Back to Journals » Infection and Drug Resistance » Volume 16
Bacterial Etiology and Antimicrobial Resistance Pattern of Pediatric Bloodstream Infections in Beijing, 2015–2019
Authors Lyu ZY, Zhen JH, Meng QY, Zhou W, An JY, Dong F
Received 15 June 2023
Accepted for publication 14 September 2023
Published 25 September 2023 Volume 2023:16 Pages 6297—6308
DOI https://doi.org/10.2147/IDR.S426000
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Zhi-yong Lyu, Jing-hui Zhen, Qing-ying Meng, Wei Zhou, Jing-yun An, Fang Dong
Department of Clinical Laboratory Center, Beijing Children’s Hospital, Capital Medical University, National Center for Children’s Health, Beijing, 100045, People’s Republic of China
Correspondence: Fang Dong, Department of Clinical Laboratory Center, Beijing Children’s Hospital Affiliated to Capital Medical University, No. 56 Nan Lishi Road, Beijing, 100045, People’s Republic of China, Email [email protected]
Purpose: Bloodstream infections (BSIs) was an essential cause of morbidity and mortality in children. Empiric broad-spectrum treatment of BSIs may be costly and unable to effectively eliminate the correct pathogenic microbes, resulting in downstream antimicrobial resistance. The purpose was to provide evidence for diagnosis and treatment of bloodstream infections in pediatrics, by revealing the pathogen distribution and antibiotic resistance pattern of BSIs.
Methods: In this 5-year study, a total of 2544 pathogenic bacteria stains, isolated from 2368 patients with BSI, were retrospectively analyzed, to define the species distribution and the antimicrobial resistance pattern in Beijing.
Results: The most frequently isolated pathogenic bacteria were K. pneumoniae (12.1%), S. aureus (11.5%), E. coli (11.2%), and E. faecium (11.2%). Hematological malignancies were the most common disease among patients with underlying conditions. Methicillin resistance was detected in 30.0% of S. aureus and 81.7% of coagulase-negative Staphylococcus (CoNS), respectively. The detection rates of carbapenem-resistant-E. coli (CRECO) and carbapenem-resistant-K. pneumoniae (CRKPN) were 10.8% and 50.8%, respectively. In terms of 122 isolates of S. pneumonia, 5 isolates (4.1%) were penicillin-resistant Streptococcus pneumoniae (PRSP); meanwhile, 50 isolates (41.0%) were penicillin-intermediate Streptococcus pneumoniae (PISP). Among the non-fermentative gram-negative bacilli isolates, 22.8% and 26.9% of the P. aeruginosa, were resistant to imipenem and meropenem. Furthermore, the resistance rates of A. baumannii to imipenem and meropenem both were 54.5%.
Conclusion: In the study, we demonstrated the characteristics of bloodstream infections and antimicrobial susceptibility pattern of pediatrics in Beijing. Gram positive bacteria were the main pathogens of BSIs. CoNS strains presented even higher resistance to multiple antibiotics, including methicillin, than S. aureus. K. pneumoniae and E. coli represent the most common isolated gram-negative bacteria and exhibited high resistance to a variety of antimicrobial agents. Therefore, it was of critical importance to implement appropriate antimicrobial medication according to pathogen distribution and drug susceptibility test.
Keywords: bloodstream infections, children, etiology, antimicrobial resistance, methicillin-resistant S. aureus, methicillin-resistant coagulase-negative staphylococci, S. pneumoniae, carbapenem-resistant Enterobacter
Introduction
Bloodstream infections (BSIs) are associated with high morbidity and mortality in children, especially in neonates. A recent review on pediatric sepsis demonstrated that bloodstream infections accounted for 26.5% of the global disease burdens and resulted in 25% of deaths in children all over the world.1 A systemic study on global burdens of bacterial infections shows that more than 2 million deaths were caused by BSIs.2 Many factors are associated with BSIs, such as prolonged skin rupture, extensive use of catheters and bone marrow transplantation.3,4
In many studies, a wide range of bacteria strains have been described to be mainly responsible for BSIs, such as E. coli, P. aeruginosa, K. pneumoniae, H. influenza, Coagulase negative staphylococci (CoNS), S. aureus, P. aeruginosa, and S. pneumoniae.5–7 The difference in distribution and antimicrobial resistance profiles of bacteria strains causing BSIs were mainly associated with age, geographical alterations and physical conditions. In China, the causative pathogens of BSIs vary in different regions. Studies on BSIs from two provinces in China revealed that K. pneumoniae was the predominant pathogen in Chongqing, whereas, E. coli was the most prevalent pathogen in Henan and Hubei.8,9 BSIs requires emergent antimicrobial treatment, especially for the life threatening infections. Due to the particularity and complexity of blood culture, empirical therapy is predominately carried out prior to susceptibility report of antimicrobial agents. The most serious and common problem caused by empirical treatment is the resistance of antibiotics, especially in developing countries.10,11 Frequent and unreasonable use of antimicrobial agents is giving rise to antibiotic resistance in current clinical settings.10,12 Therefore, understanding bacterial epidemiology and antibiotic resistance patterns is critical.
