Back to Journals » Clinical Epidemiology » Volume 15
Benchmarking Maintenance Therapy Survival in First-Line Platinum-Based Chemotherapy–Treated Patients with Advanced Urothelial Carcinoma Using Simulated Disease Modeling
Authors Galsky MD, Wirtz HS, Bloudek B , Hepp Z, Farrar M, Timmons J, Lenero E, Powles T
Received 24 February 2023
Accepted for publication 1 June 2023
Published 21 June 2023 Volume 2023:15 Pages 765—773
DOI https://doi.org/10.2147/CLEP.S409791
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Henrik Sørensen
Matthew D Galsky,1 Heidi S Wirtz,2 Brian Bloudek,3 Zsolt Hepp,2 Mallory Farrar,2 Jack Timmons,3 Enrique Lenero,4 Thomas Powles5
1Tisch Cancer Institute, Icahn School of Medicine at Mount Sinai, New York, NY, USA; 2Seagen Inc., Bothell, WA, USA; 3Curta Inc., Seattle, WA, USA; 4Astellas Pharma Inc., Northbrook, IL, USA; 5Barts Cancer Centre, Queen Mary University of London, London, UK
Correspondence: Matthew D Galsky, Tisch Cancer Institute, Icahn School of Medicine at Mount Sinai, New York, NY, USA, Tel +1 212 241 6756, Fax +1 646 537 9639, Email [email protected]
Objective: First-line (1L) maintenance avelumab prolonged overall survival (OS) in patients with advanced urothelial carcinoma (aUC) in JAVELIN Bladder 100. OS was measured from maintenance initiation in patients with disease control following 1L platinum-based therapy (PBT). The OS impact of maintenance for the 1L PBT–treated population is unknown since it was not measured from 1L initiation, nor can it be benchmarked with other 1L therapies. To characterize the OS impact of maintenance avelumab, we used an oncology simulation model to estimate the OS of maintenance-eligible and -ineligible patients with aUC from 1L PBT initiation.
Methods: We developed a simulated cohort of 1L PBT–treated patients with aUC, including those who did and did not receive maintenance avelumab. Eligibility was assessed at 5.6 months post 1L PBT initiation based on the JAVELIN trial design. Among the 1L-treated population, 58% (95% credible interval [CrI] 49– 67%) were projected to be eligible (calculated from contemporary phase 3 trials); of those, 85% were assumed to receive maintenance. The model estimated median OS (mOS) among a maintenance-ineligible simulated cohort which when combined with the maintenance-eligible cohort yielded an estimated OS in the overall maintenance- intended population from 1L PBT initiation.
Results: Approximately half of the modeled 1L PBT–treated population received maintenance. Estimated mOS was 10.1 months (95% CrI 7.5– 13.5) for the maintenance-ineligible cohort, 29.3 months (95% CrI 24.8– 33.9) for the maintenance-eligible, received maintenance cohort, and 15.9 months (95% CrI 13.2– 19.1) in the overall maintenance-intended, 1L PBT–treated population, including those eligible and ineligible for maintenance.
Conclusion: The model shows that maintenance avelumab has a modest impact on OS in the overall 1L PBT–treated population of patients with aUC. While maintenance avelumab improves OS for eligible patients, a large proportion of the maintenance-intended population may not receive maintenance due to ineligibility or physician/patient choice.
