Back to Journals » Neuropsychiatric Disease and Treatment » Volume 19
Associations Between the Suicidal Ideation and the Tolerance for Psychological Pain and Tolerance for Physical Pain in Patients Diagnosed with Major Depressive Disorder
Authors Yeşiloğlu C , Tamam L , Demirkol ME , Namlı Z , Karaytuğ MO
Received 11 July 2023
Accepted for publication 17 October 2023
Published 25 October 2023 Volume 2023:19 Pages 2283—2294
DOI https://doi.org/10.2147/NDT.S430139
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Roger Pinder
Caner Yeşiloğlu,1 Lut Tamam,2 Mehmet Emin Demirkol,2 Zeynep Namlı,2 Mahmut Onur Karaytuğ2
1Department of Psychiatry, Kırşehir Training and Research Hospital, Kırşehir, Turkey; 2Department of Psychiatry, Çukurova University, School of Medicine, Adana, Turkey
Correspondence: Mehmet Emin Demirkol, Department of Psychiatry, Çukurova University, School of Medicine, Adana, Turkey, Email [email protected]
Purpose: Patients with major depressive disorder (MDD) may experience more frequent and severe psychological and physical pain complaints compared to those without depression. As the tolerance to psychological pain decreases in patients with MDD, the severity of suicidal ideation tends to increase. Furthermore, the tolerance for physical pain (TPP) has been related with suicidal behavior. We aimed to demonstrate the impact of TPP on suicidal ideation in patients with MDD in the presence of psychological pain.
Patients and Methods: We included 123 patients with MDD and 114 healthy volunteers who had no previous psychiatric diagnosis. Sociodemographic data form, Psychache Scale (PS) and Tolerance for Mental Pain Scale (TMPS) were used to assess psychological pain. Beck Scale for Suicide Ideation (BSIS) and Beck Depression Inventory (BDI) were administered to participants. To assess the TPP, we used a device based on the principle of electronic dynamometry.
Results: The mean BDI, BSIS, PS, and TPP scores in the MDD group were higher, and the mean TMPS score was lower than those in the control group (p < 0.001 for each, p = 0.03 for TPP). We found statistically significant correlations between BDI, TMPS, BSIS, PS, and TPP scores (p < 0.05 for each). TPP was a partial mediator in the relationship between TMPS and BSIS scores (β = − 1.814; p < 0.001).
Conclusion: We found that tolerance of psychological pain was a strong predictor of suicidal ideation, and TPP was mediating this relationship. These findings suggest that considering both tolerance to psychological pain and TPP may be beneficial when assessing the risk of suicide in individuals with MDD.
Keywords: depression, tolerance of psychological pain, tolerance of physical pain, psychache, suicide
Introduction
Major depressive disorder (MDD) is a common psychiatric disorder that is associated with high morbidity and mortality. MDD is characterized by a depressive mood, loss of interest and desire, difficulty paying attention, lack of energy, and additional somatic symptoms; these symptoms tend to persist and drive patients to seek medical attention. Approximately 65% of patients with MDD experience a painful condition during their lifetime compared to 29% of those without depression.1 Patients with MDD may complain of more severe pain in more body parts than those without it. Similarly, the incidence of MDD in people with continuous pain is four times higher than that in those without pain.2 Chronic pain has been proposed as a risk factor for MDD.3
In addition to biological mechanisms, such as inflammatory processes, changes in melatonin levels, dysregulation of neurotransmitters, and oxidative stress, psychosocial factors like low self-esteem, decreased self-reliance, anger management issues, and a history of sexual abuse may play a role in the etiopathogenesis of pain.4–6 These aforementioned factors also play a role in the etiopathogenesis of MDD.7 Cognitive variables, including pessimism, fear-avoidance, and perception of insufficient support, mediate the relationship between pain and depression.8,9
Conflicting results have been reported in studies on physical pain threshold and tolerance in patients with MDD. Marsala et al demonstrated reduced physical pain tolerance to electrical stimuli in patients with MDD.10 Bar et al reported a lower tolerance level for ischemic pain in patients with MDD compared to healthy controls.11 Dickens et al reported that pain perceived by individuals with depression was milder than that perceived by the healthy population; furthermore, intergroup comparisons for pressure, thermal, and cold pain perception revealed that pressure and cold pain thresholds were higher in patients with MDD than in healthy controls.12
Franklin reported that the association between painful events and acquiring the capability for suicide might be explained by tolerance for physical pain.13 Dodd et al demonstrated a positive correlation between resilience toward physical pain and suicidal behavior.14 Although the association between the tolerance for physical pain and suicidal behavior has been reported previously, the psychological implications of tolerance toward physical pain have not been evaluated.15 Orbach suggested that an increased tolerance for physical pain alone might not be a determinant of a suicide attempt, but an increased pain tolerance might facilitate suicidal behavior in the presence of other psychological risk factors for suicide, such as depression, psychological pain, and hopelessness.16
