, Grosset L, et al. Elderly CADASIL patients with intact neurological status. J Stroke. 2022;24(3):352–362. doi:10.5853/jos.2022.01578
124. Ni W, Zhang Y, Zhang L, Xie JJ, Li HF, Wu ZY. Genetic spectrum of NOTCH3 and clinical phenotype of CADASIL patients in different populations. CNS Neurosci Ther. 2022;28(11):1779–1789. doi:10.1111/cns.13917
125. Paraskevas GP, Stefanou MI, Constantinides VC, et al. CADASIL in Greece: mutational spectrum and clinical characteristics based on a systematic review and pooled analysis of published cases. Eur J Neurol. 2022;29(3):810–819. doi:10.1111/ene.15180
126. Huang H, Xie W, Hu F, Lv H, Wu Y, Cai B. Acute bilateral multiple subcortical infarcts as manifestation in cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Neurol Sci. 2023. doi:10.1007/s10072-023-06949-9
127. Oka F, Lee JH, Yuzawa I, et al. CADASIL mutations sensitize the brain to ischemia via spreading depolarizations and abnormal extracellular potassium homeostasis. J Clin Invest. 2022;132(8). doi:10.1172/jci149759
128. Zhang W, Zhao X, Qi X, Kimber SJ, Hooper NM, Wang T. Induced pluripotent stem cell model revealed impaired neurovascular interaction in genetic small vessel disease Cerebral Autosomal Dominant Arteriopathy with Subcortical Infarcts and Leukoencephalopathy. Front Cell Neurosci. 2023;17:1195470. doi:10.3389/fncel.2023.1195470
129. Moreton FC, Cullen B, Dickie DA, et al. Brain imaging factors associated with progression of subcortical hyperintensities in CADASIL over 2-year follow-up. Eur J Neurol. 2021;28(1):220–228. doi:10.1111/ene.14534
130. Argirò A, Sciagrà R, Marchi A, et al. Coronary microvascular function is impaired in patients with cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy. Eur J Neurol. 2021;28(11):3809–3813. doi:10.1111/ene.14678
131. Taniguchi A, Shindo A, Tabei KI, et al. Imaging Characteristics for Predicting Cognitive Impairment in Patients With Cerebral Autosomal Dominant Arteriopathy With Subcortical Infarcts and Leukoencephalopathy. Front Aging Neurosci. 2022;14:876437. doi:10.3389/fnagi.2022.876437
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


