Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Automated Oxygen Administration Alleviates Dyspnea in Patients Admitted with Acute Exacerbation of COPD: A Randomized Controlled Trial
Authors Sandau C , Hansen EF , Ringbæk TJ , Kallemose T , Bove DG, Poulsen I, Nørholm V , Pedersen L , Jensen JUS , Ulrik CS
Received 16 November 2022
Accepted for publication 27 March 2023
Published 18 April 2023 Volume 2023:18 Pages 599—614
DOI https://doi.org/10.2147/COPD.S397782
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Charlotte Sandau,1 Ejvind Frausing Hansen,1 Thomas Jørgen Ringbæk,2 Thomas Kallemose,3 Dorthe Gaby Bove,4 Ingrid Poulsen,3,5 Vibeke Nørholm,3 Lars Pedersen,6 Jens Ulrik Stæhr Jensen,7,8 Charlotte Suppli Ulrik1,9
1Department of Respiratory Medicine and Endocrinology, Pulmonary Section, Copenhagen University Hospital Hvidovre, Hvidovre, Denmark; 2Allergy and Lung Clinic, Elsinore, Denmark; 3Department of Clinical Research, Copenhagen University Hospital Hvidovre, Hvidovre, Denmark; 4University College Absalon, Centre for Nursing, Roskilde, Denmark; 5Research Unit Nursing and Health Care, Aarhus University, Aarhus, Denmark; 6Department of Respiratory Medicine and Infectious Diseases, Copenhagen University Bispebjerg Hospital, Copenhagen, Denmark; 7Respiratory Medicine Section, Department of Medicine, Herlev-Gentofte Hospital, Hellerup, Denmark; 8Department of Clinical Medicine, Faculty of Health Sciences, University of Copenhagen, København, Denmark; 9Institute of Clinical Medicine, University of Copenhagen, Copenhagen, Denmark
Correspondence: Charlotte Sandau, Email [email protected]
Objective: Devices for Automated Oxygen Administration (AOA) have been developed to optimize the therapeutic benefit of oxygen supplementation. We aimed to investigate the effect of AOA on multidimensional aspects of dyspnea and as-needed consumption of opioids and benzodiazepines, as opposed to conventional oxygen therapy, in hospitalized patients with Acute Exacerbation of COPD (AECOPD).
Method and Patients: A multicenter randomized controlled trial across five respiratory wards in the Capital Region of Denmark. Patients admitted with AECOPD (n=157) were allocated 1:1 to either AOA (O2matic Ltd), a closed loop device automatically delivering oxygen according to the patient’s peripheral oxygen saturation (SpO2), or conventional nurse-administered oxygen therapy. Oxygen flows and SpO2 levels were measured by the O2matic device in both groups, while dyspnea, anxiety, depression, and COPD symptoms were accessed by Patient Reported Outcomes.
Results: Of the 157 randomized patients, 127 had complete data for the intervention. The AOA reduced patients’ perception of overall unpleasantness significantly on the Multidimensional Dyspnea Profile (MDP) with a difference in medians of − 3 (p=0.003) between the intervention group (n=64) and the control group (n=63). The AOA also provided a significant between group difference in all single items within the sensory domain of the MDP (all p-values≤ 0.05) as well as in the Visual Analogue Scale – Dyspnea (VAS-D) within the past three days (p=0.013). All between group differences exceeded the Minimal Clinical Important Difference of the MDP and VAS-D, respectively. AOA did not seem to have an impact on the emotional response domain of the MDP, the COPD Assessment Test, the Hospital Anxiety and Depression Scale, or use of as-needed opioids and/or benzodiazepines (all p-values> 0.05).
Conclusion: AOA reduces both breathing discomfort and physical perception of dyspnea in patients admitted with AECOPD but did not seem to impact the emotional status or other COPD symptoms.
