Back to Journals » Infection and Drug Resistance » Volume 15
Bacterial and Fungal Superinfections in COVID-19 Patients Hospitalized in an Intensive Care Unit from Timișoara, Romania
Authors Novacescu AN , Buzzi B, Bedreag O, Papurica M, Rogobete AF, Sandesc D, Sorescu T , Baditoiu L , Musuroi C, Vlad D, Licker M
Received 22 September 2022
Accepted for publication 19 November 2022
Published 1 December 2022 Volume 2022:15 Pages 7001—7014
DOI https://doi.org/10.2147/IDR.S390681
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Alexandru Noris Novacescu,1,2,* Bettina Buzzi,3 Ovidiu Bedreag,3,4 Marius Papurica,3,4 Alexandru Florin Rogobete,3,4 Dorel Sandesc,3,4 Teodora Sorescu,5,6 Luminita Baditoiu,7,8,* Corina Musuroi,9,10 Daliborca Vlad,10,11 Monica Licker8– 10,*
1Doctoral School, ‘Victor Babes’ University of Medicine and Pharmacy, Timisoara, Romania; 2Compartment of Anesthesia and Intensive Care, ‘Dr. Victor Babes’ Infectious Diseases and Pulmonology Clinical Hospital, Timisoara, Romania; 3Clinic of Anesthesia and Intensive Care, ‘Pius Brînzeu’ Emergency Clinical County Hospital, Timisoara, Romania; 4Department of Anaesthesia and Intensive Care, ‘Victor Babes’ University of Medicine and Pharmacy, Timisoara, Romania; 5Department of Diabetes, Nutrition and Metabolic Diseases, ‘Victor Babes’ University of Medicine and Pharmacy, Timisoara, Romania; 6Clinic of Diabetes, Nutrition and Metabolic Diseases, ‘Pius Brînzeu’ Emergency Clinical County Hospital, Timisoara, Romania; 7Department of Epidemiology, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania; 8Multidisciplinary Research Center on Antimicrobial Resistance, ‘Victor Babes’ University of Medicine and Pharmacy, Timisoara, Romania; 9Department of Microbiology, ‘Victor Babes’ University of Medicine and Pharmacy, Timisoara, Romania; 10Clinical Laboratory, ‘Pius Brînzeu’ Emergency Clinical County Hospital, Timisoara, Romania; 11Department of Pharmacology, ‘Victor Babes’ University of Medicine and Pharmacy, Timisoara, Romania
*These authors contributed equally to this work
Correspondence: Teodora Sorescu, Department of Diabetes, Nutrition and Metabolic Diseases, ‘Victor Babes’ University of Medicine and Pharmacy, 2 Eftimie Murgu Square, Timisoara, Romania, Tel +40724515424, Email [email protected]
Purpose: Critically ill patients hospitalized in the intensive care unit (ICU) have an increased infection risk. The aim of this study was to determine the bacterial and fungal superinfections rate in Coronavirus disease 2019 (COVID-19) patients stationed in the ICU, identify risk factors associated with their development and to determine whether superinfection plays a role in patients’ outcome in this population.
Patients and Methods: In this retrospective, non-interventional, single centre, cohort study, medical records of 302 consecutive patients with SARS-COV-2 pneumonia admitted into the COVID-19 ICU of the largest university hospital from Western Romania between October 2020 and May 2021, were reviewed, of whom 236 patients met the inclusion criteria.
Results: One hundred and nineteen patients developed a superinfection ≥ 48 h after being admitted to the hospital. Superinfection rate in the ICU was 50.42%. Coagulase-negative Staphylococci (CoNS) and Enterococcus spp. were predominantly isolated from blood cultures, while Acinetobacter baumannii, Staphylococcus aureus and Candida spp. from tracheobronchial aspirates. Significant independent risk factors regarding bacterial/fungal superinfection in COVID-19 patients were obtained for the following variables: number of days of central venous catheter (HR = 1.13 [1.07– 1.20], p < 0.001) and prior administration of corticosteroids (HR = 2.80 [1.33– 5.93], p = 0.007). Four independent predictive risk factors were associated with unfavorable outcome: age (HR = 1.07 [95% CI 1.03– 1.12], p = 0.001); Carmeli Score (HR = 6.09 [1.18– 31.50], p = 0.031); body mass index (HR = 1.11 [1.02– 1.21], p = 0.011) and the presence of a central venous catheter (HR = 6.49 [1.93– 21.89], p = 0.003).
Conclusion: The superinfection rate in COVID-19 patients was high in this study group. Exogenous risk factors were associated with superinfection more than endogenous factors. Only a small percentage of uninfected COVID-19 patients were not prescribed antibiotics during their hospitalization, raising serious concerns regarding the judicious prescribing of antibiotics in viral infections.