MDD and perception of psychache are the potential predictors of suicide.17 Shneidman defined psychache as a psychological pain associated with a negative inner experience including feelings of guilt, shame, helplessness, and grief.18 Psychache is felt more intense than the pain associated with depression and emerges when the basic psychosocial needs are not satisfied.19 Meerwijck reported that suicide ideation cannot occur without psychache; however, the inability to tolerate psychache—rather than the intensity of psychache—promotes suicidal ideation.20
Many theories have been proposed on suicide. Shneidman’s theory of psychological pain explains the internal conflicts and suffering processes that lead to suicidal thoughts and behaviors. A lack of meaning in life, hopelessness, and psychological distress are the main factors in psychological pain theory, and there would be no suicide without psychache.15 Orbach has suggested that a person experiencing psychological pain will withdraw from communication and become isolated. Furthermore, due to escalating psychological pain, life appears meaningless to the patient, leading to contemplation regarding ending their life to alleviate the suffering. Pompili reported that feelings of worthlessness, hopelessness, and helplessness are associated with suicide in patients with MDD and that the risk of suicide increases as the duration of the disorder increases, symptoms become heightened, and the response to treatment decreases. Moreover, Pompili suggested that psychological pain intensifies in patients with depression and that they consider life meaningless and tedious due to psychological pain. According to Joiner’s interpersonal theory of suicidal Behavior (ITPS), the main components of suicidality are the desire to die and suicidal capability. ITPS consists of the desire for suicide, which refers to a person’s state of having suicidal thoughts and desires; perceived acceptability of suicide, which refers to a situation in which a person accepts suicidal thoughts as usual; and capability for suicide, which refers to a person’s ability to commit suicide. Consequently, the risk of suicide is increased if a person has a high level of suicidal desire and acceptability and has developed suicidal functioning. The capability for suicide develops with increased tolerance to physical pain and insensitivity to fear.21,22 Psychache, tolerance for psychache, and hardiness of physical pain are the risk factors of suicide. However, possible interactions between these risk factors remain unclear.
The primary objective of this study, which evaluated 237 participants using the Psychache Scale (PS), Tolerance for Mental Pain Scale (TMPS), Beck Scale for Suicidal Ideation (BSIS), Beck Depression Inventory (BDI), and tolerance of physical pain in a cross-sectional design was to investigate a mediator role of tolerance toward physical pain in the relationship between tolerance for psychache and suicide. We hypothesized that suicidal thoughts would increase with increasing tolerances toward psychache and physical pain. Our secondary objective was to compare the risk factors, including tolerance for physical pain, tolerance for psychache, and severity of depressive symptoms, in terms of their effects on suicidal ideation. We hypothesized that, among all risk factors, tolerance for psychache is the strongest determinant of suicide. The tertiary objective of our study was to investigate whether tolerance toward physical pain increased in participants with MDD. We hypothesized that tolerance for physical pain would increase in participants with severe depressive symptoms.
Although the cross-sectional design of the study and the measurement of tolerance to physical pain using only the pressure method limit our findings, we believe that our results contribute to a more precise assessment of suicidal thoughts.
Materials and Methods
Sample
This study included 123 participants who attended Psychiatry Clinics of Balcalı Hospital at the Medical School of Çukurova University between January 2023 and April 2023. Participants were aged 18–65 years, literate, and diagnosed with MDD based on Diagnostic Statistical Manual of Mental Disorders, 5th edition (DSM-5) criteria. Patients who were being treated with only selective serotonin-reuptake inhibitors (SSRIs) were included in the study. The control group included 114 healthy hospital employees and their relatives with no previous diagnosis of psychiatric disorders and whose sociodemographic characteristics matched those of the participants in the MDD group. The exclusion criteria included a diagnosis of upper limb neuropathies or disc herniations that could result in hypoalgesia, dermatoses, or endocrine disorders, which were identified from the participants’ health records.
The participants were informed about the purpose of the study. Participants underwent a 45-minute interview using the Structured Clinical Interview for DSM-5 Disorders – Clinical Version (SCID-5-CV). We employed a sociodemographic and clinical data form to assess sociodemographic and clinical characteristics. We evaluated psychache using PS, TMPS and the severity of depressive symptoms and suicidal ideation using BDI and BSIS. The interviewer explained questions that the participants did not understand.