Keywords: maintenance eligibility, maintenance avelumab, oncology simulation model, overall survival, urothelial carcinoma
Introduction
The National Comprehensive Cancer Network (NCCN) and European Society for Medical Oncology (ESMO) guidelines recommend platinum-based therapy (PBT) for first-line (1L) treatment of patients with advanced urothelial carcinoma (aUC) followed by maintenance avelumab in patients without disease progression after 1L PBT.1,2 However, differences in overall survival (OS) endpoint assessment, inclusion criteria, and trial populations between the JAVELIN Bladder 100 trial (JAVELIN), which investigated maintenance avelumab, and a traditional trial design for a 1L therapy mean the survival benefit of maintenance avelumab cannot be well characterized or benchmarked with other 1L therapies using conventional methods such as network meta-analyses or indirect treatment comparisons.3 In JAVELIN, patients were enrolled and received maintenance avelumab if they had no disease progression (ie, complete response, partial response, or stable disease after 4–6 cycles of PBT: gemcitabine [Gem] + cisplatin [Cis]/ carboplatin [Carbo]), and following a treatment-free interval (TFI) of 4–10 weeks4 (Supplemental Figure 1). Because of these rigorous inclusion criteria, the patient cohort is not representative of the overall aUC population. Patients who could not receive at least 4 cycles of PBT or who progressed on or immediately following PBT were not included in JAVELIN. Thus, the OS from PBT treatment initiation in the overall population of all patients with the intention to later receive maintenance avelumab (1L PBT maintenance intended) is unknown (Supplemental Figure 2). Subsequently, physicians and researchers are not able to characterize the survival benefit of 1L PBT followed by maintenance avelumab relative to other 1L treatments at the population level, limiting the ability to make informed treatment decisions now, and in the future. It is difficult for clinicians to know with certainty if patients will maintain stable disease, tolerate or respond to 1L PBT, and, hence, be eligible for maintenance avelumab. In addition, due to the design of JAVELIN, the OS of maintenance-ineligible patients from initiation of 1L PBT is unknown. To address this, we used an oncology simulation model (OSM) framework to estimate the OS of patients with aUC who received 1L PBT, including both maintenance-eligible and -ineligible patients, measured from initiation of 1L PBT. Disease modeling is increasingly being used to answer similar questions related to patient outcomes and can be used to inform decision-making.5 The OSM framework estimate was performed to align the OS estimate for the maintenance-intended population with the common initiation point to benchmark with other 1L clinical trials.6,7
Methods
Overall Model Framework–Base Case
The OSM framework was utilized because it offers a robust methodological structure for generating estimates of population-level patient survival in oncology and may be utilized to benchmark outcomes from trials of different design such as JAVELIN and other 1L therapies (Figure 1). In addition, the OSM framework was previously used to estimate disease prevalence in breast cancer;8 prevalence and survival outcomes in bladder cancer;9 progression-free survival (PFS), OS, and patient productivity losses in classical Hodgkin lymphoma;10,11 and PFS and OS in T-cell lymphoma.12
 |
Figure 1 Comparison of the design of an oncology maintenance therapy trial with a traditional 1L oncology therapy trial. Common 1L oncology clinical trial designs measure OS from initiation of 1L therapy at randomization. Bladder cancer maintenance clinical trial designs4,20 measure OS from initiation of maintenance therapy, a period of time after the initiation of 1L therapy in those patients who had no disease progression after 1L chemotherapy (nonprogressors). Comparing these two trial designs is a controversial issue and has been described in a recent publication.21 Abbreviation: 1L, first line. |
The OSM uses a continuous, dynamic, Markov cohort model to generate estimates of population-level patient survival in oncology. In the OSM, patient cohorts transition between defined health states, eg, from the progressed disease state to death, with transitions informed by PFS and OS as reported in published literature.9
This OSM framework was utilized in this study to estimate the OS of 1L PBT–treated patients ± maintenance avelumab (1L PBT maintenance intended) from treatment initiation (1L PBT start). To estimate OS from 1L PBT start in 1L PBT maintenance–intended patients, it was necessary to consider the three patient populations that exist in a 1L-treated cohort: (1) The maintenance avelumab-eligible, received maintenance population consisted of patients who were maintenance eligible and received maintenance; (2) The maintenance avelumab–eligible, did not receive maintenance population consisted of patients who were eligible for maintenance avelumab but did not receive maintenance avelumab treatment due to patient or provider decision-making; (3) The maintenance avelumab–ineligible population consisted of patients who progressed on 1L PBT and were ineligible to receive maintenance.
