Back to Journals » Infection and Drug Resistance » Volume 11
Benchmarking for surgical site infections among gastrointestinal surgeries and related risk factors: multicenter study in Kuwait
Authors Hamza WS , Salama MF, Morsi SS , Abdo NM, Al-Fadhli MA
Received 4 March 2018
Accepted for publication 17 June 2018
Published 3 September 2018 Volume 2018:11 Pages 1373—1381
DOI https://doi.org/10.2147/IDR.S167213
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Eric Nulens
Wafaa S Hamza,1,2 Mona F Salama,1,3 Samar S Morsi,1,4 Naglaa M Abdo,1,5 Mariam A Al-Fadhli1
1Infection Control Directorate, Ministry of Health, Kuwait City, Kuwait; 2Department of Public Health and Community Medicine, Faculty of Medicine, Assiut University, Assiut, Egypt; 3Department of Microbiology and Medical Immunology, Faculty of Medicine, Mansoura University, Mansoura, Egypt; 4Department of Microbiology and Immunology, Faculty of Medicine, Zagazig University, Zagazig, Egypt; 5Department of Community, Environmental and Occupational Medicine, Faculty of Medicine, Zagazig University, Zagazig, Egypt
Purpose: To measure surgical site infection (SSI) rates among gastrointestinal surgeries and to identify the associated risk factors.
Patients and methods: We conducted a multicenter, retrospective, surveillance-based study of adults undergoing gastric, colon, and small bowel (SB) procedures from January to December 2016. Univariate and multivariate analyses were conducted to determine the predictive variables in each surgery.
Results: In total, 71 of 2,099 patients developed SSI – 0.8%, 19.8%, and 10.8% following gastric, colon, and SB surgeries, respectively. In gastric surgery, the risk factors identified by univariate analysis were age, duration, wound class, risk index, emergency, and scope use (P<0.05). Logistic regression analysis revealed that the laparoscopic approach was the only significant predictor, with an inverse relationship of SSI rate vs open gastric surgery (P<0.05). Prolonged duration was a significant risk factor for developing SSI in colon surgery, and emergency was a significant risk for development of SSI in SB surgery. Gram-negative bacilli were the main causative pathogens, with a high percentage of multidrug-resistant organisms.
Conclusion: Variances in SSI rates and risk factors among gastric, colon, and SB surgery were detected. The use of an endoscope in gastric surgeries exhibited a protective effect against the development of SSI. The reduction of the SSI rate can be achieved by targeted preventive interventions for the identified risk factors.
Keywords: surveillance, health care-associated infections, laparoscope, gastric surgery, Gram-negative bacilli, post-discharge surveillance
Introduction
Surgical site infections (SSIs) are the most common type of health care-associated infections (HAIs) in patients undergoing surgery and remain a major source of postoperative morbidity. Among surgical patients, SSIs account for 38% of HAIs.1 Among patients undergoing gastrointestinal (GI) surgeries, 12.2% develop SSIs,2 which result in prolonged hospitalization, increased morbidity and mortality, and increased surgery-related costs. Therefore, to reduce SSI, it is important to investigate risk factors, and these have been well studied in various types of GI surgeries, particularly colorectal surgery.1 Epidemiological studies have identified risk factors as well as protective factors for SSIs including, but not limited to, demographic factors, preoperative preparation, and laparoscopic procedures.2
Surveillance of SSIs should be a priority for infection-control programs, and SSI surveillance has been implemented in Kuwait as part of the Kuwait National Healthcare-associated Infections Surveillance System (KNHSS) which adopted the guidelines issued by the National Health Safety Network (NHSN) that are updated regularly. The SSI surveillance system specifies operative procedures for each governmental hospital, including the GI procedures – namely, colon (COLO), gastric (GAST), and small bowel (SB) surgeries. This study aimed to measure SSI rates among the selected GI surgeries and to identify the associated potential risk factors.
Patients and methods
Setting and design
A descriptive, retrospective, multicenter study of the collected GI-SSI surveillance from all governmental hospitals in all health regions in Kuwait was conducted. The bed capacity of participating hospitals ranged from 400 to 900 beds. All adult patients who underwent the selected GI surgeries from January to December 2016 in all Kuwait governmental hospitals were evaluated in this study.