Keywords: dyspnea, oxygen, automated oxygen therapy, multidimensional dyspnea profile, COPD, hospital, admission, therapy
Introduction
In patients with Chronic Obstructive Pulmonary Disease (COPD), acute exacerbations are a major cause of hospitalizations, and in most cases associated with dyspnea, anxiety, and hypoxemia.1,2
Supplemental oxygen is a key component of the in-hospital management of these patients. Titrated oxygen therapy to achieve oxygen saturation (SpO2) between 88 and 92% reduces the risk of hypercapnic acidosis and the need for assisted ventilation compared to higher flow rates, reaching higher SpO2 levels.3,4 To optimize the administration of oxygen and thereby therapeutic impact, devices with Automatic Oxygen Administration (AOA), in response to the patient’s SpO2, have been developed.5,6 It has been shown that AOA significantly increases the proportion of time within the guideline-recommended ranges of SpO2 compared to conventional oxygen therapy.5–8
Dyspnea is often associated with hypoxemia and is a major cause of suffering and therefore a treatment target. The clinical management of Acute Exacerbation in COPD (AECOPD) is complex and includes inhaled bronchodilators and oxygen therapy for hypoxemic patients. To reduce the intensity of dyspnea, these primary therapies may, if necessary, be supplemented by as-needed opioids or benzodiazepines for the related anxiety, despite their respiratory risk profiles.9–12 Dyspnea is defined as “a subjective experience of breathing discomfort that consist of qualitatively distinct sensations that vary in intensity”.10 The patient’s experience of dyspnea is based on several afferent paths, which the brain processes into physical perceptions as well as affective responses often linked to emotions such as fear and anxiety.10,13 Thus, dyspnea is a multidimensional symptom and can be measured as such by The Multidimensional Dyspnea Profile (MDP).14 However, most studies investigating dyspnea as an outcome of supplemental oxygen therapy in patients with COPD have primarily been carried out in out-of-hospital settings measuring the symptom uni-dimensionally and based on recall of physical activity.15 Hypoxemia, hypercapnia, and dyspnea are associated in healthy subjects16, whereas the relationship between hypoxemia, hypercapnia, and the perception of dyspnea in patients with COPD is unclear, and evidence is inconsistent on whether or not oxygen therapy can relieve dyspnea.17–19
We hypothesized that optimized oxygen therapy via AOA can reduce dyspnea and the need for as-needed opioids and benzodiazepines in patients hospitalized with AECOPD and hypoxemia. Therefore, the primary aim of this study was to investigate the effect of AOA, compared to conventional oxygen therapy, on patients’ perception of dyspnea measured by the MDP, and secondary is the need for opioids and/or benzodiazepines in patients hospitalized with AECOPD.
Materials and Methods
This study (ClinicalTrials.gov Identifier: NCT04370990) is a study nested within the open-labeled, multicenter randomized controlled trial “Automated oxygen-control with O2matic during admission with exacerbation in COPD” (ClinicalTrials.gov Identifier: NCT03661086). Patients were included and randomized 1:1 to either conventional oxygen therapy or automated oxygen therapy provided by O2matic. The study was approved by The Danish Medicines Agency, the Committee on Health Research Ethics of the Capital Region (H-17040114), and the Data Protection Authority (VD-2018-44, 6248) and conducted in accordance with the Declaration of Helsinki.
Materials
Patients were recruited from five respiratory wards in the Capital Region of Denmark between December 2018 and April 2022. Patients were eligible for inclusion within the first 48 hours following admission if they had a primary diagnosis of COPD (International Classification of Diseases [ICD] code J440, J441, J448, or J449), an expected length of hospital stay (LOS) >24 hours, an SpO2 <88% breathing room air, age ≥35 years, and cognitively able and willing to provide written informed consent to participate. A concomitant diagnosis of pneumonia was accepted.
Patients were excluded if they required mechanical ventilation within the first 48 hours of admission, had a verified pulmonary embolism within two weeks prior to admission, had concomitant asthma or any other disease requiring an SpO2 >94%. Women <55 years of age had to have a negative pregnancy test to be eligible for inclusion.
Baseline Assessment
Baseline data in the form of descriptive demographic, clinical, and paraclinical data and data on comorbidities were collected from the patients’ medical records at inclusion.
The paraclinical data were obtained from the first measurement taken on arrival of the active admission. The descriptive demographic data and data on comorbidity were obtained from the latest registration in the medical records with pneumonia verified by radiology, whereas the clinical data were obtained from EWS registration at the time of inclusion.
The administration of medication during the intervention was collected retrospectively from the medical records.
Intervention
The O2matic (O2matic Ltd, Herlev, Denmark) is a device that delivers AOA by a closed-loop system, that continuously measures patients’ peripheral oxygen saturation by pulse oximetry and automatically titrates oxygen flows according to it. In the O2matic, acceptable ranges for SpO2 and oxygen flows are individually defined and increments or decrements in oxygen flows are based on the average SpO2 of the past 15 seconds input from the pulse oximeter. The proportional change in flow will be relative to the difference between defined and actual measurements of SpO2.
Before randomization and initiation of the intervention, the accepted SpO2 range (88–92% or 90–94% depending on clinical evaluation of the risk of hypercapnia) and accepted range of oxygen flows (0–6 L/min, 0–10 L/min, or 0–15 L/min) were selected. Patients were randomized and allocated 1:1 using REDCap electronic data capture tools (REDCap consortium, Vanderbilt University Medical Center, Nashville, TN, USA) hosted by the Capital Region of Denmark to either an intervention of AOA by the O2matic device or to standard care with manually nurse administered supplemental oxygen via O2matic. In the standard care group, the O2matic was converted into a manual device only showing oxygen flow and range on screen, with no data on SpO2. When in manual mode, oxygen flows were administered manually by the nurses like it is done in conventional oxygen therapy by flowmeters. In both groups the O2matic saves records of patients’ saturation levels and oxygen flows throughout the intervention. The intervention would last for a maximum of three days or until patients were titrated back to pre-admission Long Term Oxygen Therapy (LTOT) flow or no oxygen flows. The intervention would stop earlier if patients were non-compliant, wished to stop the intervention, were dismissed, were transferred to another ward, or needed Non-Invasive Ventilation (NIV). If patients died or needed mechanical ventilation it was considered a serious adverse event and the intervention would also be stopped.