Keywords: COVID-19, viral pandemic, ICU, bacteria, fungi, superinfection
Introduction
In late 2019, an outbreak of viral pneumonia emerged in Wuhan, China, with patients experiencing severe respiratory symptoms.1 The clinical features of Coronavirus disease 2019 (COVID-19) patients and the pathophysiologic evolution of the disease have been extensively described over the last 2 years.2–7 Superinfections are known to be the plague of Intensive care Units (ICUs) of all around the world. Although COVID-19 is a viral disease, empirical antibiotherapy has been widely administered to patients admitted with COVID-19.3,8,9 Bacterial or fungal superinfections have been described over the course of other viral pandemics, thus increasing awareness upon this subject in the present pandemic.10
In Romania, data regarding bacterial and fungal superinfections in COVID-19 patients are scarce and still emerging. According to the ECDC (European Centre for Disease Prevention and Control) European Antimicrobial Resistance Surveillance Network (EARS-Net) 2022 report, although the average total consumption of antibiotics decreased by almost 18% during the COVID-19 pandemic (between 2019 and 2020), the same changes in the antimicrobial resistance (AMR) rates were not observed in the European Union/European Economic Area (EU/EEA) and the relative use of broad-spectrum antibiotics has increased in many European countries.11
Regarding the Gram negative bacilli (GNB), the percentage of AMR is clearly increasing from Western to Eastern Europe. The high rates of antibiotic resistance are worrying in many states from Central and South-Eastern Europe, including Romania, especially for Klebsiella pneumoniae resistant to third-generation cephalosporins and carbapenems or carbapenem-resistant non-fermenters.12 However, there is still a lack of knowledge regarding the dynamics of bacterial and fungal infection in severely and critically ill COVID-19 patients.13
Our study aimed to determine the hospital acquired infection rate in patients with COVID-19 pneumonia hospitalized in the COVID-19 ICU of the largest university hospital from Western Romania, risk factors associated with the development of bacterial and fungal superinfections and predictive risk factors regarding fatality in the aforementioned patient population.
Materials and Methods
Study Design, Setting and Population
A retrospective cohort, non-interventional, single centre study was conducted and the medical records of 302 consecutive patients with SARS-COV-2 pneumonia admitted to the COVID-19 ICU of “Pius Brinzeu” Emergency Clinical County Hospital Timișoara, Romania (SCJUPBT) between October 2020 and May 2021, were reviewed. This institution is a tertiary care, University-affiliated, teaching hospital with 1174 beds, providing medical care for the Western region of Romania. During the third wave of COVID-19 in Romania, a 12-bed COVID-19 ICU has been set up, along with a 56-bed non-critical mixed pathology ward, isolated in a separate building of SCJUPBT.
In order to be included in this study, patients had to be aged ≥18 years, to have a positive reverse transcription-polymerase chain reaction (RT-PCR) test result for SARS-CoV-2 virus isolated from nasopharyngeal swab or tracheobronchial aspirates/bronchoalveolar lavage (BAL) upon hospital admission and to present clinical and/or radiological signs of COVID-19 pneumonia. Patients aged <18 years and patients with an ICU length of stay (LOS) of under 48 hours were excluded. Two hundred and thirty-six Caucasian patients met the study inclusion criteria.
The study was approved by the Ethics Committee of SCJUPBT (no 206/7.09.2020) and it was performed in accordance with the Declaration of Helsinki. All patients provided written informed consent upon hospital admission regarding the procedures performed during hospitalization, including the test results used in this study and the use of the resulting data in scientific research publications, with the assurance that they would remain anonymous. In the cases where obtaining informed consent from the patients was impossible due to their critical condition, a legal representative provided informed consent.
Study Protocol and Definitions
Hospital records of all the enrolled patients were reviewed by two independent reviewers. Variables were grouped into: demographic data, comorbidities, clinical data (including relevant biological variables for COVID-19, obtained at the ICU admission), microbiological data, antibiotic treatment, LOS, patient discharge status. The data was anonymized and collected in a database designed for this study.
Patients with COVID-19 pneumonia hospitalized in our ICU had 3 forms of severity: moderate – individuals who showed evidence of lower respiratory disease during clinical assessment or imaging and who had an oxygen saturation measured by pulse oximetry (SpO2) ≥94% on room air at sea level; severe – individuals who had a ratio of arterial partial pressure of oxygen to fraction of inspired oxygen (PaO2/FiO2) <300 mm Hg, a respiratory rate >30 breaths/min, or lung infiltrates >50% on radiologic examination; critical – individuals who presented acute respiratory failure, septic shock, and/or had multiple organ dysfunction.14
Patients were divided into two groups: group 1, which included patients with unfavorable outcomes (deceased or aggravated during their hospitalization) and group 2 – patients with favorable outcomes (improved status upon discharge). The same patients were regrouped in group 3 and group 4, depending on their bacterial/fungal infection (group 3) or non-infected status (group 4) over their ICU hospitalization.