To estimate the mOS of the maintenance-intended, 1L PBT–treated population (the unknown endpoint), inputs were needed for each of the three subgroups. Some were readily available in the literature and some were unknown (Table 1 and Supplemental Figure 2) and needed to be calculated or estimated: (1) mOS and OS curve data for patients who were maintenance eligible, received maintenance were informed by results from the JAVELIN avelumab arm;4 (2) mOS and OS curve data for patients who were maintenance eligible, did not receive maintenance were informed by results from the JAVELIN best supportive care (BSC) arm;4 (3) the mOS of the maintenance-ineligible population was estimated using the OS curves of the JAVELIN BSC arm and the KEYNOTE-361 PBT arm (see Supplemental Materials 2 Statistical Analysis Methodology, Supplemental Table 1, and Supplemental Figure 3).
 |
Table 1 Summary of Known and Unknown Data in the 1L PBT–Treated, Maintenance Avelumab–Intended Population of Patients with aUC |
Control arm data of patients that received 1L PBT from contemporary 1L clinical trials were evaluated for inclusion in the OSM. KEYNOTE-36113 was ultimately considered the best choice for the OSM base case based on expert (MG and TP) clinical opinion and because it included the greatest proportion of patients that received programmed cell death protein 1/ligand 1 (PD1/L1) immunotherapy in the second-line (2L) setting compared with the other 1L trials considered (48%; Supplemental Table 2). Additionally, it provided the most contemporary data, it was the best representation of real-world treatment patterns, and it had the most overall similarities between the simulated cohort and the JAVELIN population, particularly in median duration of 1L PBT treatment. Patient characteristics for the trials included in the OSM base case are summarized in Supplemental Table 3.
A time period of 5.6 months between initiation of 1L PBT and starting maintenance was used in the model (corresponding to the model assumption of 6 cycles of PBT [18 weeks] and a 6-week TFI). Based on PFS data from the KEYNOTE-361 chemotherapy arm, 58% (95% credible interval [Crl] 49–67%) of patients were eligible for maintenance treatment, and 42% were ineligible at 5.6 months post-initiation of 1L PBT.
As JAVELIN BSC4,14 and KEYNOTE-361 control arm data are available for 1L PBT–treated patients who received Gem + Carbo specifically,13 we also investigated OS within this subgroup. Model variations were also conducted using data from the Gem + Cis subgroup; however, as data for the Gem + Cis subgroup were not available from KEYNOTE-361,13 data from the IMvigor130 trial15 were used to address this data gap.
The following subsections further explain the methodology for estimating the mOS for each population: maintenance avelumab eligible, received maintenance; maintenance avelumab eligible, did not receive maintenance; and maintenance avelumab ineligible (Table 1/Supplemental Figure 2). Methodology for estimating the proportion of patients in each patient group is also described.
Maintenance Eligible, Received Maintenance
OS in patients who were eligible for and received maintenance was derived from JAVELIN, which reported mOS of 23.8 months (95% CI 19.9-28.8)4 for maintenance avelumab. As not all patients who are eligible for a therapy go on to receive it in the real world, the authors’ (MG and TP) clinical experience informed the assumption that 85% of eligible patients would receive maintenance treatment, and 15% of maintenance-eligible patients would not. This was chosen as a conservative estimate, and recent real-world data suggests that maintenance avelumab uptake may be lower in clinical practice.16 Based on these estimates, maintenance avelumab utilization was estimated to be 49% at the population level (58% x 85% = 49%).13
Maintenance Eligible, Did Not Receive Maintenance
OS in patients who were eligible for but who did not receive maintenance was derived from the BSC arm of JAVELIN: 15.0 months (95% CI 13.5–18.2),4 combined with the estimated 1L treatment and TFI. Based on the authors (MG and TP) clinical experience that 15% of maintenance-eligible patients would not receive it, we estimated that 9% of patients at the population level (58% x 15% = 9%) were maintenance eligible but did not receive maintenance.