Data collection
The Kuwait Infection Control Directorate had assigned select GI surgeries – COLO, GAST, and SB – for inclusion under the KNHSS. These assignments were based on previously analyzed SSI rates at each hospital. Data for the current study were retrieved from the SSI forms (denominator, nominator, and post-discharge forms) for the selected GI procedures. During the surveillance period, all operated patients were prospectively and actively monitored for signs of SSI for 1 month through the KNHSS. The surgical denominator form was filled for each procedure in all governmental hospitals by trained infection-control staff. This denominator form included: patient name, gender, nationality, hospital file number, procedure name, code, date and duration, wound class, American Society for Anesthesiologists (ASA) score, scope use, emergency or non-emergency, and the SSI Risk Index category. SSI was diagnosed during the primary patient hospitalization, after discharge, or re-hospitalization by using the following methods.
Ante-discharge surveillance method
This method was used for the diagnosis of postoperative SSI during the primary patient hospitalization. For patients who developed SSIs, a numerator form was filled that included: patient name, gender, nationality, hospital file number, procedure name, code, date of procedure and infection event, SSI category, SSI signs, symptoms, laboratory diagnosis, physician diagnosis, pathogen identified, pathogen susceptibility, occurrence of secondary bloodstream infection, and patient outcome (death or discharge).
Post-discharge surveillance method
The post-discharge surveillance method was used for the diagnosis of SSIs after patient discharge or at readmission. The post-discharge surveillance form was filled for patients who presented with SSI to outpatient clinics in primary health care or any governmental hospital. This post-discharge surveillance form included the name of the hospital where the operation was done and the reporting facility in addition to patients’ demographic data. For those diagnosed after discharge or readmission, the previously described nominator form was additionally filled.
The state of Kuwait is divided into six health regions and according to the residential address of people seeking medical care in each health region. Self-treatment is very difficult; all patients visit the primary health care or health regions hospitals to receive antibiotics (if needed) as there are no over-the-counter medications. Postoperatively and before the patients’ discharge, the staff nurses do the following: educate patients about signs and symptoms of wound infection, schedule each patient for regular wound dressing (follow-up visits), and instruct patients to visit the hospital, even outside of consultation hours, if any signs or symptoms of SSI develop. During the follow-up visits, each patient was examined for signs of SSI and wound dressing done in primary health care or regional hospitals clinics based on the previous written follow-up visits, depending upon appointment and residential address. Infection-control staff actively and periodically follow-up these patients under the post-discharge surveillance method in primary health care and hospitals. Any case that was diagnosed in Kuwait governmental health care facilities after patient discharge was reported, and the complete data were collected (numerator forms were filled).
All the previously described tools (forms) were distributed to all primary health care centers and governmental hospitals. All infection-control and nursing staff in these locations were trained on the use of these previously described methods. All filled forms were collected regularly from all governmental sectors.
Definitions
The criteria used to define SSIs and a patient’s risk index categories were established according to the US Centers for Disease Control and Prevention (CDC) guidelines. SSIs were classified into three groups: superficial, involving skin and subcutaneous tissue; deep, involving muscle and fascia; and organ space.3 According to the NHSN that was adapted from the American College of Surgeons classification, wounds were classified into four classes: clean, clean-contaminated, contaminated, or dirty-infected.4 The NHSN cutoff point (75th percentile) for the duration of the operative procedures was specified in minutes: 187 for COLO, 160 for GAST, and 192 for SB surgeries.5 The ASA score was based on an assessment by the anesthesiologist of the patient’s preoperative physical condition using the ASA classification. The NHSN surgical risk index category was calculated for all operated patients. The NHSN SSI Risk Index ranges from 0 (lowest risk) to 3 (greatest risk),6 and is the sum of a number of risk factors: 1) a patient with an ASA score of 3, 4, or 5; 2) an operative wound classified as contaminated or dirty/infected; and 3) an operation lasting longer than the duration cutoff point. Each risk factor listed was considered as one risk according to the NHSN risk index.6 Patients with SSIs were defined as patients who underwent the selected surgeries during the study period at any of Kuwait’s governmental hospitals and acquired an SSI according to the CDC criteria.