COVID-19 patients were treated based on the latest available evidence and guidelines, with a combination of antivirals (remdesivir, favipiravir), corticosteroids (dexamethasone, methylprednisolone), anticoagulants [(low molecular weight heparin (LMWH), unfractioned heparin (UFH)] and antibiotics, based on clinical judgement.
Upon admission into the ICU, microbiological screening tests were performed (nasal and anal exudates) and cultures were double-checked for patients who were transferred from the non-critical COVID-19 ward.
In order to determine whether patients developed a superinfection, clinical judgement was used, based on clinical, paraclinical and radiological findings: fever (>38°C), development of purulent sputum, cardiovascular instability requiring vasopressors, escalation of respiratory support, worsening of ventilatory parameters, increase in leucocyte count or leukopenia, increase in CRP, procalcitonin, worsening of chest imagistic, or patterns such as consolidations, pleural effusions not characteristic for COVID-19. When deemed necessary, cultures were sampled, based on the suspected infection site. In order to confirm a superinfection, microbiological isolation of a bacterial or fungal etiological agent was mandatory.
Infections were defined as hospital-acquired infections (HAI) if fulfilling the criteria of the case definitions included in the Commission Implementing Decision (EU) 2018/945 of 22 June 201815 on the communicable diseases and related special health issues to be covered by epidemiological surveillance as well as relevant case definitions.
The superinfections acquired in the ICU were considered those with an onset ≥48 h after the COVID-19 ICU admission, without the identification of a bacterial strain with the same resistance phenotype from the admission screening tests or from previous infections in the non-critical ward.
The case fatality rate was calculated as the percentage of COVID-19 patients who died during hospitalization in our ICU out of the total number of patients with this diagnosis, during the surveillance period.
The superinfection rate was calculated as the percentage of COVID-19 patients that presented a new infection at 48 h or more since being admitted to the ICU out of the total number of patients included in this study. All non-repetitive bacterial strains were included. Clostridioides difficile, identified by toxigenesis, not by culture, is included in the total number of positive samples/total number of infected patients, but not in the total number of bacterial strains.
Multi-drug resistant (MDR) strains were defined as resistant to at least one antibiotic from three or more classes of antimicrobial agents. Extensively drug-resistant (XDR) strains were defined as resistant to at least one agent of all categories of antimicrobials except one or two classes.16
The percentage of resistance phenotypes [(extended spectrum beta-lactamase producing Enterobacterales (ESBLE), carbapenem-resistant organisms (CRO)] was calculated from the total number of Gram negative strains or the total number of strains from the same species/genus [for methicillin-resistant Staphylococcus aureus (MRSA), methicillin-resistant coagulase-negative Staphylococci (MR-CoNS) and vancomycin-resistant Enterococcus (VRE)]. The percentage of multidrug resistance was calculated by reporting the number of MDR/XDR strains to the total number of strains isolated from the specific biological sample.
Microbiological Method
Cultures were performed according to the working protocol of the Bacteriology Laboratory of SCJUPBT. All isolates were first identified using the VITEK® 2 GN, VITEK® 2 GP ID cards (BioMérieux, Marcy l’Etoile, France). Antimicrobial susceptibility tests (AST) were performed using the VITEK 2 GN AST-N222 and VITEK 2 AST GP 67 cards (BioMérieux, Marcy l’Etoile, France) by determination of the minimum inhibitory concentration (MIC) and classification into resistance phenotypes, according to the Clinical Laboratory and Standards Institute (CLSI) 2020/2021 criteria. The reference strains used were: Escherichia coli ATCC 25922 and Klebsiella pneumoniae ATCC 1705, Pseudomonas aeruginosa ATCC 27853, Staphylococcus aureus ATCC 25923. Clostridioides difficile enterocolitis was diagnosed by determining the A and/or B toxin from the spontaneously emitted feces by using the LIAISON® Analyzer through an automatic immunoassay testing.
Statistical Analysis
Data were analyzed using IBM SPSS Statistics 20 software (SPSS Inc., Chicago, USA). Continuous variables were characterized by median and interquartile range (IQR), while category variables by value and percent. Data distribution was tested using the Shapiro–Wilk test. Numerical variables were compared by Mann–Whitney U-test for comparison between two independents sub-samples, while for nominal ones the chi2 test was used (Fisher exact test). For bivariate correlation, we applied the Pearson correlation. Variables that met the statistical significance (p ≤ 0.05) in univariate analysis were further investigated by logistic regression, the model being chosen according to the Nagelkerke R2 coefficient and the Hosmer-Lemeshow test for assessing the deviation from the theoretical model. The avoidance of multicollinearity was achieved by linear regression, with the calculation of the variance inflation factor (VIF). All statistical tests were two-tailed and the statistical significance threshold p was set at 0.05.