To assess the pressure pain tolerance, we used a digital dynamometer with alternating pressure and a base plate’s surface of “0.8 cm2” with a measurement range of “0–17 kg” (Force Ten FDX Compact; Wagner Instruments; Greenwich, CT, USA). For the first trial, we placed the plate on the forearm on the dominant side between the proximal skin crease of the wrist and the transverse crease of the inner elbow. During the second and third trials, we placed the plate slightly distal or proximal to the initial measurement site to minimize hyperalgesia. The investigator was trained to increase the pressure at a constant rate of 10 N/s until the participants indicated perception of pain. The threshold value was calculated as the average of the three trials.23
In the MDD group, five participants (two with obsessive-compulsive disorder and three with panic disorder) were excluded from the study to avoid the confounding effects of comorbid conditions. Additionally, five participants were excluded from the study because they did not fill out the questionnaires. In the control group, three participants diagnosed with MMD and three with generalized anxiety disorder were excluded from the study along with two who did not complete the questionnaires. Overall, 113 participants with MDD and 106 healthy controls were included in this study. The study was approved by the Non-Interventional Clinical Research Ethics Committee of the Medical School of Çukurova University (decision no. 44; dated January 6). All the participants provided written informed consent. This study was conducted in accordance with the principles of the Declaration of Helsinki.
Measures
Sociodemographic and Clinical Data Form
Data regarding age, sex, educational qualification, occupational status, family history of mental disorders, physical illness, and suicide attempts were collected.
Psychache Scale (PS)
The PS is a 13-item self-report scale for adults. This Likert scale assesses psychological pain based on responses ranging from “never” to “always” or “I totally disagree” to “I totally agree”. Higher total scores indicate more severe psychological pain.24 Demirkol et al revealed that the Cronbach’s alpha value of the Turkish version of the scale was 0.98.25 In our study, the Cronbach’s alpha coefficient was 0.96.
Tolerance for Mental Pain Scale (TMPS-10)
TMPS-10 aims to assess the degree of the ability to tolerate psychological pain since it differs between persons and is important in determining the risk of suicide. This is a 5-item Likert scale ranging from 1 (not true at all) to 5 (very true)20,26 with higher scores indicating better tolerance for psychological pain. The Cronbach’s alpha of the Turkish version is 0.98,27 whereas that of the scale in our study was 0.78.
Beck Scale for Suicidal Ideation (BSIS)
BSIS was developed to determine the severity, properties, feasibility, and factors that contribute to suicidal ideation. It is a 24-item scale with item scores ranging from 0 to 2. The scale includes five subtitles: the responder’s thoughts on living or dying, features of suicidal ideation, planned suicide attempts, background factors, and features of planned suicide attempts and committing suicide. Higher total scores indicate more severe suicidal ideation.28 Ozcelik et al evaluated the validity and reliability of the Turkish version of the scale and reported a Cronbach’s alpha of 0.84.29
Beck Depression Inventory (BDI)
BDI is a 21-item self-report inventory that assesses the severity of depressive symptoms using a 4-point Likert scale. Higher scores indicate more severe depressive symptoms.30 Its Cronbach alpha was found to be 0.80 by Hisli who determined the validity and reliability of the Turkish version of the inventory.31
Statistical Analysis
We analyzed the data using SPSS 24.0. As the study sample size was within the range of 50–300 participants, the distribution of the variables was considered to be normal based on the histograms and if the skewness and kurtosis values were between –1.5 and 1.5 and z-scores varied from –3.29 to 3.29.32 The t-test was used to determine if there was a significant difference in the means of normally distributed variables between the two independent groups. The data are presented as mean ± standard deviation (SD). The Mann–Whitney U-test was used to determine whether there was a significant intergroup difference in the medians of non-normally distributed variables. Data are presented as median and interquartile range (medians [1st–3rd quartile]).33
Fisher’s exact test was used to analyze the associations between categorical variables when the number of observations was less than five. Yate’s statistical method was used if the number of observations ranged between 5 and 25, and the Chi-square test was used in other situations. Data are presented as percentages and frequencies.
Pearson’s correlation test was used to analyze correlations between normally distributed numerical variables, and Spearman correlation analysis was used for correlations between non-normally distributed numerical variables.33 The effect sizes for independent groups t-test and Mann–Whitney test were calculated using R (R Foundation for Statistical Computing, Vienna, Austria). BSIS-dependent variables were chosen for multiple linear regression analysis in the MDD group, and all the requirements for using a multiple linear regression model were satisfied.
Analyses were conducted, and data were modeled to determine whether there was a mediating effect of tolerance for physical pain between BDI and BSIS scores, tolerance for physical pain between TMPS and BSIS scores, tolerance for physical pain between PS and BSIS scores, and TMPS scores between BDI and BSIS scores. The mediating effects were investigated using the SPSS Process Macro extension developed by Hayes.34
The bootstrap method (bootstrap 5000) and the maximum likelihood parameter estimation method were used in the mediation analysis. First, we tested whether the outer variable significantly predicted the inner variable in a simple model before including the mediator in the analysis. The mediating variable was then included in the model and its direct and indirect effects were analyzed. The inner and outer variables were continuous in both mediation analyses. Statistical significance was set at p <0.05.
