Back to Journals » Infection and Drug Resistance » Volume 16
Barriers and Intention to Get Vaccinated for COVID-19 and Associated Factors Among Adults in Southwest Ethiopia: A Theory of Planned Behavior Approach
Authors Sisay AL , Getahun HA , Getachew N , Gebremedhin T , Sebero FM , Birhanu A , Gizaw AT
Received 19 May 2023
Accepted for publication 22 August 2023
Published 31 August 2023 Volume 2023:16 Pages 5741—5754
DOI https://doi.org/10.2147/IDR.S419952
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Assefa Legesse Sisay,1 Habtamu Abebe Getahun,1 Nigusu Getachew,2 Tadesse Gebremedhin,1 Feyissa Mama Sebero,3 Addis Birhanu,1 Abraham Tamirat Gizaw4
1Department of Epidemiology, Faculty of Public Health, Institute of Health, Jimma University, Jimma, Ethiopia; 2Department of Health Policy and Management, Faculty of Public Health, Institute of Health, Jimma University, Jimma, Ethiopia; 3Jimma Emergency Operation Center, Jimma University, Jimma, Ethiopia; 4Department of Health, Behavior and Society, Faculty of Public Health, Institute of Health, Jimma University, Jimma, Ethiopia
Correspondence: Assefa Legesse Sisay, Email [email protected]; [email protected]
Background: Different vaccines have been approved for use against coronavirus disease and distributed globally in different regions. Efforts should be made on the vaccination to control the spread and impacts of the coronavirus pandemic. However, the general population’s attitudes and intention to uptake coronavirus disease 2019 (COVID-19) vaccinations were poor.
Objective: This study aimed to assess the barriers to and intention to be vaccinated against COVID-19 and the associated factors among adults in the Jimma zone, Ethiopia.
Methods: A community-based cross-sectional study with multistage sampling was conducted with 621 participants from 16 April to 17 May 2022. Multivariable logistic regression was used to identify factors associated with the outcome of interest. Statistical p-value ≤ 0.05 was set at p ≤ 0.05. Qualitative data were supplemented with quantitative results.
Results: The majority of the study participants (382 [61.5%]) intended to uptake the COVID-19 vaccine. In this study, travel history (Adjusted Odds Ratio (AOR) = 2.18, 95% CI 1.23– 3.87), vaccination history (AOR = 2.64, 95% CI 1.69– 4.12), perceptions of infection prevention for COVID-19 (AOR = 1.97, 95% CI 1.28– 3.03), subjective norm (AOR = 2.27, 95% CI 1.52– 3.39), and perceived behavioral control (PBC) (AOR = 2.30, 95% CI 1.55– 3.41) were significantly associated with the intention to be vaccinated against COVID-19.
Conclusion: More than half of the adult participants intended to be vaccinated against COVID-19. The study participant’s traveling history, vaccination history, perception of infection prevention for COVID-19, subjective norms, and Perceived Behavioral Control were significantly associated with the intention to be vaccinated.
Keywords: barrier, COVID-19 vaccine, intention, theory of planned behavior, vaccine acceptance, Ethiopia
Background
The coronavirus disease 2019 (COVID-19) has become a pandemic and is a topic of high public health priority.1 The pandemic spread to many countries, affecting more than 13 countries in one day.2 The International Monetary Fund estimated that the world might lose 5.2 trillion dollars by 2026 if COVID-19 continues to spread.3
As it is known that the virus has no curative approach, the government has developed a vaccine for the community. It has started providing it to high-risk and elderly individuals. The World Health Organization planned to vaccinate 10%, 40%, and 70% of the population by the end of September 2021, December 2021, and June 2022, respectively. Based on this strategy the first two dates by the end of 2021 were not implemented by 56 countries. This underachievement required a rapid strategy to achieve the midyear of the 2022 plan. According to the Statistics and Research Coronavirus (COVID-19) Vaccinations report of 13 November 2021, only 3.11% (1.18% were fully vaccinated and 1.19% were partly vaccinated) of the target population in Ethiopia had been vaccinated. If this trend continues, the world could not achieve its goal by mid-2022 (June 2022).3
A study conducted in north-central Ethiopia revealed that knowledge, attitudes, and practices toward COVID-19 prevention were poor. In this study, less than one-third of the participants reported that avoidance of outdoor activities, social distancing, and wearing masks were not implemented. Common perceived barriers to vaccine uptake are lack of training, lack of policy, and less commitment to infection control.4
Awareness and knowledge of COVID-19 prevention practices are high worldwide; however, their attitudes and perceptions are poor. A study conducted on adults in Canada showed that willingness to take up the vaccine was significantly associated with sex and educational status. A study conducted among medical students in Egypt revealed that perceived adverse effects of the vaccine were the most common reasons for vaccine hesitancy.5
