Back to Journals » Cancer Management and Research » Volume 14
Bevacizumab Combined with Continuation of EGFR-TKIs in NSCLC Beyond Gradual Progression
Authors Xu Z , Teng F, Hao X, Li J, Xing P
Received 21 February 2022
Accepted for publication 28 May 2022
Published 4 June 2022 Volume 2022:14 Pages 1891—1902
DOI https://doi.org/10.2147/CMAR.S363446
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Ahmet Emre Eşkazan
Ziyi Xu,* Fei Teng,* Xuezhi Hao, Junling Li, Puyuan Xing
Department of Medical Oncology, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, 100021, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Junling Li; Puyuan Xing, Department of Medical Oncology, National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, 100021, People’s Republic of China, Email [email protected]; [email protected]
Objective: Continuation of epidermal growth factor receptor (EGFR)-tyrosine kinase inhibitors (TKIs) has shown potential in prolonging survival in patients with non-small cell lung cancer (NSCLC) harboring EGFR mutation who had gradual progression at initial targeting therapy. However, it remains unknown whether the combination of bevacizumab and continuation of EGFR-TKIs would benefit this subpopulation. This study retrospectively explored the effect of bevacizumab combined with EGFR-TKIs in NSCLC beyond gradual progression in the real-world setting.
Methods: The records of 48 patients were reviewed who received bevacizumab and continuation of EGFR-TKIs beyond gradual progression at initial targeting therapy. The response to the treatment and post progression survival (PPS) were reviewed and analyzed.
Results: The median PPS was 11.4 months (95% CI 7.368– 15.492) for all patients included at the median follow-up time of 17.3 months. The objective response rate (ORR) was 8.3%, and the disease control rate (DCR) was 86.1% (with 3 partial response and 28 stable disease) in 36 patients who were evaluable for response with at least one measurable lesion. Univariate Cox analysis showed that age < 60, male sex, and EGFR exon19 deletion mutation were associated with longer PPS (P< 0.05). Patients harboring EGFR exon19 deletion mutation had significantly longer PPS than those with EGFR exon21 L858R mutation, with an mPPS of 15.5 months and 5.7 months, respectively (HR=0.251, 95% CI 0.112– 0.561, P=0.019). Multivariate Cox analysis indicated that age < 60 and EGFR exon19 deletion mutation were associated with longer PPS (P< 0.05).
Conclusion: Continuation of EGFR-TKI with the combination of bevacizumab is a reasonable strategy in NSCLC patients beyond gradual progression in previous EGFR-TKI treatment. Younger patients with EGFR exon19 deletion mutation may benefit more from the combination therapy.
Keywords: EGFR-TKI, bevacizumab, NSCLC, gradual progression, combination therapy
Background
The application of epidermal growth factor receptor (EGFR)-tyrosine kinase inhibitors (TKIs) has greatly influenced the treatment of non-small-cell lung cancer (NSCLC) with activating EGFR mutations such as EGFR exon19 deletion and EGFR exon21 L858R mutation.1,2 However, the resistance of EGFR-TKIs has been inevitable in the majority of NSCLC patients with EGFR mutation. Scientists have suggested that acquired resistance should meet the following criteria: objective clinical benefit from treatment with an EGFR-TKI as defined by either partial or complete response, or significant and durable stable disease of at least six months with an EGFR-TKI.3 Underlying mechanisms of resistance have been proved complicated, including the T790M substitution,4 MET amplification,5 transformation to small-cell lung cancer, mutations in PI3KCA gene,6 etc. Therefore, the clinical strategy is well worth exploring in EGFR-mutated NSCLC patients treated with EGFR-TKIs beyond progressive disease. Chinese scholars have established a clinical mode including three failure modes, namely dramatic progression, gradual progression, and local progression, aiming to favor subsequent strategies and predict survival benefit based on the previous definition of acquired resistance.