Results
Table 1 shows the sociodemographic characteristics of the participants. We found no significant intergroup differences in the demographic variables. As shown in Table 2, BDI, BSIS, PS, and TMPS scores, and tolerance for physical pain in the MDD group were significantly higher than those in the control group (p <0.001 for each, p = 0.003 for physical pain tolerance). As shown in Table 3, tolerance of physical pain scores significantly correlated with BDI, BSIS, PS, and TMPS scores. We assessed the scales that were significantly related to the BSIS scores using regression analysis, as presented in Table 4. The TMPS scores demonstrated the strongest relationship with the BSIS scores.
 |
Table 1 Socio-Demographic Characteristics |
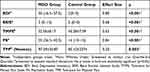 |
Table 2 Scale Scores of Participants |
 |
Table 3 Correlations Among the Scale Scores in Patients with Major Depressive Disorders |
 |
Table 4 Regression Analysis of Variables Contributing to Suicidal Thoughts |
We found no significant differences in the mean age, mean years of education, and marital status between participants who had a history of suicide attempts and those who did not in the MDD group. However, the median disease duration significantly differed between participants who had a history of suicide attempts and those who did not (p <0.001); the mean disease duration was longer in participants who had a history of suicide. We noted no significant differences in BSIS scores between male and female participants (p = 0.40). We found no significant differences in the tolerance to physical pain between male and female participants (p = 0.071). Table 5 presents the mediating effect of tolerance toward physical pain on BDI and BSIS scores in the MDD group.
 |
Table 5 The Mediating Effect of Tolerance Toward Physical Pain on Beck Depression Inventory and Beck Suicidal Ideation Scale Scores in the MDD Group |
Before including the tolerance for physical pain, BDI scores had a positive and significant effect on the BSIS scores (β = 0.322; p <0.001). After including the tolerance for physical pain, BDI predicted the tolerance for physical pain (β = 0.826; p = 0.0001), and the tolerance for physical pain predicted BSIS (β = 0.099; p <0.001). We modelled the mediation using a path diagram. Figure 1 shows the mediating effects of BDI and BSIS scores and tolerance for physical pain measurements. Table 6 summarizes the mediating effects of tolerance to physical pain on TMPS and BSIS scores in the MDD group. The following analysis was performed to test this hypothesis.
 |
Table 6 The Mediating Effects of Tolerance for Physical Pain on Tolerance for Mental Pain Scale Scores and Beck Suicidal Ideation Scale Scores in the MDD Group |
 |
Figure 1 Mediating effect of the tolerance for physical pain between BDI scores and BSIS scores in the MDD group. |
Before including the tolerance for physical pain, TMPS scores had a negative and significant impact on the BSIS (β = –0.757; p <0.001). After including the tolerance for physical pain, the TMPS predicted the tolerance for physical pain (β = –1.814; p <0.001), and the tolerance for physical pain predicted the BSIS scores (β = –0.639; p <0.001). The mediating effects of the TMPS and BSIS scores and tolerance for physical pain measurements are shown in Figure 2.
 |
Figure 2 Mediating effect of the tolerance for physical pain between TMPS scores and BSIS scores in the MDD group. |
We found no significant differences in the mean age, mean years of schooling, and marital status between participants who had a history of suicide attempts and those who did not in the MDD group. However, the median disease duration significantly differed between participants who had a history of suicide attempts and those who did not (p <0.001); the mean disease duration was longer in participants who had a history of suicide attempts. We found no significant differences in BSIS scores between male and female participants (p = 0.40). No significant differences were found in the tolerance to physical pain between male and female participants (p = 0.071).
In summary, the MDD group had significantly higher mean BDI, BSIS, PS, and physical pain tolerance scores than the control group. Conversely, the mean TMPS score in the MDD group was significantly lower than that in the control group. We also discovered statistically significant correlations between BDI, TMPS, BSIS, and PS scores and tolerance for physical pain. Additionally, we found a mediating role for physical pain tolerance in the relationship between TMPS and BSIS scores.
Discussion
Patients with MDD may engage in suicidal thoughts to eliminate psychological pain. Suicidal thoughts may intensify when the psychological pain becomes unbearable. Although intolerance to psychological pain is a risk factor for suicide, it is not the only predictor of the latter.35,36 The most important outcome of this study was that the severity of suicidal thoughts was directly and indirectly related to the tolerance toward psychache through the mediation of tolerance toward physical pain. This study also demonstrated the mediating role of physical pain tolerance in the relationship between depressive symptom severity, psychache intensity, and suicidality.
Psychache may be defined as psychological pain felt as negative experiences, such as guilt, shame, helplessness, and angst.36 Depressive symptoms may be more severe in patients with MDD who experience intensive psychache or have a lower tolerance for psychological pain.37–41 In line with previous studies, we revealed that patients with MDD had heightened depressive symptoms when experiencing more intense psychache or lower psychological pain tolerance.