Maintenance Ineligible
OS in patients who initiated 1L PBT and were maintenance ineligible is unknown. This was estimated in the model using the known OS of the overall aUC population (informed by the PBT control arm of KEYNOTE-361)13 and the known OS of patients who were maintenance eligible but did not receive maintenance (informed by the JAVELIN BSC arm).4 OS was estimated based on the difference between the OS curves of the JAVELIN BSC arm (20.6 months),4 and the KEYNOTE-361 chemotherapy arm (14.3 months).13 mOS of the maintenance-ineligible patient population was estimated from an exponential survival curve based on the hazard function derived from the OS curves of the JAVELIN BSC arm and the KEYNOTE-361 chemotherapy arm. Exact calculations for this estimate can be found in the Supplemental Materials 2 Statistical Analysis Methodology. Based on PFS data from the KEYNOTE-361 chemotherapy arm, 42% of 1L PBT–treated patients were estimated to have disease progression at 5.6 months post 1L PBT start and, therefore, were ineligible for maintenance, because in JAVELIN only patients without progression after 1L PBT were eligible.
First-Line PBT Treated, Maintenance Intended
OS in the overall 1L PBT-treated, maintenance-intended patient population was estimated using a weighted average hazard function of survival among the three populations (maintenance-eligible, received maintenance; maintenance-eligible, did not receive maintenance; and maintenance-ineligible) (Supplemental Materials 2 Statistical Analysis Methodology).
Stratified Model Framework by Type of PBT Received in Gem + Carbo and Gem + Cis–Treated Patients
The OSM framework was also applied to the subgroups of 1L PBT–treated patients who received Gem + Carbo or Gem + Cis to estimate OS in these patient subgroups. KEYNOTE-361 reported a median PFS of 5.8 months in 1L PBT–treated patients who received Gem + Carbo, so the proportion eligible for maintenance was based on the Gem + Carbo subgroup PFS data.13 Based on the PFS curve, 52% (95% Crl 40–62%) of patients that received Gem + Carbo were assumed to be eligible, and 85% of these eligible patients were estimated to receive maintenance in the model (consistent with the base case); thus, 44% of patients who received Gem + Carbo at the population level received maintenance. KEYNOTE-361 did not report median PFS for the subgroup of 1L PBT–treated patients who received 1L Gem + Cis,13 so the proportion eligible for maintenance was estimated using data from the Gem + Cis subgroup of the IMvigor 130 trial.15 Based on the PFS of the Gem + Cis subgroup, 54% (95% CrI 40–66%) of patients were assumed to be eligible, and, as in the base case, 85% of these eligible patients were estimated to receive maintenance in the model, so 46% of patients who received Gem + Cis at the population level received maintenance.
Stratified Model Framework Varying OS Inputs
To confirm the robustness of the OS findings for the combined OS in the 1L PBT–treated, maintenance-intended patients, we modeled different scenarios by varying the OS inputs. These scenarios used OS inputs from the control arms of the IMvigor130 and DANUBE trials, along with base case data from KEYNOTE-361.13,15,17
Results
Estimated mOS in Modeled Patient Populations
Using the OSM model, the mOS for the maintenance-eligible, received maintenance cohort was 29.3 months (95% CrI 24.8–33.9); the mOS for patients who were maintenance eligible, but did not receive maintenance was 20.6 months (95% CrI 17.8–23.3); and the estimated mOS for patients who were maintenance ineligible was 10.1 months (95% CrI 7.5–13.5) (Figure 2A). Combined, the estimated mOS in 1L PBT–treated, maintenance-intended patients was 15.9 months (95% CrI 13.2–19.1) (Figure 2B). As an illustrative comparison, the mOS with PBT alone was 14.3 months (95% CI 12.3–16.7), as reported in the control arm of KEYNOTE-361.13
 |
Figure 2 Estimated OS in 1L PBT maintenance–intended patients with aUC from initiation of 1L PBT. (A) OS in maintenance eligible, received maintenance from the JAVELIN active arm (green), OS in maintenance eligible, did not receive maintenance from the JAVELIN BSC arm (yellow), and the estimated OS in maintenance ineligible (red) were used to calculate (B) the combined OS in the 1L PBT–treated, maintenance-intended patient population (black) by calculating the weighted average hazard of the three subgroups.4 Abbreviations: 1L, first-line; aUC, advanced urothelial carcinoma; BSC, best supportive care; mOS, median overall survival; PBT, platinum-based therapy; TFI, treatment-free interval. Note: aIncludes 5.6-month run-in period. |
mOS Stratified by Type of PBT Received. Gem + Carbo and Gem + Cis–Treated Patients
The proportions of maintenance-eligible patients were estimated from KEYNOTE-36113 and IMvigor-130.15 In patients treated with Gem + Carbo (assumed to be Cis ineligible), the estimated OS was 13.5 months (95% CrI 10.2–17.3). In patients treated with Gem + Cis, the estimated OS was 16.2 months (95% CrI 10.9–23.0).