Results
During the 8 months of surveillance, a study group of 236 patients was constituted, with a median age of 66.50 [58.00–72.00] years, the predominance of the male sex - 58.90% [95% CI 52.33–65.24]) versus female - 41.10% [95% CI 34.76–47.67] and a median of days of hospitalization in the ICU of 9.00 [5.00–13.00] days. Most of the patients had severe forms of the disease (64.41% [95% CI 57.94–70.51]), 33.47% [95% CI 27.48–39.89] were critical, while 2.12% [95% CI 0.69–4.87] had moderate forms of COVID-19 but with severe underlying pathology.
Case fatality rate was 74.58% [95% CI 68.52–80.00], similar between patients with bacterial/fungal superinfections - 73.11% [95% CI 64.21–80.82] versus non-infected patients 76.07% [95% CI 67.30–83.47], p = 0.602.
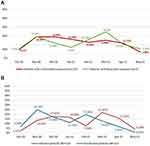
A powerful and statistically significant direct correlation (r = 0.787, p = 0.020) was obtained between the monthly distribution of cases with negative outcome and the number of infected patients, while between the distribution of cases with positive evolution and that of non-bacterial/fungal infected cases, the direct, moderate correlation was above the threshold of statistical significance (r = 0.689, p = 0.058) (Figure 1).
The univariate analysis presented in Table 1 identified 19 variables that met the statistical conditions of risk factors for negative outcomes and 4 protective factors. However, after applying the logistic regression model, only 4 independent risk factors predictive for an unfavorable outcome emerged:
- Age (HR = 1.07 [95% CI 1.03–1.12], p = 0.001);
- Carmeli Score (HR = 6.09 [1.18–31.50], p = 0.031);
- Body mass index (BMI) (HR = 1.11 [1.02–1.21], p = 0.011) and
- Presence of a central venous catheter (CVC) (HR = 6.49 [1.93–21.89], p = 0.003).
 |
Table 1 Univariate Analysis of Factors Associated with Unfavorable Outcome in COVID-19 Patients Hospitalized in the ICU (Timișoara, Romania, October 2020–May 2021) |
The protective factors were female gender (HR = 0.31 [95% CI 0.11–0.85], p = 0.022) and the number of days of oxygen delivery on face mask (HR = 0.37 [95% CI 0.26–0.53], p < 0.001).
One hundred and nineteen patients presented a superinfection after 48 h or more from admission. In all cases, the infection involved a different strain than the one identified by screening at admission, where 15.97% [95% CI 9.90–23.81] of the cases presented colonization with ESBL-producing strains, 13.45% [95% CI 7.88–20.91] with CRO strains, 6.72% [95% CI 2.95–12.82] with VRE and 3.36% [95% CI 0.92–8.38] with MRSA, respectively. The rate of bacterial or fungal superinfection was 50.42% [95% CI 43.86–56.97].
In order to identify the predictive factors for bacterial/fungal superinfection in COVID-19 patients, the statistically significant items presented in Table 2 were introduced in logistic regression models.
 |
Table 2 Univariate Analysis of Factors Associated with Superinfection in COVID-19 Patients Hospitalized in the ICU (Timișoara, Romania, October 2020–May 2021) |
The variables related to the administered antibiotic therapy, subsequent to the onset of the infection, were not entered into the model. Significant values for independent risk factors were obtained for the following variables:
- Number of days of central venous catheter (HR = 1.13 [1.07–1.20], p < 0.001);
- Prior administration of corticosteroids (HR = 2.80 [1.33–5.93], p = 0.007).
The logistic regression model also identified the following protective factors:
- Higher O2 saturations (HR = 0.003 [0.00–0.16], p = 0.004);
- Older age (HR = 0.96 [0.94–0.99], p = 0.014);
- Cardiovascular disease (HR = 0.48 [0.25–0.89], p = 0.021) – in fact, a marker associated with advanced age.
It is worth noting that only 13 patients (11.11%) with COVID-19 not infected with bacteria/fungi did not receive antibiotic chemotherapy during hospitalization.
Of the 119 cases with a superinfection, 183 microbiological samples were collected, of which 155 (84.70%) were positive for bacteria and 31 (16.94%) were positive for fungi, with the isolation of 152 non-repetitive bacterial strains, according to the distribution presented in Table 3. Gram negative strains (52.63%) were identified in a similar proportion to Gram positive ones (47.37%). Most of the biological samples were tracheobronchial aspirates (35.52% [95% CI 28.60–42.92]) and blood cultures (26.23% [95% CI 20.02–33.23]), with statistically significant differences regarding the isolation of different species - CoNS (p < 0.001) and Enterococcus spp (p = 0.002) predominant in blood, respectively, Acinetobacter baumannii (p < 0.001), Staphylococcus aureus (p = 0.009), MRSA (p = 0.037), Candida spp. (p = 0.040) in tracheobronchial aspirates. MDR strains were isolated predominantly from blood cultures (p = 0.009), while XDR strains from tracheobronchial aspirates (p < 0.001).