Discontinuation of EGFR-TKI may accelerate disease progression for patients with gradual progression,7 which was clinically defined as disease control lasting for at least six months and with progression in no more than two non-targeted lesions, and with the asymptomatic status or stability of pre-existing symptoms.7 Continuation of EGFR-TKI could be an optional treatment strategy for subsequent therapy after failure, and obtained a longer overall survival (OS) than chemotherapy in this cohort (39.4 months vs 17.8 months, P=0.02).8 A retrospective study in Japan also indicated that the continuation of EGFR-TKI beyond progressive disease (PD) may prolong OS compared with switching to chemotherapy (32.2 months vs 23.0 months, P=0.005).9 However, it remains unknown whether the combination of EGFR-TKI and chemotherapy or other anti-tumor regimen would bring further benefit to EGFR-mutated NSCLC patients failed in EGFR-TKI treatment. Results in the IMPRESS trial have shown that continuation of gefitinib does not prolong progression-free survival (PFS) or OS in patients who received chemotherapy as subsequent therapy after PD on first-line gefitinib.10,11 Few studies have explored the combination of EGFR-TKI and anti-angiogenic targeted agents such as bevacizumab and anlotinib after PD on previous EGFR-TKI treatment, especially for second- and third-generation EGFR-TKIs.12,13 Anti-angiogenesis is potential in anti-tumor therapy as angiogenesis is another important process in the micro-environment related to tumor growth. Vascular endothelial growth factor (VEGF) binds to VEGF receptor (VEGFR)-2 and promotes tumor growth and progress by intriguing angiogenesis. Bevacizumab is a recombinant monoclonal VEGF-targeted agent that has been proved to prolong survival in advanced NSCLC patients when combined with chemotherapy.14,15 Bevacizumab is widely used in various stages of lung cancer, which is also under study in combination with other anti-tumor agents, although the adverse events (AEs) such as hypertension and hemorrhage may lead to the discontinuation of treatment and will potentially be enhanced when combined with other anti-tumor agents. Preclinical studies have shown evidence that VEGF inhibitors may work synergistically with EGFR-TKIs16 since EGFR influences VEGF signaling,17 therefore the potent strategy of combining EGFR-TKIs and VEGF inhibitors might enhance the clinical efficacy in these patients. Clinical trials have demonstrated that using EGFR-TKI together with bevacizumab may prolong PFS compared to EGFR-TKI monotherapy as first-line treatment in EGFR-mutated NSCLC patients, although no significant difference was shown in long-term survival.18,19 Furthermore, bevacizumab has played an essential role in improving the OS beyond initial PD for metastatic colorectal cancer patients.20
In this study, we explored the efficacy of combining bevacizumab and continuation of EGFR-TKI in NSCLC patients with gradual progression after EGFR-TKIs treatment to provide more evidence for an optimal clinical strategy in the real-world setting.
Methods
Patients
Patients who received combination of EGFR-TKI and bevacizumab beyond PD of previous EGFR-TKI treatment in the Chinese Academy of Medical Sciences (CAMS) during April 2018 to April 2021 were included in this retrospective study. The clinicopathological features have been collected from their medical records, including their gender, age, Eastern Cooperative Oncology Group performance status (ECOG-PS), smoking status, EGFR mutation status, and lines of EGFR-TKI therapy. The dates of EGFR-TKI initiation, bevacizumab initiation, and Response Evaluation Criteria of Solid Tumors (RECIST)-defined PD were also obtained.
This study was approved by the Ethics Committee of the National Cancer Center/National Clinical Research Center for Cancer/Cancer Hospital, CAMS and Peking Union Medical College (approval No. 19–096-1881).
Treatment Strategy
All patients were treated with EGFR-TKIs, including first-generation EGFR-TKI erlotinib, gefitinib, icotinib, second-generation EGFR-TKI afatinib and dacomitinib, and third-generation osimertinib, which were all proved by National Medical Products Administration. When gradual progression occurred, these patients continued previous EGFR-TKI combined with bevacizumab as subsequent treatment, with or without local treatment such as radiotherapy. Tissue or liquid biopsy for further gene tests using next-generation sequencing (NGS) assay was suggested after progression. The patients were excluded if they were suspended from therapy with bevacizumab due to tolerability or any other reason, and only those who had continuation of EGFR-TKI combined with bevacizumab until progression were included in this study.
Clinical Assessment
Gradual progression was considered to occur in patients with the disease control lasting for at least six months by using previous EGFR-TKI therapy, with progression in no more than two non-targeted lesions, and with the symptomatic status or stability of pre-existing symptoms according to previous studies. The assessment of efficacy of subsequent treatment was based on the RECIST version 1.1.21 The indexes of efficacy assessment were evaluated by post progression survival (PPS), overall survival (OS), objective response rate (ORR), complete response (CR), partial response (PR), disease control rate (DCR), and stable disease (SD) rates. PPS was defined as the period between initial PD confirmation and either discontinuation of bevacizumab plus EGFR-TKI or death from any cause, and OS was defined as the period from the initiation of combination treatment to death from any cause or the last follow-up. ORR was defined as the sum of CR and PR rates, and DCR was defined as the sum of the CR, PR, and SD rates.
The relationship between PPS and clinicopathological characteristics was analyzed using univariate analysis and multivariate analysis, including age, gender, ECOG PS, tumor stage, brain metastases, best response to prior EGFR-TKI, type of disease progression lesion, treatment strategy, and line of targeted therapy. EGFR mutation status at diagnosis was also analyzed as a factor.