Varying OS Inputs for Different Scenarios
Modeling using OS data from the KEYNOTE-361 trial13 found that varying the proportion of patients who were eligible for and who received maintenance between 20% and 50% led to a mOS ranging from 14.9–15.9 months (Supplemental Table 4). If the proportion of eligible patients that received maintenance using IMvigor13015 and DANUBE17 data were varied between 20% and 50%, mOS ranged from 13.9–14.9 months and 12.5–13.3 months in IMvigor13015 and DANUBE17 respectively.
An illustrative comparison (ie naïve cross-trial comparison of the model results to the results from published meta-analysis) demonstrated that if key baseline assumptions (% of eligible patients that received maintenance and mOS following PBT using different clinical trials) were varied, the incremental survival benefit of 1L PBT followed by maintenance relative to PBT alone among 1L PBT maintenance-intended patients was shown to vary between 2 and 8 weeks (or approximately 0.5–2 months; Figure 3).
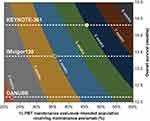 |
Figure 3 Contour plot of population-level OS impact across included clinical trials.4,13,15,16 By varying the proportion of the 1L PBT maintenance-intended population that received maintenance (x-axis) and varying the mOS associated with PBT between 12.0 and 15.0 months (y-axis), the survival benefit from maintenance compared with PBT alone (based on OS data from the KEYNOTE-361,13 IMvigor130,15 and DANUBE17 clinical trials) ranged from 2 to 8 weeks (shown in colored bands). mOS for included clinical trials is shown by the dotted lines. The red dot highlights the expected survival benefit of 2 weeks based on PBT control-arm data from DANUBE17 if 22.5% of eligible patients received maintenance avelumab. (The green dot highlights the expected survival benefit of 4 weeks based on PBT control-arm data from IMvigor13015 if 36% of eligible patients received maintA. The yellow dot highlights the expected survival benefit of 6 weeks based on PBT control-arm data from KEYNOTE-36113 if 46% of eligible patients received maintenance (compared with 5 weeks from IMvigor13015 and 4 weeks from DANUBE17). Abbreviations: 1L, first-line; mOS, median overall survival; OS, overall survival; PBT, platinum-based therapy. |
Discussion
The conditional eligibility of the maintenance avelumab cohort in the JAVELIN trial meant that patients with progressive disease on 1L PBT were not included in the study. This makes it difficult to understand the impact of maintenance on mOS in the overall, 1L PBT–treated population from 1L treatment initiation on a population level or to benchmark outcomes with maintenance avelumab relative to other 1L treatments. Our model estimated that approximately half of 1L PBT–treated patients with aUC would not receive maintenance, regardless of their eligibility. This contributed to the modest estimated mOS of 15.9 (95% Crl 13.2–19.1) months in the overall 1L PBT–treated, maintenance-intended population. Increasing the proportion of eligible patients who receive maintenance to 100% resulted in a mOS of 16.3 months at the population level, indicating that maintenance therapy would still provide only modest improvement in overall 1L PBT–treated mOS even in ideal circumstances, because a large proportion of patients are ineligible for maintenance due to disease progression on 1L PBT therapy. Our modeling suggests that the estimated mOS benefit of maintenance in the 1L PBT–treated patient population is approximately 1–2 months when contextualized against the 14.3-month (95% CI 12.3–16.7) OS with PBT alone13 (Figure 3).