Based on studies conducted in different countries, the intent to be vaccinated in developing countries is not optimal when considering the severity of the infection. Evidence from low-income countries revealed that 46% of participants did not intend to take up the vaccine, and close to half of the study subjects were unsure (33%) or not interested (21%) in being vaccinated.6 As much evidence has shown, the vaccine is effective, and among all deaths reported in Ethiopia, only one percent of vaccinated individuals die of the disease. This result showed that the vaccine was sufficiently effective to save the lives of people. A systematic review reported that the vaccine intensity ranged from 27.7% (Congo) to 91.3% (China).7 Despite the importance of the vaccine, its uptake is very low; research conducted in Dessie specialized hospitals among chronic disease patients reported that approximately 60% were willing to take the vaccine. Possible factors that affect the acceptance of the vaccine have also been studied, including age, educational status, gender, income, residency, attitude towards vaccine, perceived benefit of vaccine, perceived vaccine barriers, self-efficacy, tested for COVID-19 in the past, mandatory COVID-19 vaccination, perceived potential vaccine harm, perceived severity of COVID-19, perceived effectiveness of COVID-19 vaccine, presence of chronic disease, working in healthcare settings, and receiving any vaccine in the past 5 years were associated with the willingness to accept a COVID-19 vaccine.1,6–9
Moreover, an approach to behavioral studies using a theory is a possible solution for exploring determinants of different public health protective and professional behaviors. Theory-based studies provide a better understanding of health-related behaviors, and theory-based interventions are more effective in practice.7,9 Hence, the two prominent theoretical frameworks (theory of planned behavior (TPB) and health belief models (HBM)) are essential tools for understanding the factors behind decision-making by assessing what motivates and initiates people to adopt health-related behavior. HBM is one of the most widely used models for examining the relationship between health behavior and the use of health services. It was developed in the 1950s by social psychologists at the US Public Health Service.10 The second approach TPB suggests that an individual’s behavior can be predicted by his or her behavioral intention. A few recent studies have combined the TPB and HBM approaches to identify health-related behaviors and intentions to receive the influenza vaccine among the general public.11,12 Several studies also have applied HBM and/or TPB to explain COVID-19 vaccination intentions. A study conducted in Malaysian used components of the HBM (perceived susceptibility, severity, benefits, and barriers) to explain the intention to get vaccinated for the COVID-19 vaccine.13
According to the TPB model, the intention to get an influenza vaccination depends on several predictors, including the attitude towards the vaccine, subjective norms for carrying out vaccination, and perception of behavioral control (PBC) of vaccination. Self-efficacy for vaccination is another predictor that was added to the original model, as it has been proven that a distinction must be made between the perception of control of behavior and self-efficacy. Self-efficacy was found to be the most important predictor of health behavioral intention.14,15 As many studies showed that, the efficiency in explaining vaccination uptake for influenza and HIV, the TPB has been successfully used for predicting intentions to uptake COVID-19 vaccination.11,16 A recent study revealed that individuals who had a more positive attitude toward vaccination uptake, scored higher on subjective norms and self-efficacy had higher willingness to uptake vaccination against COVID-19.17,18 The study done in Shenzhen, China, showed that parents’ positive attitudes, perceived family members’ supporting COVID-19 vaccination for children, and perceived behavioral control (PBC) of having the children uptake COVID-19 vaccination were associated with higher parental acceptability of COVID-19 vaccination for children.19 These two general health behavioral theories play a crucial role to examine the intention to get vaccinated for the COVID-19 vaccine.
Previous studies on COVID-19 vaccine barriers have almost all focused on cross-sectional quantitative studies on chronic patients and healthcare workers; however, the current study explored the major barriers by using quantitative studies supplemented with qualitative data for adults, which are the most productive age groups. To the best of our knowledge, this study has not been conducted so far for such productive age group individuals in this area; this might be crucial for policymakers and resource allocators and might be very important for researchers as a baseline. Therefore, this study aimed to assess the barriers and intention to be vaccinated and the associated factors for COVID-19 vaccines among Jimma zone adults based on the TPB.
Methods
Study Design, Study Setting, and Period
A community-based cross-sectional study was conducted from 16 April to 17 May 2022, in seven randomly selected districts of the Jimma zone in southwest Ethiopia. The Jimma zone is one of the Oromia zones, 356 km southwest of Addis Ababa, the capital city of Ethiopia. According to 2017 projected population census, Jimma Zone had an estimated population of 3,261,371, of which 49.9% were women.20 There are 21 districts with 561 Kebeles in the Jimma zone. Population: All adults aged 18 years and older who had lived in the study area for at least six months were considered the source population, and all adults in the zone that met the selection criteria were considered the study population.
Eligibility Criteria
Adults who were seriously ill, unable to respond to the interview, and stayed in the kebele for less than 6 months were excluded.
Sample Size Determination and Sampling Procedures
Sample Size Determination
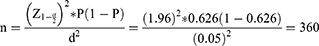
The sample size was determined using a single population formula by assuming a 95% confidence interval with an estimated prevalence of 62.6% for intention to accept the COVID-19 vaccine from a study conducted in Gurage zone,21 and a 5% level of precision. The formula for calculating the sample size (n) is as follows:
By adding a 15% nonresponse rate and 1.5 design effects, the final sample size was 621.