In this study, we aim to demonstrate the prevalence and antibiotic resistance profiles of pathogens causing pediatric BSIs in Beijing. We hope that our findings will support rational use of antimicrobial agents, provide epidemiological information for development of surveillance measures, and further contribute to reduction of hospitalizing costs and antimicrobial resistance.
Experimental Materials and Methods
Study Population and Data Collection
This 5-year retrospective study on patients with positive blood culture was conducted in Beijing Children’s Hospital (BCH) affiliated to Capital Medical University, from January 2015 to December 2019. The BCH was a tertiary care children’s hospital in China, with more than 3 million outpatients and 80,000 inpatients admitted per year. A total of 2544 pathogenic bacteria stains isolated from 2368 patients, were collected as our research subjects. The inclusion criteria were as follows: (1) positive blood culture and (2) presence of bloodstream infection symptoms, such as fever, rash, rapid heartbeat and signs of inflammation. Definite pathogens which were known to cause diseases, such as Streptococcus agalactiae, Staphylococcus aureus, and gram-negative organisms were included in our study. If the pathogens were identified as coagulase-negative Staphylococcus, Corynebacterium, Bacillus, Propionibacterium or other potential skin contaminants, two or more separate blood cultures were required for reconfirmation. If the bloodstream isolate was a potential skin contaminant, we need to investigate case records to determine whether it is contaminated. We excluded duplicate strains, only the first strain was incorporated into our study, while two or more strains were isolated at the same time. The following information were collected, such as gender, age, symptom, diagnosis, underlying disease, and antimicrobial susceptibility. Our study was a retrospective study based on the clinical samples, which were part of the routine hospital laboratory procedures, and all the clinical samples in this study were not specifically isolated for this research. The Ethics Committees of Beijing Children’s Hospital affiliated to Capital Medical University and Children’s Hospital Capital institute Pediatrics exempted this study from review.
Strain Identification
Blood samples were collected from 2 different sites (avg. 3 mL per site) in every patient. It should be noted that patients under one-month old were drawn from only one site due to safety concerns. All the blood specimens were cultured on BD BACTEX FX for up to 5 days. Positive cultures were trans-inoculated into 3 types of blood culture plates: MacConkey agar, chocolate agar and blood agar (5% sheep blood). All the plates were incubated in microaerophilic conditions (5% CO2) for 16–18 hours. Microbial identification was performed by VITEK-MS (bio Mérieux, France).
Antibiotic Sensitivity Testing
Antibiotic sensitivity testing was performed on VITEK 2 (bio Mérieux, France), and results were interpreted in accordance with CLSI recommendations.13 The MIC method was used in Staphylococcus, Enterococcus, S. pneumoniae, Acinetobacter and carbapenem non-sensitive Enterobacteriaceae. Antimicrobial susceptibility testing of carbapenem-sensitive Enterobacteriaceae (out-patient), P. aeruginosa, S. pyogenes, S. lactis and Haemophilus were conducted by Kirby-Bauer (K-B) method. E-tests were applied for reconfirmation. When the method of K-B, MIC, and E-test were carried out at the same time, the results of E-test were preferred, followed by MIC and K-B. Since there was no CLSI breakpoint recommended for cefoperazone-sulbactam, we adopted the CLSI breakpoint of cefoperazone. S. aureus (ATCC 25923), E. coli (ATCC 25922), E. coli (ATCC 35218), S. pneumoniae (ATCC 49619), P. aeruginosa (ATCC 27853), E. faecalis (ATCC 29212), and H. influenza (ATCC 49247) were used as control strains for susceptibility tests.
Statistical Analysis
Data were managed and analyzed with SPSS software (Version 17.0). Antibiotic susceptibility results were analyzed using WHONET 5.6 software. Results were expressed as number of the patients or bacteria isolates, as well as proportion of the total number. All figures were prepared with the GraphPad Prism 8.0 software (GraphPad Software, La Jolla, CA).