Statistical Analysis
Clinical characteristics and responses to therapy of patients were analyzed with descriptive statistics. Continuous variables were compared by t-tests, and categorial variables were analyzed by χ2 tests. All statistical analysis was performed by utilizing SPSS version 26.0, and P value <0.05 was considered significant. Median PPS was calculated by Kaplan–Meier product limit method. Risk factors for PPS were analyzed with the univariate Cox proportional hazards regression model and the multivariate analysis by using a Cox proportional hazards model, using the following covariates: age, gender, ECOG PS, tumor stage, brain metastases, best response to prior EGFR-TKI, type of disease progression lesion, treatment strategy, line of targeted therapy, and EGFR mutation status at diagnosis.
Results
Characteristics of Patients and Treatments
Until 28th July 2021, the median time of follow-up was 17.3 months. Totally 48 patients were incorporated into this retrospective study, including 19 patients (39.5%) who received first-generation EGFR-TKIs, 14 patients (29.2%) who received second-generation EGFR-TKIs, and 15 patients (31.3%) who received third-generation EGFR-TKI. All patients continued previous EGFR targeted treatment with the addition of bevacizumab when gradual progression occurred, assessed by investigators. The majority of patients were female who never smoked with a good ECOG-PS, with a median age 57 (range 33–74) (Table 1). All patients had an EGFR mutation, and the exon19 deletions and L585R point mutations covered about 87.6% of this cohort. The median time on initial EGFR-TKI was 13.1 months (range 6.0–62.1 months). EGFR-TKIs had been given in the first-line setting for 64.6% of patients (Table 1).
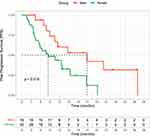
The Assessment of Clinical Efficacy
A total of 36 patients were evaluable for response with at least one measurable lesion (Table 2). The PR, SD, ORR, and DCR were observed in 8.3% (3/36), 77.8% (28/36), 8.3% (3/36), and 86.1% (31/36) of patients, respectively. Progression occurred in 13.8% of patients (5/36) at first evaluation, and totally 33 of 48 patients (68.8%) had PD until last follow-up on 28th July 2021, and 11 patients (22.9%) had died. Median PPS for all patients included was 11.4 months (95% CI 7.368–15.492), as shown in Figure 1. Overall survival was immature at the time of data cutoff.
 |
Table 2 Treatment Outcomes of Combining Bevacizumab and EGFR-TKIs Beyond Progressive Disease in 36 NSCLC Patients Harboring EGFR-Activating Mutations with at Least One Measurable Lesion |
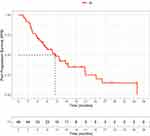 |
Figure 1 Kaplan–Meier curves of post progression survival (PPS) for the entire population. |
In 22 patients out of 33 (66.7%) who progressed beyond first- or second-generation EGFR-TKIs combining bevacizumab, 4 patients had died of dramatic progression and thus had not received further gene tests. Among 18 patients who underwent a liquid biopsy for NGS testing, 12 patients (66.7%) had T790M-positive status, while the other 6 patients (33.3%) had no acquired T790M mutation.
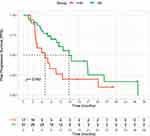
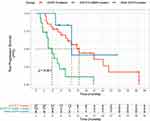
The Exploration of Risk Factors
The univariate Cox proportional hazards regression model indicated that female patients had significantly shorter PPS than male patients, with an mPPS of 8.4 months and 20.8 months, respectively (HR=2.726, 95% CI 1.176–6.319, P=0.019), as shown in Figure 2. Younger patients (<60 years old) had significantly longer PPS than older patients (≥60 years old), with an mPPS of 14.7 months and 7.0 months, respectively (HR=0.485, 95% CI 0.237–0.990, P=0.047), as shown in Figure 3. Patients who had recurrence after operation had numerically longer PPS than those who were diagnosed at stage IV (24.2 months vs 10.5 months); however, no significant difference has been observed (P=0.160). Patients harboring EGFR exon21 L858R mutation had significantly shorter PPS than those with EGFR exon19 deletion mutation, with an mPPS of 5.7 months and 15.5 months, respectively (HR=4.003, 95% CI 1.810–8.855, P<0.01) (Figure 4). No significant difference has been observed in PPS in patients with and without brain metastases before combination treatment (10.5 vs 11.4 months, P=0.896), and PPS did not differ in patients with brain metastases who received brain radiotherapy and those who did not (10.5 vs 7.9 months, P=0.424). The results for univariate Cox analyses are displayed in Figure 5. A multivariate analysis of prognostic factors was further performed by using a Cox proportional hazards model (Figure 6). Results showed that EGFR exon19 deletion mutation was an independent prognostic factor in PPS (P=0.003). Younger patients (<60 years old) had significantly a lower risk of disease progression or death than older patients (≥60 years old), indicating that age was also an independent prognostic factor in PPS (P=0.003).