Outcomes
The effect of AOA on dyspnea was assessed by Patient Reported Outcome Measurements (PROMs). The PROMs were collected bedside, interview-based, and in paper form, before patients were connected to the O2matic and after completing the intervention, preferably while still connected to the O2matic (see Figure 1). There were three different procedures for collecting end of intervention data:
- When the patients were back on the usual LTOT dose, the first author would come by the site, interview the patient who was still using the device, and discontinue the intervention afterward.
- When the patients still had a need for supplemental oxygen throughout the intervention, in which case the intervention was ended after three days. Also, in this case, the first author would come by the site, interview the patient who was still using the device, and discontinue the intervention afterward.
- The patients had become normoxic and weaned from oxygen within the three intervention days. In this case, patients were disconnected from the device by the ward nurses and the interviews would be conducted after weaning the intervention, but within a maximum of 12 hours.
Dyspnea was measured with the Multidimensional Dyspnea Profile (MPD)14,20 and the Visual Analogue Scale – Dyspnea (VAS-D).21 COPD symptoms were measured by the COPD Assessment Test (CAT)22–24 and symptoms of anxiety and depression were measured by the Hospital Anxiety and Depression Scale (HADS).25,26
Primary outcome was the between group difference in perception of overall unpleasantness of dyspnea as assessed by the scale A1 on the MDP. The perception was assessed for the focal period of “past three days” at baseline and for “the duration of the intervention” by the end of intervention.
Secondary outcomes were the between group differences in:
- VAS-D assessed for the focal period of “current dyspnea” at baseline and at end of intervention, and VAS-D assessed for the focal period of “past three days” at baseline and for “the duration of the intervention” by the end of intervention.
- The sensory and emotional items of dyspnea as given on the MDP assessed for the focal period of “past three days” at baseline and for “the duration of the intervention” by the end of intervention.
- The respiratory symptoms by CAT assessed for the focal period of “past three days” at baseline and for “the duration of the intervention” by the end of intervention.
- Anxiety and depression symptoms by the HADS assessed for the focal period of “past three days” at baseline and for “the duration of the intervention” by the end of intervention.
- The consumption of opioids and/or benzodiazepines reported in number of as-needed administrations for the duration of the intervention.
The Multidimensional Dyspnea Profile
The MDP is a symptom specific questionnaire developed for clinical use. It has a user specified focus period, and measures dyspnea multidimensionally by a global scale A1 “Breathing discomfort” (range 0–10), a sensory dimension consisting of five single items (range 0–10, cumulated 0–40), and an emotional response domain also consisting of five single items (range 0–10, cumulated 0–40).14 The higher the number, the more intense the symptom. The construct, dimensions, and domains are shown in Figure 2.
The questionnaire has a construct validity providing an ability to discriminate items and dimensions into separable components of dyspnea, making it possible to detect if a particular therapy may reduce a specific dyspnea sensation or emotional response by single items such as eg “air hunger” or “anxiety”.14 The MDP questionnaire has been extensively tested and has shown a high reliability, validity, and sensitivity to clinical changes in different populations.27–30 The MDP has been translated and linguistic validated for Danish.20 The Minimal Clinical Important Difference (MCID) of the MDP has been given by Ekström et al in 2020 from a sample of cardiorespiratory outpatients.31 The study found the mean (95% CI) of the COPD-specific MCIDs of the MDP A1 unpleasantness to be 0.58 (0.06–1.10) (n=35); MDP perception 3.02 (0.06–5.99) (n=28), and MDP emotional score 2.07 (−0.71 to 4.86) (n=37), respectively.31
Visual Analogue Scale – Dyspnea (VAS-D)
The VAS-D measures dyspnea on a 0–100 mm scale, anchored between extreme lowest or highest points, with 100 being most extreme dyspnea.32 It is known that measures of “current dyspnea” and “usual dyspnea” correlatepoorly,33,34 thus we used the VAS-D to measure “dyspnea now” and “dyspnea over the past three days” at both inclusion and by the end of intervention. The MCID of VAS-D ranges from −13.9 mm to −9.5 mm, with effect sizes classed as large (−15.0 to −20.0 mm), moderate (−9.4 to −12.5 mm) and small (−4.7 to −6.3 mm).34
COPD Assessment Test (CAT)
The CAT questionnaire is a COPD specific symptom screening tool that assesses disease severity.22,23,35 The CAT consists of 8 items (range 0–40). A CAT score of 0–10 indicates low disease severity impact, a score of 11–20 medium impact, a score of 21–30 high impact, and 31–40 very high impact.36 A change of 2 units is suggested as MCID.22,35
Hospital Anxiety and Depression Scale (HADS)
The HADS has been developed to assess symptoms of depression or anxiety in hospitalized patients.26,37 It consists of 14 items (range 0–3), with seven items reflecting symptoms of anxiety HADS-A scale (range 0–21) and seven reflecting symptoms of depression HADS-D scale (range 0–21). A score ≥8 in each scale is accepted as threshold for either clinical anxiety or depression.26 The questionnaire has been extensively validated and has proved high sensitivity and specificity in both scales on somatic in-hospital populations.38 It has also been validated in a COPD specific out of hospital population.39,40 Based on effect sizes in a sample of 88 hospitalized patients with COPD, Puhan et al found the MCID for the HADS total score to be 1.17 and for the HADS anxiety and depression score the MCID was 1.32 and 1.40 respectively.41
Statistical Analysis
As no MCID of the A1 scale of the MDP was published as we initiated this study, we assumed, based on literature, a reduction ≥1 unit on the MDP, with a standard deviation (SD) of 2 units, a sample size of 126 patients met the criterion of α=5% and β=20%.27,42 Only patients who received the intervention and had completed follow-up measurements were included in the present analysis (per protocol). In anticipation of a maximum 20% of lack of completion, our study was rounded up to a sample size of a minimum of 150 patients.