Results
Clinical Characteristics of Children with BSIs
During the five-year study period, a total of 2544 pathogenic bacteria stains were isolated from 2368 patients. Of these patients, 59.9% (n=1399) were male, 40.1% (n=969) were female, 69.3% of these patients were less the one-year old. Among all the infection cases, 95.3% were monomicrobial. As shown in Table 1, according to the patients’ ward, the proportions of patients from emergency, out-patient, and in-patient were 15.0%, 19.9%, and 65.1%, respectively. In hospitalized population, nearly one-third of patients were admitted in hematological-oncology (13.9%), neonatology (12.9%) and intensive care unit (9.0%). 21.4% of patients (n=508) had underlying diseases, mainly divided into the following three categories: hematological malignancy (n=355), congenital heart disease (n=133) and pyelonephritis (n=20) (Table 1).
 |
Table 1 Epidemiological and Clinical Characteristics of Pediatric Patients with Bloodstream Infections (BSIs) |
Distribution of Pathogenic Bacteria
Among the 2544 bacterial isolates, gram-positive strains were the most prevalent pathogens, accounting for 54.6% (n=1389). In addition, 1155 strains were gram-negative. The most frequently isolated bacterial strains were K. pneumoniae (12.1%), followed by S. aureus (11.5%), E. coli (11.2%), E. faecium (11.2%) and CoNS (9.9%). 95.3% of episodes of BSIs were monomicrobial. (Table 2).
 |
Table 2 Distribution of Organisms Isolated from Patients with BSIs |
Antimicrobial Susceptibility
For Staphylococcus, 30.0% of S. aureus isolates and 81.7% of CoNS isolates were resistant to methicillin, respectively. From 2015 to 2019, the detection rate of MRSA was fluctuated between 25.0% and 36.5%, with the lowest rate in 2017 and the highest rate in 2018. However, the rate of MRCNS was relatively stable ranging from 80.1% to 83.5%. The annual detection rate of MRSA and MRCNS is shown in Figure 1.
 |
Figure 1 Detection rates of MRSA and MRCNS from 2015 to 2019. |
As shown in Table 3, more than 80% of S. aureus strains were resistant to penicillin, erythromycin and clindamycin. However, the most effective antimicrobial agents against S. aureus were ciprofloxacin, moxifloxacin and levofloxacin. The resistance rates of S. aureus to these three antibiotics were less than 5%. Compared with MSSA (methicillin sensitive S. aureus), MRSA presented higher resistance to penicillin, clindamycin, erythromycin and tetracycline, and lower resistance to gentamicin and trimethoprim-sulfamethoxazole. The CoNS isolates exhibited higher resistance to penicillin and erythromycin, than S. aureus strains. All Staphylococcus isolates were susceptible to vancomycin and linezolid (Table 3).
 |
Table 3 Antimicrobial Resistance Rate of Staphylococcus Strains (%) |
In terms of Enterococci, more than 75% of E. faecium isolates were found to be resistant to penicillin, ampicillin and ciprofloxacin. Whereas the resistance rates of E. faecalis against penicillin, ampicillin, and ciprofloxacin were 2.0%, 2.1% and 6.8%, respectively, much lower than that of E. faecium. One Linezolid-resistant strain was found in E. faecium isolates. In addition, two E. faecalis isolates were also resistant to Linezolid. None of the Enterococci strains were resistant to vancomycin (Table 4).
 |
Table 4 Antimicrobial Resistance Rate of Enterococci Strains (%) |
Among the 2544 isolates, there were 122 S. pneumoniae isolates, 5 of which were resistant to penicillin. The resistance rates of S. pneumoniae strains against amoxicillin, cefotaxime and cefepime were 16.4%, 13.1%, 19.7%, respectively. More than 89% of the S. pneumoniae isolates were resistant to tetracycline, clindamycin and erythromycin. However, nearly 95% of the S. pneumoniae isolates were susceptible to moxifloxacin, levofloxacin and chloramphenicol. All the S. pneumoniae strains were sensitive to linezolid and vancomycin (Table 5).