The comparison of samples collected from patients with unfavorable outcomes versus those related to improved outcomes (139 versus 44) identified only two statistically significant differences – ESBLE and CRO strains were more prevalent in patients with favorable outcome (OR = 0.46 [0.22–0.94], p = 0.032) and OR = 0.42 [0.20–0.88], p = 0.020, respectively).
Discussion
In the study conducted in our center, we have found a bacterial or fungal superinfection rate of 50.42%, with a high percentage of MDR and XDR strains isolated from the biological specimens. The regression model identified 2 predictors of bacterial or fungal superinfection: the long duration of CVC maintenance and previous corticosteroid therapy. Bacterial or fungal superinfection did not, however, come up as a risk factor for unfavorable outcome, not even in the univariate analysis. But the monthly distribution of cases with unfavorable evolution and the one of infected cases correlated directly, strongly, statistically significant, which argues for a link between bacterial superinfection and severity of the disease in the context of COVID-19. The predictors of unfavorable outcome, identified by logistic regression, were advanced age, Carmeli score, BMI and the presence of a CVC. The case fatality rate was similar in the subsamples of superinfected and uninfected patients, reinforcing the fact that in our study population, superinfection did not play a significant role in patient outcomes.
In our center, the rate of superinfection was high (50.42%), while this rate varies greatly across the globe from centre to centre, being as low as 3% and as high as 60% or more.4,17,18 Hughes et al17 reported an incidence of 3.20% for co-infection, in 2020 in the UK. In another meta-analysis, it was estimated at 3.50%19 and in the study led by Moreno-Torres20 it was 8.50%. In a study led in two clinics from Medellin, Colombia, Juan Carlos Cataño-Correa et al21 found similar superinfection rates to those obtained in our study (49.6%). Similar values have been obtained in the University hospital of Zurich (42%) and in the ICU of Brescia University Hospital (57.6%).18,22
Antibiotic stewardship programs, socioeconomic, demographic, and cultural factors, medical culture might be some of the reasons behind this great variation. Overwhelmed medical services, stress, burnout, non-ICU personnel or the lack of trained personnel, etc. might also have weighed hard on controlling hospital acquired outbreaks.
The percentages for the Gram negative and the Gram positive isolated germs were similar in our study (52.63% vs 47.37%). GNB were represented mostly by Acinetobacter baumannii (19.13% of the cases), Klebsiella spp. (10.38%) and Pseudomonas aeruginosa (5.46% of the samples), respectively. On the other hand, Gram positive cocci were represented by CoNS (16.94% of the samples), Enterococcus spp. (14.75%) or Staphylococcus aureus (4.92% of the samples), respectively. As the HAI were not limited to pneumonia and bacteremia, the samples in which Clostridioides difficile toxins were detected (14.21%) should also be noted. In a study published by Marinescu et al and conducted in Timisoara,23 it was found that 75% of COVID-positive patients who developed Clostridioides difficile were treated with antibiotics during the last 2 months. The destruction of the balance of the intestinal microbiota is inherent in the conditions of generalized antibiotic therapy. In the present study, 88.89% of non-bacterially infected cases received antibacterial chemotherapy. Moreover, the COVID-19 pandemic has aggravated the problem of overuse of antimicrobial therapy, with the acceleration of the risk of bacterial resistance, both in the community environment and in the hospital one. Rawson et al8 showed that 72% of hospitalized patients with COVID-19 received empiric antibiotic therapy to prevent bacterial superinfections, possibly to treat possible community infections, and in the study conducted by Nasir et al,24 64% of the control subjects had antibiotic therapy, despite the lack of coinfection/superinfection.8 Empirical antibiotic chemotherapy was discouraged in our national COVID-19 protocol25, its use being reserved only for patients with bacterial/fungal infection.
The high percentage of XDR strains isolated from tracheobronchial aspirates is also noteworthy, as a result of the intense circulation of Acinetobacter baumannii strains with extended resistance, while MDR strains were prevalent in blood cultures, being mainly represented by MR-CoNS. Hospitalization for COVID-19, especially in the ICU, involves high invasiveness of therapeutic procedures, the wide use of empiric antibiotic therapy, possibly prolonged hospitalization, all with an increased risk of bacterial or fungal superinfection.26–29
A particularity of this study is the significantly higher incidence of the ESBLE and CRO strains in patients with favorable outcome, which shows that a bacterial infection, even with a multidrug resistant strain, can be controlled by appropriate antibiotic therapy and it is not necessarily a determining factor for the unfavorable outcome of the patient.