Discussion
EGFR-TKIs are the standard treatment for NSCLC patients harboring activating EGFR mutations.22 However, the majority of patients develop acquired resistance with the eventual appearance of PD, usually assessed by RECIST. This criterion, though widely used, does not comprehensively reflect the diversity of EGFR-TKI failure, which might cause the discontinuation of EGFR-TKIs. Previous studies have demonstrated that the duration of disease control, evaluation of tumor burden by documentations of target and non-target lesions, and clinical symptoms are closely correlated to prognosis.8 Therefore, it is reasonable to further categorize EGFR-TKI failure modes based on the factors mentioned above, and to make a clinical decision on subsequent management according to more precise and personalized information. This retrospective study focused on the combination strategy of EGFR-TKI and bevacizumab in EGFR-mutated NSCLC patients who had gradual progression in previous EGFR-TKI treatment. Compared to historical data of continuation of EGFR-TKI beyond gradual progression, with a median duration time of 3.2 to 5.4 months,10,23 our results showed that this combination strategy could be an option for patients who had gradual progression on EGFR-TKIs with a prolonged duration time, especially for younger (<60 years old) patients with EGFR exon19 deletion mutation.
It has been hypothesized that the combination strategy may delay the resistance of EGFR-TKIs, given that EGFR-TKIs may work synergically with chemotherapy or antiangiogenic agents. The efficacy has been explored in several clinical trials for combining platinum-based chemotherapy and EGFR-TKIs for NSCLC patients harboring EGFR-sensitive mutation,24,25 suggesting that this combination regimen may obtain a longer PFS and OS than EGFR-TKI monotherapy as first-line treatment.24,25 However, continuation of EGFR-TKI combined with chemotherapy has not improved clinical outcomes compared to chemotherapy alone in first-generation EGFR-TKI failures.26 Therefore, continuation of EGFR-TKI was not recommended for patients who received platinum-based chemotherapy after EGFR-TKI progression.10,11 A preclinical experiment established that bevacizumab suppressed tumor regrowth even in erlotinib-refractory phase to prolong the anti-tumor effect in mouse xenograft models.27 The study found that complete tumor regression was observed in 2/7 mice treated with concurrent therapy of bevacizumab and erlotinib but not in erlotinib monotherapy,27 while addition of bevacizumab still suppressed tumor regrowth in those that were erlotinib-refractory,27 through comparing the anti-tumor activity by evaluating tumor volume (TV) with concurrent therapy and bevacizumab add-on treatment in erlotinib-refractory phase and defining complete tumor regression as a TV below detection limit <15 mm.27 In clinical trials, the concurrent strategy of bevacizumab and first-generation EGFR-TKI has shown potential in achieving higher response and longer survival than EGFR-TKI alone.28,29 However, the concurrent combination strategy has failed to prolong long-term survival, and has caused a higher rate of adverse events compared with monotherapy.18,19 Moreover, little evidence has been given on whether the addition of bevacizumab would benefit patients who are EGFR-TKI-refractory, and thus the optimization of scheduling is still under investigation for this combination therapy. Evidence has also been scarce for combining bevacizumab and second- or third-generation EGFR-TKI beyond PD. Our study has analyzed the efficacy of bevacizumab combined with continuation of first-, second-, and third-generation EGFR-TKIs beyond gradual progression, and has observed a median PPS of 11.4 months with no significant difference among the three generations of EGFR-TKIs, indicating that this strategy may be beneficial to patients who had gradual progression after EGFR-TKIs of any generation.