 |
Table 5 Antimicrobial Resistance Rate of S. pneumoniae Strains (%) |
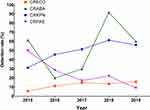
In terms of Enterobacteriaceae, K. pneumoniae was the most frequently identified pathogen, followed by E. coli and E. cloacae (Table 6). 72.7% of K. pneumoniae and 62.9% of E. coli were phenotypically characterized to be positive for ESBL (Extended-Spectrum β-Lactamases). Annual detection rates of ESBL+ strains in K. pneumoniae and E. coli are summarized in Figure 2. The resistance rate of K. pneumoniae to ceftazidime, cefatriaxone and cefepime were 70.2%, 77.3% and 72.8%. The resistance rate of E. coli to ceftazidime, cefatriaxone and cefepime were 38.5%, 61.9% and 53.1% (Table 6). 50.8% of K. pneumoniae and 12.9% of E. coli were found to be resistant to carbapenems (imipenem and/or meropenem) (Table 6 and Figure 3). E. cloacae isolates were naturally resistant to ampicillin, amoxicillin-clavulanic acid, cefazolin, and cefoxitin. Among the non-fermentative gram-negative bacilli, P. aeruginosa (n=145) and A. baumannii (n=124) were the most frequently observed pathogens. Regarding the antimicrobial resistance of P. aeruginosa, the resistance rates against imipenem and meropenem were 22.8% and 26.9%. Meanwhile, A. baumannii presented higher resistance rates to most of the test antimicrobial agents. The detection rates of CRPAE and CRABA were 26.9% and 54.5%, respectively (Figure 3 and Table 7).
 |
Table 6 Antimicrobial Resistance Rate of Enterobacteriaceae Strains |
 |
Table 7 Susceptibility of Non-Fermentative Gram-Negative Bacilli to Antimicrobial Agents |
 |
Figure 2 Detection rates of ESBL+ strains in Enterobacteriaceae isolates from 2015 to 2019. |
Discussion
BSIs can cause serious diseases with high morbidity and mortality all over the world. The global incidence of BSIs ranged between 113 and 220 per 100,000 population.6 Data from a recent retrospective study in a tertiary hospital indicated that the proportion was as high as 0.65% in China.14 The incidence of BSIs was 2.5% in neonatal patients, which was much higher than adults, reported by a children’s medical center in China.15 Since BSIs can lead to systemic sep sis and severe multiple organ dysfunction, empirical therapy should be carried out promptly. With the frequent use of antibiotics, antimicrobial resistance is becoming more and more serious. Inadequate mastery on bacterial etiology and antibiotic resistance patterns may lead to misjudgment in prescribing decisions and further give rise to increased healthcare and economic burdens.16 Therefore, surveillance studies focusing on etiology of BSIs and antimicrobial susceptibility of corresponding causative microorganisms could provide critical information for physicians.
Our surveillance data revealed that K. pneumoniae (12.1%) was the most prevalent pathogen causing BSIs in children, followed by S. aureus (11.5%), E. coli (11.2%), E. faecium (11.2%), and CoNS (9.9%) in our hospital from 2015 to 2019. These results were different from observations by other studies, in which CoNS was the predominant pathogen causing pediatric BSIs.15,17,18 Diagnosis of CoNS dominated BSIs was challenging because of the possible contamination of these strains during the process of blood sample collection. In particular, only single blood culture was conducted for precarious infants. In this study, CoNS isolates considered as contaminants were excluded, especially for those without clinical symptoms of sepsis. Therefore, compared with previous findings of other investigators,15,19 the proportion of CoNS strains causing BSIs was relatively lower in our study. In spite of this, the pathogen spectrum of major bacterial strains in our study was consistent with the results reported in other literature.19,20 However, due to differences in economic, climate, and medical conditions, the distribution of pathogens causing BSIs varied from region to region across the whole world.5,21
Our results demonstrated that gram-positive bacteria were the most common pathogens, accounting for 54.6% of BSIs episodes. Most of the gram-positive organisms causing BSIs were staphylococci. The proportions of MRSA and MRCNS were 30.0% and 81.7%, respectively. Both MRSA and MRCNS were associated with substantial morbidity and mortality, leading to severe hospital and community acquired infections.22,23 In our study, the proportion of MRSA was 30.0%, which was consistent with the data reported by China Antimicrobial Resistance Surveillance System. However, in North America and Switzerland, the MRSA proportions were much lower than our results.17,24 The high resistance of MRSA to antimicrobial agents has brought significant challenges to clinicians. Antimicrobial resistance surveillance and sufficient precautions should be strictly carried out in treating MRSA-infected patients, in order to prevent the spread of MRSA.25 Additionally, we found that CoNS strains presented even higher resistance to multiple antibiotics than S. aureus. Based on our data, all of the staphylococcus isolates were sensitive to vancomycin. Therefore, it was effective for vancomycin in dealing with MRCNS and MRSA cases.