Exclusion criteria
Operated patients for the selected procedures who had undergone nonprimary closure of the wound and developed an infection would not be considered to have an SSI and were excluded from this study according to the KNHSS.4
Ethical considerations
The study protocol was reviewed and approved by the Kuwait Ministry of Health Standing Committee for the Coordination of Health and Medical Research, and patient confidentiality was protected; all data were entered and analyzed anonymously.
Statistical analysis
Data were coded, entered anonymously, and analyzed using SPSS version 19. Qualitative variables were presented as frequency (%); quantitative variables were presented as the median and interquartile range. Chi-squared or Fisher’s exact test were used to compare qualitative variables values, whereas the Mann–Whitney U test was used to compare quantitative variables. SSI rates per 100 operative procedures were calculated for each selected procedure according to the CDC/NHSN, SSI protocol 2013. Binary logistic multivariate regression analysis was conducted for the statistically significant variables identified by the univariate analysis to determine independent predictive factors for the development of SSI. A P-value of <0.05 was considered statistically significant.
Results
Patient characteristics and potential risk factors
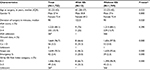
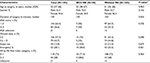
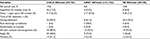
A total of 2,099 patients met the eligibility criteria for GI surgeries: 1,722 GAST, 192 COLO, and 185 SB included in this study. The characteristics and potential risk factors of the study participants are summarized in Tables 1–3.
GAST surgery
Univariate analysis of risk factors showed that the median duration of surgery in the SSI group was longer than in the non-SSI group (122.5 vs 90 minutes, respectively, P=0.02). Moreover, it showed that, in the SSI group, there was a trend toward statistical significance for emergency surgery as well as higher wound class, scope use, and risk index (P<0.001; Table 1). Bariatric surgeries represented 96%, and the scope was used in 96% of these surgeries. Scope use had a protective effect (P≤0.05; results not shown).
COLO surgery
The SSI group had a statistically significant longer median duration of operative time compared to the non-SSI group – 195 vs 150 minutes, respectively (P<0.001; Table 2).
SB surgery
Half of the subjects in the SSI group were emergency cases, with a statistically significant difference between the SSI and non-SSI groups (P=0.02; Table 3).
Characteristics of SSIs
SSIs were noted in 71 patients out of 2,099: 13 patients following GAST surgery (incidence rate 0.8%), 38 patients following COLO surgery (incidence rate 19.8%), and 20 patients following SB surgery (incidence rate 10.8%). The superficial SSI rate vs deep/organ space SSI rate was, respectively, 13.5% and 6.3% in COLO, 0.2% and 0.5% in GAST, and 4.8% and 7.3% in SB surgeries. With regard to the time of diagnosis, the vast majority of patients with SSIs following COLO surgery (94.7%), all SSIs after SB surgery, and 61.5% following GAST surgery were diagnosed during the primary hospital admission. Besides this, the SSI diagnosis was established after hospital discharge consecutively in 38.5% and 5.2% of patients following GAST and COLO surgeries (Table 4). A high percentage of infected wounds following SB and COLO surgeries had multiple microbial infections – 63.2% and 41.2%, respectively – whereas in 75% of infected wounds following GAST surgery a single pathogen was isolated as shown in Table 4. The SSI rate following bariatric surgeries was 0.4% compared with 9.4% among non-bariatrics and 14.3% among cancer stomach surgeries, and the difference between the groups was statistically significant (P<0.001; data not shown).
  | Table 4 Characteristics of surgical site infections of the studied gastrointestinal surgical categories Abbreviations: COLO, colon; GAST, gastric; SB, small bowel; SSI, surgical site infection. |
Logistic regression analysis
Binary logistic multivariate analysis was done using all the significant variables for the SSI group identified in the univariate analysis for GAST surgery. Age at surgery, operative duration, wound class, emergency SSI Risk Index, and laparoscopic approach were dependent factors affecting occurrence of SSI. However, the laparoscopic approach was the only significant predictor with a protective effect against developing SSIs as compared to open GAST surgery (P≤0.05). The overall prediction of the regression model was 26.4% (P<0.001; Table 5).