The two representative EGFR mutations, EGFR exon19 deletion and EGFR exon21 L858R missense mutation, have led to constitutively activated EGFR kinase readily inhibited by EGFR-TKIs.30 Subgroup analyses in large clinical trials have shown that the efficacy of EGFR-TKIs still varied in these two subpopulations of NSCLC patients.31 The underlying mechanisms remained controversial regarding whether patients harboring EGFR exon19 deletion tended to have longer survival than those with EGFR exon21 mutations.32 EGFR exon21 mutation is a Class II mutation and is a single-nucleotide substitution,33 which is unlike EGFR exon19 deletion, a Class I mutation including short in-frame deletions that result in the loss of four to six amino acids.33 For one thing, concomitant genetic alterations, such as PIK3CA, AKT1, and ERBB2, were correlated with reduced response to EGFR-TKI and poorer survival, and studies have indicated that patients with EGFR exon21 mutation had a significantly higher incidence of concomitant mutation somatic than those with EGFR exon19 deletion mutation.34,35 Moreover, tumor mutation burden was shown to be negatively associated with clinical outcomes in EGFR-mutant NSCLC patients by treating with EGFR-TKI, which was higher in EGFR exon21 L858R patients than in those with EGFR exon19 deletion.36 Previous studies have indicated that these two kinds of mutations should be considered distinct clinical entities due to their different response to EGFR-TKIs, therefore it is necessary to seek an optimal strategy for each subset of patients harboring EGFR mutations. Second-generation EGFR-TKI dacomitinib has shown efficacy in NSCLC patients harboring EGFR exon21 L858R, representing benefit in both PFS and OS.37 However, the study has not proved whether the single agent will benefit patients with brain metastasis at diagnosis, and combination therapy of EGFR-TKI and bevacizumab seems to be a promising strategy for this subpopulation. In the subgroup study of trial CTONG1509, the PFS was 19.5 months for patients harboring L858R mutations treated by bevacizumab plus erlotinib, twice that by erlotinib monotherapy (9.7 months).28 The HR for risk of PD in EGFR exon21 mutation and EGFR exon19 deletion was 0.51 and 0.62, respectively, indicating that patients harboring exon21 L858R mutations might benefit more from the combination therapy than those harboring exon19 deletion mutation.28 Further evidence is still required to determine the optimal strategy for EGFR exon21 L858R mutation. Results suggested that EGFR mutation status could be an independent factor for survival even beyond progression, with a longer PPS in patients harboring EGFR exon19 deletion than those with EGFR exon21 L858R point mutation (P=0.001) in this study. Previous studies have indicated that EGFR-T790M mutation accounts for approximately 50% of acquired resistance to first- or second-generation EGFR-TKIs.4 Our study reported a relatively higher rate of T790M occurrence (66.7%) after progression of combining bevacizumab and EGFR-TKI. However, a future study of larger sample size is still needed to further explore the mechanisms of acquired resistance.
Brain metastasis is one of the leading causes of lung cancer mortality, and brain tumors are often surrounded by brain edema that perhaps causes neurological symptoms and affects the quality of life. Treatment strategies are limited, including surgery and radiotherapy, which would also cause permanent damage to brain. Preclinical data suggested that bevacizumab prevented brain metastasis formation and prolonged the survival in a NSCLC mouse model,38 possibly via inhibiting the endothelial cell.38 Evidence has been also shown that bevacizumab relieved the clinical symptoms and reduced the edema volumes in brain metastatic patients by blocking the binding of VEGF-A to its receptors.39 A phase II trial has demonstrated the efficacy of bevacizumab plus paclitaxel and carboplatin as first-line treatment in NSCLC patients with asymptomatic,40 untreated brain metastases, with the mPFS, mOS, and ORR of 6.7 months, 16.0 months, and 62.7%, respectively.40 EGFR-TKIs may be favorable options which lowered the incidence of intracranial progression,41,42 since chemotherapy had trouble in crossing the blood–brain barrier and acting on micrometastatic brain lesions.41,42 A phase I/II study has explored the safety and efficacy of combining osimertinib and bevacizumab as initial treatment for NSCLC patients, in whom 31% of patients diagnosed with brain metastases were enrolled. The ORR was 100% for six patients with measurable brain lesions, compared to 66% in the FLAURA study, indicating the intracranial efficacy of combination therapy.12 A phase II study has further researched the efficacy of osimertinib and bevacizumab as subsequent therapy in NSCLC patients with EGFR T790M mutation after prior EGFR-TKI treatment.13 The result of this phase II study, however, has failed to identify the advantage of bevacizumab and osimertinib in patients with brain metastases, due to the small sample size of this subgroup.13 In our study, no significant difference has been observed in patients with or without brain metastases prior to combination therapy of EGFR-TKI and bevacizumab beyond gradual progress (P=0.896), and the addition of brain radiotherapy has not prolonged the PPS of those patients with brain metastases (P=0.421). This result is parallel to previous studies,13 which may also be due to the limitation of sample size. Notably, three patients have partial response to the continuation of EGFR-TKI plus bevacizumab in our study, including a complete intracranial response in one patient, despite the evidence that had been suggested by previous preclinical experiment.27
There are several limitations in this study. As a single-arm retrospective study, the sample is not large enough especially for subgroup analysis, therefore, it has failed to compare the efficacy of bevacizumab combined with continuation of EGFR-TKIs to other anti-tumor strategies in the control group. Studies with larger samples and multiple cohorts in multi-centers or meta-analyses are needed to further verify the conclusion. Moreover, data for OS have been immature until last follow-up, therefore the relationship between the treatment duration of bevacizumab beyond progression and OS should be explored in future studies.