To supplement the key informants’ perceptions, thoughts, and opinions; an in-depth interview was conducted with the community leaders and Religious leaders. One community leader from each selected district and two religious leaders from the zone were purposively selected and interviewed. Overall, for the in-depth interview, nine key informants were considered.
Sampling Procedures
The study participants were recruited using a multistage sampling technique. From the 21 Jimma zone districts, seven (30%) of the districts were randomly selected using simple random sampling (SRS) technique and, from each selected district, 30% of the kebeles were randomly selected using SRS. Then, the total number of households was determined from the family folders of health extension workers for each selected kebeles, and the sample was distributed in proportion to the kebeles. Individual households were identified using systematic random sampling. After the total number of households was determined, the interval “K” was calculated for each selected kebeles. Random start/the first household was selected by lottery method and then the study participants were selected by every Kth interval.
For the qualitative data, seven (one community leader from each selected district) and two religious leaders from the Zone were recruited purposively. Totally, nine key informants were considered for the in-depth interview.
Study Variables
The dependent variable was the intention to uptake COVID-19 vaccines and the independent variables were sociodemographic (sex, age, level of education, marital status, religion, occupation, residence, having family and travel history), health-related (overweight, allergy status, smoking status, …), knowledge-related (included five items with yes/no responses), preventive behavior-related (eg, I put on a facemask persistently each time I go out to my home and other preventive related items was included), and theory of planned behavior (TPB)(Attitude, Subjective norms, perceived behavioral control (PBC) and Self-efficacy), and health belief model (Perceived susceptibility, Perceived benefits, Perceived barriers and Cues to action) construct-related variables.
Measurements and Operational Definitions
Intention to get vaccinated with the COVID-19 vaccine: This is defined as the intention to take the COVID-19 vaccine. Accordingly, participants who responded “willing” and “definitely willing” were recorded as having the intention to get vaccinated, and responses of being “unwilling” and “definitely unwilling” were defined as not intending to get vaccinated.22
Knowledge about COVID-19 vaccine: Participants who scored above the mean (2.91) on the five knowledge assessment questions.22
Attitude towards the COVID-19 vaccine: This was assessed using six attitude-related questions with a 5-point Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree). In summary, respondents who scored greater than or equal to the mean value of the sum of the attitude-related questions were categorized as having a favorable attitude, and those who scored less than the mean value of the sum of the items were categorized as having an unfavorable attitude. Similarly, the TPB dimension variables were categorized in the same manner as attitude.23
Data Collection Tools and Procedure
Structured data collection tools were used for quantitative data collection. The data was collected by an interviewer-administered face-to-face interview method using a self-administered, structured questionnaire adapted from the WHO COVID-19 Prevention and Control Guidelines and from different related literature.24–26 Data collectors and supervisors were trained for two days on detailed information about the questionnaire and data collection procedures. The quantitative data collection tools included sociodemographic variables, health-related variables, knowledge related to COVID-19 vaccines (five items), and constructs of the health belief model (HBM) (12 items) and TPB (16 items). The qualitative data collection tool included 11 interview questions and an in-depth interview was conducted by the trained qualitative data collectors.
Data Quality Control
To ensure data quality, a high emphasis was placed on designing the data collection tool. Structured questionnaire tools were prepared in English and translated into the local language, Afan Oromo, for ease of understanding. Before data collection, pretesting was performed on 5% of the total sample from adjacent districts, and the necessary adjustments were made. Two days of training were provided to the data collectors and supervisors during the data-collection process. Daily meetings were held between data collectors, supervisors, and chief authors to discuss potential issues and assess the progress of the data collection. Before the main data collection, the reliability of the tools for the constructs in the HBM and TPB was assessed, and the overall Cronbach’s alpha coefficients were 0.75 and 0.80 respectively.
Data Processing and Analysis
Collected data were checked for completeness and consistency. The data were entered into a computer using EpiData Manager and exported to STATA version 14.2 for statistical analysis. The necessary data processing, exploration, and management were performed prior to the actual data analysis. All variables with a P-value ≤0.050 under bivariate analysis were considered candidates for multivariable hierarchical logistic regression analysis to control for possible confounding effects. The independent variables are divided into four blocks and entered sequentially using a series of models. Socio-demographics, health-related variables, and knowledge and perceptions of infection prevention variables were entered in Block 1 under model-1. The variables under Block 1 and the HBM dimensions were entered into Block 2 under model-2. Variables nested under model-1 and the TPB dimensions were entered into Block 3 and fitted as model-3. Finally, all candidate variables were entered into Block 4 and nested in model-4. This hierarchical multivariable logistic regression analysis was used to identify factors associated with the intention to be vaccinated against COVID-19 while adjusting for other potential predictors. Adjusted odds ratios and 95% confidence intervals (CI) were used to measure the strength of the associations and their statistical significance, respectively. The goodness-of-fit of the model was assessed using the Hosmer-Lemeshow test of significance. Finally, the qualitative results were supplemented with quantitative results.