The subgroup analyses suggest that patients treated with Gem + Carbo at 1L may have less OS gain from the addition of maintenance treatment (13.5 months [95% Crl 10.2–17.3] compared with 12.3 months [95% CI 10.0–15.5] without maintenance in KEYNOTE-361) than patients who received Gem + Cis (16.2 months [95% Crl 10.9–23.0] compared with 14.6-months [95% CI 10.8–19.6] without maintenance in IMvigor130).15 This difference in outcomes highlights the even greater unmet need in this subgroup of patients.
There are several difficulties faced by clinicians in determining the population-level benefit of new therapies in oncology, and this model can help contextualize and benchmark 1L PBT plus maintenance with emerging therapies for 1L aUC. The OSM methodology is also of value due to the current lack of real-world data on use of maintenance avelumab. These data underscore the difficulties physicians face when deciding to use switch-maintenance therapies, such as avelumab, due to the uncertainty regarding if patients will respond to 1L therapy and be eligible for maintenance. Similarly, a current gap in the knowledge is the impact of PD1/L1 therapies on longer-term survival. The OSM methodology highlights these challenges and offers a solution by combining survival data with anachronistic anchor points. Additional uses of the OSM methodology include estimating the impact of treatment sequences ahead of real-world data availability, which underscores the value of this methodology to researchers and physicians.18 This approach will become increasingly relevant in the coming years as more complex treatment sequences require modeling.
Limitations
OS model inputs are based on published data from 1L clinical trials, which may overestimate real-world outcomes. For instance, the 23.8 month (95% CI 19.9–28.8) OS for the maintenance-eligible, received maintenance population used in the OSM base case was taken from the JAVELIN trial, which may be an overestimate, as the trial design effectively selected for patients with less aggressive disease. Conversely, the OS model inputs from published clinical trials may underestimate current real-world outcomes among patients who progressed after 1L treatment, as new 2L+ treatment options that can improve the outcomes for these patients have recently become available, and further research is required to confirm if these findings apply to real-world clinical practice. However, there were minimal differences in OS when the proportion who received maintenance was varied in scenario analysis testing. The inclusion of additional clinical trial data investigating the survival benefit of vinflunine19 and pembrolizumab20 as maintenance therapies were considered; however, they were not included in the model, because these therapies are not currently recommended by US or European treatment guidelines for this indication in patients with aUC.1,2 A lack of patient-level data meant that assumptions were made for the modeling of OS in the maintenance-ineligible subpopulation. However, this was necessary because existing trials, including JAVELIN4 did not enroll patients from 1L-treatment initiation. Because of a lack of patient-level data, model estimates were based on optimistic assumptions. Subgroup analyses, including those reported for the Gem + Cis and Gem + Carbo subgroups, are subject to limitations due to the much smaller sample sizes in subgroups compared with overall trial treatment arms and differences in the characteristics of the patient populations studied.
Conclusion
Robust disease modeling estimates that maintenance avelumab may provide a modest improvement in mOS for eligible, maintenance-intended patients and that overall, about half of patients with aUC who receive 1L PBT treatment will not be eligible to receive maintenance. While outcomes in maintenance avelumab–treated patients are improved, compared with 1L PBT alone, outcomes for the other half of 1L PBT–treated patients who are not eligible and who do not receive avelumab are worse, reducing the overall survival impact of avelumab on the overall 1L PBT–treated, maintenance-intended population. These model results highlight the continued unmet need, even with the introduction of avelumab maintenance in 1L aUC and have implications for patients with aUC both individually and at the population level.
Data Sharing Statement
This analysis is based on previously published data.
Ethics Approval and Informed Consent
This analysis is based on published data and ethical approval was not required.
Acknowledgments
Parts of these data have previously been presented at the American Society of Clinical Oncology (ASCO) Annual Meeting, Chicago, IL, June 3–7, 2022. Medical writing support was provided by Philip Ruane of Curo Consulting, a division of Envision Pharma Group, and funded by Seagen Inc.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by funding from Seagen Inc. and Astellas, Inc.