  | Table 5 Logistic regression analysis of independent risk factors for surgical site infection following gastric surgery |
Causative pathogens
Pathogens associated with SSI were isolated from 91.5% of patient wounds of the studied surgical categories. Among COLO, GAST, and SB SSIs, 41.2%, 25.0%, and 63.2%, respectively, were caused by multiple microbes. Among the pathogens isolated from COLO SSIs, Gram-negative bacilli (GNB) were the main causative pathogen (representing 70% of SSIs), and more than half of these GNB (60.0%) were multidrug-resistant organisms (MDROs) – most (81.1%) being an extended-spectrum β-lactam producer (ESBL). Escherichia coli (46%) and Enterococcus spp. (24%) were the most common isolated pathogen. In GAST-SSI, GNB were the commonest pathogens 43.8%, of which 42.9% were Pseudomonas aeruginosa MDRO. The Candida spp. represented 37.5% of the isolated pathogens. Among the pathogens isolated from SB-SSIs, 64.1% were GNB and 27.7% were Gram-positive cocci and candida. MDROs represented 59.1% of the GNB; of these, 61.5% were ESBL, and E. coli was the most commonly isolated pathogen (25%; Table 6).
Discussion
SSI rates are an indicator of health care quality.7 To our knowledge, this study represents the first attempt in the state of Kuwait to measure SSI rates following COLO, GAST, and SB surgeries and to explore its related risk factors. The potential risk factors for SSI in our patients were assessed. The CDC guidelines specify identification of risk factors for SSIs before operations permits directed preventive strategy.8 Therefore, we believe that investigating the risk factors for GI-SSI could suggest targeted preventive interventions.
SSIs were noted in 71 of 2,099 patients: 38 patients following COLO surgery (incidence rate 19.8%), 13 patients following GAST surgery (incidence rate 0.8%), and 20 patients following SB surgery (incidence rate 10.8%). Among colon surgeries, we identified rates of 13.5% superficial and 6.3% deep/organ space SSIs, which are higher than that the SSI rates reported by Lawson et al (6.2% for superficial and 4.7% for deep/organ space infection).9 However, in another study, the organ space SSI rate was 7.9%, which is higher than the SSI rate in the present study.10 We found that superficial and deep/organ space SSI rates postgastric surgeries were 0.2% and 0.5%, respectively, which were lower than what was reported by other study, with superficial SSI and organ/space SSI rates of 3% and 2%, respectively.11 Another study revealed a rate of 6.1% for superficial SSIs.12 These variances may be attributed to different patient populations with different risk factors in addition to the different risk factors for superficial and deep/organ-space SSIs.9,13
The diagnosis rate of SSI on admission was 100% after SB surgeries and 94.0% following COLO. With the application of post-discharge surveillance, 38% GAST-SSIs and 6% COLO-SSIs were detected during the 30-day follow-up. Different studies have shown that 12%–84% of SSIs are diagnosed after hospital discharge, thereby confirming the importance of post-discharge surveillance in the detection and reporting of SSI rates.14
The observed SSI rate following GAST surgery was 0.8%. This result was lower than those in reports from other studies following GAST surgery, where SSI rates ranged between 1.7% and 4.23%.1,15 We noticed that bariatric surgeries accounted for the majority of GAST surgeries (96%), with an SSI rate of 0.4%. This rate was lower than that reported in other research works; large series of bariatric surgeries have described SSI rates of between 5.8% and 20%.7,16 Furthermore, we recognized that the scope was used in 96% of bariatric surgeries and exhibited a protective effect against the development of SSIs among bariatric surgery patients (P<0.001 results not shown), and this might explain our low rate of SSI.