Results
Socio-Demographic and Health-Related Characteristics of Study Participants
A total of six hundred twenty-one adults participated in the study, with a response rate of 100%. The average age of the participants was 37.03 years (SD = 12.69 years). The majority, 405 respondents (65.2%), were male. One hundred and ninety-seven (31.7%) of the study participants were not educated. Most, 451 (72.6%) and 508 (81.8%), respondents were married and had family members, respectively. Almost half of the respondents were from rural areas and half were from urban residences. From the health-related characteristics in the current study, 82 (13.2%) respondents had chronic cases and, of the total respondents, 26 (4.2%) were overweight. Most of the respondents, 262 (42.2%), had heard of COVID-19 on the radio (Table 1).
 |
Table 1 Socio-Demographic and Health Related Characteristics of Respondents by Intention to Get Vaccinated for COVID-19 Vaccine Among Adults in Jimma Zone, Ethiopia (n = 621) |
This table also includes the 95% crude odds ratio and corresponding p-values for the univariate analysis. In this univariate analysis, the results of sociodemographic and health-related characteristics, educational status, occupational status, having family members, having a travel history, having ever been vaccinated, and having family members or friends who have died due to COVID were found to be statistically significant with p-values of ≤0.050 (Table 1).
Study Participants’ Prevention Practice, Knowledge, HBM, and TPB Constructs Toward COVID-19 Vaccines
Four hundred and twenty-four (68.3%) study participants had good knowledge of the intention to be vaccinated against COVID-19. Almost half of the study participants had favorable perceived health beliefs (perceived susceptibility, 281 (45.2%); perceived benefits, 359 (57.8%); perceived barriers, 325 (52.3%); and cues to action, 258 (41.5%)). Almost half of the respondents had a positive attitude and 324 (52.2%) had a negative attitude. However, the majority of the study participants (388 [62.5%]) had poor perceptions of infection prevention. Over half, 335 (53.9%), the study participants had a positive subjective norm and 343 (55.2%) had perceived higher control in their behavior, while most, 350 (56.4%), participants had poor self-efficacy.
The univariate analysis results from the last two columns in the table indicate that knowledge about the COVID-19 vaccine and perceptions towards COVID-19 infection prevention, HBM dimensions (perceived susceptibility, perceived benefits, and cues to action), and all TPB constructs (attitude towards COVID-19 vaccines, subjective norms, perceived behavioral control (PBC) and self-efficacy) were significantly associated with the intention to take the COVID-19 vaccine at a p-value of ≤0.050 (Table 2).
 |
Table 2 Study Participants Prevention Practice, Knowledge, HBM and TPB Constructs Towards COVID-19 Vaccine by Intention to Get Vaccinated for COVID-19 Vaccine, Ethiopia (n = 621) |
The majority, 382 (61.5%), of respondents intended to take up the COVID-19 vaccine (Figure 1).
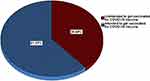 |
Figure 1 Respondents intention towards COVID-19 vaccine among adults in Jimma Zone, Southwest Ethiopia, 2022 (n = 621). |
Multivariable Hierarchical Logistic Regression Analysis of Factors Associated with Intention to Get Vaccinated Against COVID-19
Four nested models were fitted using hierarchical logistic regression analysis. However, the fourth and final models included both the HBM and TPB dimensions, which improved the explained variance compared to the first three models, showing that this model fits better (P-value = 0.614). Under this model, having a travel history (AOR = 2.18, 95% CI 1.23–3.87), having a vaccination history (AOR = 2.64, 95% CI 1.69–4.12), having family or friends who died due to COVID (AOR = 0.15, 95% CI 0.05–0.46), perceptions of infection prevention for Covid-19 (AOR = 1.97, 95% CI 1.28–3.03), and the TPB model constructs (subjective norm (AOR = 2.27, 95% CI 1.52–3.39) and PBC (AOR = 2.30, 95% CI 1.55–3.41)) were significantly associated with the intention to take up the COVID-19 vaccine (Table 3).
 |
Table 3 Hierarchical Logistic Regression Analysis on Intention to Get Vaccinated for COVID-19 Vaccine Among Adults in Jimma Zone, Ethiopia (n = 621) |
As we discovered from the participant’s in-depth interview results in the prevention of the COVID-19 pandemic, most of the respondents exercised prevention methods by wearing masks, proper hand washing with soap and water, rubbing hands with sanitizer and keeping distanced in and outside of the home. As some participants wrote, masks and hand washing were not enough to protect the person from the COVID-19 virus, when he/she appropriately used the protective equipment. A 41-year-old female said, “Initially we practice everything as commanded officially we keep our distance as much as possible. We used mask, avoiding close to each other even in bed, and made the dining in good ventilation during the pandemic time”.
Barriers to Intention to Get Vaccinated for COVID-19
As seen from the quantitative results, the majority of study participants were unsafe or not comfortable with the COVID-19 vaccine (Figure 2).
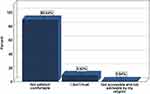 |
Figure 2 Reason for refusing the COVID-19 vaccine among adults in Jimma Zone, Southwest Ethiopia, 2022. |
Challenges to Get the COVID-19 Vaccine
The participants in the in-depth interview stated that the vaccine is important for protecting people from different diseases; however, in the case of the COVID-19 vaccine, many rumors related to the effectiveness of the vaccine were raised, after which the individual was infected by the virus and the vaccine could not protect from the virus completely. The community doubted the safety and effectiveness of the vaccine, and there is ambiguity related to how and from where it comes what ingredient is produced since it is not produced in our country and the like leads the communities to refuse the vaccine.