Regarding the predictors of bacterial/fungal superinfection, the regression model identified only 2: the long duration of CVC maintenance and previous corticosteroid therapy. Procalcitonin was not retained among them, nor were the comorbidities or possible organic effects generated by SARS-CoV2. Instead, high oxygen saturation was an independent protective factor. The sub-samples were not matched by age, both older age and cardiovascular pathology meeting the statistical conditions of a protective factor (the latter being, in fact, a marker associated with advanced age). In general, increasing age is also associated with increased susceptibility to infections, but in this study, exogenous hospital acquired factors seem more important than endogenous ones. Significant associations were also found between bacterial co-infection and the severity of the clinical form of COVID-19 at admission (Nasir et al24 AOR: 4.42 [95% CI 1.63–11.9]), as well as with liver damage, but not with renal damage.30
Regarding corticosteroid therapy, while some studies associate it with an increased risk of infection (Nasir et al24 identify a 4.60 increase in risk [95% CI 1.24–17.05]), the use of steroids – alone or with tocilizumab – did not confer a greater risk of bacterial infections and improved survival rates in other analyses.20
The logistic regression identified 4 risk factors for unfavorable outcome. While age is recognized as a biological risk factor, BMI was also associated with a negative outcome in a previous study conducted in a different center from Timisoara, Romania, being identified as an independent factor of death OR = 1.08 [1.04–1.13], p < 0.001.31 The Carmeli score is a marker related both to age, comorbidities and to contact with the hospital environment, and the need for a CVC advocates for the invasiveness of the treatment and indirectly, for the severity of the initial viral infection. It was also associated with fatality due to COVID-19 in the study led by Nasir et al, where the presence of a central venous catheter increased the risk of death by 11.08 times [95% CI: 4.02–30.5], p < 0.001.24
In Romania, COVID-19 patients were admitted to ICUs based only on the clinical form of the disease and the general condition of the patient, while age, comorbidities or the presence of terminal pathology were not admission criteria, which resulted in a high case fatality rate, compared to other European studies. Thus, at the University Clinical Hospital of Valladolid, Spain, a mortality rate of 37% was recorded. Likewise, a retrospective study conducted in seven ICUs in six French hospitals reported a mortality rate of 31%.32,33
In our study, the case fatality rate was similar in the subsamples of superinfected (74.78%) and uninfected (76.92%) COVID-19 patients. Studies from 2020 revealed that bacterial superinfection, especially bacteremia and pneumonia, correlated with a negative evolution and death of patients affected by the emerging virus.9,34,35 Subsequently, the interrelationship between SARS-CoV-2 infection, bacterial/fungal superinfection and death has diversified. In a study from 2021, Farrell et al36 opine that a decline in the patient’s general condition, concurrent with the onset of the bacterial infection, can be linked to the increase in fatality, but a deterioration prior to the diagnosis of a superinfection, when the evolution should be attributed solely to the infection with the SARS-CoV-2 virus, is also possible.
Also, in 2022, Moreno-Torres et al20 published a study in which bacterial infections were not independently associated with mortality (OR = 0.85, [95% CI 0.47–1.53], p > 0.05), which strengthens the hypothesis that bacterial/fungal infections are only a surrogate marker of the patients most severely affected by the viral infection. Following multivariate analysis, in the aforementioned study, Moreno-Torres et al20 obtained the following independent factors associated with increased mortality: age (OR 1.13, 95% CI 1.10–1.16, p < 0.0001), neurological (OR 2.77, 95% CI 1.77–4.34, p < 0.0001) or renal comorbidities (OR 3.46, 95% CI 1.92–6.24, p < 0.0001), immunosuppression (OR 3.33, 95% CI 1.91–5.81, p < 0.0001) and severity of respiratory distress – from mild (OR 4.67, 95% CI 1.50–14.54, p = 0.008) to severe (OR 282.10, 95% CI 79.18–1005.33, p < 0.0001).
The results of this investigation have led to changes in local practice in two areas: firstly, an increased adherence of medical staff to hand hygiene, an increased adherence to complete sterile barrier when performing invasive maneuvers and finally the use of disposable, single-use non-sterile gown, gloves, cape and face-mask by the whole medical staff whenever care is provided to the patient were reinforced. Secondly, the antibiotic stewardship program intensified its work by having two ICU specialists supervising antibiotic prescriptions jointly with the infectious diseases specialist in our unit.
Our study has some limitations. Since it is a unicentric study, there are difficulties in generalizing the obtained results. No data are provided regarding the incidence of HAI in the non-COVID-19 ward of the same ICU, in order to compare the incidence and the circulating microbial flora and the prevalence of resistance phenotypes, respectively. Genotyping of the isolated strains in order to identify the genetic substrate of multiresistance was not carried out. It should also be noted that no periodical sampling in order to diagnose infection was performed, cultures being drawn strictly upon clinical/paraclinical signs of infection relying exclusively on the judgement of the clinicians, thus some infections could have eluded from being diagnosed. Also, the collection of biological test results for this study only at admission and not in dynamics, as well as the lack of data on the fraction of inspired oxygen, could have biased certain results.