In our 5-year study, the annual isolation rate of Enterococcus in blood was relatively stable. The annual isolation rate of E. faecium was 12.2%, 11.2%, 10.4%, 11.0%, and 8.2%. Meanwhile, the annual isolation rate of E. faecalis was 6.0%, 5.2%, 6.2%, 5.4%, and 5.4%, respectively. E. faecium had distinct antibiotic resistance patterns compared with E. faecalis. Therefore, clinicians should select appropriate antibiotics on the basis of identification and results of the antimicrobial susceptibility test.
S. pneumoniae, one of the main etiological agents causing infections in children, accounted for 4.8% of the BSIs episodes. In our study, the detection rates of PRSP and PISP in S. pneumoniae, were 4.1% and 41.0%. Several factors contributed to the high rate of PRSP and PISP in our hospital. Many hospitalized children with complex and severe clinical symptoms had experienced empiric therapy in primary or secondary hospitals before admitting to our hospital. Inappropriate antibiotic therapy in primary and secondary hospitals potentially precipitated the emergence of multi-drug resistant bacteria prior to clinical treatment by tertiary hospitals. Therefore, the unsusceptibility of S. pneumoniae to penicillin and other β-lactam antibiotics has been increasing in recent years, exhibiting severe multiple drug resistance.26
In our research, K. pneumoniae was the most commonly identified pathogen. In a recent study on mortality caused by bloodstream infections in Korea, K. pneumoniae was found to be the leading frequently isolated pathogen, emphasizing the importance of this microbe in provoking BSIs.27 The frequencies of ESBL-producing K. pneumoniae and E. coli isolates were increasing all over the world.28–30 As shown in our surveillance data, both the frequencies of ESBL-producing K. pneumoniae and ESBL-producing E. coli moderately decreased in recent years, which was similar with the result from other medical units in China,8 and the data from China Antimicrobial Resistance Surveillance System (CARSS).31 This finding may be associated with the strategies of China implemented to controlling the transmission of MDR infections. Medical institutions have actively implemented national policies on the rational use of antibiotics and strengthened hospital infection control. Among K. pneumoniae and E. coil isolates, the resistance rates of ESBL-producing stains to the antibiotics tested were significantly higher than those bacilli without producing ESBL, especially for carbapenems and third-generation cephalosporins. Interestingly, in terms of E. coli isolates, the resistance rate to cefepime (the fourth generation) was significantly higher than to ceftazidime (the third generation). The specific molecular mechanism for this phenomenon was not clear and further studies were being carried out in progress.
With the increase of infections caused by ESBL-producing Enterobacter, carbapenems were extensively used in clinical settings, resulting in the emergence of carbapenem-resistance-Enterobacter (CRE). The infection of CRE has become one of the top serious problem in the global anti-infection area due to limited therapy options. In an EuSCAPE study, the incidence of CRKPN and CRECO increased from 0.124 per 1000 admissions in 2013 to 0.223 per 1000 admissions in 2014.32 In our study, the incidence of CRE was increasing from 21.6% to 41.4% steadily, meanwhile, CRKPN exhibited substantial increase from 31.3% to 56.2%. Our retrospective data showed that the total proportion of CRE isolated from ICU, hematology department and infection department had amount to 78.0% (data not shown). The patients in these departments were associated with poor physical conditions, prolonged use of broad-spectrum antibiotics, indwelling catheters, and deep venous intubation. All of these were risk factors of CRE acquisition.33 The highest resistance rate to carbapenems (91.7%) was observed in A. baumannii in 2018 (Figure 3). Fortunately, our results demonstrated a sharp decrease in the proportion of CRPAE, from 50.0% in 2015 to 9.1% in 2019 (Figure 3). Horikoshi et al reported that the stable reduction of carbapenem utilization in pediatric patients was associated with the significant decrease in resistance of P. aeruginosa to meropenem.34,35 Although most of the E. coli strains were still susceptible to carbapenems, the resistance of CRECO has been increased, from 5.8% in 2015 to 15.9% in 2019 (Figure 3). Conclusively, the frequency of CRE has been greatly increasing, leading to high hospitalizing costs and poor therapeutic outcomes. Therefore, much more attention should be paid to medical care of CRE-infected patients, such as screening, quarantine, strict disinfection of every aspect of medical treatment, and limited use of certain antimicrobial agents.28,36
The distribution of pathogens causing BSIs and their antibiotic resistance patterns were very complicated and serious in our hospital, probably due to more admissions of pediatric patients with serious conditions. As for sepsis or septic shock, delayed medical treatment was associated with a significant increase in mortality rate.37 Therefore, emergent adequate antimicrobial therapy was crucial to improve the patient’s physical conditions and prognosis. The initial antimicrobial agents selected should cover all the potential pathogenic microbes.38,39 In our hospital, the combination of vancomycin and meropenem/cefoperazone-sulbactam was the possible choice for empirical medication on patients with sepsis or septic shock. For suspected BSIs, clinicians would first evaluate potential sources of infection and then select the initial antibacterial agents. In emergency and ward, clinicians gave priority to ceftriaxone, cefoperazone-sulbactam, and meropenem. It was important for clinicians to keep track of the results of bacterial identification and drug sensitivity test, to further choose appropriate narrow-spectrum antibiotics.