In the present study, univariate analyses of SSI following GAST surgeries revealed a significant relationship between increased age, longer operative duration, and contaminated or dirty wound class in patients with SSI vs those without SSI; regardless of the differences in methodology and study designs, previous investigators have reported similar associations.1,17 The association between increased age and occurrence of SSIs may be attributed to a decrease in physiological defense mechanisms and immune function.18,19 Surgical wound classification has been recognized as a predictive factor in developing SSIs after surgery, and the incidence of SSI can be expected in patients with a higher surgical wound class.19
The SSI rate in COLO surgeries was the highest among the studied GI surgeries, with an incidence rate of 19.8%. Colorectal surgeries have been associated with the highest risk of SSIs, predominately because of the heavy bacterial load of the colon and rectum.20,21 This finding was in concordance with previous studies in different countries, with SSI rates ranging from 14% to 25%.13,21 On the other hand, the NHSN report displayed lower SSI rates in COLO surgery – between 4% and 9.5%.15
The current study demonstrated that prolonged operation duration, beyond the cutoff point (>median), was a significant predictor for the development of SSIs in COLO surgery, and this association had often been described by other researchers.22–24 The observed association between longer operative duration and development of SSIs among the studied COLO and GAST surgery patients might be attributable to the increased duration of exposure to microorganisms in the operating theater.25,26 Therefore, SSI prevention strategies focusing on longer surgical duration are needed to improve patient outcomes.19 By applying both univariate and multivariate regression analyses, we found that the laparoscopic approach served as an independent protective factor against the development of SSIs in GAST surgery (P=0.001). This finding was described in previous research work where scope use significantly reduced SSI rates.7,27,28 A review of the literature showed scarce research evidence on SSIs following SB surgeries; most researchers had studied SSIs of either the large bowel alone or in combination with SB surgeries.10,29,30 The present study showed that the incidence of SSIs following SB surgery was 10.8%. This rate was higher than the rate in other reports; the NHSN reports SSI rates between 3.5% and 7%.15 A retrospective study identified an SSI rate of 8.7% following SB and large bowel surgeries.31 Conversely, in a meta-analysis, Fiorio et al demonstrated a higher rate of SSIs following SB surgeries (16.3%).32
Our analysis revealed that the incidence of SSIs among emergency SB surgery was higher than in elective surgery (50% vs 25.5%, P=0.021). This finding was concordant with results from other research.28 A possible explanation for the higher incidence of SSIs in emergency surgeries could be attributed to inadequate preoperative preparation, as these surgeries usually take place beyond normal clinical working hours. Therefore, it is of high importance to emphasize the management of emergency surgeries.19
Following COLO, GAST, and SB surgeries, a considerable percentage of poly-microbes were isolated. GNB were the most common isolated pathogens, and this finding was comparable with other researches.33,34 However, other previous studies showed a higher proportion of Gram-positive organisms, which are associated with SSIs in different countries.35,36 Staphylococcus aureus, coagulase-negative Staphylococcus, and E. coli were the most common organisms associated with SSI according to a recent report by the NHSN.37 Moreover, MDROs accounted for a high proportion of the isolated GNB, especially ESBL-producing organisms, following COLO and SB surgeries among our patients. A high proportion of methicillin-resistant S. aureus and carbapenem-resistant Acinetobacter baumannii isolates were identified in a study of SSIs in large teaching hospital in Southern Italy.38 The diversity of the study population and the different antimicrobial use could be the reason for identifying a different pattern of bacterial isolates in different study settings. The majority of GNB identified in our SSI patients were possibly due to the predominance of Gram-negative isolates from SSIs following intra-abdominal procedures.39 Our findings highlight the importance of knowing the local epidemiology of antibiotic resistance to facilitate proper selection of prophylactic and therapeutic antibiotics, with subsequent optimization of the outcomes and reduction of the length of hospital stay.40
Strengths and limitations
Among the strengths of the study are its multi-centric design and the fact that all data were collected by trained infection-control staff. However, the study has limitations that should be admitted. There are certain risk factors that have been linked to SSIs that are not limited to perioperative hyperglycemia, hypothermia, and comorbidities were not recorded in this study. Due to the small number of SB and COLO surgeries, their SSI rates cannot be generalized and further studies are needed.
Conclusion
Variances in SSI rates and risk factors among gastric, colon, and SB surgeries were detected. The use of an endoscope in gastric surgeries exhibited a protective effect against the development of SSIs. The reduction of the SSI rate can be achieved by targeted preventive interventions for the identified risk factors.
Disclosure
The authors report no conflicts of interest in this work.