Estimates are presented as either frequency and percentage for categorical variables or mean/median with standard deviation (SD)/interquartile range (IQR) for continuous variables.
Changes from baseline to end of intervention of the primary and secondary outcomes were analyzed by either two-sample t-test or Wilcoxon rank sum test with continuity correction, if normality assumptions were not satisfied. Normality assumption of variables was evaluated by histograms and QQ-plots. Estimates from test are presented as mean or medians with p-values and 95% confidence intervals (CIs) where possible. Patients included in the primary analysis had no missing values on variables used in the analysis. p-Values of less than 0.05 were considered statistically significant. All analyses were done using R version 4.1.2.43
Results
We included and randomized 157 patients allocated equally to either AOA (n=79) or conventional oxygen therapy (n=78), with a total of 127 patients completing the intervention and filling in questionnaires by end of intervention. Further details of inclusion and exclusion are displayed in Figure 3.
Patient Characteristics
The patients’ demographic characteristics, including markers of disease severity (MRC, comorbidity and exacerbation history), oxygen therapy, smoking status, spirometry values, and questionnaire scores, did not differ between groups at baseline (Table 1). However, the maintenance daily doses of morphine at baseline did differ slightly between the two groups (Table 2).
 |
Table 1 Characteristics of the Included Patients, n=157 |
 |
Table 2 Baseline Symptom Scores are Given in Medians and Inter Quartile Ranges (IQR) and Fixed Daily Dose of Drugs in mg are Given in Mean (SD) |
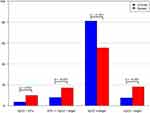
The mean duration of the intervention was 40 hours in both groups and the median length of stay across the two groups was 6.0 days, whereas the median time from randomization to discharge was 5.7 days. The fraction of time with normoxemia (SpO2 in target, either 88–92% or 90–94%), hyperoxemia (SpO2>target), hypoxemia (SpO2 between 85 and target), and severe hypoxemia (SpO2<85%), respectively, are presented in Figure 4, for the intervention group and the control group.
Primary Outcome
The overall unpleasantness of dyspnea on the A1 scale of the MDP was reduced significantly by AOA with a between group difference in medians of −3 (p=0.003), median [IQR] of −5 [−6: –2] in the intervention group and −2 [−6: 0] in the control group. Overall unpleasantness on the MDP had an intensity at baseline of median [IQR] 8 [7: 10] in the intervention group and 8 [5: 9] in the control group. The intensities given by median [IQR] at follow-up were respectively 3 [2: 5] in the intervention group and 4 [2.5: 7] in the usual care group. The within group differences are illustrated in the spaghetti plots Figure 5.
All within group changes are presented in Table 3.
 |
Table 3 Data are shown as medians with Inter Quartile Ranges [IQR]. |
Secondary Outcomes
Differences in median change between the intervention group and the control group in the five items within the sensory dimension of the MDP and “VAS-dyspnea past three days” are given in medians [IQR] in Table 4 (all p-values≤0.03). No significant difference between groups was found for the CAT-score, HADS-A, HADS-D, or the cumulated number of as-needed administrations of opioids and/or benzodiazepines (p=0.061).
 |
Table 4 Reflection of Patients' Answers to the SQ Descriptor Choice Shown in Figure 2: The Construct, Dimensions, and Domains of the Multidimensional Dyspnea Profile |
The choice of “Air hunger” as the most accurate descriptor was reduced during the intervention from 26 to 6 patient choices in the intervention group as opposed to a reduction from 28 to 20 patient choices in the control group (Table 3).