Some participants commented that they did not believe in the vaccine for some reason, that instead the vaccine is to prepare the world for injected microchips and for the devil. A 42-year-old respondent said that “a religious taken as a spirit of 666 because during the end of the century, devil utilize people for bad things even they talk to get market also need to be a member of the spirit and they implanted chips into hands and to access several information from the person simply without expending any resource”.
Discussion
In the present study, more than half of the participants (61.5%) intended to be vaccinated against COVID-19. The current finding is lower than that of a study conducted at the global level; a study done in the general Israeli adult population (80%), in Australia (85.8%), in the UK (71.7%), in China (87.3%), in Bangladeshi adults (85%), in India (89.3%) and Ghana (83%).27–33 The possible differences could be due to respondent characteristics, awareness, information, attitude differences, and the availability and accessibility of the infrastructure. However, studies conducted in the US were almost equivalent 57.6%, and a study conducted in Indonesia 66.8%.34,35 This finding was smaller than that of a cross-sectional study of diabetic patients at Woldia Comprehensive Specialized Hospital, northern Ethiopia (82.6%) and the community-based study conducted at Hawassa City about COVID-19 vaccine acceptance (73.5%).36,37 This difference might be due to the differences in the health status of the study population. This result is equivalent to that of studies conducted in the Gurage zone of Ethiopia (62.6%), a population-based anonymous online survey in Ethiopia (64.9%), a study conducted on healthcare workers in northeastern Ethiopia (64.0%), a study conducted at Wolkite University among medical and health science students with COVID-19 vaccine hesitancy (58.8%), a study conducted among Adult clients at public hospitals in Eastern Ethiopia using the HBM approach (54.6%), and two separate systematic and meta-analysis studies that pooled the prevalence of vaccine acceptance in Ethiopia (51.2% and 57.8%).8,21,38–42 In contrast, the recent study done in Uganda showed that a majority (66.9%) of the study participants were distrust for COVID-19 vaccination.43
In the current hierarchical logistic regression results, having a primary level of education were less likely to get vaccinated for COVID-19 vaccine as compared to Adults who had no education. A study conducted on mothers’ hesitancy to receive COVID-19 vaccine revealed that mothers’ who had higher education level were more likely to report vaccine hesitancy which support with our study finding.44 Student in occupation, and having family or friends who died due to COVID-19 were negatively associated with the intention to be vaccinated for COVID-19 vaccine. Study participants with a travel history were 2.18 times more likely to be vaccinated against COVID-19 than their counterparts. However, to the best of our knowledge, these predictors have not been reported to be significant predictors of COVID-19 vaccine acceptance in other studies.
This study found that study participants who had good perceptions of infection prevention during the COVID-19 pandemic were almost 2 times more likely to be vaccinated against COVID-19. Consistent with our findings, in China among factory workers45 and a study conducted in northeastern Ethiopia among healthcare workers (HCW) on perceptions of the COVID-19 vaccine and refusal to receive COVID-19 vaccine, HCWs who had poor perceptions were found to refuse to accept the COVID-19 vaccines.41 The qualitative findings also elaborated that the perception of the participant was good towards COVID-19 infection prevention by wearing masks, proper hand washing with soap and water, rubbing hands with sanitizer, and keeping distance in and outside of the home. Some participants stated that the mentioned prevention methods were not sufficient to protect the person from the COVID-19 virus and every individual should take the vaccine to prevent the pandemic.
Study participants with a history of vaccination were 2.64 times more likely to be vaccinated against the COVID-19 vaccine than their counterparts. This result is consistent with a study conducted in an Israeli adult population among nurses in Hong Kong, China, a study conducted among Egyptian adults, and a survey result in US adults.29,34,46,47
These study findings were based on two prominent social marketing theories: the HBM and TPB. Under the HBM dimensions, the study participants’ perceived susceptibility to COVID-19 and perceived benefits of the vaccine were positively associated with COVID-19 vaccine acceptance. These findings are also consistent with findings from Bangladeshi, India, a study conducted on Hong Kong patients, and on healthcare workers in Vietnam.32,33,48–50 In the final model regarding TPB constructs, only subjective norms and PBC were positively associated with the intention to receive the COVID-19 vaccine. Study participants with higher subjective norms were 2.27 times more likely to take the COVID-19 vaccine. This finding is in line with a study conducted in Vietnam, Jiangsu China, Israel, Ghana, and Hong Kong.9,25,29–31,46 This result is consistent with that of a population-based anonymous online survey conducted in other parts of Ethiopia.38 Study participants with a higher PBC were 2.30 times more likely to take the COVID-19 vaccine. This finding is consistent with a study conducted among Chinese parents and factory workers in Ghana.30,31,45 This result is also consistent with that of a study conducted in other parts of Ethiopia.38 According to this TPB model, for behavior to perform a person should believe in and be motivated by oneself to accept the behavior, and intentions to perform behaviors of different kinds can be determined with high accuracy from attitudes towards the behavior, subjective norms, and perceived behavioral control.51 Therefore, we suggest that efforts should be made to improve or change the attitudes and behaviors of communities or organizations to improve the intention to be vaccinated against COVID-19.