Depressive disorders are associated with an increased secretion of excitatory neuromodulators, such as substance P, and decreased blood flow to the caudate nuclei and thalamic areas that are involved in the central processing of stimuli.7,42 The etiology of depression and physical pain often includes similar circumstantial factors such as childhood traumas, primitive defense mechanisms, and negative cognitions.42
Depression is associated with an increased perception of physical pain, whereas prolonged acute pain may lead to mood dysregulation. Although the pain sensitivity is higher in patients with MDD, the results of induced pain sensitivity remain conflicting.43 Klatzkin et al reported that tolerance for physical pain caused by cold or pressure stimuli might be increased in patients with MDD.44 Bar et al evaluated 30 patients with MDD and healthy controls in terms of endurance by inducing thermal, electrical, and ischemic pain; they detected hypoalgesia due to heat and electrical pain and hyperalgesia due to ischemic pain in the MDD group, which demonstrated that painful stimuli are processed differently.11 However, Schaible reported a decreased or unchanged sensitivity to thermal, cold, or electrical stimuli and an increased sensitivity to intense ischemic pain in patients with MDD.45 Our study demonstrated that the tolerance for pressure pain increased as the severity of depressive symptoms increased, which may be caused by the activation of low-density peripheral pain pathways by pressure stimuli and decreased neurochemical sensitivity.46 In addition to sensory stimuli, pain is an emotional and cognitive experience. Our results are consistent with those of a study that reported decreased sensitivity to low-intensity pain with increasing symptom severity in patients with MDD.1,47
Several biological, genetic, and psychosocial hypotheses have been proposed to explain suicide. According to ITPS, suicidal desire and capability increase the suicide risk. A person’s state of suicidal thoughts and desires, normalization of suicidal ideation, and ability to commit suicide are the main factors in suicidality. Suicide capability increases as the tolerance for physical pain increases.21,48 A study on the relationship between suicide capability, painful event history, and pressure and pain induction in undergraduate students found that suicide capability was moderately correlated with the tolerance for physical pain and the risk for suicide.22,48,49 Although an increased tolerance for physical pain is a risk factor for suicide, it cannot lead to a suicide attempt without suicidal ideation.48 Based on previous studies, we assessed the associations between resilience for physical pain, tolerance for psychache, and suicidal thoughts and demonstrated the partial mediating role of increased tolerance for physical pain in the relationship between tolerance to psychache and suicidal thoughts. We also demonstrated that tolerance of physical pain mediated the relationship between depression severity and suicide. Our results can also be explained by the hypothesis that repeated exposure to frustrating and physically painful stimuli desensitizes the harm avoidance response and normalizes the feelings of physical pain, fear, and suicidal thoughts.50
Previous studies have demonstrated that increases in the intensity of psychological pain, severity of depression, and ability to tolerate physical pain and a reduction in the ability to tolerate psychological pain might increase suicidal thoughts.20,21,51,52 Our study demonstrated associations between increased suicidal thoughts and increases in the intensity of psychological pain and inability to tolerate psychological pain, increase in the severity of depressive symptoms, and ability to tolerate physical pain as well as a prolonged duration of the disease in patients with MDD. None of these risk factors were predominant over the others. Tolerance of psychological pain demonstrated the strongest association with suicidal thoughts. This finding further supports the hypothesis that suicidal thoughts do not occur without unbearable psychological pain.18
Although the pathophysiological basis of the differences between sexes in pain tolerance has not been clearly established, it has been demonstrated that the pain thresholds were lower and the frequency of pain symptoms was higher in women than those in men.42,53–55 Our study demonstrated that the threshold of tolerance for physical pain was higher in men than that in women; however, the difference was not statistically significant. The results of our study can be explained by the similarity in the biological basis of tolerance of physical pain between men and women. Results from previous studies have explained this phenomenon as pain control efforts in male participants in the societies in which those studies were conducted.56
The results of this study have several practical implications. Implementing strategies to manage psychological pain in patients with MDD may reduce their risk of suicide. Zou et al supported the effectiveness of cognitive therapy based on the psychological pain theory, which consists of identifying the underlying cognitive biases and applying cognitive reframing and problem-solving to increase motivation and improve social relationships.57 Zou et al also suggested that correcting cognitive distortions in patients with depression and replacing them with more appropriate coping methods based on psychological pain theory may reduce the risk of suicide.57
Patients with severe depressive symptoms or those who cannot tolerate psychological pain and avoid activities that would increase their tolerance for physical pain may experience a positive effect on suicidal thoughts. High-risk sports activities, self-mutilation, and non-life-threatening accidental injuries could increase the tolerance for physical pain and suicide capability.50 Clinicians should prioritize suicide prevention efforts in patients by addressing their tolerance for physical pain and emotional support.