This study had several limitations. First, it was a retrospective study on etiology and drug resistance patterns of pediatric bloodstream infections based on data collected from a single tertiary pediatric hospital, inapplicable to other situations in community settings or in primary and secondary hospitals. Second, detailed clinical data and treatment before enrollment was not fully and accurately collected in this study. Therefore, comparison between community-acquired and hospital-acquired infections was not carried out in our study. Third, only one site of blood was collected from children under one-month-old, some suspicious strains could not be determined as contaminated bacteria or pathogenic bacteria. In this situation, whether it was bloodstream infections could only be diagnosed by clinicians.
Conclusions
Our 5-year study revealed the characteristics of bloodstream infections and antibiotic resistance patterns in a tertiary pediatric hospital in Beijing. K. pneumoniae was the most important pathogens causing pediatric BSIs in gram-negative bacteria, followed by E. coil, P. aeruginosa and A. baumannii. At the same time, S. aureus represented the major pathogen in gram-positive bacteria followed by Enterococcus faecium, Coagulase-negative staphylococci and Enterococcus faecalis. In resistance patterns, all the gram-positive bacteria (including MRSA, MRCNS, enterococcus and PRSP) were susceptible to vancomycin. Only one E. faecium and two E. faecalis were resistant to linezolid. In Gram-negative bacteria, the resistance rates of E. coil, K. pneumoniae, P. aeruginosa and A. baumannii to carbapenems were 10.8%, 50.8%, 26.9% and 54.5%, respectively. Disclosure of the distinct resistance profiles could help to avoid the irrational use of antibiotics and reduce antimicrobial resistance.
Abbreviations
BSIs, bloodstream infections; CRECO, Carbapenem-resistant E. oli; CRKPN, Carbapenem-resistant Klebsiella pneumoniae; PRSP, penicillin-resistant Streptococcus pneumoniae; PISP, penicillin-intermediate Streptococcus pneumoniae; CoNS, Coagulase negative staphylococci; MRSA, Methicillin resistant Staphylococcus aureus; MRCNS, Methicillin resistant coagulase negative Staphylococcus; ESBL, Extended-Spectrum β-Lactamases; CRABA, Carbapenem-resistant A. baumannii; CRPAE, Carbapenem-resistant Pseudomonas aeruginosa.
Funding
This study was supported by Beijing Natural Science Found [L202004-02].
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Menon K, Schlapbach LJ, Akech S, et al. Criteria for pediatric sepsis-a systematic review and meta-analysis by the pediatric sepsis definition taskforce. Crit Care Med. 2022;50(1):21–36. doi:10.1097/CCM.0000000000005294
2. Ikuta KS, Swetschinski LR, Robles Aguilar G; Collaborators GAR. Global mortality associated with 33 bacterial pathogens in 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2022;400(10369):2221–2248. doi:10.1016/S0140-6736(22)02185-7
3. Li X, Ye H. Clinical and mortality risk factors in bloodstream infections with carbapenem-resistant Enterobacteriaceae. Can J Infect Dis Med Microbiol. 2017;2017:6212910. doi:10.1155/2017/6212910
4. Rudd KE, Johnson SC, Agesa KM, et al. Global, regional, and national sepsis incidence and mortality, 1990–2017: analysis for the global burden of disease study. Lancet. 2020;395(10219):200–211. doi:10.1016/S0140-6736(19)32989-7
5. Guzek A, Rybicki Z, Wozniak-Kosek A, Tomaszewski D. Bloodstream infections in the intensive care unit: a single-center retrospective bacteriological analysis between 2007 and 2019. Pol J Microbiol. 2022;71(2):263–277. doi:10.33073/pjm-2022-025
6. Kern WV, Rieg S. Burden of bacterial bloodstream infection-a brief update on epidemiology and significance of multidrug-resistant pathogens. Clin Microbiol Infect. 2020;26(2):151–157. doi:10.1016/j.cmi.2019.10.031