Conclusion
A high rate of superinfection - 50.42% was observed in this population of COVID-19 patients hospitalized in our ICU during the third wave of the pandemic. Only a small percentage of COVID-19 patients that did not develop bacterial or fungal superinfections were not prescribed antibiotics over their hospitalization period, raising serious concerns regarding the judicious prescribing of antibiotics in viral infections, taking into consideration the fact that some clinical (especially fever, cough, dyspnea, diaphoresis, etc.) and paraclinical (radiological signs of pneumonia, high inflammation, etc.) findings in viral infection can mimic bacterial infection. Therefore, we consider that the optimization of antimicrobial stewardship programs is indispensable for the future, in order to relieve the burden of antimicrobial resistance, reduce hospitalization costs and ultimately offer patients the best possible care regarding the prescription of antibiotics.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi:10.1016/S0140-6736(20)30183-5)30183-5
2. Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with Pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi:10.1056/NEJMOA2001017/SUPPL_FILE/NEJMOA2001017_DISCLOSURES.PDF
3. Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 Pneumonia in Wuhan, China. JAMA Intern Med. 2020;180(7):934–943. doi:10.1001/JAMAINTERNMED.2020.0994
4. Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323(16):1574–1581. doi:10.1001/JAMA.2020.5394
5. Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC. Pathophysiology, transmission, diagnosis, and treatment of Coronavirus Disease 2019 (COVID-19): a review. JAMA. 2020;324(8):782–793. doi:10.1001/JAMA.2020.12839
6. Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–422. doi:10.1016/S2213-2600(20)30076-X
7. Docea AO, Tsatsakis A, Albulescu D, et al. A new threat from an old enemy: re-emergence of coronavirus. Int J Mol Med. 2020;45(6):1631–1643. doi:10.3892/IJMM.2020.4555/HTML
8. Rawson TM, Moore LSP, Zhu N, et al. Bacterial and fungal coinfection in individuals with coronavirus: a rapid review to support COVID-19 antimicrobial prescribing. Clin Infect Dis. 2020;71(9):2459–2468. doi:10.1093/CID/CIAA530
9. Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study Lancet. 2020;395(10229):1054–1062. doi:10.1016/S0140-6736(20)30566-3
10. Martín-Loeches I, Sanchez-Corral A, Diaz E, et al. Community-acquired respiratory coinfection in critically III patients with pandemic 2009 influenza A(H1N1) virus. Chest. 2011;139(3):555–562. doi:10.1378/chest.10-1396
11. Antimicrobial resistance surveillance in Europe 2022-2020 data. Available from: https://www.ecdc.europa.eu/en/publications-data/antimicrobial-resistance-surveillance-europe-2022-2020-data.
12. Antimicrobial resistance in the EU/EEA (EARS-Net) - annual epidemiological report for 2019. Available from: https://www.ecdc.europa.eu/en/publications-data/surveillance-antimicrobial-resistance-europe-2019.
13. Coppola S, Ciabattoni A, Pozzi T, Castagna V, Bassi GL, Chiumello D. Hazardous mismatch between pulmonary pathogens and antibiotic treatments in COVID-19 patients. Br J Anaesth. 2020;125(4):e380–e382. doi:10.1016/j.bja.2020.07.019
14. COVID-19 treatment guidelines. Available from: https://www.covid19treatmentguidelines.nih.gov/.
15. Decizia de punere în aplicare (UE) 2018/945 a Comisiei din 22 iunie 2018 privind bolile transmisibile și problemele de sănătate speciale conexe care trebuie să facă obiectul supravegherii epidemiologice, precum și definițiile de caz relevante (Text cu relevanță pentru SEE.) - Publications Office of the EU. Available from: https://op.europa.eu/ro/publication-detail/-/publication/57ed0506-80e4-11e8-ac6a-01aa75ed71a1.