Discussion
This study shows that AOA reduces dyspnea overall unpleasantness, in patients hospitalized with AECOPD and hypoxemia, when compared to conventional oxygen therapy. The AOA also reduces all the five items within the sensory dimension of dyspnea, as well as dyspnea within past three days, significantly when compared to conventional oxygen therapy. All of these results were substantial in size and according to MCID the effect size, they should be considered clinically relevant.31,34
The effect of AOA on dyspnea measured on the A1 scale is clinically relevant, with a within group reduction in the intervention group of more than eight times the MCID and a between group difference of more than three times the reported MCID.31 Furthermore, Stevens et al found an intensity of dyspnea on the A1 scale to be acceptable to patients if <4 on the 0–10 rating scale,44 underlining the clinical important impact of AOA in our study, as dyspnea on the A1 scale was reduced to a median of 3 in the intervention group and 4 in the control group.
Moreover, AOA reduced patients’ perception of anxiety by 2 units in the intervention group as opposed to 0.5 units in the control group on the MDP. We found no reports on the MCIDs on item level for the MDP except from the A1 scale.31 However, the MCIDs are reported on domain level by Ekström et al, and are given by a mean (95% CI) 3.02 (0.06: 5.99) for the “sensory domain” and 2.07 (−0.71: 4.86) for the “emotional domain”,31 making the effect of the AOA on the sensory domain not only significant but also clinically relevant. Given that the item scales have identical rating scales, with ranges from 0 to 10, the reduction of 2 units on the anxiety item, could potentially be considered clinically important, but psychometric evidence lacks. We also found a trend towards a reduction in as-needed use of opioids and benzodiazepines, however this was not significant.
Our results on patients’ perceptions of dyspnea showed the five items within the sensory dimension on MDP to have higher intensity by admission and a greater sensitivity to AOA, than the five items within the emotional dimension. Our study also reports that “Air hunger” was the descriptor that most accurately describes how patients hospitalized with AECOPD’s breathing feel at admission. A finding consistent with a study that assessed dyspnea in 156 hospitalized patients of mixed diagnoses via MDP, which found that “air hunger” was the most predominant and intense component of severe dyspnea.44 Furthermore, our study shows that the choice of “Air hunger” as the most accurate descriptor was reduced by 20 patient choices in the intervention group as opposed to 8 patient choices the control group, indicating an effect of AOA on sensations of “Air hunger”.
Air hunger is known to be unpleasant and to induce a more intense emotion of anxiety than eg work effort, which may explain why the anxiety item was the only item within the emotional domain that was also reduced by the AOA intervention.45 A laboratory study, on healthy subjects, showed that hypoxic and hypercapnic drives to breath generate sensations of “air hunger”.16 The semantic structure of the MDP, that makes single items responsive to specific exposures, provides an option to relate the measures to literature. A trial including patients hospitalized with AECOPD from the same wards as our study found the fraction of time with SpO2<89% to be 42.9%, whereas the fraction of time with SpO2>92% was 10.5% when oxygen was administered by a nurse.5 Therefore, we believe that hypoxemia and oxygen under-treatment may be the main contributor to the intensity of breathing discomfort, the sensory predominance of air hunger, and the emotional response of anxiety, in hospitalized patients with AECOPD. The results from Hansen et al in combination with our results indicates a limited impact of hyperoxemia on dyspnea and anxiety. We believe this to be an important point, since hyperoxemia must be considered a therapeutic consequence of oxygen supplementation. A “side effect” identified across settings by several observational studies, showing a severe tendency of hyperoxygenation in patients hospitalized with AECOPD, increasing their risk of hypercapnic respiratory failure.46–49 The association between the fraction of time with hypoxemia or hyperoxemia and specific items on the MDP in patients admitted with AECOPD needs to be investigated further.
Dyspnea is a cardinal symptom of COPD, with a severe and debilitating impact on patients’ quality of life. The symptom is one of the main reasons for patients seeking hospital emergency units, and getting hospitalized, and it remains a major limit for discharging patients and it is a contributing cause of readmission. During admission the high intensity of dyspnea often requires nurse attention, interventions, and time. Alleviating dyspnea by AOA may therefore not only impact the patients’ quality of life, the length of hospital stays, and nurse resources, but may also be a potential palliative intervention across different etiologies.
Strength and Limitations
A main strength of our study is the multicenter RCT design. Further, the treatment groups were fairly balanced on key predictors of outcomes in patients with COPD reflecting a valid method of randomization, and we had a reasonable degree of follow-up. Patients recruited in our study were very ill and might have been excluded from participating in other randomized trials, and we find it a strength that we hereby contribute to solid data in a rigid design on these severely ill patients.
We prioritized to collect our data through individual interviews, not self-administration, and thereby we believe we have provided the study with data of high quality and completeness. To ensure this, some end-of intervention data were collected while the patient were still receiving the intervention (if the patients were back on the usual LTOT dose or if the patient had a need for supplemental oxygen throughout the intervention), while some were collected without the patient being connected to the device (if the patient had become normoxic and had weaned from oxygen, then the ward nurses would have disconnected the device) and the different procedures must be considered when interpreting the results. However, despite the different procedures for data collection, we do not think this procedure to have had an effect on our results, since our focus period is short, the risk of recall bias equally split between the two groups due to the randomized design, and the patients, although severely sick, were cognitive capable to provide clinically relevant PROMS. By describing both the physical and emotional dimensions of dyspnea, as an outcome of AOA, the study has provided a wide description of the impact of the intervention, which must be considered a strength.