Disclosure
MDG is a paid consultant for AbbVie, Aileron Therapeutics, Alligator, Asieris, Astellas, AstraZeneca, Basilea, Bicycle, BioMotiv, Bristol Myers Squibb, Curis, Dendreon, Dracen Pharmaceutical, Dragonfly, EMD Serono, Genentech, Gilead, Fujifilm, GSK, Incyte, Inovio Pharmaceuticals, Janssen, Lilly, Merck, Novartis, Numab Therapeutics, Pfizer, Seagen, Urogen; has equity ownership in Rappta Therapeutics; holds patents/royalties for “Methods and compositions for treating cancer and related methods (20120322792)”; and has received research funding from AstraZeneca, Bristol Myers Squibb, Dendreon, Genentech, Janssen, Merck, and Novartis. HSW and ZH are employees of, and own stock in, Seagen. HSW is a former employee of and owns stock in Amgen Inc. At the time of this study MF was an employee of Seagen, and owns stock in Seagen. BB and JT are employees of Curta and paid consultants to Seagen in connection with this project. EL is an employee of Astellas. TP is a paid consultant for Incyte, has received consultancy fees and research funding from Astellas, AstraZeneca, Bristol Myers Squibb, Eisai, EMD Serono, Exelixis, Roche, Incyte, Ipsen Biopharm Limited, Johnson & Johnson, Mash Up Ltd, Merck, MSD, Novartis, Pfizer, and Seagen; and has received travel costs from AstraZeneca, Roche, Ipsen Biopharmaceuticals, MSD, and Pfizer. The authors report no other conflicts of interest in this work.
References
1. National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology (NCCN Guidelines): Bladder Cancer. National Comprehensive Cancer Network; 2022. Available from: https://www.nccn.org/professionals/physician_gls/pdf/bladder.pdf.
2. Powles T, Bellmunt J, Comperat E, et al. Bladder cancer: ESMO clinical practice guideline for diagnosis, treatment and follow-up. Ann Oncol. 2022;33(3):244–258. doi:10.1016/j.annonc.2021.11.012
3. Bloudek L, Hepp Z, McKay C, et al. Systematic literature review (SLR) and network meta-analysis (NMA) of first-line therapies (1L) for locally advanced/metastatic urothelial carcinoma (la/mUC). J Clin Oncol. 2022;40(suppl 6):570. doi:10.1200/JCO.2022.40.6_suppl.570
4. Powles T, Park SH, Voog E, et al. Avelumab first-line (1L) maintenance for advanced urothelial carcinoma (UC): long-term follow-up results from the JAVELIN bladder 100 trial. J Clin Oncol. 2022;40(suppl 6):487. doi:10.1200/JCO.2022.40.6_suppl.487
5. Food and Drug Administration. Successes and Opportunities in Modeling and Simulation for FDA. Food and Drug Administration; 2022.
6. Viscardi G, Tralongo AC, Massari F, et al. Comparative assessment of early mortality risk upon immune checkpoint inhibitors alone or in combination with other agents across solid malignancies: a systematic review and meta-analysis. Eur J Cancer. 2022;177:175–185. doi:10.1016/j.ejca.2022.09.031
7. Mollica V, Rizzo A, Montironi R, et al. Current strategies and novel therapeutic approaches for metastatic urothelial carcinoma. Cancers. 2020;12(6):1449. doi:10.3390/cancers12061449
8. Schwartz N, DeBusk K, Bloudek L, Migliaccio-Walle K, Bloudek B. Estimation of the prevalence of HER2+ metastatic breast cancer in the United States. J Manag Care Pharm. 2021;27(suppl 10b):S1–S119.