7. Tsuzuki S, Matsunaga N, Yahara K, Shibayama K, Sugai M, Ohmagari N. Disease burden of bloodstream infections caused by antimicrobial-resistant bacteria: a population-level study, Japan, 2015–2018. Int J Infect Dis. 2021;108:119–124. doi:10.1016/j.ijid.2021.05.018
8. Tian L, Sun Z, Zhang Z. Antimicrobial resistance of pathogens causing nosocomial bloodstream infection in Hubei Province, China, from 2014 to 2016: a multicenter retrospective study. BMC Public Health. 2018;18(1):1121. doi:10.1186/s12889-018-6013-5
9. Wang S, Chen S, Feng W, et al. Clinical characteristics of nosocomial bloodstream infections in neonates in two hospitals, China. J Trop Pediatr. 2018;64(3):231–236. doi:10.1093/tropej/fmx054
10. Ferri M, Ranucci E, Romagnoli P, Giaccone V. Antimicrobial resistance: a global emerging threat to public health systems. Crit Rev Food Sci Nutr. 2017;57(13):2857–2876. doi:10.1080/10408398.2015.1077192
11. Ikhimiukor OO, Odih EE, Donado-Godoy P, Okeke IN. A bottom-up view of antimicrobial resistance transmission in developing countries. Nat Microbiol. 2022;7(6):757–765. doi:10.1038/s41564-022-01124-w
12. Hu F, Zhu D, Wang F, Wang M. Current status and trends of antibacterial resistance in China. Clin Infect Dis. 2018;67(suppl_2):S128–S134. doi:10.1093/cid/ciy657
13. CLSI. Performance standards for antimicrobial susceptibility testing.
14. Cui J, Li M, Cui J, Wang J, Qiang X, Liang Z. The proportion, species distribution and dynamic trends of bloodstream infection cases in a tertiary hospital in China, 2010–2019. Infection. 2022;50(1):121–130. doi:10.1007/s15010-021-01649-y
15. Zhang X, Li Y, Tao Y, Ding Y, Shao X, Li W. Epidemiology and drug resistance of neonatal bloodstream infection pathogens in East China children’s Medical Center from 2016 to 2020. Front Microbiol. 2022;13:820577. doi:10.3389/fmicb.2022.820577
16. Widmer AF, Lakatos B, Frei R. Strict infection control leads to low incidence of methicillin-resistant Staphylococcus aureus bloodstream infection over 20 years. Infect Control Hosp Epidemiol. 2015;36(6):702–709. doi:10.1017/ice.2015.28
17. Larru B, Gong W, Vendetti N, et al. Bloodstream infections in hospitalized children: epidemiology and antimicrobial susceptibilities. Pediatr Infect Dis J. 2016;35(5):507–510. doi:10.1097/INF.0000000000001057
18. Huttunen R, Attman E, Aittoniemi J, et al. Nosocomial bloodstream infections in a Finnish tertiary care hospital: a retrospective cohort study of 2175 episodes during the years 1999–2001 and 2005–2010. Infect Dis (Lond). 2015;47(1):20–26. doi:10.3109/00365548.2014.956791
19. Qiu Y, Yang J, Chen Y, et al. Microbiological profiles and antimicrobial resistance patterns of pediatric bloodstream pathogens in China, 2016–2018. Eur J Clin Microbiol Infect Dis. 2021;40(4):739–749. doi:10.1007/s10096-020-04069-2
20. Bielicki JA, Lundin R, Sharland M. Antibiotic resistance prevalence in routine bloodstream isolates from children’s hospitals varies substantially from adult surveillance data in Europe. Pediatr Infect Dis J. 2015;34(7):734–741. doi:10.1097/INF.0000000000000652
21. Musicha P, Cornick JE, Bar-Zeev N, et al. Trends in antimicrobial resistance in bloodstream infection isolates at a large urban hospital in Malawi (1998–2016): a surveillance study. Lancet Infect Dis. 2017;17(10):1042–1052. doi:10.1016/S1473-3099(17)30394-8
22. He S, Lin J, Li Y, et al. Insights into the epidemiology of methicillin-resistant coagulase-negative Staphylococci carriage in community-based drug users. J Infect Public Health. 2020;13(11):1742–1748. doi:10.1016/j.jiph.2020.09.011
23. Monaco M, Pimentel de Araujo F, Cruciani M, Coccia EM, Pantosti A. Worldwide epidemiology and antibiotic resistance of Staphylococcus aureus. Curr Top Microbiol Immunol. 2017;409:21–56. doi:10.1007/82_2016_3