Despite the strengths, some limitations deserve careful consideration. First, the open-labeled design may have been a limitation, as it may have biased the patients’ subjective experiences of the sensory and emotional aspects of dyspnea. Thus, the reduction seen on the anxiety item could be explained by this mechanism, but this remains speculative as the design does not provide further arguments to prove or disprove this assumption. It should be mentioned that dyspnea is by definition subjective and cannot be consistently measured, and that subjective data are more sensitive to open label originated biases. Also, the first author both enrolled patients in the study and collected the data, a combination that may have generated social-desirability bias. Our inclusion was somewhat slow, partly due to COVID-19 and partly due to NIV as an exclusion criteria. Nonetheless, we believe the risk of NIV therapy is generalizable across advance stages of COPD. Because we included a population of severely ill patients in an acute phase of their disease, fatigue, delirium, breathlessness, and terminal stage of disease were the main reasons for non-participation and loss to follow up, although this was at a reasonable level. Excluding the sickest and expectedly the population with the most severe symptoms may introduce selection bias and must be evaluated as a limitation of the study. Nonetheless, we consider these circumstances to be an unavoidable condition in any acute setting and a reflection of the reality we seek to mirror, and our results needs to be interpreted considering these limitations.
In conclusion, AOA reduces the overall breathing discomfort and the sensory dimension of dyspnea significantly, but not the emotional response or consumption of as-needed opioids or benzodiazepines, in patients hospitalized with AECOPD and hypoxemia.
The high intensity of dyspnea during admission often requires intense nurse interventions and time. Alleviating dyspnea by AOA may not only increase the patients’ quality of life, but may also reduce the length of hospital stays and the use of nurse resources.
Data Sharing Statement
The authors will share all study data. However, we must comply to national and international data regulations to protect patient's right to own data. Thus, scientists can approach the corresponding author with a plan, and we will do every effort to help formulating the request within legislative frames.
Ethics Approval and Informed Consent
All patients involved in the study signed an informed consent approved by the Capital Regions’ Committee on Health Research Ethics (H-17040114).
Consent for Publication
All authors involved in the study gave consent for publication.
Acknowledgments
The authors kindly thank the patients participating in this study and the contributing hospital wards, especially Dr. Imane Achir Alispahic, Dr. Claire Præst Holm and RN Silvia Lau Henriksen for their engagements.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
We thank the Niels Christian Nielsen Foundation, Danish Lung Association and Copenhagen University Hospital Hvidovre for supporting and financing this study.
Disclosure
O2matic Ltd has not been involved in the study. EFH is the main inventor of O2matic Ltd and a shareholder but has not been involved in data collection or analysis. The authors report no conflicts of interest in this work.
References
1. Halpin DMG, Miravitlles M, Metzdorf N, Celli B. Impact and prevention of severe exacerbations of COPD: a review of the evidence. Int J COPD. 2017;12:2891–2908. doi:10.2147/COPD.S139470
2. Halpin D, Hyland M, Blake S, et al. Understanding fear and anxiety in patients at the time of an exacerbation of chronic obstructive pulmonary disease : a qualitative study. JRSM Open. 2015;6(12):1–8. doi:10.1177/2054270415614543
3. Austin MA, Wills KE, Blizzard L, Walters EH, Wood-baker R. Effect of high flow oxygen on mortality in chronic obstructive randomised controlled trial. BMJ Res. 2010;34:1–8. doi:10.1136/bmj.c5462
4. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for prevention, diagnosis and management of COPD GOLD REPORT 2021; 2021.
5. Hansen FE, Ove JD, Bech CS, Kallemose T, Jensen J, Vestbo J. automated oxygen control with O2matic ® during admission with exacerbation of COPD. Int J COPD. 2018;13:3997–4003. doi:10.2147/COPD.S183762
6. Lellouche F, Bouchard P-A, Roberge M, et al. Automated oxygen titration and weaning with FreeO2 in patients with acute exacerbation of COPD: a pilot randomized trial. Int J COPD. 2016;11(1):1983–1990. doi:10.2147/COPD.S112820
7. Hansen EF, Bech CS, Vestbo J, Kofod LM, Kofod LM. Automatic oxygen titration with O2matic ® to patients admitted with COVID-19 and hypoxemic respiratory failure. Eur Clin Respir J. 2020;7(1):1–8. doi:10.1080/20018525.2020.1833695
8. L’Her E, Dias P, Gouillou M, et al. Automatic versus manual oxygen administration in the emergency department. Eur Respir J. 2017;50:1–9. doi:10.1183/13993003.02552-2016
9. Marciniuk D, Goodridge D, Hernandez P, et al. Managing dyspnea in patients with advanced chronic obstructive pulmonary disease : a Canadian Thoracic Society clinical practice guideline. Can Respir J. 2011;18(2):69–78. doi:10.1155/2011/745047
10. Parshall MB, Schwartzstein RM, Adams L, et al. American Thoracic Society documents an official American Thoracic Society Statement : update on the mechanisms, assessment, and management of dyspnea. American J Respir Crit Care Med. 2012;185:435–452. doi:10.1164/rccm.201111-2042ST
11. Pisani L, Hill NS, Pacilli AMG, Polastri M, Nava S. Management of dyspnea in the terminally ill. Chest. 2018;154(4):925–934. doi:10.1016/j.chest.2018.04.003
12. Global Initiative for Chronic Obstructive Pulmonary Disease. Global strategy for the diagnosis, management and prevention of COPD. GOLD-REPORT-2022; 2022. Available from: https://goldcopd.org/wp-content/uploads/2021/12/GOLD-REPORT-2022-v1.1-22Nov2021_WMV.pdf.