Conclusion
This study has provided evidence that continuation of EGFR-TKI with the combination of bevacizumab is a reasonable strategy in NSCLC patients beyond gradual progression in previous EGFR-TKI treatment. Younger patients with EGFR exon19 deletion mutation may benefit more from the combination therapy.
Abbreviations
EGFR-TKIs, epidermal growth factor receptor-tyrosine kinase inhibitors; NSCLC, non-small cell lung cancer; PPS, post progression survival; ORR, objective response rate; DCR, disease control rate; OS, overall survival; PD, progressive disease; PFS, progression-free survival; VEGF, vascular endothelial growth factor; VEGFR, VEGF receptor; CAMS, Chinese Academy of Medical Sciences; ECOG-PS, Eastern Cooperative Oncology Group performance status; RECIST, Response Evaluation Criteria of Solid Tumors; CR, complete response; PR, partial response; SD, stable disease; COX, Cox proportional hazards regression model; TV, tumor volume.
Data Sharing Statement
Data are available on request to our corresponding authors via e-mail address provided in the title page.
Ethics Committee Approval and Patient Consent
The present study was approved by the ethics committee of Cancer Hospital, CAMS and Peking Union Medical College (approval No. 19-096-1881). Informed consent was waived by the ethics committee due to the retrospective nature of review. The data were maintained with confidentiality, and this study was performed in compliance with the Declaration of Helsinki.
Consent for Publication
All authors consent to publication.
Funding
There is no funding to report.
Disclosure
The authors have no competing interests.
References
1. Rosell R, Carcereny E, Gervais R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised Phase 3 trial. Lancet Oncol. 2012;13:239–246. doi:10.1016/S1470-2045(11)70393-X
2. Maemondo M, Inoue A, Kobayashi K, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med. 2010;362:2380–2388. doi:10.1056/NEJMoa0909530
3. Jackman D, Pao W, Riely GJ, et al. Clinical definition of acquired resistance to epidermal growth factor receptor tyrosine kinase inhibitors in non-small-cell lung cancer. Am J Clin Oncol. 2010;28:357–360. doi:10.1200/JCO.2009.24.7049
4. Kobayashi S, Boggon TJ, Dayaram T, et al. EGFR mutation and resistance of non-small-cell lung cancer to gefitinib. N Engl J Med. 2005;352:786–792. doi:10.1056/NEJMoa044238
5. Turke AB, Zejnullahu K, Wu YL, et al. Preexistence and clonal selection of MET amplification in EGFR mutant NSCLC. Cancer Cell. 2010;17:77–88. doi:10.1016/j.ccr.2009.11.022
6. Sequist LV, Waltman BA, Dias-Santagata D, et al. Genotypic and histological evolution of lung cancers acquiring resistance to EGFR inhibitors. Sci Transl Med. 2011;3:75ra26. doi:10.1126/scitranslmed.3002003
7. Chaft JE, Oxnard GR, Sima CS, Kris MG, Miller VA, Riely GJ. Disease flare after tyrosine kinase inhibitor discontinuation in patients with EGFR-mutant lung cancer and acquired resistance to erlotinib or gefitinib: implications for clinical trial design. Clin Cancer Res. 2011;17:6298–6303. doi:10.1158/1078-0432.CCR-11-1468
8. Yang JJ, Chen HJ, Yan HH, et al. Clinical modes of EGFR tyrosine kinase inhibitor failure and subsequent management in advanced non-small cell lung cancer. Lung Cancer. 2013;79:33–39. doi:10.1016/j.lungcan.2012.09.016
9. Nishie K, Kawaguchi T, Tamiya A, et al. Epidermal growth factor receptor tyrosine kinase inhibitors beyond progressive disease: a retrospective analysis for Japanese patients with activating EGFR mutations. J Thorac Oncol. 2012;7:1722–1727. doi:10.1097/JTO.0b013e31826913f7
10. Soria JC, Wu YL, Nakagawa K, et al. Gefitinib plus chemotherapy versus placebo plus chemotherapy in EGFR-mutation-positive non-small-cell lung cancer after progression on first-line gefitinib (IMPRESS): a phase 3 randomised trial. Lancet Oncol. 2015;16:990–998. doi:10.1016/S1470-2045(15)00121-7
11. Mok TSK, Kim SW, Wu YL, et al. Gefitinib plus chemotherapy versus chemotherapy in epidermal growth factor receptor mutation-positive non-small-cell lung cancer resistant to first-line gefitinib (IMPRESS): overall survival and biomarker analyses. Am J Clin Oncol. 2017;35:4027–4034. doi:10.1200/JCO.2017.73.9250
12. Yu HA, Schoenfeld AJ, Makhnin A, et al. Effect of osimertinib and bevacizumab on progression-free survival for patients with metastatic EGFR-mutant lung cancers: a phase 1/2 single-group open-label trial. JAMA Oncol. 2020;6:1048–1054. doi:10.1001/jamaoncol.2020.1260
13. Akamatsu H, Toi Y, Hayashi H, et al. Efficacy of osimertinib plus bevacizumab vs osimertinib in patients with EGFR T790M-mutated non-small cell lung cancer previously treated with epidermal growth factor receptor-tyrosine kinase inhibitor: West Japan oncology group 8715L phase 2 randomized clinical trial. JAMA Oncol. 2021;7:386–394.