16. Magiorakos AP, Srinivasan A, Carey RB, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–281. doi:10.1111/j.1469-0691.2011.03570.x
17. Hughes S, Troise O, Donaldson H, Mughal N, Moore LSP. Bacterial and fungal coinfection among hospitalized patients with COVID-19: a retrospective cohort study in a UK secondary-care setting. Clin Microbiol Infect. 2020;26(10):1395–1399. doi:10.1016/j.cmi.2020.06.025
18. Buehler PK, Zinkernagel AS, Hofmaenner DA, et al. Bacterial pulmonary superinfections are associated with longer duration of ventilation in critically ill COVID-19 patients. Cell Rep Med. 2021;2(4):100229. doi:10.1016/j.xcrm.2021.100229
19. Langford BJ, So M, Raybardhan S, et al. Bacterial co-infection and secondary infection in patients with COVID-19: a living rapid review and meta-analysis. Clin Microbiol Infect. 2020;26(12):1622–1629. doi:10.1016/j.cmi.2020.07.016
20. Moreno-Torres V, de Mendoza C, de la Fuente S, et al. Bacterial infections in patients hospitalized with COVID-19. Intern Emerg Med. 2022;17(2):431–438. doi:10.1007/S11739-021-02824-7/FIGURES/1
21. Cataño-Correa JC, Cardona-Arias JA, Mancilla JPP, García MT. Bacterial superinfection in adults with COVID-19 hospitalized in two clinics in Medellín-Colombia, 2020 PLoS One. 2021;16(7):e0254671. doi:10.1371/JOURNAL.PONE.0254671
22. Signorini L, Moioli G, Calza S, et al. Epidemiological and clinical characterization of superinfections in critically ill coronavirus disease 2019 patients. Crit Care Explor. 2021;3(6):e0430. doi:10.1097/CCE.0000000000000430
23. Marinescu AR, Laza R, Musta VF, et al. Clostridium difficile and COVID-19: general data, ribotype, clinical form, treatment-our experience from the largest infectious diseases hospital in Western Romania. Medicina 2021, 57(10):1099. doi:10.3390/MEDICINA57101099
24. Nasir N, Rehman F, Omair SF. Risk factors for bacterial infections in patients with moderate to severe COVID-19: a case-control study. J Med Virol. 2021;93(7):4564–4569. doi:10.1002/JMV.27000
25. Protocol-tratament-covid19-ms. Available from: https://www.cnscbt.ro/index.php/legislatie_cov/1617-protocolul-de-tratament-covid-19/file.
26. Rus M, Licker M, Musuroi C, et al. Distribution of NDM1 carbapenemase-producing proteeae strains on high-risk hospital wards. Infect Drug Resist. 2020;13:4751–4761. doi:10.2147/IDR.S280977
27. Muntean D, Licker M, Horhat F, et al. Extensively drug-resistant Acinetobacter baumannii and proteeae association in a Romanian intensive care unit: risk factors for acquisition. Infect Drug Resist. 2018;11:2187–2197. doi:10.2147/IDR.S171288
28. Ramadan HKA, Mahmoud MA, Zakaria M, et al. Predictors of severity and co-infection resistance profile in COVID-19 patients: first report from upper Egypt. Infect Drug Resist. 2020;13:3409–3422. doi:10.2147/IDR.S272605
29. Lansbury L, Lim B, Baskaran V, Lim WS. Co-infections in people with COVID-19: a systematic review and meta-analysis. J Infect. 2020;81(2):266–275. doi:10.1016/j.jinf.2020.05.046
30. Guo M, Gao M, Gao J, et al. Identifying risk factors for secondary infection post-SARS-CoV-2 infection in patients with severe and critical COVID-19. Front Immunol. 2021;12:3601. doi:10.3389/FIMMU.2021.715023/BIBTEX
31. Laza R, Lazureanu VE, Musta VF, et al. COVID-19 independent risk factors for unfavorable disease progression: a cross-sectional study from Romania. Int J Gen Med. 2022;15:2025–2036. doi:10.2147/IJGM.S350920
32. Llitjos JF, Bredin S, Lascarrou JB, et al. Increased susceptibility to intensive care unit-acquired pneumonia in severe COVID-19 patients: a multicentre retrospective cohort study. Ann Intensive Care. 2021;11(1):1–8. doi:10.1186/S13613-021-00812-W/TABLES/3
33. Nebreda-Mayoral T, Miguel-Gómez MA, March-Rosselló GA, et al. Bacterial/fungal infection in hospitalized patients with COVID-19 in a tertiary hospital in the community of Castilla y León, Spain. Enferm Infecc Microbiol Clin 2022;40(4):158–165. doi:10.1016/J.EIMCE.2022.02.002
34. Wang L, He W, Yu X, et al. Coronavirus disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. J Infect. 2020;80(6):639–645. doi:10.1016/J.JINF.2020.03.019
35. Ferrando C, Mellado-Artigas R, Gea A, et al. Patient characteristics, clinical course and factors associated to ICU mortality in critically ill patients infected with SARS-CoV-2 in Spain: a prospective, cohort, multicentre study. Rev Esp Anestesiol Reanim 2020;67(8):425–437. doi:10.1016/J.REDARE.2020.07.001
36. Farrell JM, Zhao CY, Tarquinio KM, Brown SP. Causes and consequences of COVID-19-associated bacterial infections. Front Microbiol. 2021;12:1911. doi:10.3389/FMICB.2021.682571/BIBTEX
37. APACHE II: a severity of disease classification system - PubMed. Available from: https://pubmed.ncbi.nlm.nih.gov/3928249/.
38. Carmeli Y. Strategies for managing today’s infections. Clin Microbiol Infect. 2008;14(SUPPL. 3):22–31. doi:10.1111/j.1469-0691.2008.01957.x
39. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8)90171-8
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.