Strength and Limitations of the Study
As strength, this study was conducted on a general population in the Jimma Zone districts by considering the two prominent social marketing theories. The quantitative results also supplemented with some qualitative results. On the other hand as a limitation there were social desirability bias may be faced when the study participants answered questions in a way that would have been viewed favorably by others, which may have resulted in over-reporting of vaccine uptake. Moreover, causal inferences could not be drawn because of the nature of the study design.
Conclusions
In our study, more than half of the adult participants intended to be vaccinated against COVID-19. In the final adjusted hierarchical logistic regression models, respondents’ travel history during the pandemic of COVID-19, past vaccination history, having family or friends who died due to COVID, good perception of infection prevention for COVID-19, and TPB constructs (subjective norms and PBC) were found to be statistically significantly associated with the intention to get vaccinated against COVID-19. Based on these findings, efforts should be made to target participants who have a poor intention to be vaccinated against COVID-19. Moreover, public health intervention programs need to pay more attention to awareness creation to improve or change attitudes, perceptions, and misbehavior towards the effectiveness and safety of the vaccine.
Abbreviations
HBM, health belief model; HCW, health care workers; PBC, perceived behavioral control; TPB, theory of planned behavior.
Data Sharing Statement
On reasonable request, the full dataset and other related materials relevant to this study can be obtained from the corresponding author.
Ethical Approval Statement
Before the study began, ethical clearance was obtained from the Institutional Review Board (IRB) of Jimma University Health Research Institute (Ref. No. IHRPGJ\549\22). A formal cooperation letter was given to the selected districts and town administration offices from the Jimma University Health Research Institute. The purpose and objective of the study were briefly explained to the head of the selected district administration office and official permission was secured. Moreover, after verbally communicated with the study participants about the purpose and objectives of the study, written informed consent was obtained from each respondent and informed their right to withdraw from the study at any time. The confidentiality and privacy of participants were secured by omitting any identifier. We confirm that, this study was conducted in accordance with the Declaration of Helsinki.
Acknowledgment
We are grateful to the Jimma University Ethical Review Board for providing ethical clearance in collaboration with the Jimma Emergency Operation Center for COVID-19 Prevention and Control. We also thank the data collectors who produced the dataset.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Musa TH, Ahmad T, Khan M, Haroon H, Wei P. Global outbreak of COVID-19: a new challenge? J Infect Dev Ctries. 2020;14(03):244–245. doi:10.3855/jidc.12530
2. Lin S, Kantor R, Clark E. Coronavirus Disease 2019. Clin Geriatr Med. 2021;37(4):509–522. doi:10.1016/j.cger.2021.05.001
3. Shen AK, Lindstrand A, Schreiber B, O’Brien K. Optimizing the supply of vaccines for COVID-19. Bull World Health Organ. 2021;99(12):848. doi:10.2471/BLT.21.287513
4. Birihane BM, Bayih WA, Alemu AY, Belay DM. Perceived barriers and preventive measures of COVID-19 among healthcare providers in Debretabor, North Central Ethiopia, 2020. Risk Manag Healthc Policy. 2020;13:2699. doi:10.2147/RMHP.S287772
5. Saied SM, Saied EM, Kabbash IA, Abdo SAEF. Vaccine hesitancy: beliefs and barriers associated with COVID‐19 vaccination among Egyptian medical students. J Med Virol. 2021;93(7):4280–4291. doi:10.1002/jmv.26910
6. Seboka BT, Yehualashet DE, Belay MM, et al. Factors influencing covid-19 vaccination demand and intent in resource-limited settings: based on health belief model. Risk Manag Healthc Policy. 2021;14:2743. doi:10.2147/RMHP.S315043
7. Wake AD. The willingness to receive COVID-19 vaccine and its associated factors:“vaccination refusal could prolong the war of this pandemic”–a systematic review. Risk Manag Healthc Policy. 2021;14:2609. doi:10.2147/RMHP.S311074
8. Getachew T, Negash A. COVID-19 vaccine acceptance and associated factors among adult clients at public hospitals in eastern Ethiopia using the health belief model: multicentre cross-sectional study. BMJ Open. 2023;13(3):e070551. doi:10.1136/bmjopen-2022-070551
9. Wang J, Li T, Ge J, et al. Applying two behavioral theories to predict the willingness to receive COVID-19 vaccine booster in the elderly: a cross-sectional study. Res Social Adm Pharm. 2023;19(3):495–501. doi:10.1016/j.sapharm.2022.10.011
10. Rosenstock IM. Why people use health services. Milbank Q. 2005;83(4). doi:10.1111/j.1468-0009.2005.00425.x
11. Yang ZJ. Predicting young adults’ intentions to get the H1N1 vaccine: an integrated model. J Health Commun. 2015;20(1):69–79. doi:10.1080/10810730.2014.904023