24. Buetti N, Atkinson A, Kottanattu L, Bielicki J, Marschall J, Kronenberg A. Patterns and trends of pediatric bloodstream infections: a 7-year surveillance study. Eur J Clin Microbiol Infect Dis. 2017;36(3):537–544. doi:10.1007/s10096-016-2830-6
25. Landrum ML, Neumann C, Cook C, et al. Epidemiology of Staphylococcus aureus blood and skin and soft tissue infections in the US military health system, 2005–2010. JAMA. 2012;308(1):50–59. doi:10.1001/jama.2012.7139
26. Zhao C, Li Z, Zhang F, et al. Serotype distribution and antibiotic resistance of Streptococcus pneumoniae isolates from 17 Chinese cities from 2011 to 2016. BMC Infect Dis. 2017;17(1):804. doi:10.1186/s12879-017-2880-0
27. Mun SJ, Kim SH, Kim HT, Moon C, Wi YM. The epidemiology of bloodstream infection contributing to mortality: the difference between community-acquired, healthcare-associated, and hospital-acquired infections. BMC Infect Dis. 2022;22(1):336. doi:10.1186/s12879-022-07267-9
28. Stewardson A, Fankhauser C, De Angelis G, et al. Burden of bloodstream infection caused by extended-spectrum beta-lactamase-producing Enterobacteriaceae determined using multistate modeling at a Swiss University Hospital and a nationwide predictive model. Infect Control Hosp Epidemiol. 2013;34(2):133–143. doi:10.1086/669086
29. Somily AM, Habib HA, Absar MM, et al. ESBL-producing Escherichia coli and Klebsiella pneumoniae at a tertiary care hospital in Saudi Arabia. J Infect Dev Ctries. 2014;8(9):1129–1136. doi:10.3855/jidc.4292
30. Liu J, Du SX, Zhang JN, Liu SH, Zhou YY, Wang XR. Spreading of extended-spectrum beta-lactamase-producing Escherichia coli ST131 and Klebsiella pneumoniae ST11 in patients with pneumonia: a molecular epidemiological study. Chin Med J (Engl). 2019;132(16):1894–1902. doi:10.1097/CM9.0000000000000368
31. System CARS. 2014至2017年中国儿童及新生儿患者细菌耐药监测研究 [Surveillance of bacterial resistance in children and newborns across China from 2014 to 2017]. Zhonghua Yi Xue Za Zhi. 2018;98(40):3279–3287. Chinese. doi:10.3760/cma.j.issn.0376-2491.2018.40.013
32. De Laveleye M, Huang TD, Bogaerts P, et al. Increasing incidence of carbapenemase-producing Escherichia coli and Klebsiella pneumoniae in Belgian hospitals. Eur J Clin Microbiol Infect Dis. 2017;36(1):139–146. doi:10.1007/s10096-016-2782-x
33. Moghnieh R, Abdallah D, Jadayel M, et al. Epidemiology, risk factors, and prediction score of carbapenem resistance among inpatients colonized or infected with 3rd generation cephalosporin resistant Enterobacterales. Sci Rep. 2021;11(1):14757. doi:10.1038/s41598-021-94295-1
34. Horikoshi Y, Suwa J, Higuchi H, et al. Sustained pediatric antimicrobial stewardship program with consultation to infectious diseases reduced carbapenem resistance and infection-related mortality. Int J Infect Dis. 2017;64:69–73. doi:10.1016/j.ijid.2017.09.012
35. Probst V, Islamovic F, Mirza A. Antimicrobial stewardship program in pediatric medicine. Pediatr Investig. 2021;5(3):229–238. doi:10.1002/ped4.12292
36. Leistner R, Gurntke S, Sakellariou C, et al. Bloodstream infection due to extended-spectrum beta-lactamase (ESBL)-positive K. pneumoniae and E. coli: an analysis of the disease burden in a large cohort. Infection. 2014;42(6):991–997. doi:10.1007/s15010-014-0670-9
37. Timsit JF, Ruppe E, Barbier F, Tabah A, Bassetti M. Bloodstream infections in critically ill patients: an expert statement. Intensive Care Med. 2020;46(2):266–284. doi:10.1007/s00134-020-05950-6
38. Dugar S, Choudhary C, Duggal A. Sepsis and septic shock: guideline-based management. Cleve Clin J Med. 2020;87(1):53–64. doi:10.3949/ccjm.87a.18143
39. Ferrer R, Martin-Loeches I, Phillips G, et al. Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: results from a guideline-based performance improvement program. Crit Care Med. 2014;42(8):1749–1755. doi:10.1097/CCM.0000000000000330
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.