References
Jeong SJ, Ann HW, Kim JK, et al. Incidence and risk factors for surgical site infection after gastric surgery: a multicenter prospective cohort study. Infect Chemother. 2013;45(4):422–430. | ||
Utsumi M, Shimizu J, Miyamoto A, et al. Age as an independent risk factor for surgical site infections in a large gastrointestinal surgery cohort in Japan. J Hosp Infect. 2010;75(3):183–187. | ||
National Healthcare Safety Network. Surgical Site Infection (SSI) Event. Centers for Disease Control and Prevention; Atlanta 2013. Available from: http://www.cdc.gov/nhsn/PDFs/pscManual/ 9psc SSI current.PDF. Accessed May, 2013. | ||
Surgical site infection (SSI) event. Available from: www.icdkwt.com/surveillance_out/ssi/KNHSSSSIprotocol2013.pdf. Accessed January 2017. | ||
NNIS System. National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2003, issued August 2003. Am J Infect Control. 2003;31(8):481–498. | ||
Culver DH, Horan TC, Gaynes RP, et al. Surgical wound infection rates by wound class, operative procedure, and patient risk index. Am J Med. 1991;91(3):S152–S157. | ||
Nguyen NT, Goldman C, Rosenquist CJ, Wolfe BM, et al. Laparoscopic versus open gastric bypass: a randomized study of outcomes, quality of life, and costs. Ann Surg. 2001;234(3):279–291. | ||
Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol. 1999;20(4):250–278. | ||
Lawson EH, Hall BL, Ko CY, Cy K. Risk factors for superficial vs deep/organ-space surgical site infections: implications for quality improvement initiatives. JAMA Surg. 2013;148(9):1–10. | ||
Gomila A, Carratalà J, Camprubí D, et al. Risk factors and outcomes of organ-space surgical site infections after elective colon and rectal surgery. Antimicrob Resist Infect Control. 2017;6:40. | ||
Tang R, Chen HH, Wang YL, et al. Risk factors for surgical site infection after elective resection of the colon and rectum: a single-center prospective study of 2,809 consecutive patients. Ann Surg. 2001;234(2):181–189. | ||
. Shunji Endo, ToshimasaTsujinaka, Kazumasa Fujitani, Junya Fujita, Shigeyuki Tamura, Makoto Yamasaki, et al. Risk factors for superficial incisional surgical site infection after gastrectomy: analysis of patients enrolled in a prospective randomized trial comparing skin closure methods. Gastric Cancer. 2016;19:639–644. | ||
Smith RL, Bohl JK, Mcelearney ST, et al. Wound infection after elective colorectal resection. Ann Surg. 2004;239(5):599–607. | ||
de Oliveira AC, Carvalho DV. Evaluation of underreported surgical site infection evidenced by post-discharge surveillance. Rev Lat Am Enfermagem. 2007;15(5):992–997. | ||
Edwards JR, Peterson KD, Yi Mu BBA, et al. National Healthcare Safety Network (NHSN) report: Data summary for 2006 through 2008, issued December 2009 Atlanta, Georgia Published by the Association for Professionals in Infection Control and Epidemiology. Am J Infect Control. 2009(37):783–805. | ||
Christou NV, Jarand J, Sylvestre JL, Mclean AP. Analysis of the incidence and risk factors for wound infections in open bariatric surgery. Obes Surg. 2004;14(1):16–22. | ||
Scott JD, Forrest A, Feuerstein S, Fitzpatrick P, Schentag JJ. Factors associated with postoperative infection. Infect Control Hosp Epidemiol. 2001;22(6):347–351. | ||
Kaye KS, Schmit K, Pieper C, et al. The effect of increasing age on the risk of surgical site infection. J Infect Dis. 2005;191(7):1056–1062. | ||
Cheng K, Li J, Kong Q, Wang C, Ye N, Xia G. Risk factors for surgical site infection in a teaching hospital: a prospective study of 1,138 patients. Patient Prefer Adherence. 2015;9:1171–1177. | ||
National Nosocomial Infections Surveillance System, National Nosocomial Infections Surveillance (NNIS) System Report, data summary from January 1992 through June 2004, issued October 2004. Am J Infect Control. 2004;32(8):470–485. | ||
Ishikawa K, Kusumi T, Hosokawa M, Nishida Y, Sumikawa S, Furukawa H. Incisional surgical site infection after elective open surgery for colorectal cancer. Int J Surg Oncol. 2014;2014:1–5. | ||