12. Lau JT, Yeung NC, Choi K, Cheng MY, Tsui H, Griffiths S. Factors in association with acceptability of A/H1N1 vaccination during the influenza A/H1N1 pandemic phase in the Hong Kong general population. Vaccine. 2010;28(29):4632–4637. doi:10.1016/j.vaccine.2010.04.076
13. Wong LP, Alias H, Wong P-F, Lee HY, AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum Vaccin Immunother. 2020;16(9):2204–2214. doi:10.1080/21645515.2020.1790279
14. McClenahan C, Shevlin M, Adamson G, Bennett C, O’Neill B. Testicular self-examination: a test of the health belief model and the theory of planned behaviour. Health Educ Res. 2007;22(2):272–284. doi:10.1093/her/cyl076
15. Liao Q, Cowling BJ, Lam WWT, Fielding R. Factors affecting intention to receive and self-reported receipt of 2009 pandemic (H1N1) vaccine in Hong Kong: a longitudinal study. PLoS One. 2011;6(3):e17713. doi:10.1371/journal.pone.0017713
16. Xiao X, Wong RM. Vaccine hesitancy and perceived behavioral control: a meta-analysis. Vaccine. 2020;38(33):5131–5138. doi:10.1016/j.vaccine.2020.04.076
17. Fan C-W, Chen I-H, N-Y K, et al. Extended theory of planned behavior in explaining the intention to COVID-19 vaccination uptake among mainland Chinese university students: an online survey study. Hum Vaccin Immunother. 2021;17(10):3413–3420. doi:10.1080/21645515.2021.1933687
18. Guidry JP, Laestadius LI, Vraga EK, et al. Willingness to get the COVID-19 vaccine with and without emergency use authorization. Am J Infect Control. 2021;49(2):137–142. doi:10.1016/j.ajic.2020.11.018
19. Zhang KC, Fang Y, Cao H, et al. Parental acceptability of COVID-19 vaccination for children under the age of 18 years: cross-sectional online survey. JMIR Pediatr Parent. 2020;3(2):e24827. doi:10.2196/24827
20. Central Statistical. 2007 Population and Housing Census of Ethiopia Administrative Report Central Statistical Authority Addis Ababa. Central Statistical Authority; 2012.
21. Abebe H, Shitu S, Mose A. Understanding of COVID-19 vaccine knowledge, attitude, acceptance, and determinates of COVID-19 vaccine acceptance among adult population in Ethiopia. Infect Drug Resist. 2021;14:2015. doi:10.2147/IDR.S312116
22. World Health Organization. Survey Tool and Guidance: Rapid, Simple, Flexible Behavioural Insights on COVID-19: 29 July 2020. World Health Organization; 2020.
23. Andarge E, Fikadu T, Temesgen R, et al. Intention and practice on personal preventive measures against the COVID-19 pandemic among adults with chronic conditions in southern Ethiopia: a survey using the theory of planned behavior. J Multidiscip Healthc. 2020;13:1863. doi:10.2147/JMDH.S284707
24. Myers LB, Goodwin R. Determinants of adults’ intention to vaccinate against pandemic swine flu. BMC Public Health. 2011;11:1–8. doi:10.1186/1471-2458-11-15
25. An PL, Nguyen HTN, Dang HTB, Huynh QNH, Pham BDU, Huynh G. Integrating health behavior theories to predict intention to get a COVID-19 vaccine. Health Serv Insights. 2021;14:11786329211060130. doi:10.1177/11786329211060130
26. Godin G, Kok G. The theory of planned behavior: a review of its applications to health-related behaviors. Am J Health Promot. 1996;11(2):87–98. doi:10.4278/0890-1171-11.2.87
27. Freeman D, Loe BS, Chadwick A, et al. COVID-19 vaccine hesitancy in the UK: the Oxford coronavirus explanations, attitudes, and narratives survey (Oceans) II. Psychol Med. 2022;52(14):3127–3141.
28. Dodd RH, Cvejic E, Bonner C, et al. Willingness to vaccinate against COVID-19 in Australia. Lancet Infect Dis. 2021;21(3):318–319. doi:10.1016/S1473-3099(20)30559-4
29. Shmueli L. Predicting intention to receive COVID-19 vaccine among the general population using the health belief model and the theory of planned behavior model. BMC Public Health. 2021;21(1):1–13. doi:10.1186/s12889-021-10816-7
30. Zhou M, Liu L, S-Y G, et al. Behavioral intention and its predictors toward COVID-19 booster vaccination among Chinese parents: applying two behavioral theories. Int J Environ Res Public Health. 2022;19(12):7520. doi:10.3390/ijerph19127520
31. Twum KK, Ofori D, Agyapong GK-Q, Yalley AA. Intention to vaccinate against COVID-19: a social marketing perspective using the theory of planned behaviour and health belief model. J Soc Mark. 2021;11(4):549–574. doi:10.1108/JSOCM-04-2021-0085
32. Patwary MM, Bardhan M, Disha AS, et al. Determinants of COVID-19 vaccine acceptance among the adult population of Bangladesh using the health belief model and the theory of planned behavior model. Vaccines. 2021;9(12):1393. doi:10.3390/vaccines9121393
33. Goruntla N, Chintamani SH, Bhanu P, et al. Predictors of acceptance and willingness to pay for the COVID-19 vaccine in the general public of India: a health belief model approach. Asian Pac J Trop Med. 2021;14(4):165. doi:10.4103/1995-7645.312512
34. Fisher K, Bloomstone S, Walder J, Crawford S, Fouayzi H, Mazor K. A survey of US adults annals of internal medicine attitudes toward a potential SARS-CoV-2 vaccine. Ann Intern Med. 2020;173(12):964–973. doi:10.7326/M20-3569
35. Adiyoso W, Wilopo W, Mondry M, Nurbaiti B, Suprapto FA. The use of Health Belief Model (BHM) to explain factors underlying people to take the COVID-19 vaccine in Indonesia. Vaccine X. 2023;14:100297.