14. Sandler A, Gray R, Perry MC, et al. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med. 2006;355:2542–2550. doi:10.1056/NEJMoa061884
15. Zhou C, Wu YL, Chen G, et al. BEYOND: a randomized, double-blind, placebo-controlled, multicenter, phase III study of first-line carboplatin/paclitaxel plus bevacizumab or placebo in Chinese patients with advanced or recurrent nonsquamous non-small-cell lung cancer. Am J Clin Oncol. 2015;33:2197–2204. doi:10.1200/JCO.2014.59.4424
16. Naumov GN, Nilsson MB, Cascone T, et al. Combined vascular endothelial growth factor receptor and epidermal growth factor receptor (EGFR) blockade inhibits tumor growth in xenograft models of EGFR inhibitor resistance. Clin Cancer Res. 2009;15:3484–3494. doi:10.1158/1078-0432.CCR-08-2904
17. De Luca A, Carotenuto A, Rachiglio A, et al. The role of the EGFR signaling in tumor microenvironment. J Cell Physiol. 2008;214:559–567. doi:10.1002/jcp.21260
18. Maemondo M, Fukuhara T, Saito H, et al. NEJ026: final overall survival analysis of bevacizumab plus erlotinib treatment for NSCLC patients harboring activating EGFR-mutations. J Clin Oncol. 2020;38:9506. doi:10.1200/JCO.2020.38.15_suppl.9506
19. Yamamoto N, Seto T, Nishio M, et al. Erlotinib plus bevacizumab (EB) versus erlotinib alone (E) as first-line treatment for advanced EGFR mutation–positive non-squamous non–small-cell lung cancer (NSCLC): survival follow-up results of JO25567. J Clin Oncol. 2018;36:9007. doi:10.1200/JCO.2018.36.15_suppl.9007
20. Grothey A, Sugrue MM, Purdie DM, et al. Bevacizumab beyond first progression is associated with prolonged overall survival in metastatic colorectal cancer: results from a large observational cohort study (BRiTE). Am J Clin Oncol. 2008;26:5326–5334. doi:10.1200/JCO.2008.16.3212
21. Therasse P, Arbuck SG, Eisenhauer EA, et al.; European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Ins. 2000;92:205–216.
22. Lee JK, Hahn S, Kim DW, et al. Epidermal growth factor receptor tyrosine kinase inhibitors vs conventional chemotherapy in non-small cell lung cancer harboring wild-type epidermal growth factor receptor: a meta-analysis. JAMA. 2014;311:1430–1437. doi:10.1001/jama.2014.3314
23. Asami K, Okuma T, Hirashima T, et al. Continued treatment with gefitinib beyond progressive disease benefits patients with activating EGFR mutations. Lung Cancer. 2013;79:276–282. doi:10.1016/j.lungcan.2012.11.022
24. Wu YL, Lee JS, Thongprasert S, et al. Intercalated combination of chemotherapy and erlotinib for patients with advanced stage non-small-cell lung cancer (FASTACT-2): a randomised, double-blind trial. Lancet Oncol. 2013;14:777–786. doi:10.1016/S1470-2045(13)70254-7
25. Hosomi Y, Morita S, Sugawara S, et al. Gefitinib alone versus gefitinib plus chemotherapy for non-small-cell lung cancer with mutated epidermal growth factor receptor: NEJ009 study. Am J Clin Oncol. 2020;38:115–123. doi:10.1200/JCO.19.01488
26. Goldberg SB, Oxnard GR, Digumarthy S, et al. Chemotherapy with Erlotinib or chemotherapy alone in advanced non-small cell lung cancer with acquired resistance to EGFR tyrosine kinase inhibitors. Oncologist. 2013;18:1214–1220. doi:10.1634/theoncologist.2013-0168
27. Masuda C, Yanagisawa M, Yorozu K, et al. Bevacizumab counteracts VEGF-dependent resistance to erlotinib in an EGFR-mutated NSCLC xenograft model. Int J Oncol. 2017;51:425–434. doi:10.3892/ijo.2017.4036
28. Zhou Q, Wu YL, Cheng Y, et al. 1480O - CTONG 1509: phase III study of bevacizumab with or without erlotinib in untreated Chinese patients with advanced EGFR-mutated NSCLC. Ann Oncol. 2019;30:v603. doi:10.1093/annonc/mdz260.002