This study had some limitations. We did not assess the severity of suicidal thoughts. Future research may benefit from a comprehensive assessment of suicidal thoughts using scales, such as the Columbia Suicide Severity Rating Scale. The pressure method was used to evaluate acute pain tolerance. Using multiple pain tolerance assessment methods may have increased the generalizability of our findings. We suggest assessing pain tolerance using electrical, heat, and cold stimulations to identify the potential differences between these methods. We performed mediation analysis using a cross-sectional design, which is generally used to assess longitudinal processes. Future studies may need to overcome these limitations. We investigated the relationship between physical pain tolerance and suicidality in patients with MDD. Future studies should evaluate these variables in patients with various mental disorders, such as schizophrenia, obsessive-compulsive disorder, bipolar disorder, and panic disorder, which will increase the generalizability of our findings. Although this study addressed inter-sex differences in pain tolerance, the pathophysiological basis remains unclear. This limitation can be overcome by considering the biological and psychological variables that may explain the differences between the sexes.
Estimating the likelihood of suicide can be achieved to a certain extent by considering various risk factors, such as prior suicide attempts, childhood traumas, and alcohol/substance abuse. Suicide risk is influenced by a multitude of factors, including biological elements, such as genetic and neurochemical parameters; clinical factors, such as mental and physical disorders; social factors, such as living conditions and economic hardships; and psychological factors, such as depression, hopelessness, and psychological distress. However, the prediction of suicidal behavior remains complex and intricate. It is worth noting that these risk factors typically encompass long-term behavioral risks rather than immediate ones, which adds to the complexity of prediction. The results of our study revealed the effects of physical pain tolerance on suicidal thoughts and provided a biological marker that can be used to evaluate patients at risk of suicide. Moreover, our results revealed that known psychological risk factors for suicide, along with biological and interview-measurable markers, such as tolerance to physical pain, are influential in suicidal ideation.38
Conclusion
Despite the increasing number of treatment options, the absence of a decrease in suicide rates necessitates the evaluation of suicide from new perspectives. Tolerance of psychological pain is strongly related to suicidal ideation, and tolerance of physical pain plays a partial mediating role in this relationship. In patients with depression and a history of suicidal ideation, screening for the presence of TTP will help identify those at risk for suicide. These findings suggest that considering both tolerance for psychological and physical pain may be beneficial for assessing the risk of suicide in individuals with MDD.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Thompson T, Correll CU, Gallop K, Vancampfort D, Stubbs B. Is pain perception altered in people with depression? A systematic review and meta-analysis of experimental pain research. J Pain. 2016;17(12):1257–1272. doi:10.1016/j.jpain.2016.08.007
2. Lépine JP, Briley M. The increasing burden of depression. Neuropsychiatr Dis Treat. 2011;7(Suppl 1):3–7. doi:10.2147/NDT.S19617
3. Ratcliffe GE, Enns MW, Belik SL, Sareen J. Chronic pain conditions and suicidal ideation and suicide attempts: an epidemiologic perspective. Clin J Pain. 2008;24(3):204–210. doi:10.1097/AJP.0b013e31815ca2a3
4. Scott KM, Von Korff M, Angermeyer MC, et al. Association of childhood adversities and early-onset mental disorders with adult-onset chronic physical conditions. Arch Gen Psychiatry. 2011;68(8):838–844. doi:10.1001/archgenpsychiatry.2011.77
5. Jang JM, Park JI, Oh KY, et al. Predictors of suicidal ideation in a community sample: roles of anger, self-esteem, and depression. Psychiatry Res. 2014;216(1):74–81. doi:10.1016/j.psychres.2013.12.054
6. Friborg O, Martinsen EW, Martinussen M, Kaiser S, Øvergård KT, Rosenvinge JH. Comorbidity of personality disorders in mood disorders: a meta-analytic review of 122 studies from 1988 to 2010. J Affect Disord. 2014;152:1–11. doi:10.1016/j.jad.2013.08.023
7. Han C, Pae CU. Pain and depression: a neurobiological perspective of their relationship. Psychiatry Investig. 2015;12(1):1–8. doi:10.4306/pi.2015.12.1.1
8. Goesling J, Clauw DJ, Hassett AL. Pain and depression: an integrative review of neurobiological and psychological factors. Curr Psychiatry Rep. 2013;15(12):1–8. doi:10.1007/s11920-013-0421-0
9. Philips HC. Imagery and likelihood cognitive bias in pain. Behav Cogn Psychother. 2015;43(3):270–284. doi:10.1017/S1352465813000982
10. Marsala SZ, Pistacchi M, Tocco P, et al. Pain perception in major depressive disorder: a neurophysiological case–control study. J Neurol Sci. 2015;357(1–2):19–21. doi:10.1016/j.jns.2015.06.051
11. Bär KJ, Brehm S, Boettger MK, Boettger S, Wagner G, Sauer H. Pain perception in major depression depends on pain modality. Pain. 2005;117(1–2):97–103. doi:10.1016/j.pain.2005.05.016
12. Dickens C, McGowan L, Dale S. Impact of depression on experimental pain perception: a systematic review of the literature with meta-analysis. Psychosom Med. 2003;65(3):369–375. doi:10.1097/01.PSY.0000041622.69462.06
13. Franklin JC, Hessel ET, Prinstein MJ. Clarifying the role of pain tolerance in suicidal capability. Psychiatry Res. 2011;189(3):362–367. doi:10.1016/j.psychres.2011.08.001
14. Dodd DR, Smith AR, Forrest LN, et al. Interoceptive deficits, nonsuicidal self‐injury, and suicide attempts among women with eating disorders. Suicide Life Threat Behav. 2018;48(4):438–448. doi:10.1111/sltb.12383
15. Rabasco A, Andover MS. The interaction of dissociation, pain tolerance, and suicidal ideation in predicting suicide attempts. Psychiatry Res. 2020;284:112661. doi:10.1016/j.psychres.2019.112661