13. Mahler DA, Selecky PA, Harrod CG. Management of dyspnea in patients with advanced lung or heart disease. Practical guidance from the American College of Chest Physicians Consensus Statement. Chest J Am Coll Chest Physicians. 2010;120(5):160–166. doi:10.1378/chest.09-1543
14. Banzett RB, Donnell CRO, Guilfoyle TE, et al. Multidimensional Dyspnea Profile: an instrument for clinical and laboratory. Eur Respir J. 2015;45:1681–1691. doi:10.1183/09031936.00030115
15. Ekström M, Ahmadi Z, Abernethy A, Currow D. Oxygen for breathlessness in patients with chronic obstructive pulmonary disease who do not qualify for home oxygen therapy (Review) SUMMARY OF FINDINGS FOR THE MAIN COMPARISON. Cochrane Libr. 2016;(11). doi:10.1002/14651858.CD006429.pub3
16. Binks AP, Moosavi SH, Lansing RW, Golestanian E, Banzett RB, Brown R. Hypoxic and hypercapnic drives to breathe generate equivalent levels of air hunger in humans. J Appl Physiol. 2002;94(1):141–154. doi:10.1152/japplphysiol.00594.2002
17. O’Driscoll BR, Howard L, Earis J, et al. BTS guideline for oxygen use in adults in healthcare and emergency settings. Thorax an Int J Respir Med. 2017;72:1–100.
18. O’Donnell DE, Milne KM, James MD, de Torres JP, Neder JA. Dyspnea in COPD: new mechanistic insights and management implications. Adv Ther. 2020;37(1):41–60. doi:10.1007/s12325-019-01128-9
19. Clemens KE, Quednau I, Klaschik E. Use of oxygen and opioids in the palliation of dyspnoea in hypoxic and non-hypoxic palliative care patients: a prospective study. Support Care Cancer. 2009;17(4):367–377. doi:10.1007/s00520-008-0479-0
20. Bech CS, Noerholm V, Bové DG, Poulsen I. Danish translation and linguistic validation of the multidimensional dyspnea profile. Eur Clin Respir J. 2021;8(1). doi:10.1080/20018525.2021.1905498
21. Moosavi SH, Banzett RB, Butler JP, Moosavi SH, Banzett RB, Butler JP. Time course of air hunger mirrors the biphasic ventilatory response to hypoxia Time course of air hunger mirrors the biphasic ventilatory response to hypoxia. J Appl Physiol. 2005;97:2098–2103. doi:10.1152/japplphysiol.00056.2004
22. Jones P, Jenkins C, Bauerle O. Expert guidance on frequently asked questions: introducing the COPD Assessment TestTM (CAT). Respir Med. 2012;3:3–13.
23. Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34(3):648–654. doi:10.1183/09031936.00102509
24. Jones PW, Harding G, Berry P, et al. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34:648–654.
25. Bhandari NJ, Jain T, Marolda C, Zuwallack RL. Comprehensive pulmonary rehabilitation results in clinically meaningful improvements in anxiety and depression in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil Prev. 2013;33(2):123–127. doi:10.1097/HCR.0b013e31828254d4