9. Bloudek B, Wirtz H, Hepp Z, et al. Oncology simulation model: a comprehensive and innovative approach to estimate and project prevalence and survival in oncology. Clin Epidemiol. 2022;14:1375–1386. doi:10.2147/CLEP.S377093
10. Phillips T, Migliaccio-Walle K, Yu KS, et al. An oncology simulation model to estimate 10-year progression-free survival and stem cell transplantation for frontline, stage III or IV classical Hodgkin lymphoma based on the 5-year update of the ECHELON-1 trial: a United States perspective. Blood. 2021;138(suppl 1):2440. doi:10.1182/blood-2021-147308
11. Phillips TJ, Liu N, Bloudek B, Migliaccio-Walle K, Reynolds J, Burke JM. 10-year impact on productivity costs associated with mortality in stage III or IV classical Hodgkin lymphoma based on the overall survival update of the ECHELON-1 trial: application of an oncology simulation model in the United States. Blood. 2022;140(suppl 1):10791–10792. doi:10.1182/blood-2022-162573
12. Burke JM, Yu KS, Mordi U, et al. An oncology simulation model to estimate 10-year progression-free survival and overall survival based on the 5-year update from the ECHELON-2 trial in frontline patients with peripheral T-cell lymphoma: a United States perspective. Blood. 2021;138(suppl 1):2466. doi:10.1182/blood-2021-148004
13. Powles T, Csőszi T, Özgüroğlu M, et al. Pembrolizumab alone or combined with chemotherapy versus chemotherapy as first-line therapy for advanced urothelial carcinoma (KEYNOTE-361): a randomised, open-label, phase 3 trial. Lancet Oncol. 2021;22(7):931–945. doi:10.1016/S1470-2045(21)00152-2
14. Powles T, Park SH, Voog E, et al. Avelumab maintenance therapy for advanced or metastatic urothelial carcinoma. N Engl J Med. 2020;383(13):1218–1230. doi:10.1056/NEJMoa2002788
15. Galsky MD, Arija JÁA, Bamias A, et al. Atezolizumab with or without chemotherapy in metastatic urothelial cancer (IMvigor130): a multicentre, randomised, placebo-controlled phase 3 trial. Lancet. 2020;395(10236):1547–1557. doi:10.1016/S0140-6736(20)30230-0
16. Morgans A, Powles T, Shih V, et al. C27. Real-World Avelumab Maintenance Eligibility and Treatment Patterns in Cisplatin-Ineligible Patients with Locally Advanced or Metastatic Urothelial Carcinoma. San Antonio, Texas, United States: JMCP; 2023.
17. Powles T, van der Heijden M, Castellano D, et al. Durvalumab alone and durvalumab plus tremelimumab versus chemotherapy in previously untreated patients with unresectable, locally advanced or metastatic urothelial carcinoma (DANUBE): a randomised, open-label, multicentre, phase 3 trial. Lancet Oncol. 2020;21(12):1574–1588. doi:10.1016/S1470-2045(20)30541-6
18. Galsky MD, Sonpavde GP, Bloudek B, et al. Simulating the Impact of First-Line Treatment Choice on Survival Among Patients with Locally Advanced/Metastatic Urothelial Carcinoma Considered Cisplatin Ineligible. Boston, United States: ISPOR; 2023.
19. García-Donas J, Font A, Pérez-Valderrama B, et al. Maintenance therapy with vinflunine plus best supportive care versus best supportive care alone in patients with advanced urothelial carcinoma with a response after first-line chemotherapy (MAJA; SOGUG 2011/02): a multicentre, randomised, controlled, open-label, phase 2 trial. Lancet Oncol. 2017;18(5):672–681a. doi:10.1016/S1470-2045(17)30242-5
20. Galsky MD, Mortazavi A, Milowsky MI, et al. Randomized double-blind Phase II study of maintenance pembrolizumab versus placebo after first-line chemotherapy in patients with metastatic urothelial cancer. J Clin Oncol. 2020;38(16):1797–1806. doi:10.1200/JCO.19.03091
21. Bloudek L, Campbell D, Pandey R, Migliaccio-Walle K, Bloudek B, Devine B. MSR33 application and feasibility of indirect treatment comparison of switch maintenance and non-maintenance oncology regimens to inform HTA decision-making. Value Health. 2022;25(12):S356. doi:10.1016/j.jval.2022.09.1765
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