16. Orbach I. Dissociation, physical pain, and suicide: a hypothesis. Suicide Life Threat Behav. 1994;24(1):68–79.
17. Lambert CE, Troister T, Ramadan Z, Montemarano V, Fekken GC, Holden RR. Psychache predicts suicide attempter status change in students starting university. Suicide Life Threat Behav. 2020;50(3):668–678. doi:10.1111/sltb.12624
18. Shneidman ES. Commentary: suicide as psychache. J Nerv Ment Dis. 1993;181(3):145–147. doi:10.1097/00005053-199303000-00001
19. Campos RC, Gomes M, Holden RR, Piteira M, Rainha A. Does psychache mediate the relationship between general distress and suicide ideation? Death Stud. 2017;41(4):241–245. doi:10.1080/07481187.2016.1251510
20. Meerwijk EL, Mikulincer M, Weiss SJ. Psychometric evaluation of the Tolerance for Mental Pain Scale in United States adults. Psychiatry Res. 2019;273:746–752. doi:10.1016/j.psychres.2019.01.101
21. Van Orden KA, Witte TK, Gordon KH, Bender TW, Joiner TE. Suicidal desire and the capability for suicide: tests of the interpersonal-psychological theory of suicidal behavior among adults. J Consult Clin Psychol. 2008;76(1):72. doi:10.1037/0022-006X.76.1.72
22. Bender TW, Gordon KH, Bresin K, Joiner TE. Impulsivity and suicidality: the mediating role of painful and provocative experiences. J Affect Disord. 2011;129(1–3):301–307. doi:10.1016/j.jad.2010.07.023
23. Fischer AA. Pressure algometry over normal muscles. Standard values, validity and reproducibility of pressure threshold. Pain. 1987;30(1):115–126. doi:10.1016/0304-3959(87)90089-3
24. Holden RR, Mehta K, Cunningham EJ, McLeod LD. Development and preliminary validation of a scale of psychache. Can J Behav Sci. 2001;33(4):224. doi:10.1037/h0087144
25. Demirkol ME, Güleç H, Çakmak S, et al. Psikolojik Acı Ölçeği Türkçe Formunun güvenilirliği ve geçerliliği. Anadolu Psikiyatri Derg. 2018;19:14–20.
26. Orbach I, Gilboa-Schechtman E, Johan M, Mikulincer M. Tolerance for mental pain scale. J Nerv Ment Dis. 2004;10:782–788.
27. Demirkol ME, Tamam L, Namlı Z, Eriş Davul Ö. Validity and reliability study of the Turkish version of the tolerance for mental pain scale-10. Psychiatry Clin Psychopharmacol. 2019;29(4):899–906. doi:10.1080/24750573.2019.1699309
28. Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47(2):343. doi:10.1037/0022-006X.47.2.343
29. Ozcelik HS, Ozdel K, Bulut SD, Orsel S. The reliability and validity of the Turkish version of the Beck Scale for Suicide Ideation (Turkish BSSI). Bull Clin Psychopharmacol. 2015;25(2):141–150. doi:10.5455/bcp.20141214105009
30. Beck AT, Steer RA. Internal consistencies of the original and revised Beck Depression Inventory. J Clin Psychol. 1984;40(6):1365–1367. doi:10.1002/1097-4679(198411)40:6<1365::AID-JCLP2270400615>3.0.CO;2-D
31. Hisli N. Beck Depresyon Envanterinin gecerliligi uzerine bit calisma (A study on the validity of Beck Depression Inventory.). Psikoloji Dergisi. 1988;6:118–122.