26. Snaith RP. The Hospitals Anxiety and Depression Scale - Manual.
27. Meek PM, Banzett R, Parshall MB, Gracely RH, Schwartzstein RM, Lansing R. Reliability and validity of the multidimensional dyspnea profile. Chest. 2012;141(6):1546–1553. doi:10.1378/chest.11-1087
28. Ekström M, Bornefalk H, Sköld M, et al. Validation of the Swedish Multidimensional Dyspnea Profile (MDP) in outpatients with cardiorespiratory disease. BMJ Open Respir Res. 2019;6:1–9. doi:10.1136/bmjresp-2018-000381
29. Hegendörfer E, Doukhopelnikoff A, Degryse J-M. Validity and reliability of the Multidimensional Dyspnoea Profile in older adults. ERJ Open Res. 2021;7(2):00606–2020. doi:10.1183/23120541.00606-2020
30. Yang B, Parsha K, Schaar K, Xi X, Aronowski J, Savitz S. 乳鼠心肌提取 HHS public access [Hospitalist Attitudes towards the Assessment and Management of Dyspnea in Patients with Acute Cardiopulmonary Diseases]. Physiol Behav. 2016;176(1):139–148. Chinese. doi:10.1002/jhm.2422.Hospitalist
31. Ekström MP, Bornefalk H, Sköld CM, et al. Minimal clinically important differences and feasibility of dyspnea-12 and the multidimensional dyspnea profile in cardiorespiratory disease. J Pain Symptom Manage. 2020;60(5):968–975.e1. doi:10.1016/j.jpainsymman.2020.05.028
32. Gift AG. Validation of a vertical visual analogue scale as a measure of clinical dyspnea. Rehabil Nurs. 1987;14(6):323–325. doi:10.1002/j.2048-7940.1989.tb01129.x
33. Gift A, Narsavage G. Validity of the numeric rating scale of dyspnea. Am J Crit Care. 1998;7:200–204. doi:10.4037/ajcc1998.7.3.200
34. Ekström M, Johnson MJ, Huang C, Currow DC. Minimal clinically important differences in average, best, worst and current intensity and unpleasantness of chronic breathlessness. Eur Respir J. 2020;56(2):1–22. doi:10.1183/13993003.02202-2019
35. Kardos P, van der Molen T, Ferrer M, et al. Properties of the COPD assessment test in a cross-sectional European study. Eur Respir J. 2011;38(1):29–35. doi:10.1183/09031936.00177210
36. Jones PW, Tabberer M, Chen WH. Creating scenarios of the impact of COPD and their relationship to COPD assessment test (CATTM) scores. BMC Pulm Med. 2011;11(1):42. doi:10.1186/1471-2466-11-42
37. Pooler A, Beech R. Examining the relationship between anxiety and depression and exacerbations of COPD which result in hospital admission: a systematic review. Int J COPD. 2014;9:315–330. doi:10.2147/COPD.S53255
38. Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. J Psychosom Res. 2002;52(2):69–77. doi:10.1016/S0022-3999(01)00296-3
39. Smid DE, Franssen FME, Houben-Wilke S, et al. Responsiveness and MCID estimates for CAT, CCQ, and hads in patients with COPD undergoing pulmonary rehabilitation: a prospective analysis. J Am Med Dir Assoc. 2017;18(1):53–58. doi:10.1016/j.jamda.2016.08.002
40. Bove DG, Lomborg K, Jensen AK, Overgaard D, Lindhardt BØ, Midtgaard J. Ef fi cacy of a minimal home-based psychoeducative intervention in patients with advanced COPD : a randomised controlled trial. Respir Med. 2021;121(2016):109–116. doi:10.1016/j.rmed.2016.11.009
41. Puhan MA, Frey M, Büchi S, Schünemann H. The minimal important difference of the Hospital Anxiety and Depression Scale in patients with chron. Health Qual Life Outcomes. 2008;2(6):46. doi:10.1186/1477-7525-6-46
42. Beaumont M, Mialon P, Le BC, et al. Effects of inspiratory muscle training on dyspnoea in severe COPD patients during pulmonary rehabilitation : controlled randomised trial. Eur Respir J. 2018;25(51). doi:10.1183/13993003.01107-2017
43. R Core Team R. A language and environment for statistical computing; 2021. Available from: https://www.r-project.org/.
44. Stevens JP, Sheridan AR, Bernstein HB, et al. A multidimensional profile of dyspnea in hospitalized patients. Chest. 2019;156(3):507–517. doi:10.1016/j.chest.2019.04.128
45. Banzett RB, Pedersen SH, Schwartzstein RM, Lansing RW. The affective dimension of laboratory dyspnea: air hunger is more unpleasant than work/effort. Am J Respir Crit Care Med. 2008;177(12):1384–1390. doi:10.1164/rccm.200711-1675OC
46. Devoe NC, Kyriazis P, Eltanbedawi A, et al. An audit of oxygen supplementation in a large tertiary hospital – we should treat oxygen as any other drug. Hosp Pract. 2020:1–4. doi:10.1080/21548331.2020.1845018
47. Barrett R, Catangui E, Scott R, Barrett R, Catangui E, Scott R. Expert Review of Respiratory Medicine Acute oxygen therapy : a cross-sectional study of prescribing practices at an English hospital immediately before COVID-19 pandemic hospital immediately before COVID-19 pandemic. Expert Rev Respir Med. 2021;15(2):277–284. doi:10.1080/17476348.2021.1826316
48. Deshpande S, Datey N, Liacos A, Joosten SA, Leong P. Acute oxygen use in hospitalised patients with chronic obstructive pulmonary disease is guideline discordant. Int Med J. 2021;51:780–783. doi:10.1111/imj.15318
49. De C, Wa B, Holbourn A, Wong J. Oxygen prescribing practice at Waikato Hospital does not meet guideline recommendations. Intern Med J. 2014;44:1231–1234. doi:10.1111/imj.12602
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.