36. Mesele H, Shiferaw M, Tunta A, Seid A, Kassahun W. Willingness to receive COVID-19 vaccination among adult diabetes patients in woldia comprehensive specialized hospital, North Ethiopia; A Cross-Sectional Study. Patient Prefer Adherence. 2022;16:2451. doi:10.2147/PPA.S379531
37. Yohannes S, Alemayehu A, Woldesenbet YM, et al. COVID-19 vaccine hesitancy among adults in Hawassa City Administration, Sidama Region, Ethiopia: a community-based study. Front Public Health. 2023;11:1122418. doi:10.3389/fpubh.2023.1122418
38. Asmare G, Abebe K, Atnafu N, et al. Behavioral intention and its predictors toward COVID-19 vaccination among people most at risk of exposure in Ethiopia: applying the theory of planned behavior model. Hum Vaccin Immunother. 2021;17(12):4838–4845. doi:10.1080/21645515.2021.2011651
39. Sahile AT, Gizaw GD, Mgutshini T, Gebremariam ZM, Bekele GE. COVID-19 vaccine acceptance level in Ethiopia: a systematic review and meta-analysis. Can J Infect Dis Med Microbiol. 2022;2022:1–7. doi:10.1155/2022/2313367
40. Belay GM, Alemu TG, Techane MA, et al. COVID-19 vaccine acceptance rate and its predictors in Ethiopia: a systematic review and meta-analysis. Hum Vaccin Immunother. 2022;18(6):2114699. doi:10.1080/21645515.2022.2114699
41. Adane M, Ademas A, Kloos H. Knowledge, attitudes, and perceptions of COVID-19 vaccine and refusal to receive COVID-19 vaccine among healthcare workers in northeastern Ethiopia. BMC Public Health. 2022;22(1):1–14. doi:10.1186/s12889-021-12362-8
42. Mose A, Haile K, Timerga A, Delcea C. COVID-19 vaccine hesitancy among medical and health science students attending Wolkite University in Ethiopia. PLoS One. 2022;17(1):e0263081. doi:10.1371/journal.pone.0263081
43. Kasozi KI, Laudisoit A, Osuwat LO, et al. A descriptive-multivariate analysis of community knowledge, confidence, and trust in COVID-19 clinical trials among healthcare workers in Uganda. Vaccines. 2021;9(3):253. doi:10.3390/vaccines9030253
44. Waring ME, Pagoto SL, Rudin LR, et al. Factors associated with mothers’ hesitancy to receive a COVID-19 vaccine. J Behav Med. 2023;46(1–2):179–184. doi:10.1007/s10865-021-00268-0
45. Zhang KC, Fang Y, Cao H, et al. Behavioral intention to receive a COVID-19 vaccination among Chinese factory workers: cross-sectional online survey. J Med Internet Res. 2021;23(3):e24673. doi:10.2196/24673
46. Wang K, Wong ELY, Ho KF, et al. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: a cross-sectional survey. Vaccine. 2020;38(45):7049–7056. doi:10.1016/j.vaccine.2020.09.021
47. Omar DI, Hani BM. Attitudes and intentions towards COVID-19 vaccines and associated factors among Egyptian adults. J Infect Public Health. 2021;14(10):1481–1488. doi:10.1016/j.jiph.2021.06.019
48. J-B L, Lau EYH, Chan DKC. Why do Hong Kong parents have low intention to vaccinate their children against COVID-19? Testing health belief model and theory of planned behavior in a large-scale survey. Vaccine. 2022;40(19):2772–2780. doi:10.1016/j.vaccine.2022.03.040
49. Yan E, Lai DW, Lee VW. Predictors of intention to vaccinate against COVID-19 in the general public in Hong Kong: findings from a population-based, cross-sectional survey. Vaccines. 2021;9(7):696. doi:10.3390/vaccines9070696
50. Huynh G, Tran TT, Nguyen HTN, Pham LA. COVID-19 vaccination intention among healthcare workers in Vietnam. Asian Pac J Trop Med. 2021;14(4):159. doi:10.4103/1995-7645.312513
51. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50(2):179–211. doi:10.1016/0749-5978(91)90020-T
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.