Hübner M, Diana M, Zanetti G, Eisenring MC, Demartines N, Troillet N. Surgical site infections in colon surgery: the patient, the procedure, the hospital, and the surgeon. Arch Surg. 2011;146(11):1240–1245. | ||
Young H, Knepper B, Moore EE, Johnson JL, Mehler P, Price CS. Surgical site infection after colon surgery: National Healthcare Safety Network risk factors and modeled rates compared with published risk factors and rates. J Am Coll Surg. 2012;214(5):852–859. | ||
Watanabe M, Suzuki H, Nomura S, et al. Performance assessment of the risk index category for surgical site infection after colorectal surgery. Surg Infect. 2015;16(1):84–89. | ||
Leong G, Wilson J, Charlett A. Duration of operation as a risk factor for surgical site infection: comparison of English and US data. J Hosp Infect. 2006;63(3):255–262. | ||
Ercole FF, Starling CE, Chianca TC, Carneiro M. Applicability of the national nosocomial infections surveillance system risk index for the prediction of surgical site infections: a review. Braz J Infect Dis. 2007;11(1):134–141. | ||
Imai E, Ueda M, Kanao K, et al. Surgical site infection risk factors identified by multivariate analysis for patient undergoing laparoscopic, open colon, and gastric surgery. Am J Infect Control. 2008;36(10):727–731. | ||
Sanabria A, Vega V, Dominguez LC, Espitia E, Serna A, Osorio C. The evolution of laparoscopy in abdominal surgery: a meta-analysis of the effect on infectious outcomes. Minim Invasive Ther Allied Technol. 2014;23(2):74–86. | ||
Fry DE, Fry Donald E. The prevention of surgical site infection in elective colon surgery. Scientifica. 2013;2013:1–19. | ||
Suzimar de Fátima Benato Fusco, NatiaraMedolagoMassarico, Maria Virginia Martins FariaFadul Alves, Carlos Magno Castelo Branco Fortaleza, ÉrikaCibele Pereira Pavan, Valéria de Castilho Palhares, et al. Surgical site infection and its risk factors in colon surgeries. J School Nurs. 2016;50(1):43–49. | ||
Walz JM, Paterson CA, Seligowski JM, Heard SO. Surgical site infection following bowel surgery: a retrospective analysis of 1446 patients. Arch Surg. 2006;141(10):1014–1018. | ||
Fiorio M, Marvaso A, Viganò F, Marchetti F. Incidence of surgical site infections in general surgery in Italy. Infection. 2006;34(6):310–314. | ||
Agelaw Sgebres, Tiruneh M, Fentie M. “Antimicrobial susceptibility patterns of bacterial isolates from patients with postoperative surgical site infection, health professionals and environmental samples at a tertiary level hospital, North West Ethiopia,”. Int J Pharm Sci Rev Res. 2013;3(1):1–9. | ||
Dessie W, Gebrumulugeta, Surafael Fentaw A. MuluHassen, and EngidaAbebe.Pattern of Bacterial Pathogens and Their Susceptibility Isolated fromSurgical Site Infections at Selected Referral Hospitals, Addis Ababa, Ethiopia. Int J Microbiol. 2016;2016:1–8. | ||
LopisoDessalegn, TechalewShimelis, EndaleTadesse, Solomon Gebre-selassie. Aerobic bacterial isolates from post-surgical wound and their antimicrobial susceptibility pattern: a hospital based cross-sectional study. J Med Res. 2014;3(2):18–23. | ||
Getachew Seyoum Asres. Melese Hailu Legese and Gebru Mulugeta Woldearegay. Prevalence of Multidrug Resistant Bacteria in Postoperative Wound Infections at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia. Arch Med. 2017;9(4):12. | ||
National Nosocomial Infections Surveillance (NNIS) System, “National Nosocomial Infections Surveillance (NNIS) report, data summary from October 1986–April 1996, issued May 1996,”. Am J Infect Control. 1996;24(5):380–388. | ||
Esposito S, Gioia R, de Simone G, et al. Bacterial Epidemiology and Antimicrobial Resistance in the Surgery Wards of a Large Teaching Hospital in Southern Italy. Mediterr J Hematol Infect Dis. 2015;7(1):1. | ||
Bibi S, Channa GA, Siddiqui TR, Ahmed W. “Pattern of bacterial pathogens in postoperative wounds and their sensitivity patterns in Karachi, Pakistan,”. J Surg Pakistan. 2012;17(4):164–167. | ||
Camporese A, Santini G. Surveillance of antibiotic-resistant microorganisms for the rational use of antimicrobial drugs. Infez Med. 1999;7(3):172–176. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.