29. Rosell R, Dafni U, Felip E, et al. Erlotinib and bevacizumab in patients with advanced non-small-cell lung cancer and activating EGFR mutations (BELIEF): an international, multicentre, single-arm, phase 2 trial. Lancet Respir Med. 2017;5:435–444. doi:10.1016/S2213-2600(17)30129-7
30. Sakurada A, Shepherd FA, Tsao MS. Epidermal growth factor receptor tyrosine kinase inhibitors in lung cancer: impact of primary or secondary mutations. Clin Lung Cancer. 2006;7(Suppl 4):S138–44. doi:10.3816/CLC.2006.s.005
31. Zhao Y, Liu J, Cai X, et al. Efficacy and safety of first line treatments for patients with advanced epidermal growth factor receptor mutated, non-small cell lung cancer: systematic review and network meta-analysis. BMJ. 2019;367:l5460. doi:10.1136/bmj.l5460
32. CK Lee, Wu YL, Ding PN, et al. Impact of specific Epidermal Growth Factor Receptor (EGFR) mutations and clinical characteristics on outcomes after treatment with EGFR tyrosine kinase inhibitors versus chemotherapy in EGFR-mutant lung cancer: a meta-analysis. Am J Clin Oncol. 2015;33:1958–1965. doi:10.1200/JCO.2014.58.1736
33. da Cunha Santos G, Shepherd FA, Tsao MS. EGFR mutations and lung cancer. Annu Rev Pathol. 2011;6:49–69. doi:10.1146/annurev-pathol-011110-130206
34. Hong S, Gao F, Fu S, et al. Concomitant genetic alterations with response to treatment and epidermal growth factor receptor tyrosine kinase inhibitors in patients with EGFR-mutant advanced non-small cell lung cancer. JAMA Oncol. 2018;4:739–742. doi:10.1001/jamaoncol.2018.0049
35. Liang H, Li C, Zhao Y, et al. Concomitant mutations in EGFR 19Del/L858R mutation and their association with response to EGFR-TKIs in NSCLC patients. Cancer Manag Res. 2020;12:8653–8662. doi:10.2147/CMAR.S255967
36. Offin M, Rizvi H, Tenet M, et al. Tumor mutation burden and efficacy of EGFR-tyrosine kinase inhibitors in patients with EGFR-mutant lung cancers. Clin Cancer Res. 2019;25:1063–1069. doi:10.1158/1078-0432.CCR-18-1102
37. Mok TS, Cheng Y, Zhou X, et al. Improvement in overall survival in a randomized study that compared dacomitinib with gefitinib in patients with advanced non-small-cell lung cancer and EGFR-activating mutations. Am J Clin Oncol. 2018;36:2244–2250. doi:10.1200/JCO.2018.78.7994
38. Ilhan-Mutlu A, Osswald M, Liao Y, et al. Bevacizumab prevents brain metastases formation in lung adenocarcinoma. Mol Cancer Ther. 2016;15:702–710. doi:10.1158/1535-7163.MCT-15-0582
39. Meng X, Zhao R, Shen G, Dong D, Ding L, Wu S. Efficacy and safety of bevacizumab treatment for refractory brain edema: case report. Medicine. 2017;96:e8280. doi:10.1097/MD.0000000000008280
40. Besse B, Le Moulec S, Mazières J, et al. Bevacizumab in patients with nonsquamous non-small cell lung cancer and asymptomatic, untreated brain metastases (BRAIN): a nonrandomized, phase II study. Clin Cancer Res. 2015;21:1896–1903. doi:10.1158/1078-0432.CCR-14-2082
41. Yang JJ, Zhou C, Huang Y, et al. Icotinib versus whole-brain irradiation in patients with EGFR-mutant non-small-cell lung cancer and multiple brain metastases (BRAIN): a multicentre, phase 3, open-label, parallel, randomised controlled trial. Lancet Respir Med. 2017;5:707–716. doi:10.1016/S2213-2600(17)30262-X
42. Soria JC, Ohe Y, Vansteenkiste J, et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med. 2018;378:113–125. doi:10.1056/NEJMoa1713137
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.