32. Tabachnick BG, Fidell LS. Using Multivariate Statistics: International Edition. Pearson; 2012.
33. Field A. Discovering Statistics Using IBM SPSS Statistics. Sage; 2013.
34. Hayes AF. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. Guilford Press; 2013.
35. Meerwijk EL, Weiss SJ. Tolerance for psychological pain and capability for suicide: contributions to suicidal ideation and behavior. Psychiatry Res. 2018;262:203–208. doi:10.1016/j.psychres.2018.02.005
36. Namlı Z, Demirkol ME, Tamam L, Karaytuğ MO, Yeşiloğlu C. Validity and reliability study of the Turkish version of the unbearable Psychache scale. Alpha Psychiatr. 2022;23(4):166. doi:10.5152/alphapsychiatry.2022.21604
37. Landi G, Furlani A, Boccolini G, Mikulincer M, Grandi S, Tossani E. Tolerance for Mental Pain Scale (TMPS): Italian validation and evaluation of its protective role in depression and suicidal ideation. Psychiatry Res. 2020;291:113263. doi:10.1016/j.psychres.2020.113263
38. Orbach I, Mikulincer M, Sirota P, Gilboa-Schechtman E Mental pain: a multidimensional operationalization and definition. Suicide Life Threat Behav. 2003;33(3):219–230.
39. Demirkol ME, Namlı Z, Tamam L. Psikolojik Acı. Curr Approaches Psychiatry. 2019;11(2):1.
40. Mee S, Bunney BG, Reist C, Potkin SG, Bunney WE. Psychological pain: a review of evidence. J Psychiatr Res. 2006;40(8):680–690. doi:10.1016/j.jpsychires.2006.03.003
41. Demirkol ME, Tamam L, Namlı Z, Karaytuğ MO, Uğur K. Association of psychache and alexithymia with suicide in patients with schizophrenia. J Nerv Ment Dis. 2019;207(8):668–674. doi:10.1097/NMD.0000000000001023
42. Euteneuer F, Schwarz MJ, Hennings A, et al. Depression, cytokines and experimental pain: evidence for sex-related association patterns. J Affect Disord. 2011;131(1–3):143–149. doi:10.1016/j.jad.2010.11.017
43. Michaelides A, Zis P. Depression, anxiety and acute pain: links and management challenges. Postgrad Med. 2019;131(7):438–444. doi:10.1080/00325481.2019.1663705
44. Klatzkin RR, Mechlin B, Girdler SS. Menstrual cycle phase does not influence gender differences in experimental pain sensitivity. Eur J Pain. 2010;14(1):77–82. doi:10.1016/j.ejpain.2009.01.002
45. Schaible HG. Peripheral and central mechanisms of pain generation. Analgesia. Springer; 2007:3–28.
46. Schaible HG. Basic mechanisms of deep somatic pain. In: Melzack RWP, editor. Wall and Melzack’s Textbook of Pain. Elsevier; 2006:621–633.
47. Melzack R. Gate control theory: on the evolution of pain concepts. In: Pain Forum. Vol. 5. Elsevier; 1996:128–138.
48. Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE. The interpersonal theory of suicide. Psychol Rev. 2010;117(2):575. doi:10.1037/a0018697
49. Hooley JM, Ho DT, Slater J, Lockshin A. Pain perception and nonsuicidal self-injury: a laboratory investigation. Pers Disord Theory Res Treat. 2018;9(2):123–137.
50. Smith PN, Cukrowicz KC. Capable of suicide: a functional model of the acquired capability component of the interpersonal-psychological theory of suicide. Suicide Life Threat Behav. 2010;40(3):266–275. doi:10.1521/suli.2010.40.3.266
51. Baldessarini RJ. Epidemiology of suicide: recent developments. Epidemiol Psychiatr Sci. 2020;29. doi:10.1017/S2045796019000672
52. Harmanci P. Dünya’daki ve Türkiye’deki intihar vakalarının sosyodemografik özellikler açısından incelenmesi. Hacettepe Univ Fac Health Sci J. 2020;7(2):123–137.
53. Cannon JG, Pierre BAS. Gender differences in host defense mechanisms. J Psychiatr Res. 1997;31(1):99–113. doi:10.1016/S0022-3956(96)00055-6
54. Fillingim RB, King CD, Ribeiro-Dasilva MC, Rahim-Williams B, Riley JL. Sex, gender, and pain: a review of recent clinical and experimental findings. J Pain. 2009;10(5):447–485. doi:10.1016/j.jpain.2008.12.001
55. Stubbs D, Krebs E, Bair M, et al. Sex differences in pain and pain-related disability among primary care patients with chronic musculoskeletal pain. Pain Med. 2010;11(2):232–239. doi:10.1111/j.1526-4637.2009.00760.x
56. Jackson T, Iezzi T, Gunderson J, Nagasaka T, Fritch A. Gender differences in pain perception: the mediating role of self-efficacy beliefs. Sex Roles. 2002;47(11/12):561–568. doi:10.1023/A:1022077922593
57. Zou Y, Li H, Shi C, Lin Y, Zhou H, Zhang J. Efficacy of psychological pain theory–based cognitive therapy in suicidal patients with major depressive disorder: a pilot study. Psychiatry Res. 2017;249:23–29. doi:10.1016/j.psychres.2016.12.046
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
